Dott M Vitacca FERS Divisione di Pneumologia ICS












- Slides: 51

Dott. M Vitacca FERS Divisione di Pneumologia ICS S. Maugeri IRCCS Lumezzane (BS) Italy

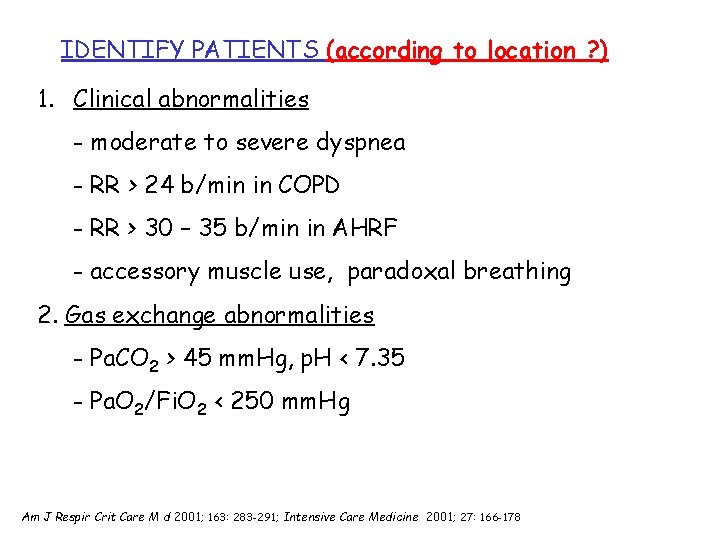
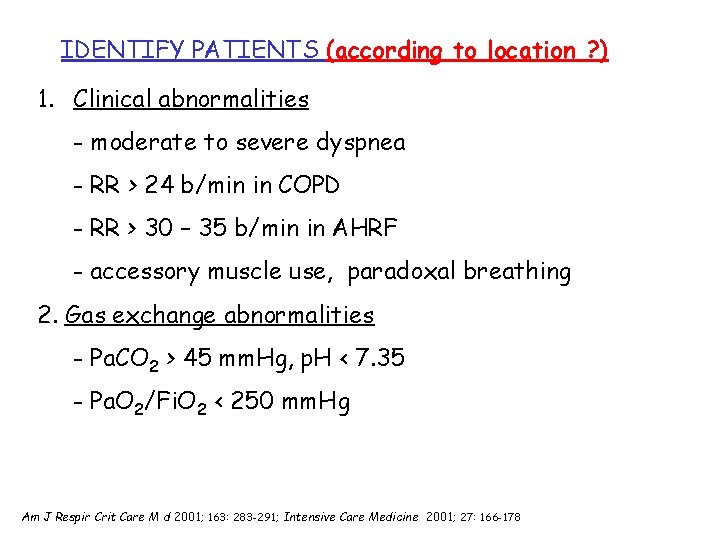
IDENTIFY PATIENTS (according to location ? ) 1. Clinical abnormalities - moderate to severe dyspnea - RR > 24 b/min in COPD - RR > 30 – 35 b/min in AHRF - accessory muscle use, paradoxal breathing 2. Gas exchange abnormalities - Pa. CO 2 > 45 mm. Hg, p. H < 7. 35 - Pa. O 2/Fi. O 2 < 250 mm. Hg Am J Respir Crit Care M d 2001; 163: 283 -291; Intensive Care Medicine 2001; 27: 166 -178

IL PAZIENTE IPOSSICO

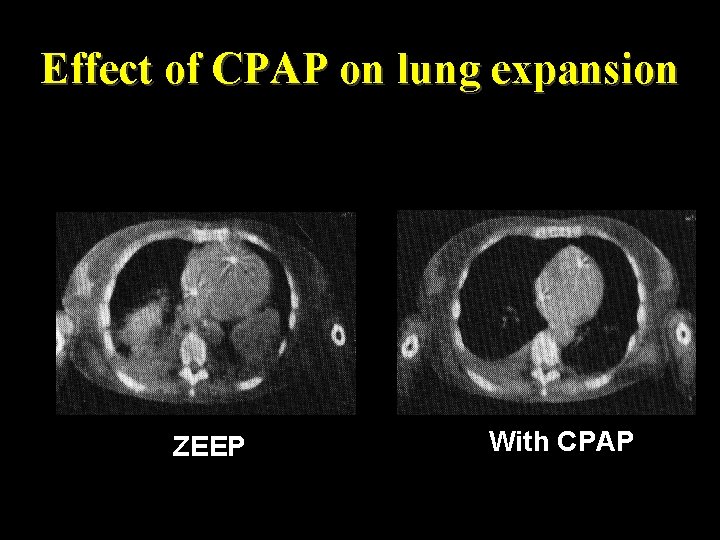
CPAP : Respiratory Effects CPAP intrathoracic pressure Shunt Improve gas Exchange alveolar pressure PEEPi compensation FRC work of breathing atelectasis hypoxemia Pelosi Chest 1996 Pelosi Anesthesiology 1999
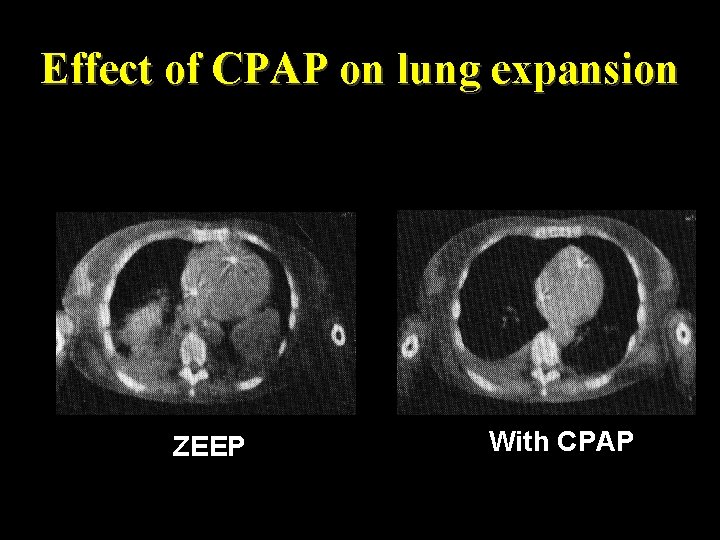
Effect of CPAP on lung expansion ZEEP With CPAP
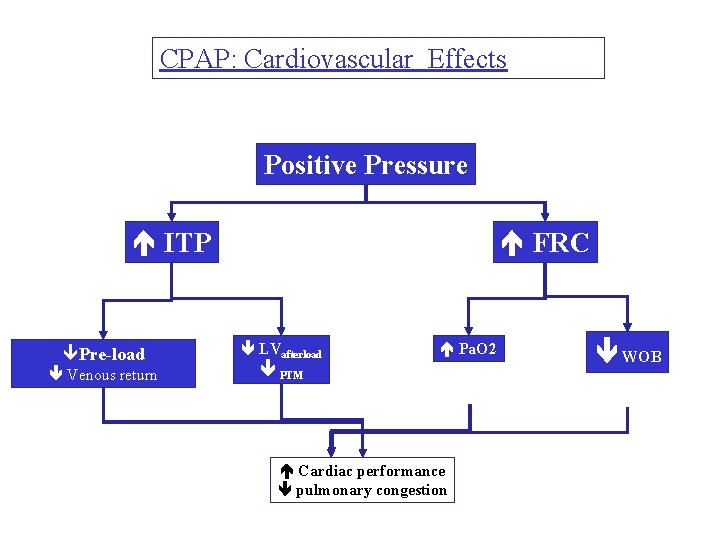
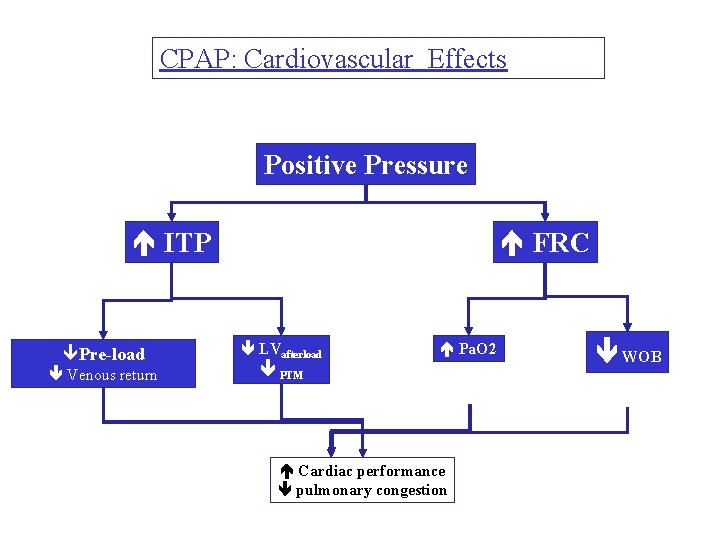
CPAP: Cardiovascular Effects Positive Pressure ITP êPre-load Venous return FRC LVafterload Pa. O 2 PTM Cardiac performance pulmonary congestion WOB

Non invasive CPAP to treat PE or CHF
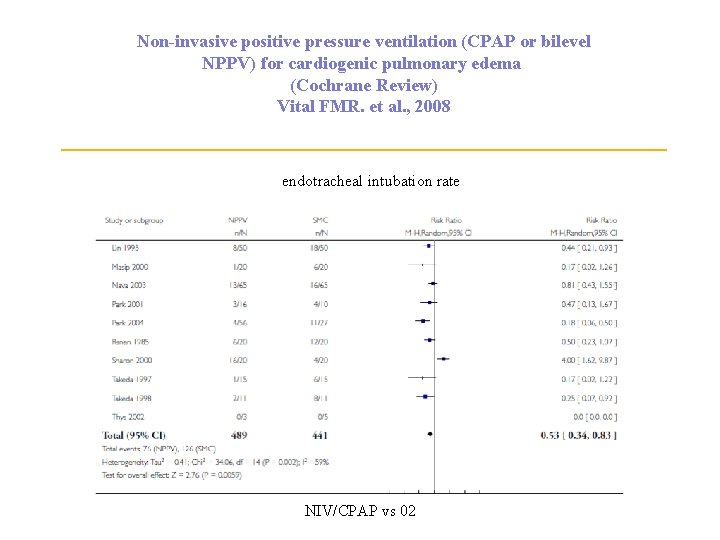
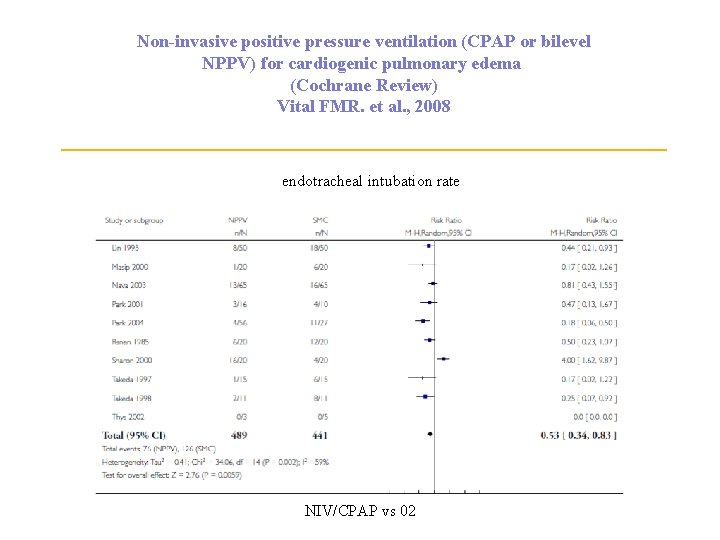
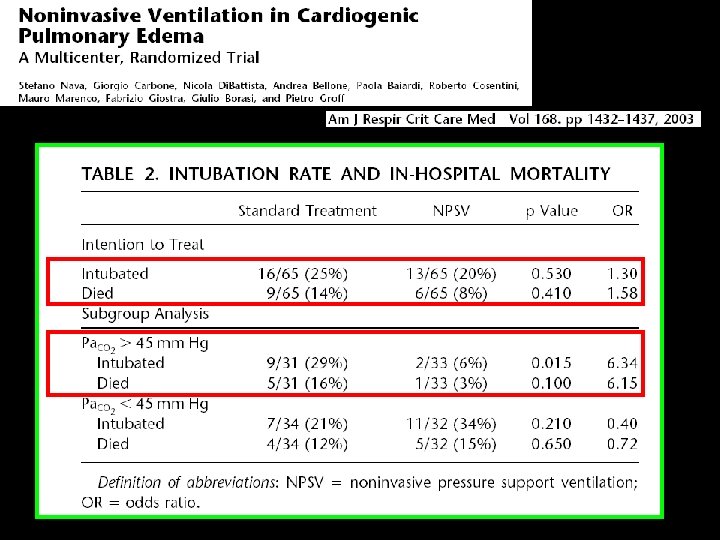
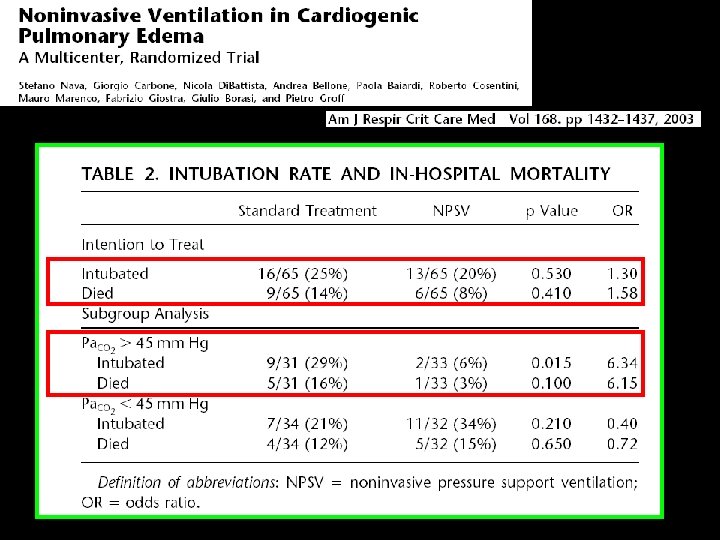
Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema (Cochrane Review) Vital FMR. et al. , 2008 endotracheal intubation rate NIV/CPAP vs 02
Prophylaxis in COPDE • Bilevel NIV may increase mortality (RR 1. 46, 95% CI 0. 64 -3. 35) • Overall low certainty in evidence
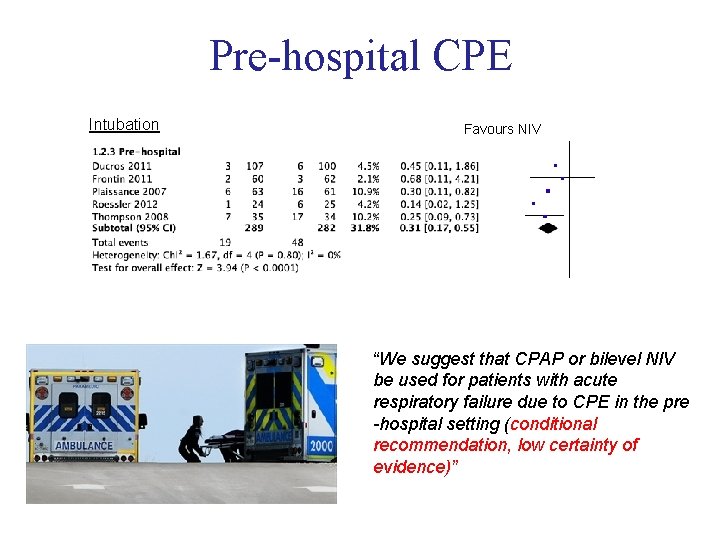
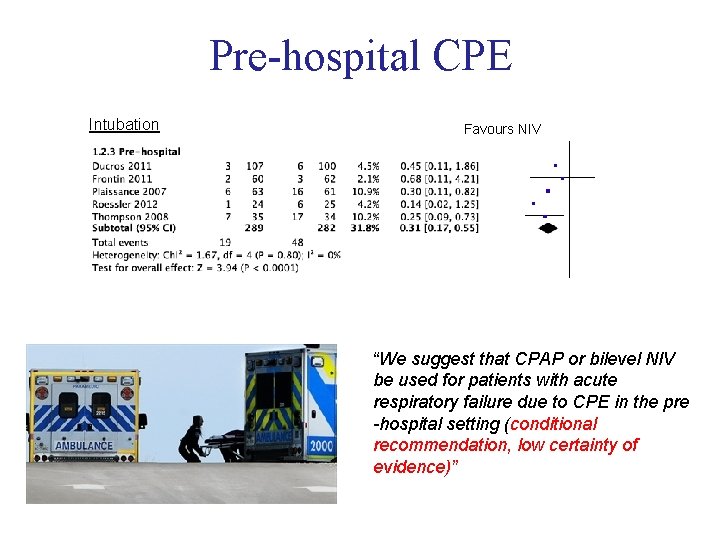
Pre-hospital CPE Intubation Favours NIV “We suggest that CPAP or bilevel NIV be used for patients with acute respiratory failure due to CPE in the pre -hospital setting (conditional recommendation, low certainty of evidence)”
Endotracheal intubation or Non invasive CPAP/PPV to treat Postoperative Hypoxiemic Respiratory Failure ?
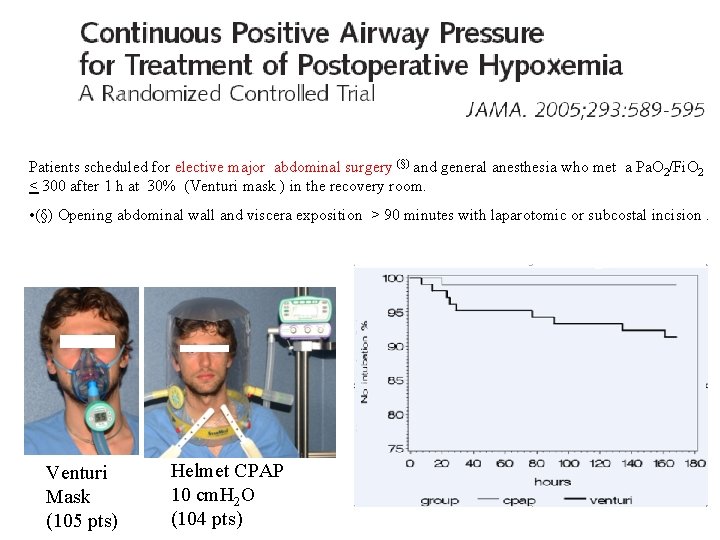
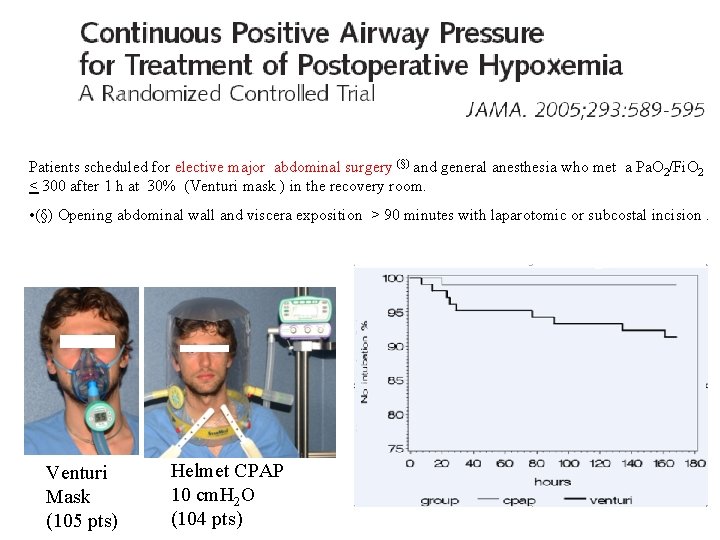
Patients scheduled for elective major abdominal surgery (§) and general anesthesia who met a Pa. O 2/Fi. O 2 < 300 after 1 h at 30% (Venturi mask ) in the recovery room. • (§) Opening abdominal wall and viscera exposition > 90 minutes with laparotomic or subcostal incision. Venturi Mask (105 pts) Helmet CPAP 10 cm. H 2 O (104 pts)
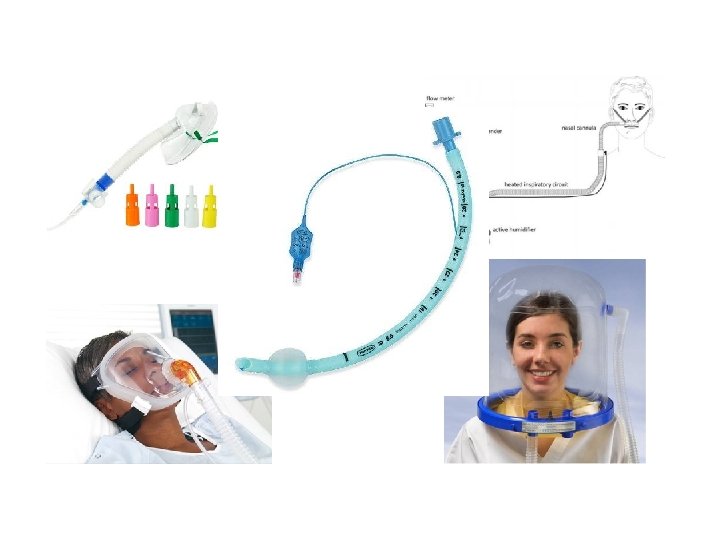
Endotracheal intubation or Non invasive CPAP/PPV to treat Hypoxiemic Respiratory Failure (Pneumonia or ARDS) ?
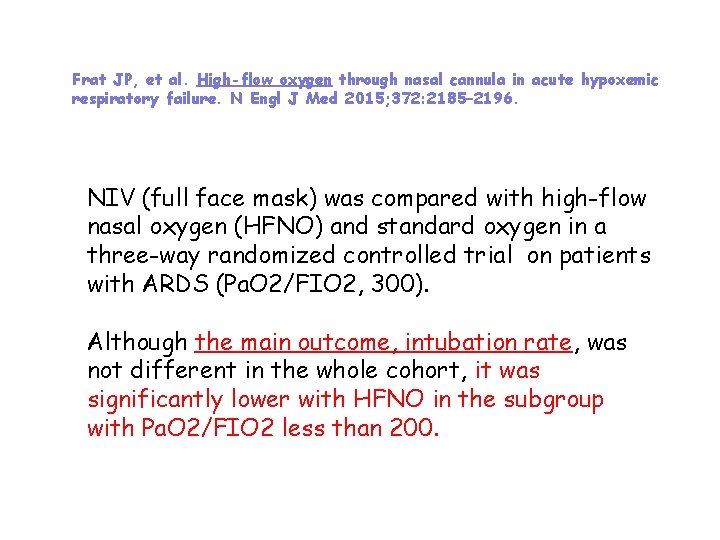
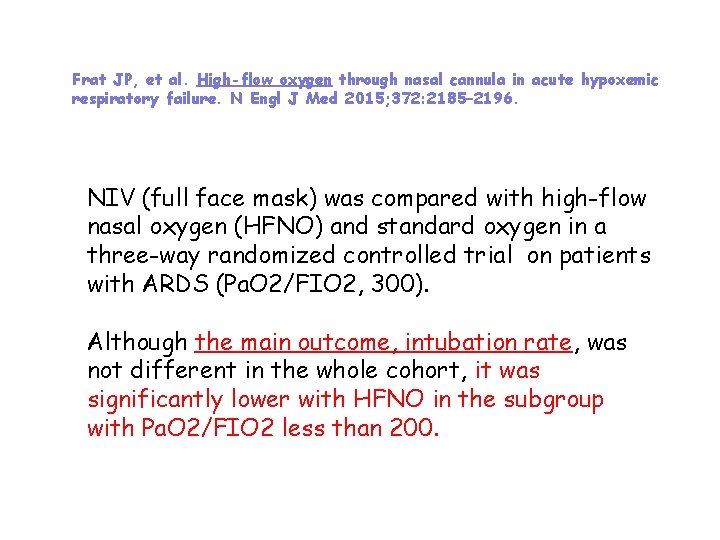
Frat JP, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015; 372: 2185– 2196. NIV (full face mask) was compared with high-flow nasal oxygen (HFNO) and standard oxygen in a three-way randomized controlled trial on patients with ARDS (Pa. O 2/FIO 2, 300). Although the main outcome, intubation rate, was not different in the whole cohort, it was significantly lower with HFNO in the subgroup with Pa. O 2/FIO 2 less than 200.

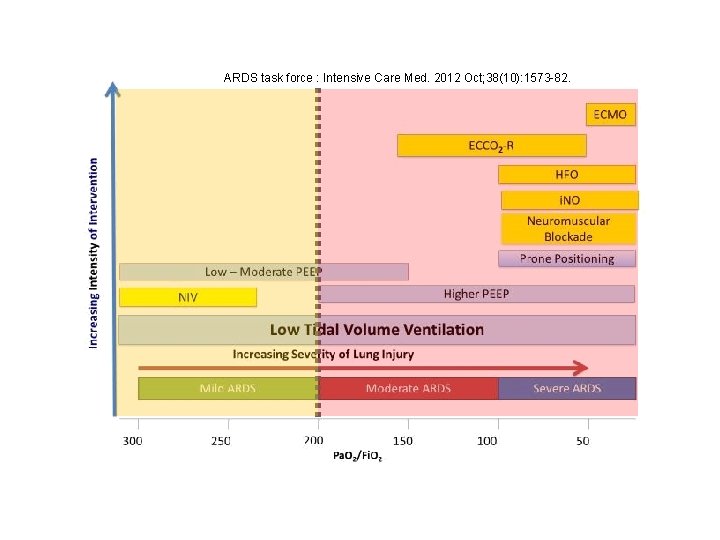
Keenan SP, et al. ; Canadian Critical Care Trials Group/Canadian Critical Care Society Noninvasive Ventilation Guidelines Group. Clinical practice guidelines for the use of noninvasive positive-pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. CMAJ 2011; 183: E 195–E 214. Ferguson ND, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med 2012; 38: 1573– 1582. Recent NIV guidelines have made no recommendation for NIV use in acute lung injury or pneumonia or have suggested its use only for mild ARDS !
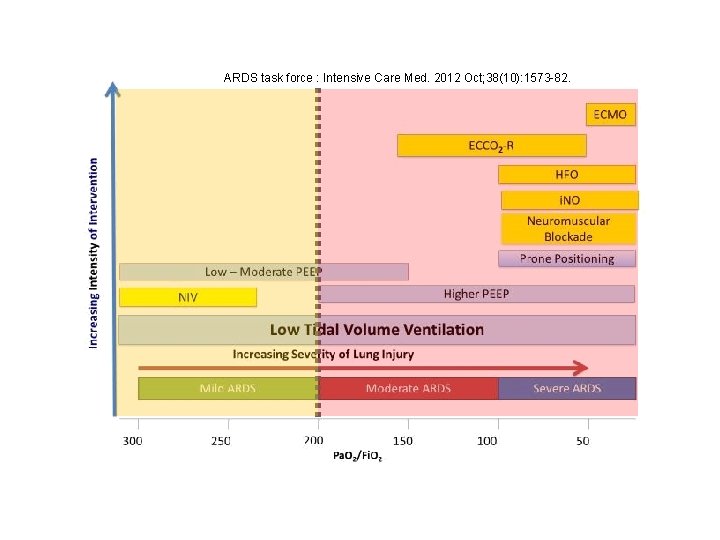
ARDS task force : Intensive Care Med. 2012 Oct; 38(10): 1573 -82.
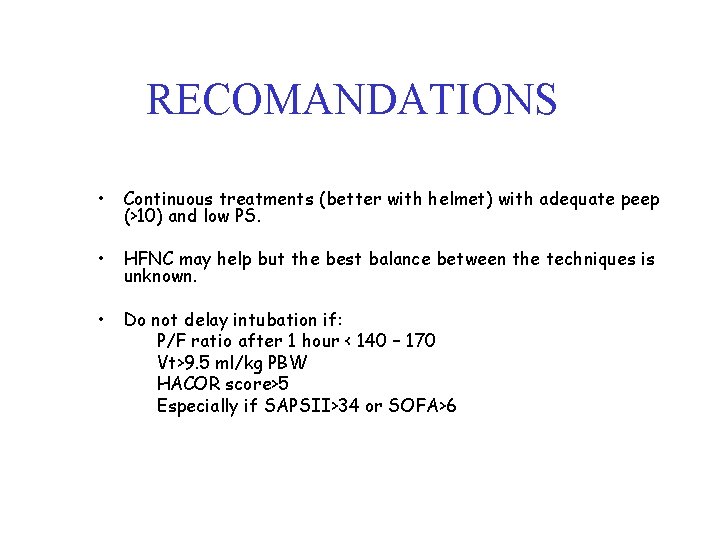
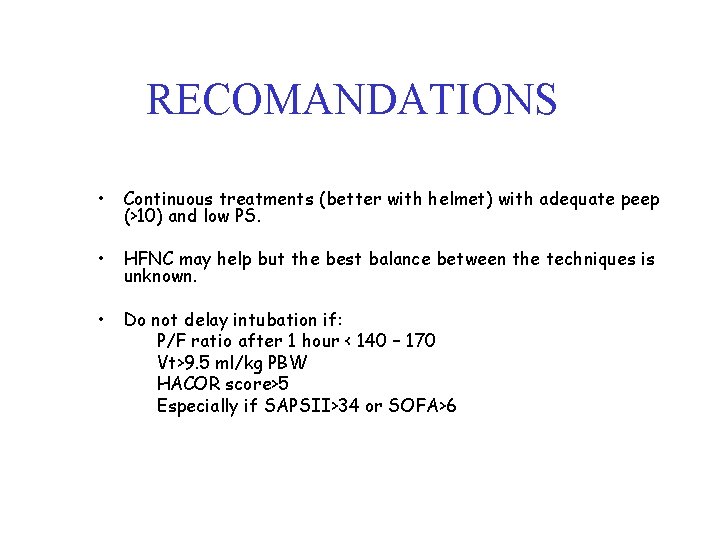
RECOMANDATIONS • Continuous treatments (better with helmet) with adequate peep (>10) and low PS. • HFNC may help but the best balance between the techniques is unknown. • Do not delay intubation if: P/F ratio after 1 hour < 140 – 170 Vt>9. 5 ml/kg PBW HACOR score>5 Especially if SAPSII>34 or SOFA>6

Recommendation Given the uncertainty of evidence we are unable to offer a recommendation on the use of NIV for de novo ARF !!! Justification …NIV use led to a decrease in mortality …and the need for intubation , low certainty of evidence. . . The overall effect in the studies is positive on this end-point, but not for other end-points such as mortality. … There is not enough evidence to recommend its use. …a trial of NIV might be offered to a patient with hypoxaemic respiratory failure, community-acquired pneumonia or early ARDS …. experienced clinical team, Careful selection are close monitoring in the ICU, reassessed early intubate promptly if they are not improving.

IL PAZIENTE IPERCAPNICO
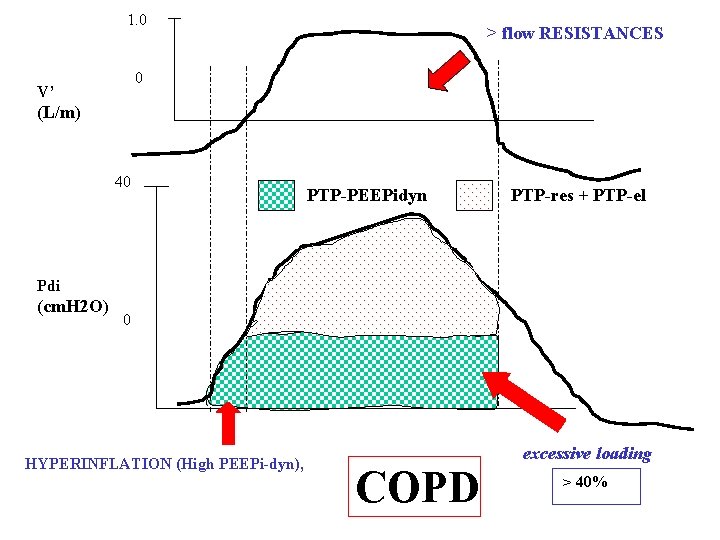
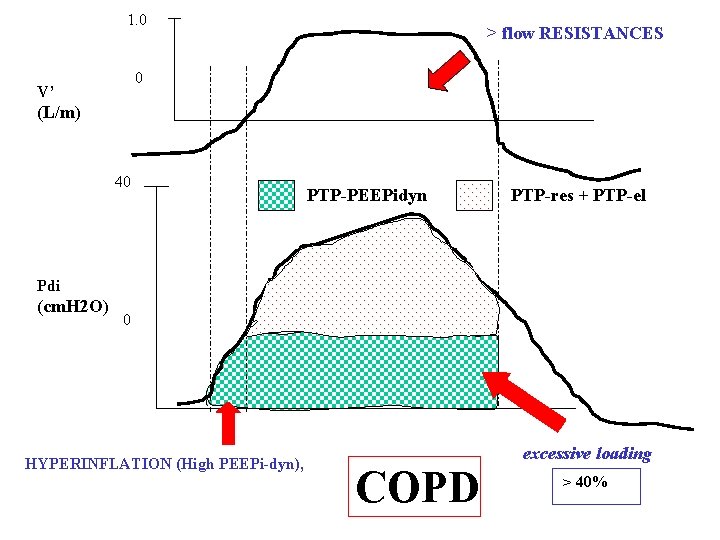
1. 0 > flow RESISTANCES 0 V’ (L/m) 40 PTP-PEEPidyn PTP-res + PTP-el Pdi (cm. H 2 O) 0 HYPERINFLATION (High PEEPi-dyn), excessive loading COPD > 40%
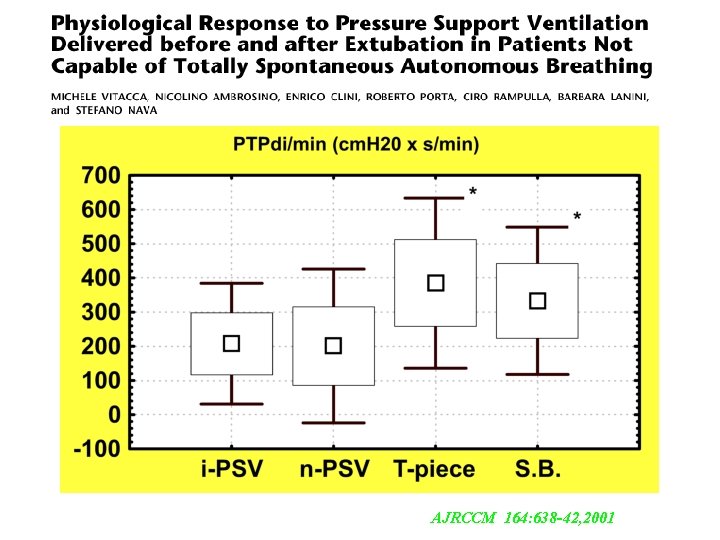
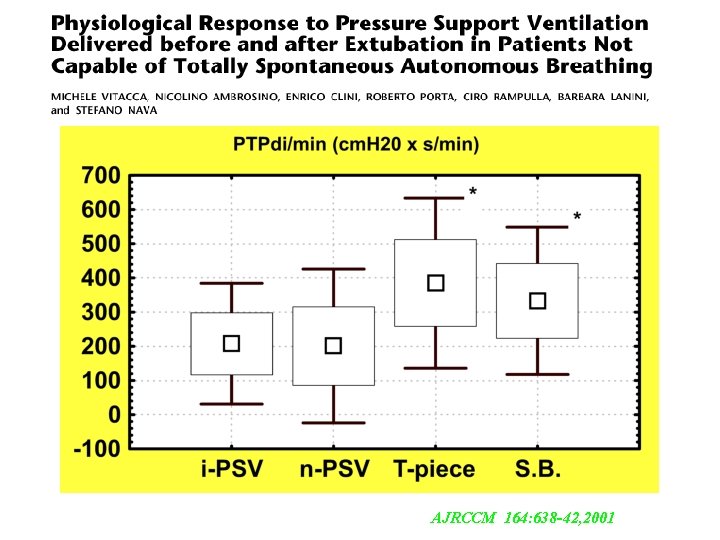
AJRCCM 164: 638 -42, 2001
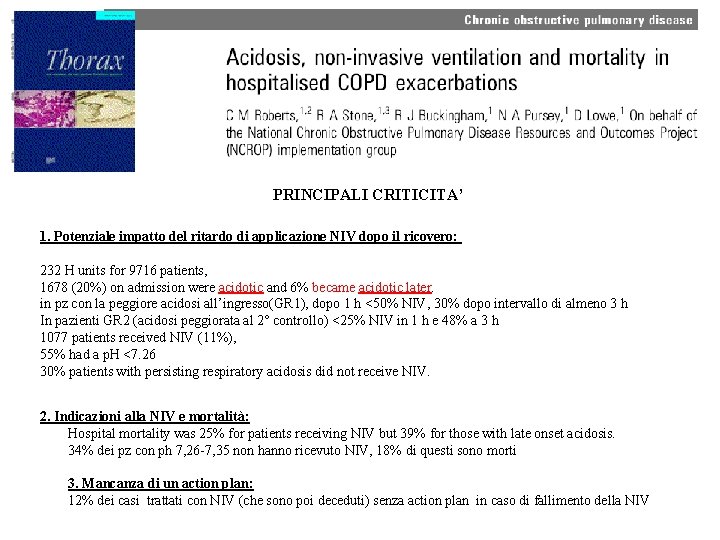
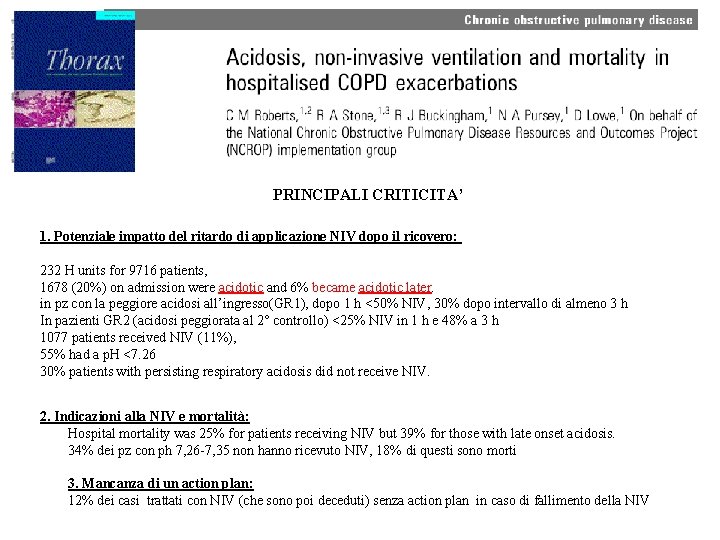
PRINCIPALI CRITICITA’ 1. Potenziale impatto del ritardo di applicazione NIV dopo il ricovero: 232 H units for 9716 patients, 1678 (20%) on admission were acidotic and 6% became acidotic later. in pz con la peggiore acidosi all’ingresso(GR 1), dopo 1 h <50% NIV, 30% dopo intervallo di almeno 3 h In pazienti GR 2 (acidosi peggiorata al 2° controllo) <25% NIV in 1 h e 48% a 3 h 1077 patients received NIV (11%), 55% had a p. H <7. 26 30% patients with persisting respiratory acidosis did not receive NIV. 2. Indicazioni alla NIV e mortalità: Hospital mortality was 25% for patients receiving NIV but 39% for those with late onset acidosis. 34% dei pz con ph 7, 26 -7, 35 non hanno ricevuto NIV, 18% di questi sono morti 3. Mancanza di un action plan: 12% dei casi trattati con NIV (che sono poi deceduti) senza action plan in caso di fallimento della NIV
Prophylaxis in COPDE “We suggest NIV not be used in patients with hypercapnia who are not acidotic in the setting of a COPD exacerbation (conditional recommendation, low certainty in the evidence)”
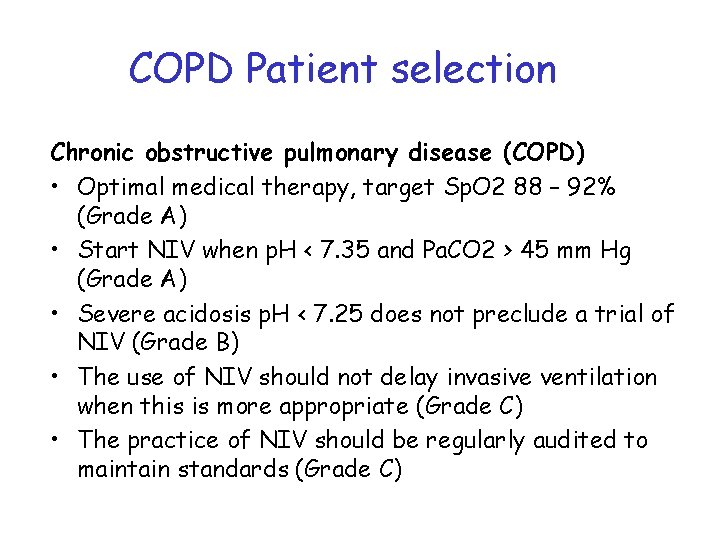
COPD Patient selection Chronic obstructive pulmonary disease (COPD) • Optimal medical therapy, target Sp. O 2 88 – 92% (Grade A) • Start NIV when p. H < 7. 35 and Pa. CO 2 > 45 mm Hg (Grade A) • Severe acidosis p. H < 7. 25 does not preclude a trial of NIV (Grade B) • The use of NIV should not delay invasive ventilation when this is more appropriate (Grade C) • The practice of NIV should be regularly audited to maintain standards (Grade C)
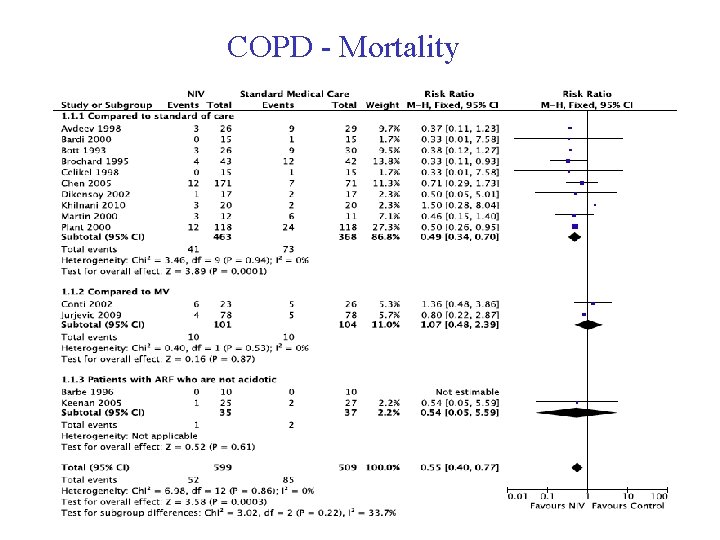
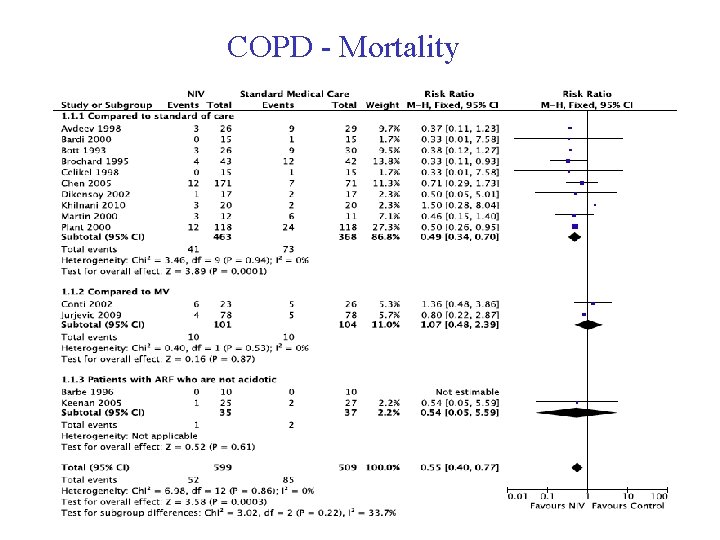
COPD - Mortality
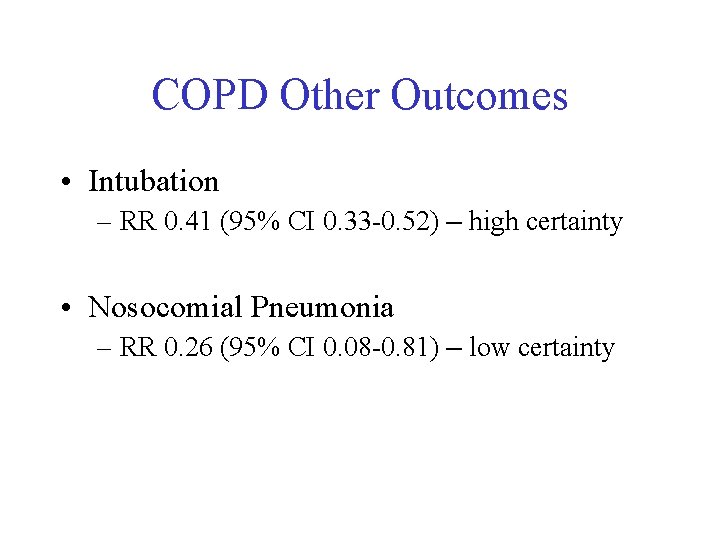
COPD Other Outcomes • Intubation – RR 0. 41 (95% CI 0. 33 -0. 52) – high certainty • Nosocomial Pneumonia – RR 0. 26 (95% CI 0. 08 -0. 81) – low certainty
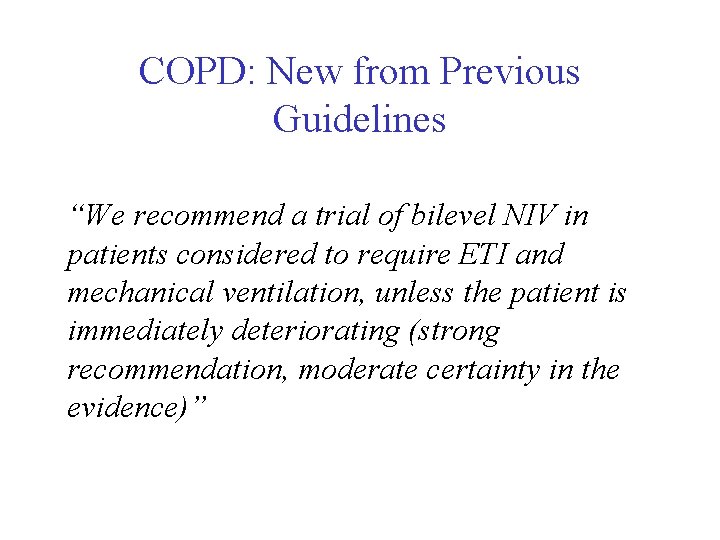
COPD: New from Previous Guidelines “We recommend a trial of bilevel NIV in patients considered to require ETI and mechanical ventilation, unless the patient is immediately deteriorating (strong recommendation, moderate certainty in the evidence)”
Others conditions

Pandemic Viral Illness • Mortality – Observational studies only
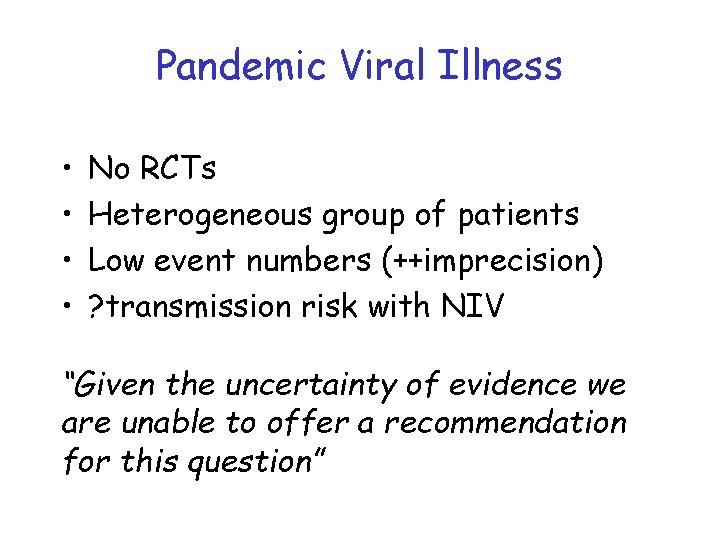
Pandemic Viral Illness • • No RCTs Heterogeneous group of patients Low event numbers (++imprecision) ? transmission risk with NIV “Given the uncertainty of evidence we are unable to offer a recommendation for this question”

Chest Trauma • Heterogenous population – Severity of illness, rib # vs flail chest, other injuries • Various comparators – Supplemental oxygen vs invasive ventilation “We suggest NIV for chest trauma patients with ARF. (Conditional recommendation, moderate certainty of evidence)”
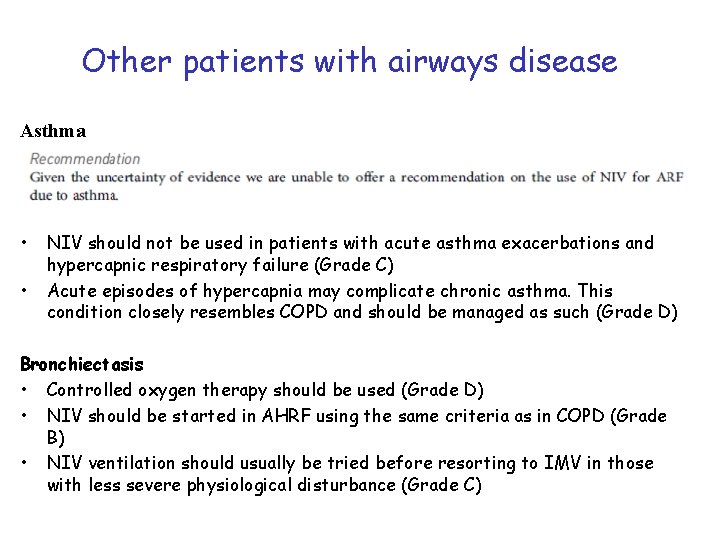
Other patients with airways disease Asthma • • NIV should not be used in patients with acute asthma exacerbations and hypercapnic respiratory failure (Grade C) Acute episodes of hypercapnia may complicate chronic asthma. This condition closely resembles COPD and should be managed as such (Grade D) Bronchiectasis • Controlled oxygen therapy should be used (Grade D) • NIV should be started in AHRF using the same criteria as in COPD (Grade B) • NIV ventilation should usually be tried before resorting to IMV in those with less severe physiological disturbance (Grade C)
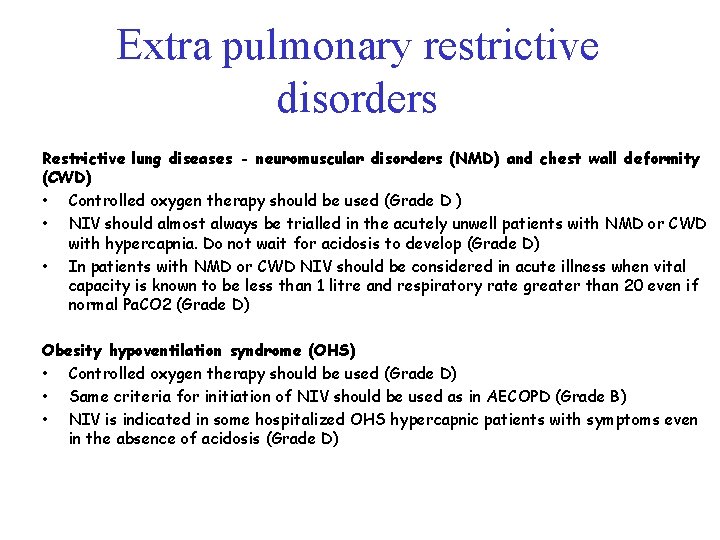
Extra pulmonary restrictive disorders Restrictive lung diseases - neuromuscular disorders (NMD) and chest wall deformity (CWD) • Controlled oxygen therapy should be used (Grade D ) • NIV should almost always be trialled in the acutely unwell patients with NMD or CWD with hypercapnia. Do not wait for acidosis to develop (Grade D) • In patients with NMD or CWD NIV should be considered in acute illness when vital capacity is known to be less than 1 litre and respiratory rate greater than 20 even if normal Pa. CO 2 (Grade D) Obesity hypoventilation syndrome (OHS) • Controlled oxygen therapy should be used (Grade D) • Same criteria for initiation of NIV should be used as in AECOPD (Grade B) • NIV is indicated in some hospitalized OHS hypercapnic patients with symptoms even in the absence of acidosis (Grade D)
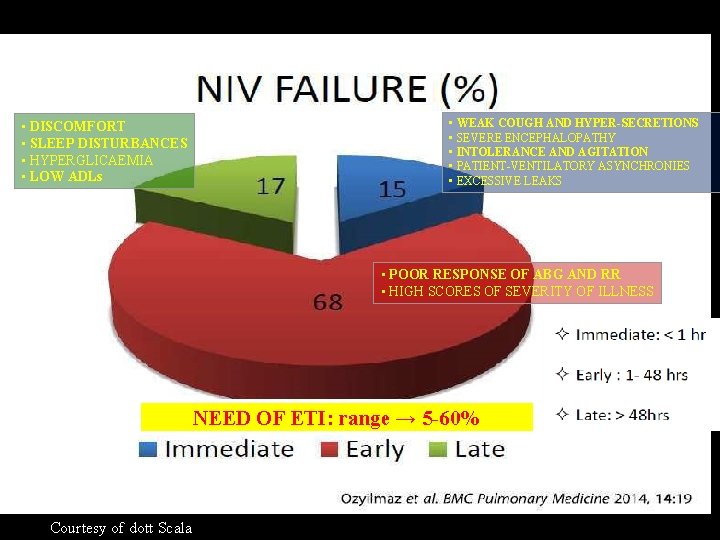
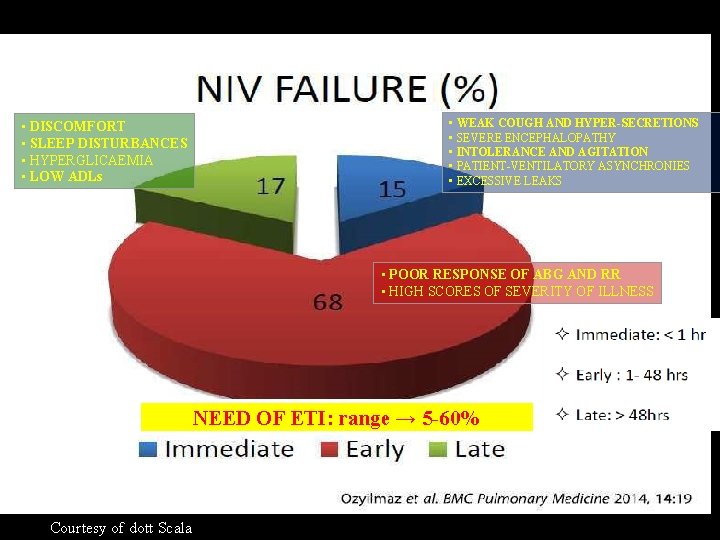
• DISCOMFORT • SLEEP DISTURBANCES • HYPERGLICAEMIA • LOW ADLs • WEAK COUGH AND HYPER-SECRETIONS • SEVERE ENCEPHALOPATHY • INTOLERANCE AND AGITATION • PATIENT-VENTILATORY ASYNCHRONIES • EXCESSIVE LEAKS • POOR RESPONSE OF ABG AND RR • HIGH SCORES OF SEVERITY OF ILLNESS NEED OF ETI: range → 5 -60% Courtesy of dott Scala
La giusta location
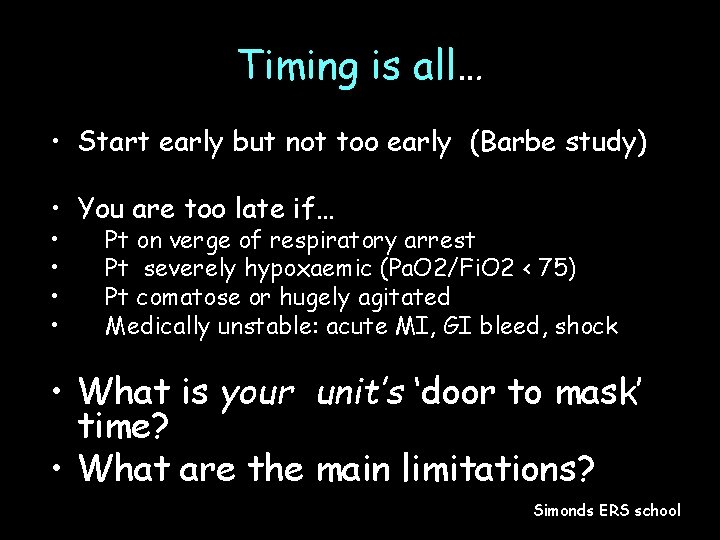
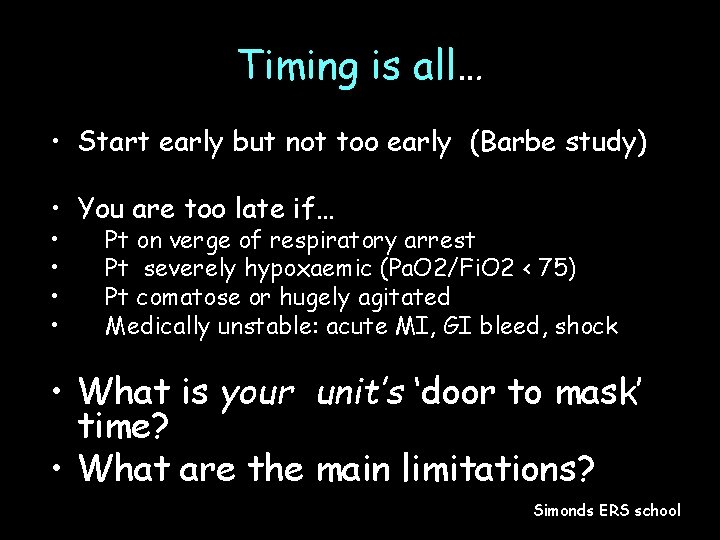
Timing is all… • Start early but not too early (Barbe study) • You are too late if… • • Pt on verge of respiratory arrest Pt severely hypoxaemic (Pa. O 2/Fi. O 2 < 75) Pt comatose or hugely agitated Medically unstable: acute MI, GI bleed, shock • What is your unit’s ‘door to mask’ time? • What are the main limitations? Simonds ERS school
Il training adeguato

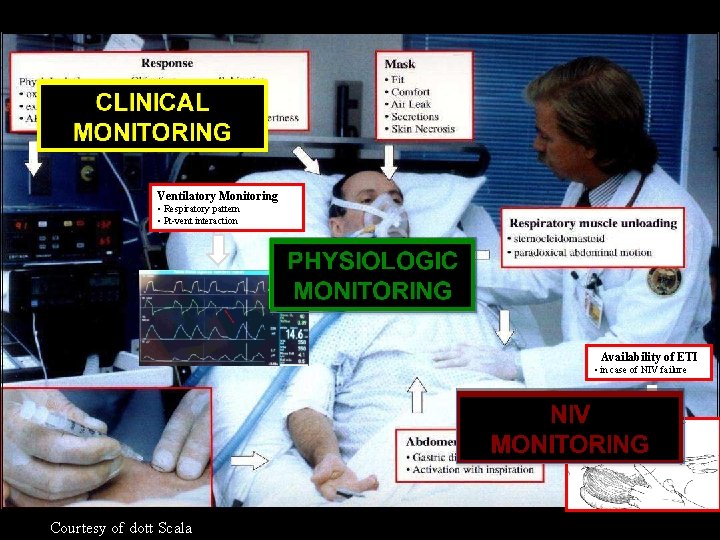
Monitoraggio
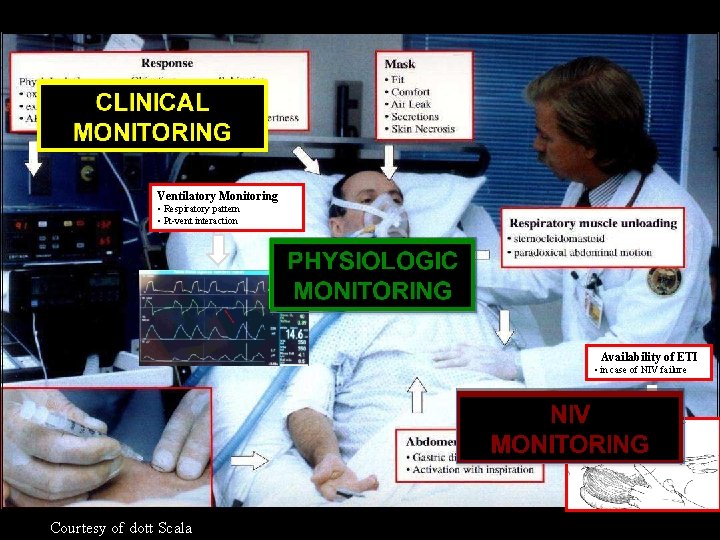
Ventilatory Monitoring • Respiratory pattern • Pt-vent interaction Availability of ETI • in case of NIV failure Courtesy of dott Scala
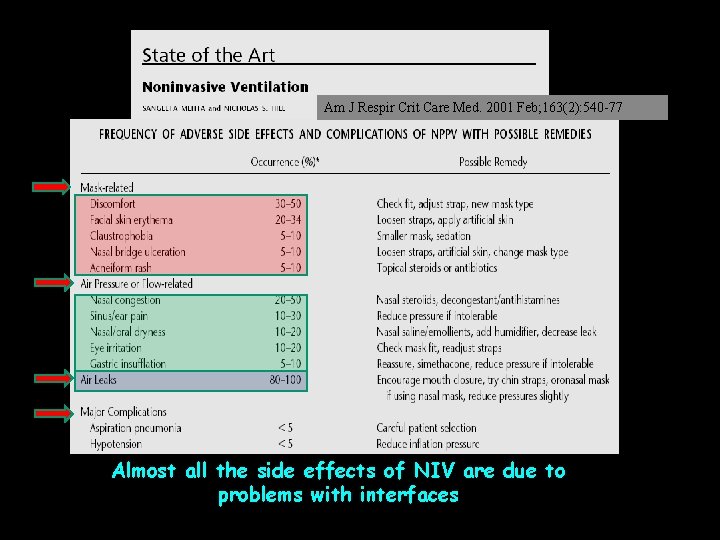
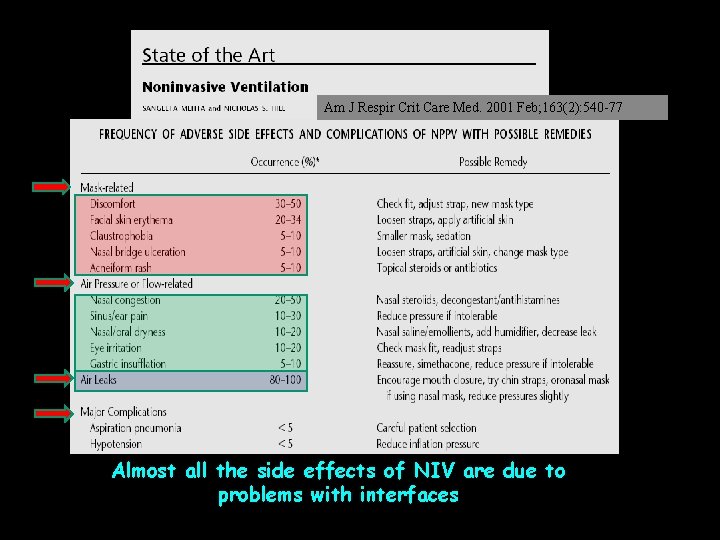
Am J Respir Crit Care Med. 2001 Feb; 163(2): 540 -77 Almost all the side effects of NIV are due to problems with interfaces
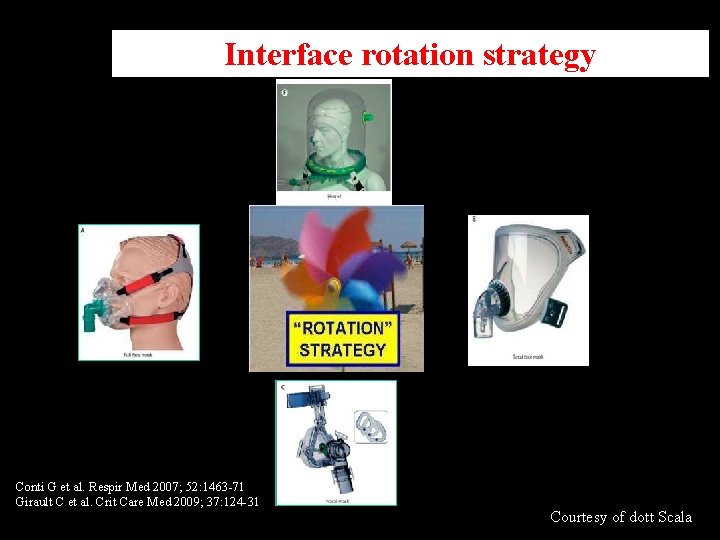
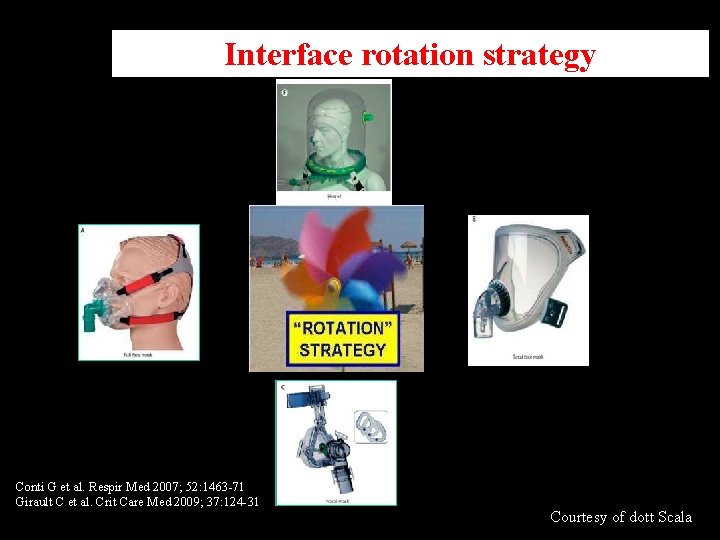
Interface rotation strategy Conti G et al. Respir Med 2007; 52: 1463 -71 Girault C et al. Crit Care Med 2009; 37: 124 -31 Courtesy of dott Scala
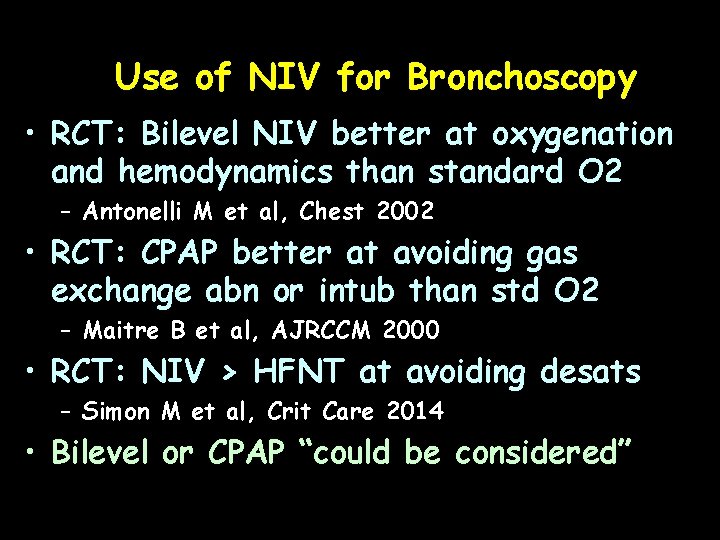
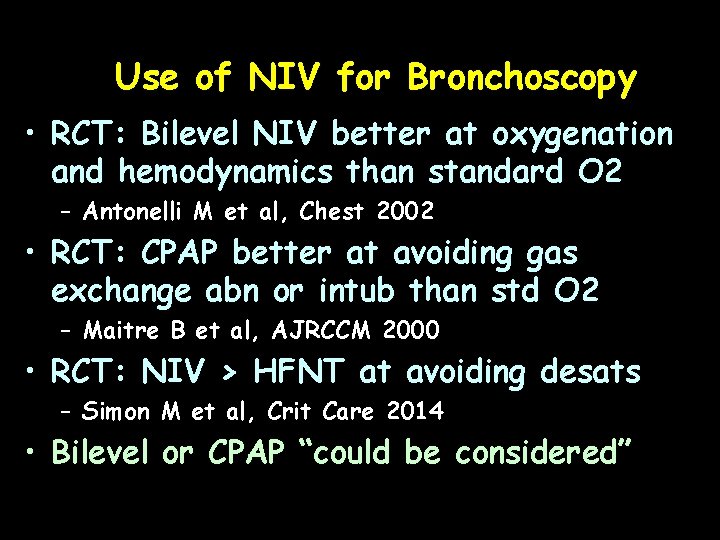
Use of NIV for Bronchoscopy • RCT: Bilevel NIV better at oxygenation and hemodynamics than standard O 2 – Antonelli M et al, Chest 2002 • RCT: CPAP better at avoiding gas exchange abn or intub than std O 2 – Maitre B et al, AJRCCM 2000 • RCT: NIV > HFNT at avoiding desats – Simon M et al, Crit Care 2014 • Bilevel or CPAP “could be considered”

Palliative Care • NIV in patients with respiratory failure receiving palliative care? – NIV improved dyspnea – lowered Borg scale by 0. 89 points (95% CI 0. 79 -0. 99) – NIV decreased opioid requirement – 32. 4 mg less morphine equivalents (95% CI 17. 4 -47. 4) “We suggest offering NIV to dyspnoeic patients for palliation in the setting of terminal cancer or other terminal conditions. (Conditional recommendation, moderate certainty of evidence)”
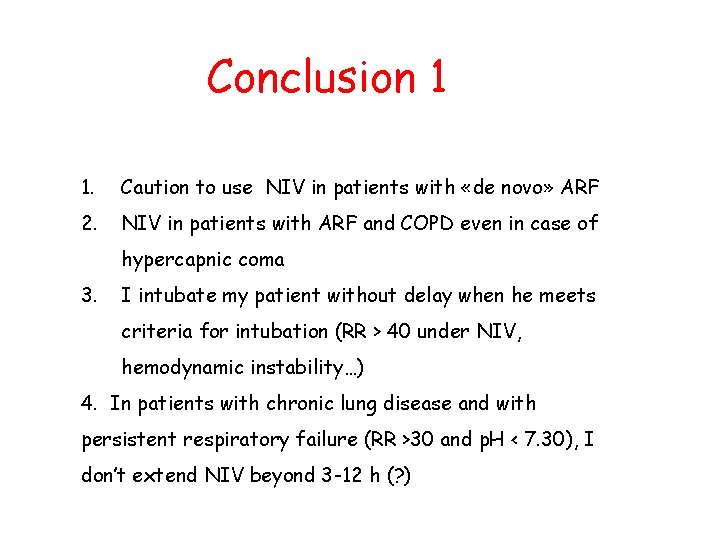
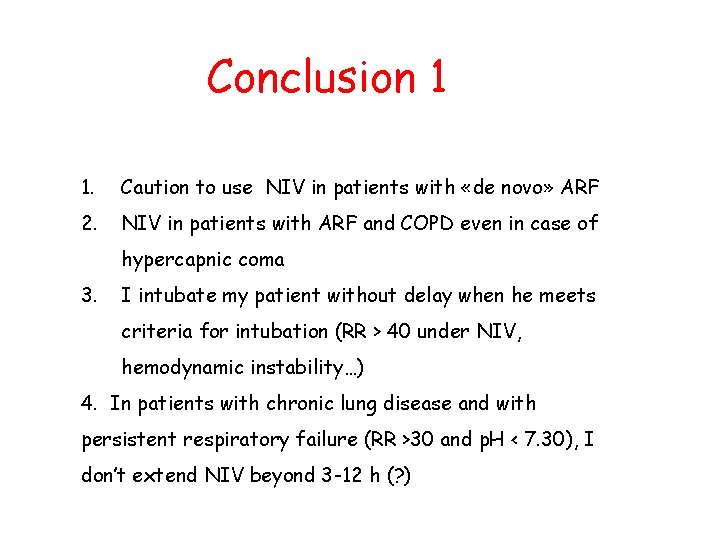
Conclusion 1 1. Caution to use NIV in patients with «de novo» ARF 2. NIV in patients with ARF and COPD even in case of hypercapnic coma 3. I intubate my patient without delay when he meets criteria for intubation (RR > 40 under NIV, hemodynamic instability…) 4. In patients with chronic lung disease and with persistent respiratory failure (RR >30 and p. H < 7. 30), I don’t extend NIV beyond 3 -12 h (? )
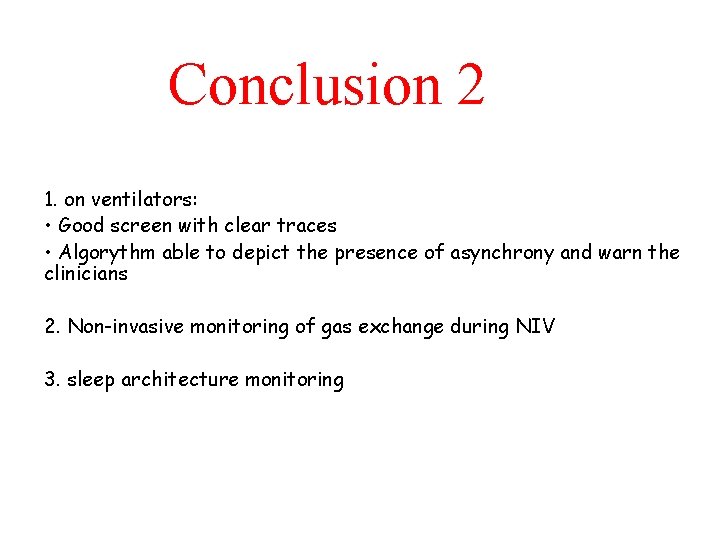
Conclusion 2 1. on ventilators: • Good screen with clear traces • Algorythm able to depict the presence of asynchrony and warn the clinicians 2. Non-invasive monitoring of gas exchange during NIV 3. sleep architecture monitoring
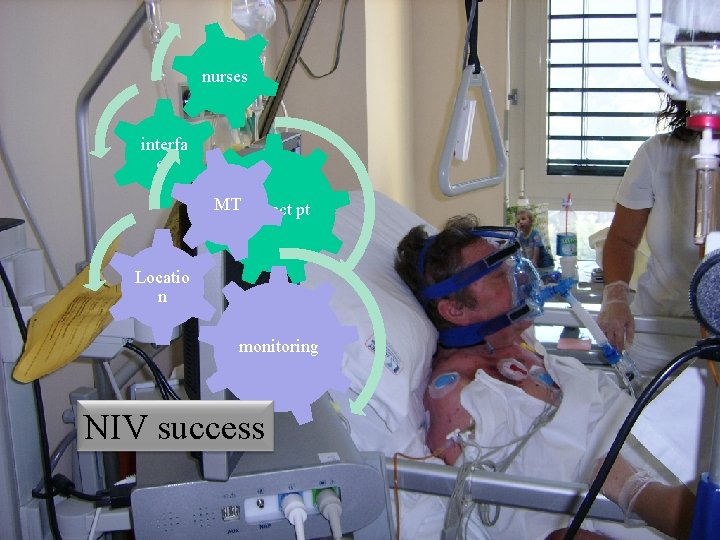
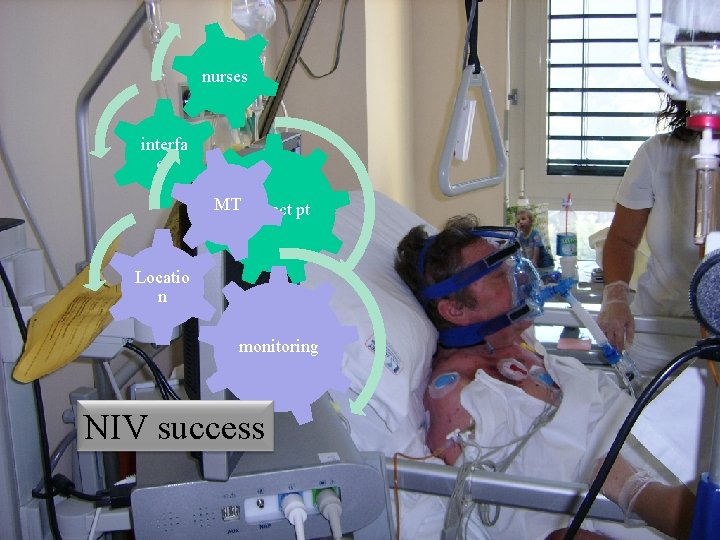
nurses interfa ce MTCorrect pt Locatio n monitoring NIV success
 Ics pneumologia
Ics pneumologia Michele vitacca model
Michele vitacca model Zobor nemocnica
Zobor nemocnica Curso nacional de atualização em pneumologia
Curso nacional de atualização em pneumologia Pneumologia gaslini
Pneumologia gaslini Ics 400: advanced ics for complex incidents-aberdeen
Ics 400: advanced ics for complex incidents-aberdeen Dott.ssa lucia lospalluti
Dott.ssa lucia lospalluti Dott. pier luigi bruni
Dott. pier luigi bruni Dott cardillo pneumologo
Dott cardillo pneumologo Giovanni lupoli endocrinologo
Giovanni lupoli endocrinologo Dieta menopausa dott migliaccio
Dieta menopausa dott migliaccio Dott arpe gastroenterologa la spezia
Dott arpe gastroenterologa la spezia Luana gualtieri
Luana gualtieri Dott riccardo simoni
Dott riccardo simoni Dolore pelvico cronico
Dolore pelvico cronico Dott ssa alessandra muliere
Dott ssa alessandra muliere Dott garozzo cremona
Dott garozzo cremona Pafi medica sud srl
Pafi medica sud srl Dott's
Dott's Straface abano
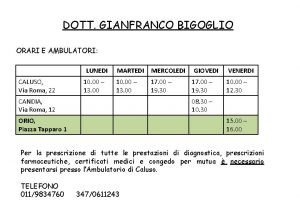
Straface abano Poliambulatorio caluso via roma 22
Poliambulatorio caluso via roma 22 Dott ssa benilde cosmi bologna
Dott ssa benilde cosmi bologna Monika hengge
Monika hengge Dott.ssa deutsch
Dott.ssa deutsch Dott mellino neurologo
Dott mellino neurologo Scala di borg dispnea
Scala di borg dispnea Alessandra guarino amato
Alessandra guarino amato Deutsch
Deutsch Dott calista donato rimini
Dott calista donato rimini Dott trabace ortopedico matera
Dott trabace ortopedico matera Ferrero rocher
Ferrero rocher Cesare burti
Cesare burti Milli cardiologo firenze
Milli cardiologo firenze Dott. giovanni magrì gastroenterologo acireale
Dott. giovanni magrì gastroenterologo acireale Silvia consorti
Silvia consorti Marco gaffi urologo
Marco gaffi urologo Dott claudio andreoli
Dott claudio andreoli Lezioni di fisica giuseppe ruffo
Lezioni di fisica giuseppe ruffo Dott carluccio urologo tricase
Dott carluccio urologo tricase Nomenkomposita
Nomenkomposita Dott belloli oculista borgomanero
Dott belloli oculista borgomanero Dott brunori pneumologo
Dott brunori pneumologo Elena bozzola pediatra
Elena bozzola pediatra Dott.ssa deutsch
Dott.ssa deutsch Pediatra natali sasso marconi
Pediatra natali sasso marconi Paolo ragni ortopedico
Paolo ragni ortopedico Muciropina
Muciropina Dott ssa piccinni endocrinologa
Dott ssa piccinni endocrinologa Dott tarroni rimini
Dott tarroni rimini Dott nano giuseppe
Dott nano giuseppe Dott
Dott Alessandro buonomo allergologo
Alessandro buonomo allergologo