Dose from Computed Tomography CT Patient Dose Tube
Dose from Computed Tomography
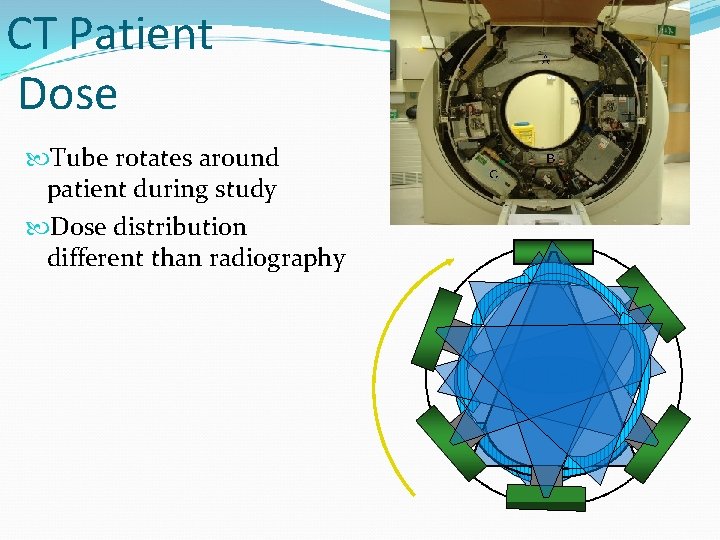
CT Patient Dose Tube rotates around patient during study Dose distribution different than radiography Patient
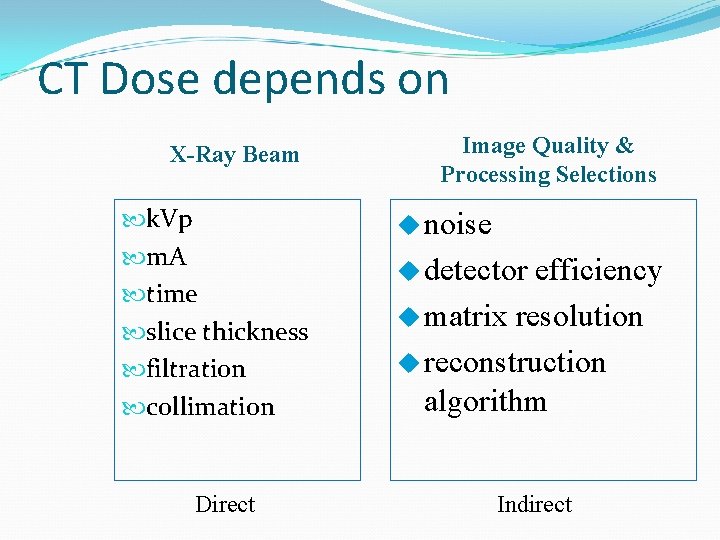
CT Dose depends on X-Ray Beam k. Vp m. A time slice thickness filtration collimation Direct Image Quality & Processing Selections u noise u detector efficiency u matrix resolution u reconstruction algorithm Indirect
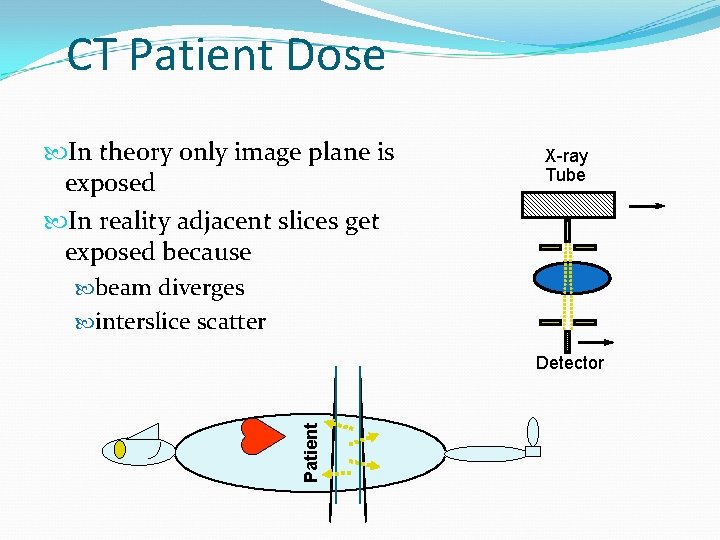
CT Patient Dose In theory only image plane is exposed In reality adjacent slices get exposed because beam diverges interslice scatter X-ray Tube Patient Detector
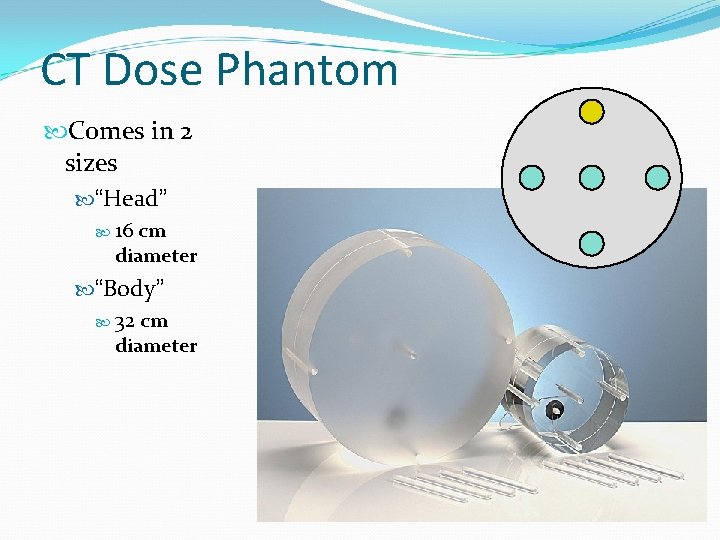
CT Dose Phantom Comes in 2 sizes “Head” 16 cm diameter “Body” 32 cm diameter
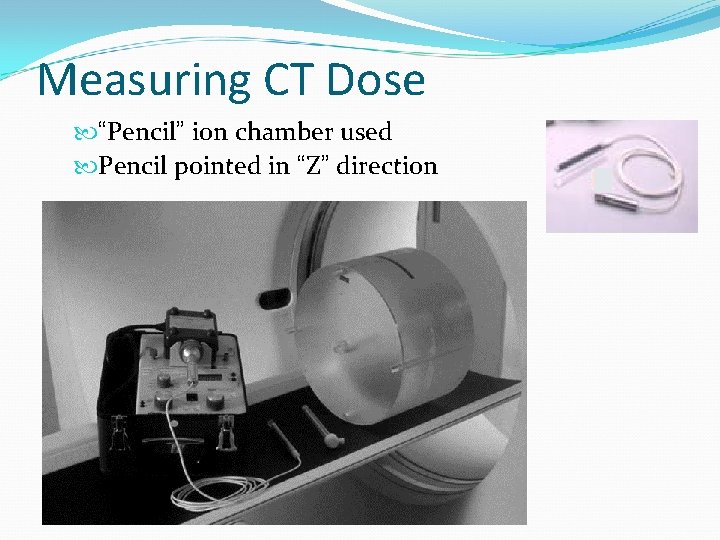
Measuring CT Dose “Pencil” ion chamber used Pencil pointed in “Z” direction
Measurement Procedure Standardize protocol k. Vp m. As scan time slice thickness table movement field of view Select appropriate phantom head body
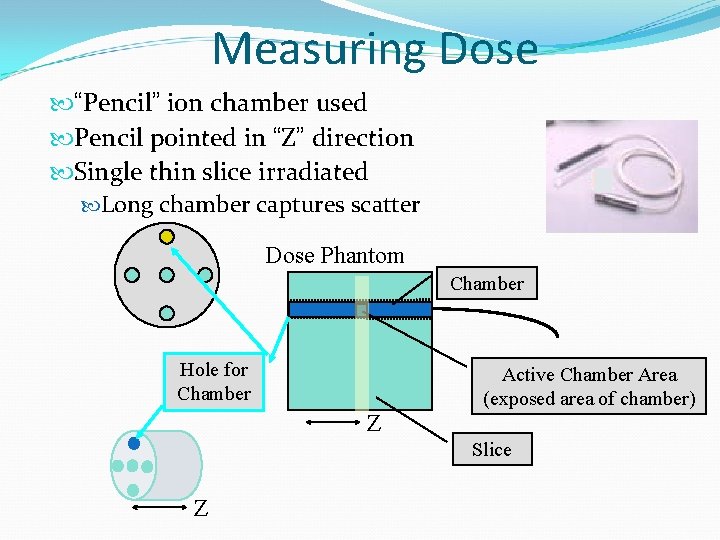
Measuring Dose “Pencil” ion chamber used Pencil pointed in “Z” direction Single thin slice irradiated Long chamber captures scatter Dose Phantom Chamber Hole for Chamber Active Chamber Area (exposed area of chamber) Z Slice Z
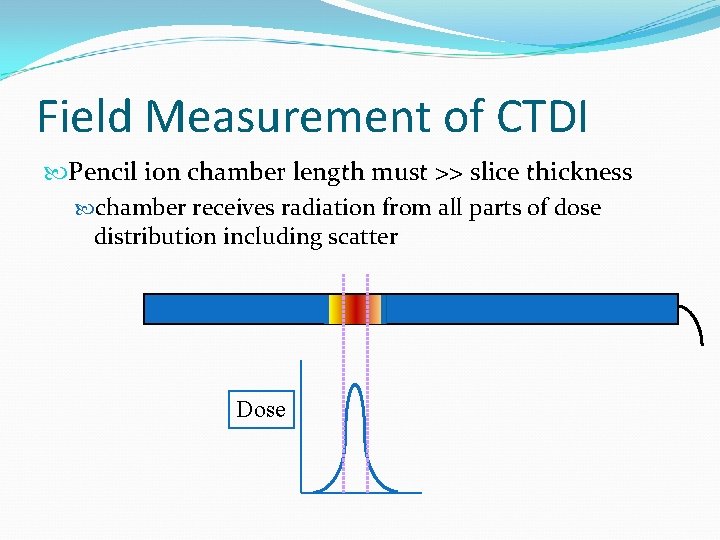
Field Measurement of CTDI Pencil ion chamber length must >> slice thickness chamber receives radiation from all parts of dose distribution including scatter Dose
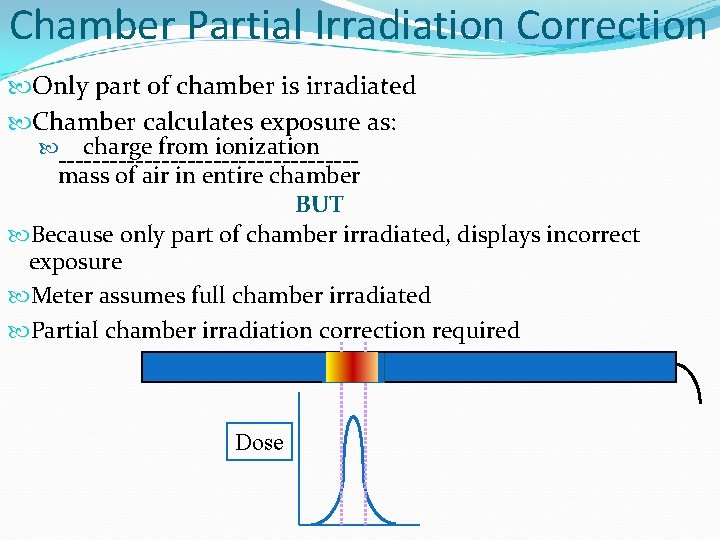
Chamber Partial Irradiation Correction Only part of chamber is irradiated Chamber calculates exposure as: charge from ionization -----------------mass of air in entire chamber BUT Because only part of chamber irradiated, displays incorrect exposure Meter assumes full chamber irradiated Partial chamber irradiation correction required Dose
CT Dose Conventions CTDI (Computed Tomography Dose Index) CTDI 100 CTDIW CTDIVOL DLP (Dose Length Product) Effective Dose
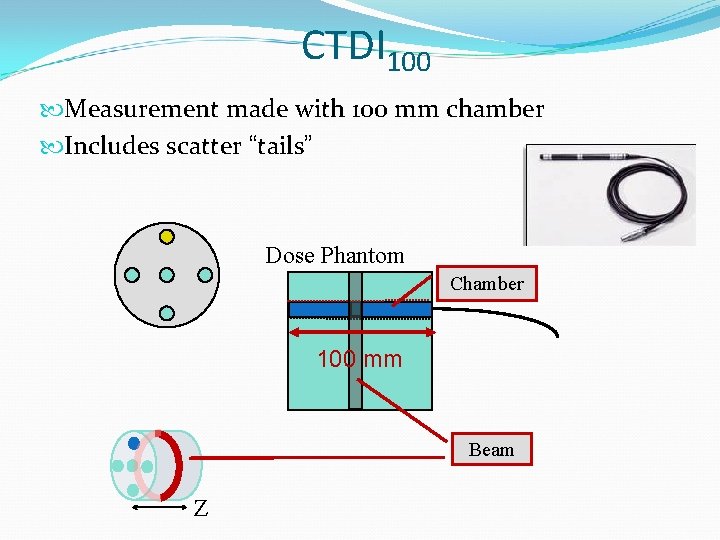
CTDI 100 Measurement made with 100 mm chamber Includes scatter “tails” Dose Phantom Chamber 100 mm Beam Z
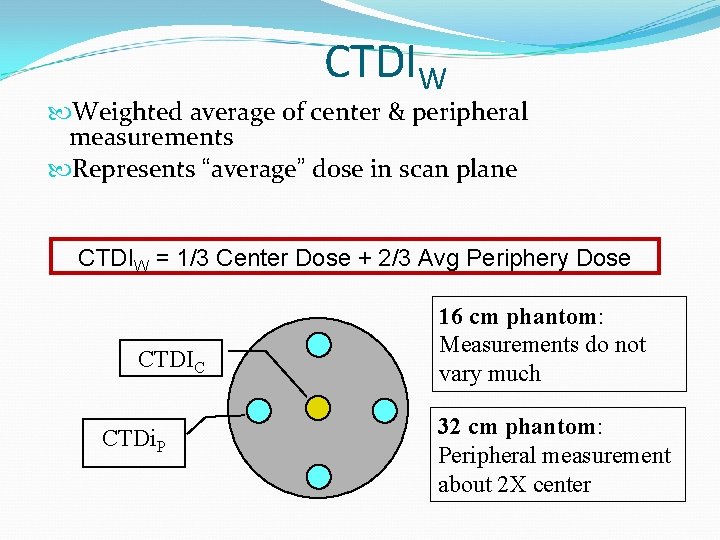
CTDIW Weighted average of center & peripheral measurements Represents “average” dose in scan plane CTDIW = 1/3 Center Dose + 2/3 Avg Periphery Dose CTDIC CTDi. P 16 cm phantom: Measurements do not vary much 32 cm phantom: Peripheral measurement about 2 X center
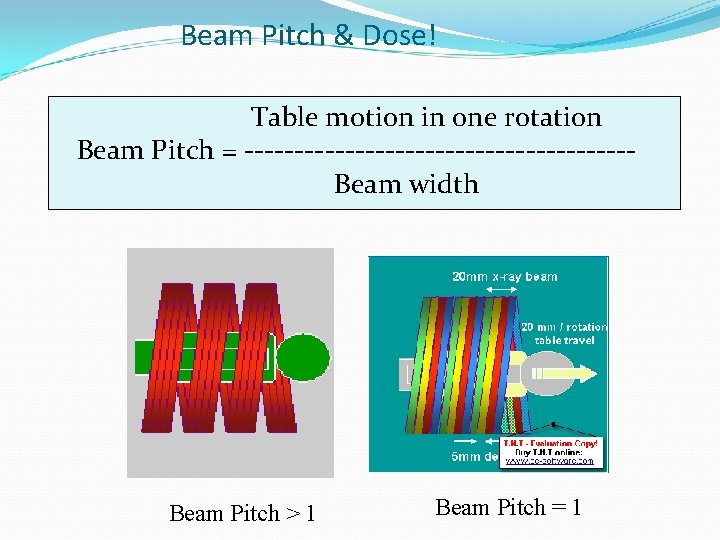
Beam Pitch & Dose! Table motion in one rotation Beam Pitch = -------------------Beam width Beam Pitch > 1 Beam Pitch = 1
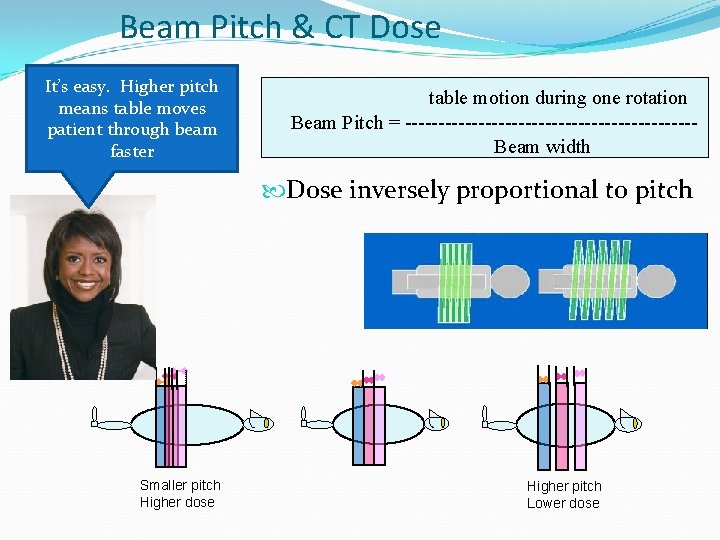
Beam Pitch & CT Dose It’s easy. Higher pitch means table moves patient through beam faster table motion during one rotation Beam Pitch = ----------------------Beam width Dose inversely proportional to pitch Smaller pitch Higher dose Higher pitch Lower dose
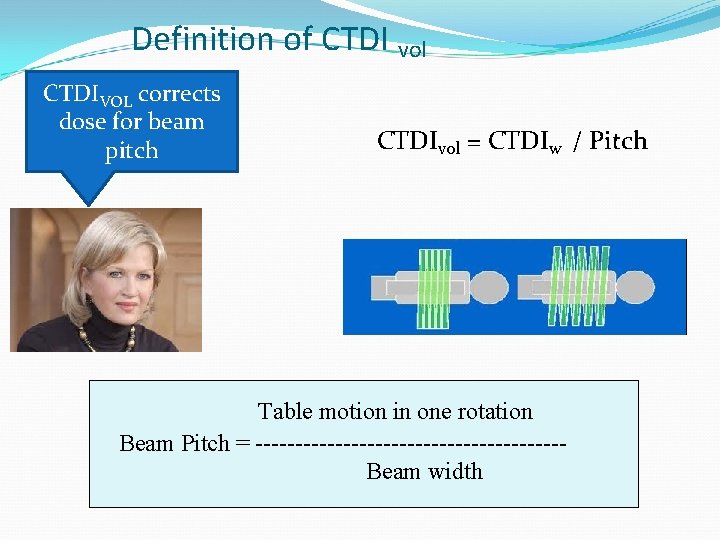
Definition of CTDI vol CTDIVOL corrects dose for beam pitch CTDIvol = CTDIw / Pitch Table motion in one rotation Beam Pitch = -------------------Beam width
Dose Length Product DLP = CTDIvol* length of scan DLP units m. Gy*cm Displayed on report page
Effective Dose Represents single dose to entire body that gives same cancer risk Allows comparison of different non-uniform exposures Units: Rem = 1 rad for x-rays Sievert = 1 Gray for x-rays
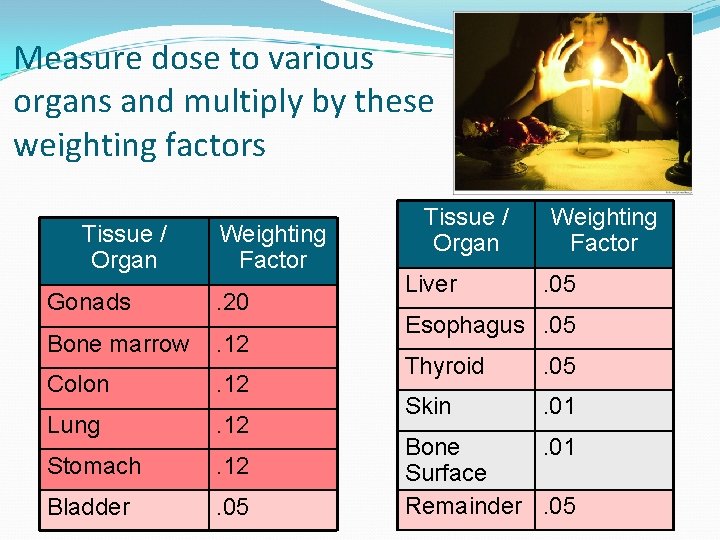
Measure dose to various organs and multiply by these weighting factors Tissue / Organ Weighting Factor Gonads . 20 Bone marrow . 12 Colon . 12 Lung . 12 Stomach . 12 Bladder . 05 Tissue / Organ Liver Weighting Factor. 05 Esophagus. 05 Thyroid . 05 Skin . 01 Bone. 01 Surface Remainder. 05
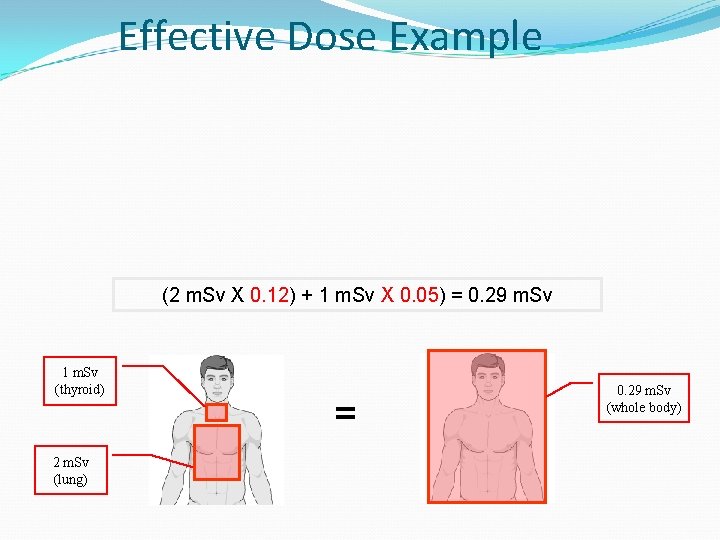
Effective Dose Example (2 m. Sv X 0. 12) + 1 m. Sv X 0. 05) = 0. 29 m. Sv 1 m. Sv (thyroid) 2 m. Sv (lung) = 0. 29 m. Sv (whole body)
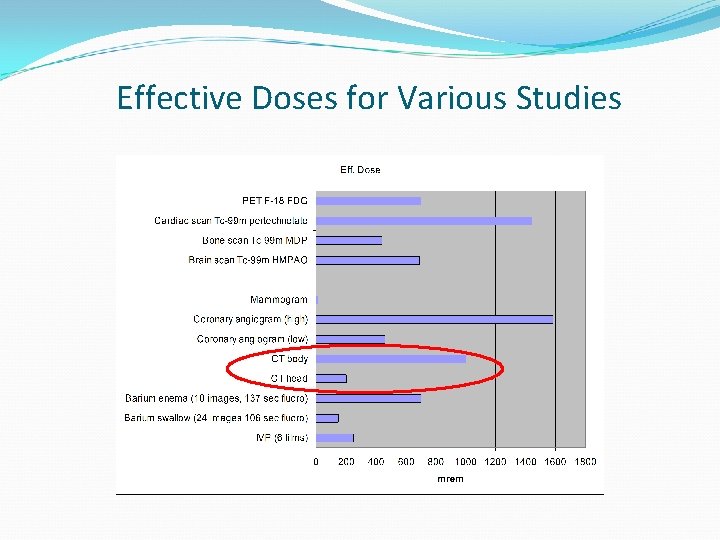
Effective Doses for Various Studies
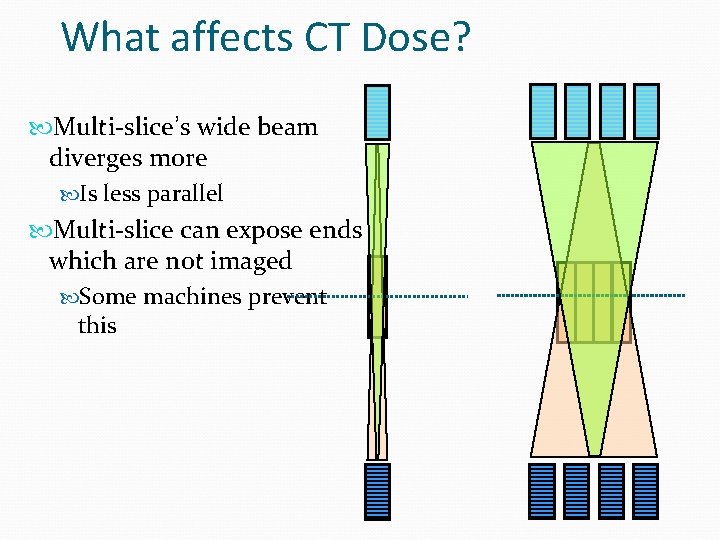
What affects CT Dose? Multi-slice’s wide beam diverges more Is less parallel Multi-slice can expose ends which are not imaged Some machines prevent this
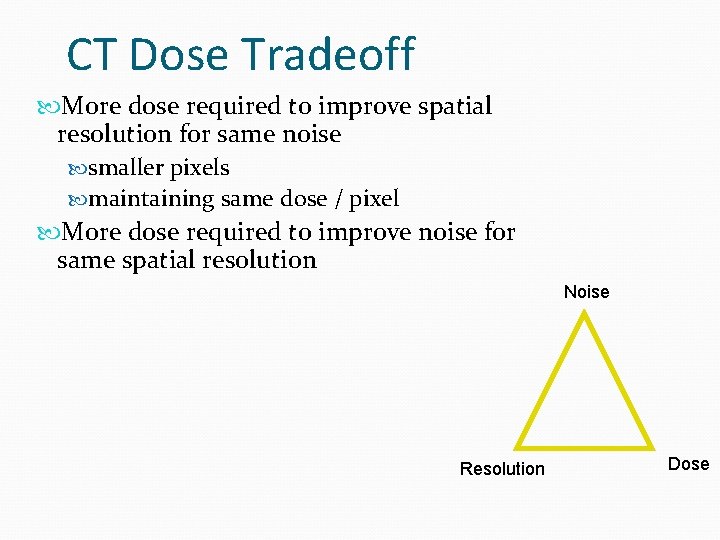
CT Dose Tradeoff More dose required to improve spatial resolution for same noise smaller pixels maintaining same dose / pixel More dose required to improve noise for same spatial resolution Noise Resolution Dose
CT Dose Reduction Reduce m. As Increases image noise Noise inversely proportional to square root of dose Proper technique: maximum tolerable noise as determined by radiologist
CT Noise Reduction Increase pixel size BUT Larger pixels obscure visualization of small objects poorer spatial resolution
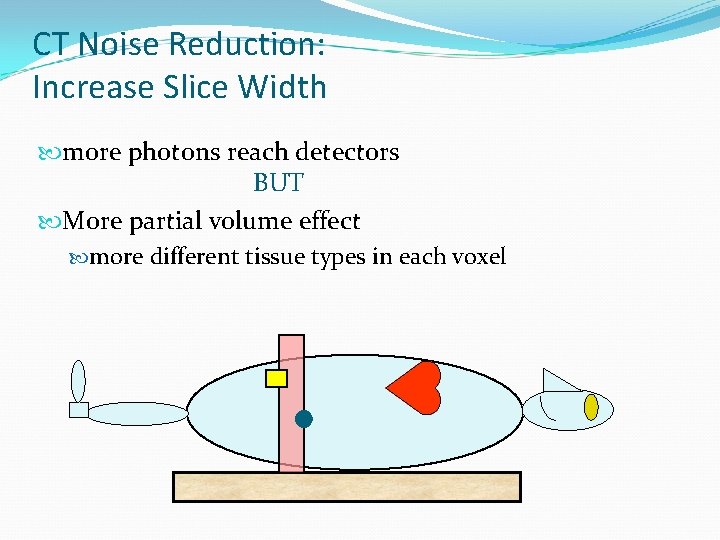
CT Noise Reduction: Increase Slice Width more photons reach detectors BUT More partial volume effect more different tissue types in each voxel
CT Noise Reduction Increase overall detector efficiency More photons detected for same technique
CT Phototiming Allow operator to specify image quality GE nomenclature: “Noise Index” Index Modulate m. A as tube rotates around patient Patient moves through gantry Goal: keep photon flux to detector constant during study
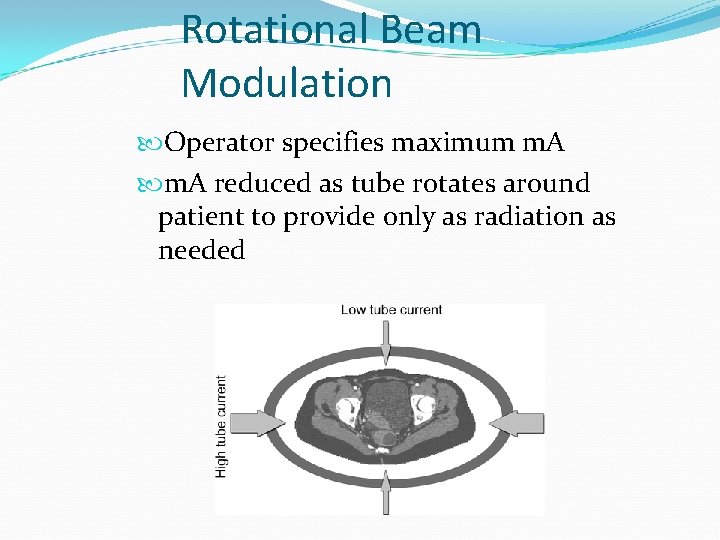
Rotational Beam Modulation Operator specifies maximum m. A reduced as tube rotates around patient to provide only as radiation as needed
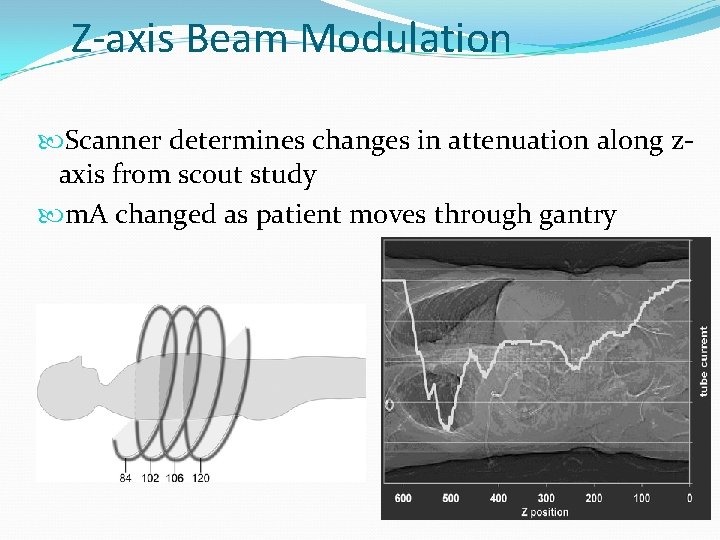
Z-axis Beam Modulation Scanner determines changes in attenuation along zaxis from scout study m. A changed as patient moves through gantry
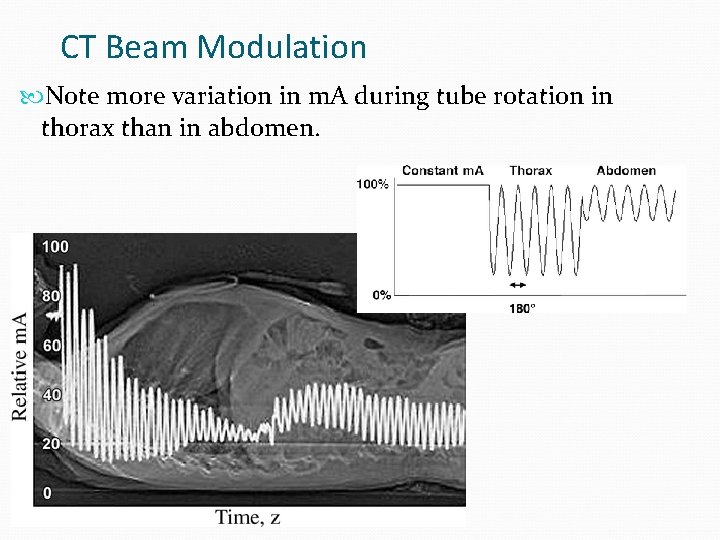
CT Beam Modulation Note more variation in m. A during tube rotation in thorax than in abdomen.
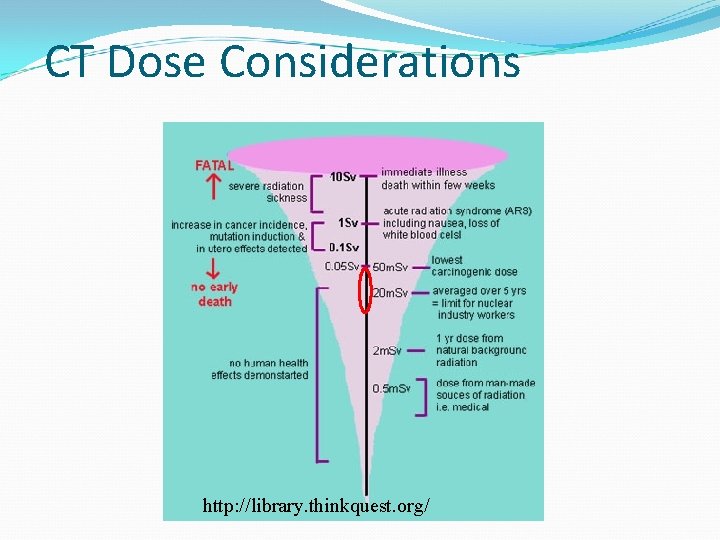
CT Dose Considerations http: //library. thinkquest. org/
NCRP Reports Ionizing Radiation Exposure of the Population of the United States # 93 Published in 1987 Data from early 1980’s Extensive data on medical exposures # 160 Re-write in 2008 National Council on Radiation Protection and Measurements
CT Usage Annual growth U. S. Population: <1% CT Procedures: >10% ~ 67, 000 procedures in 2006 about 10% pediatric CT Computed Tomography — An Increasing Source of Radiation Exposure David J. Brenner, Ph. D. , D. Sc. , and Eric J. Hall, D. Phil. , D. Sc. New England Journal of Medicine, 2007
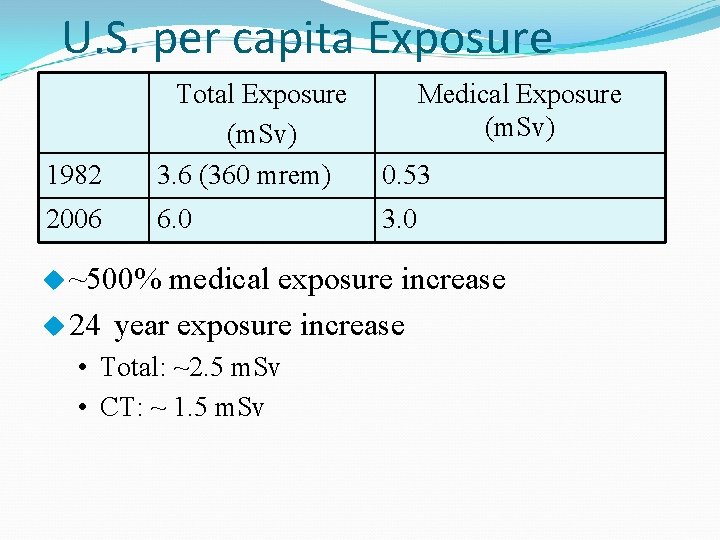
U. S. per capita Exposure 1982 Total Exposure (m. Sv) 3. 6 (360 mrem) 0. 53 2006 6. 0 3. 0 u ~500% Medical Exposure (m. Sv) medical exposure increase u 24 year exposure increase • Total: ~2. 5 m. Sv • CT: ~ 1. 5 m. Sv
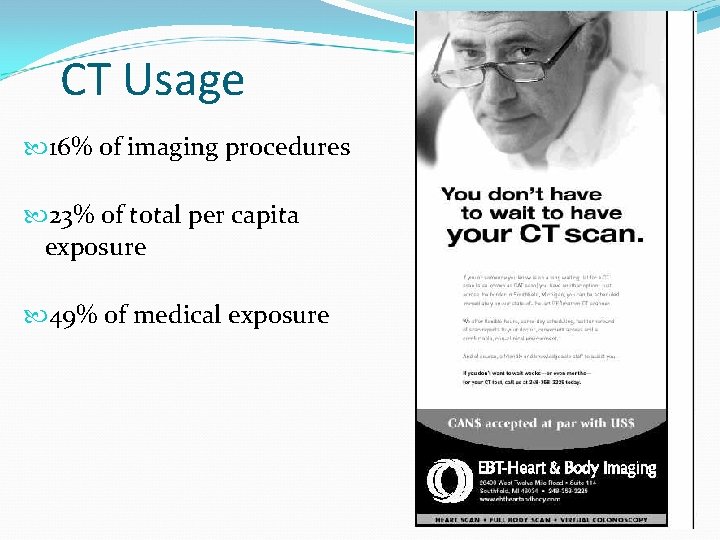
CT Usage 16% of imaging procedures 23% of total per capita exposure 49% of medical exposure
Multi-slice CT Doses Other considerations Tendency to cover more volume (anatomy) Better availability of equipment
Other Reasons for High CT Doses Repeat Exams No adjustment of technique factors for different size patients No adjustment for different areas of body
CT Usage “On the basis of …data on CT use from 1991 through 1996, it has been estimated that about 0. 4% of all cancers in the United States may be attributable to the radiation from CT studies…By adjusting this estimate for current CT use this estimate might now be in the range of 1. 5 to 2. 0%. ” Computed Tomography — An Increasing Source of Radiation Exposure David J. Brenner, Ph. D. , D. Sc. , and Eric J. Hall, D. Phil. , D. Sc. New England Journal of Medicine, 2007
CT Dose Risk Natural incidence of cancer: 1 in 5 Increase in risk from typical CT study << natural incidence This is public health concern because of large increase in volume for CT. FDA Website: http: //www. fda. gov/Radiation. Emitting. Productsand. Procedures/Medi cal. Imaging/Medical. X-Rays/ucm 115329. htm
Dose reduction mechanisms Customize settings to patient size m. A k. Vp Reduce z-axis coverage Reduce field of view Consider alternate procedures http: //www. acr. org/Secondary. Main. Menu. Categories/quality_safety/app_criteria. aspx
Big Brother California SB 1237 would require hospitals & clinics to record CT doses Accreditation Reporting of “overdosing”
Concerns Siemens automatically increases m. A when pitch is increased GE protocols can be Changed Over-written CTDI (dose index) Radiation measured in phantom Useful in comparing units Of limited use in calculating accurate dose to specific patient
Concerns CT dose report often not convenient to view No dose database on CT scanners Review of dose information in DICOM headers is cumbersome manual process
- Slides: 44