Doing more with less New Zealands response to









- Slides: 25
Doing more with less: New Zealand’s response to the health care sustainability challenge Toni Ashton Professor in health economics School of Population Health, University of Auckland School of Population Health
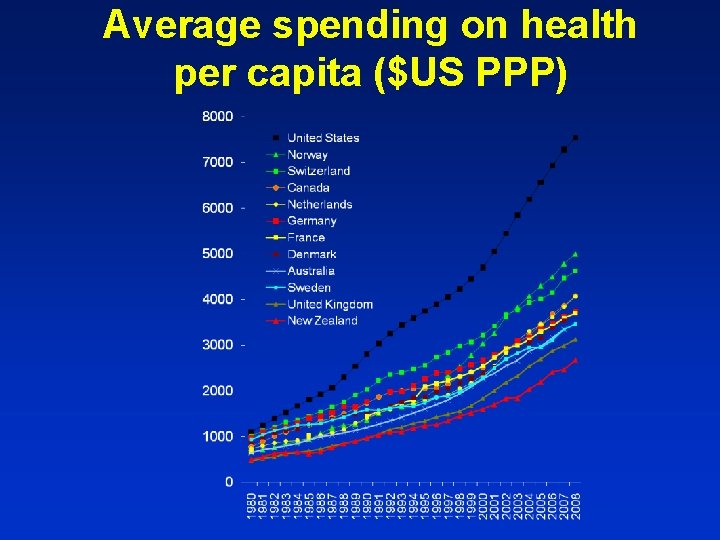
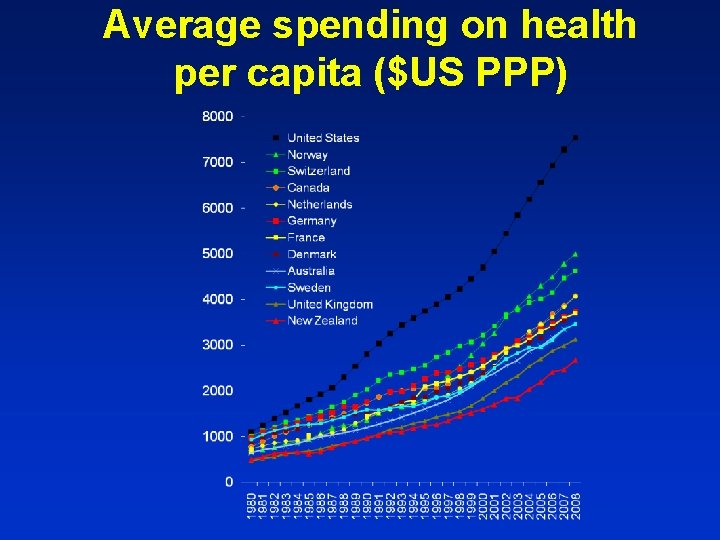
Average spending on health per capita ($US PPP)
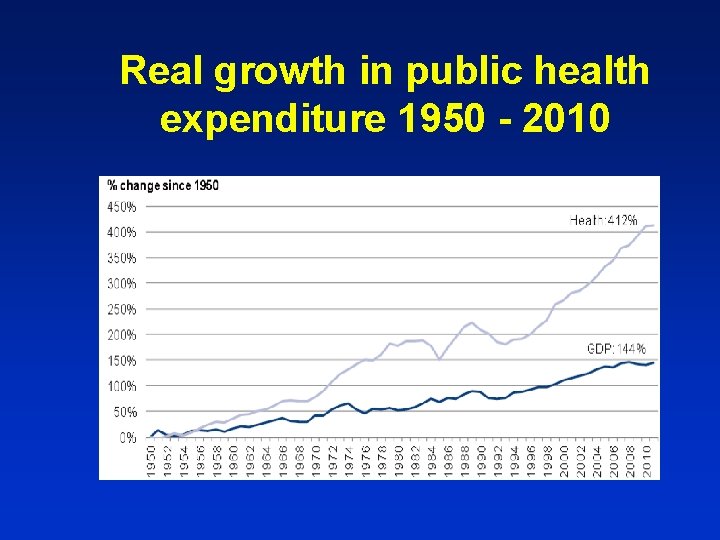
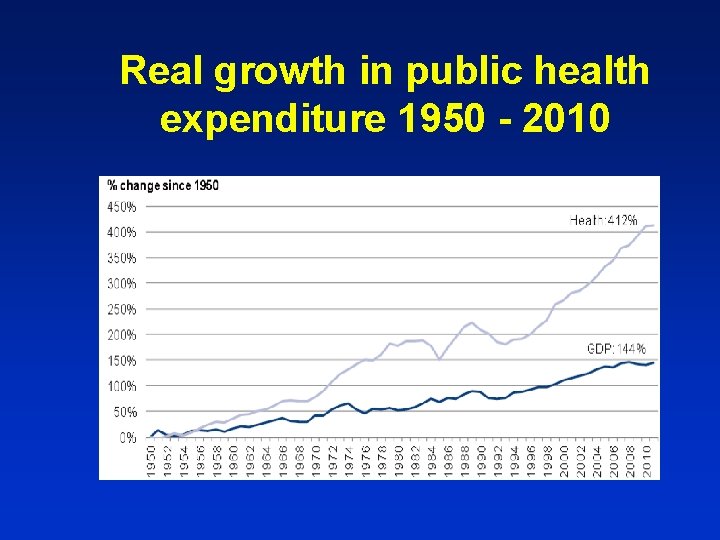
Real growth in public health expenditure 1950 - 2010
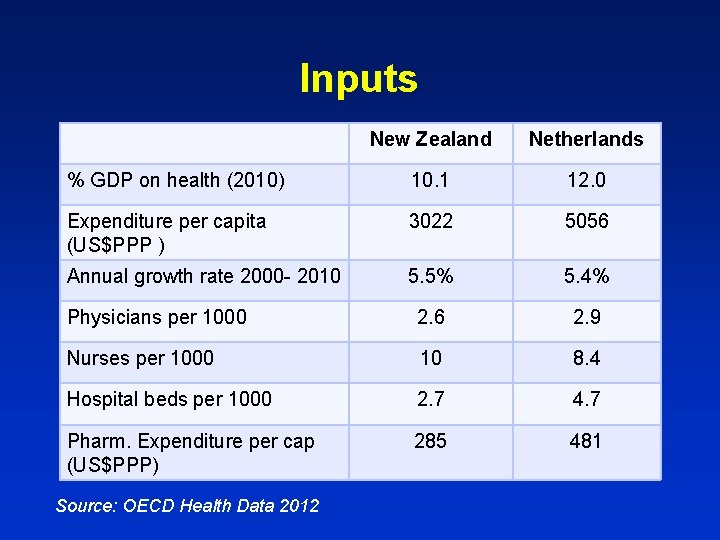
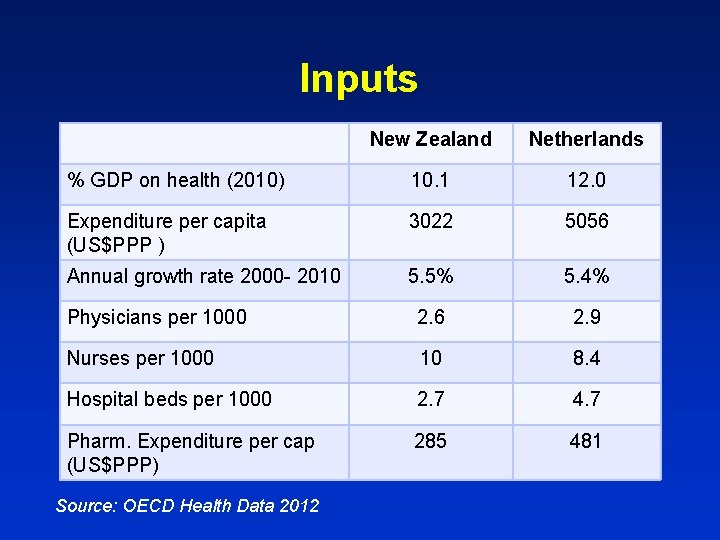
Inputs New Zealand Netherlands % GDP on health (2010) 10. 1 12. 0 Expenditure per capita (US$PPP ) 3022 5056 Annual growth rate 2000 - 2010 5. 5% 5. 4% Physicians per 1000 2. 6 2. 9 Nurses per 1000 10 8. 4 Hospital beds per 1000 2. 7 4. 7 Pharm. Expenditure per cap (US$PPP) 285 481 Source: OECD Health Data 2012
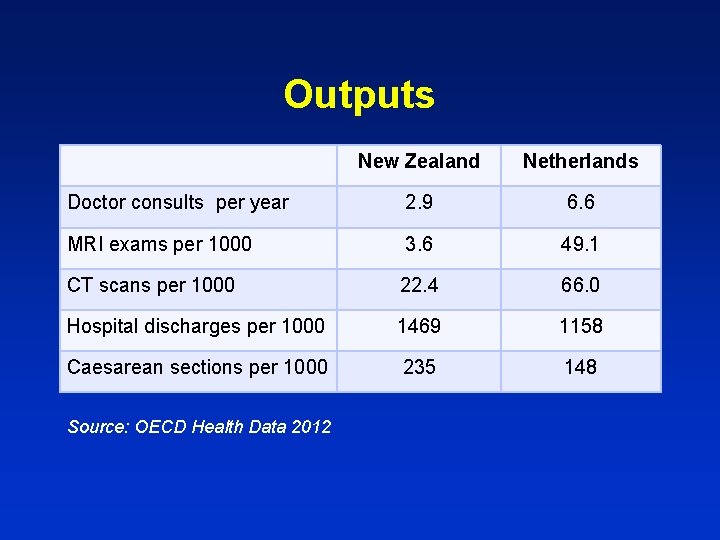
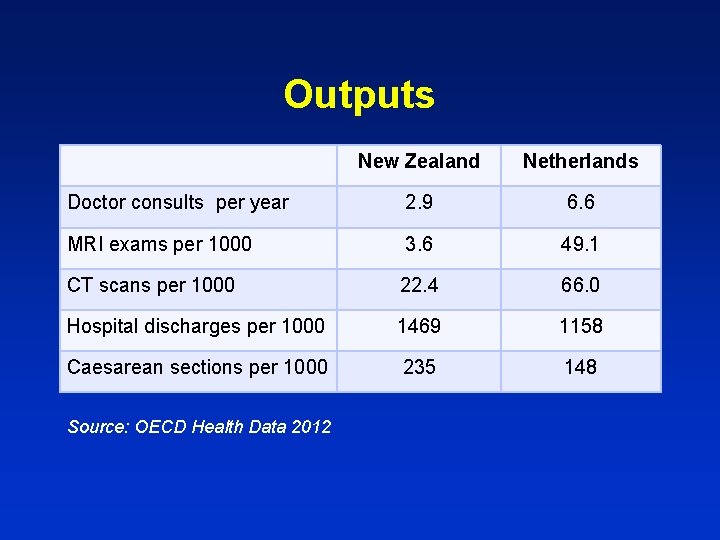
Outputs New Zealand Netherlands Doctor consults per year 2. 9 6. 6 MRI exams per 1000 3. 6 49. 1 CT scans per 1000 22. 4 66. 0 Hospital discharges per 1000 1469 1158 Caesarean sections per 1000 235 148 Source: OECD Health Data 2012
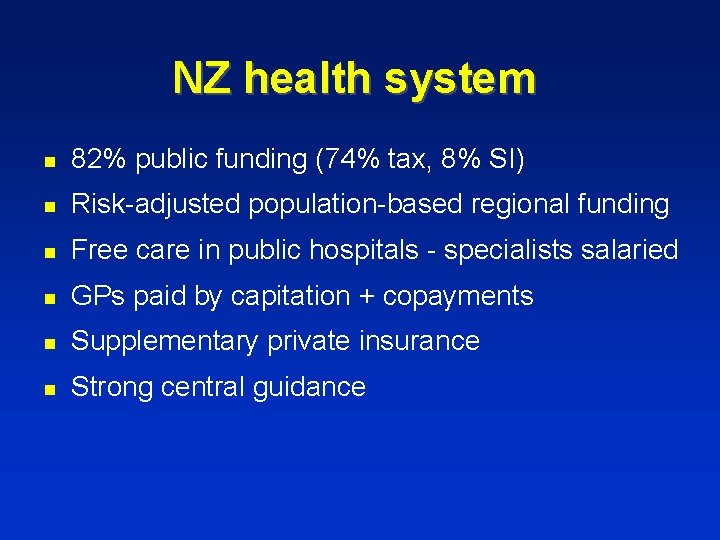
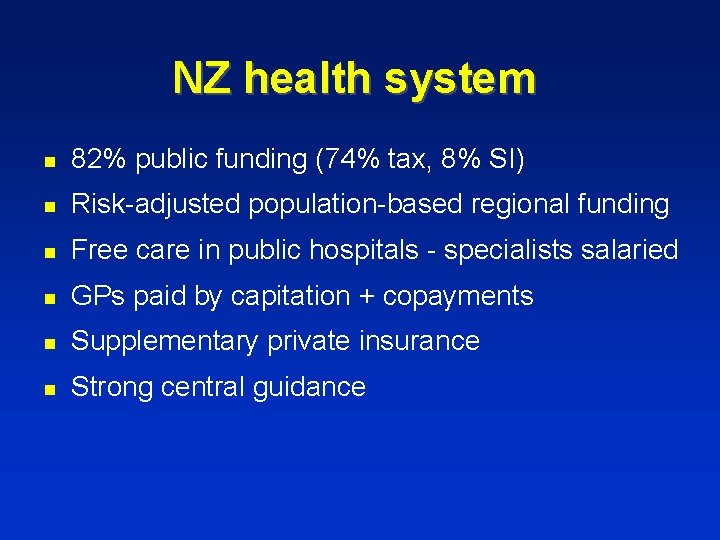
NZ health system n 82% public funding (74% tax, 8% SI) n Risk-adjusted population-based regional funding n Free care in public hospitals - specialists salaried n GPs paid by capitation + copayments n Supplementary private insurance n Strong central guidance
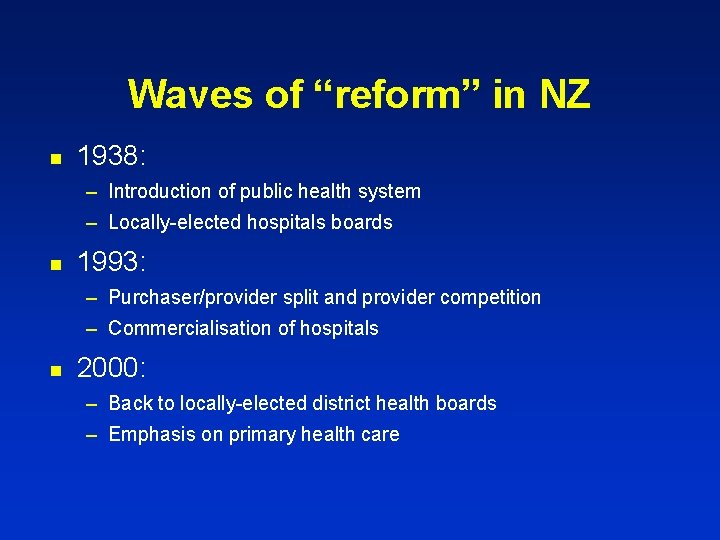
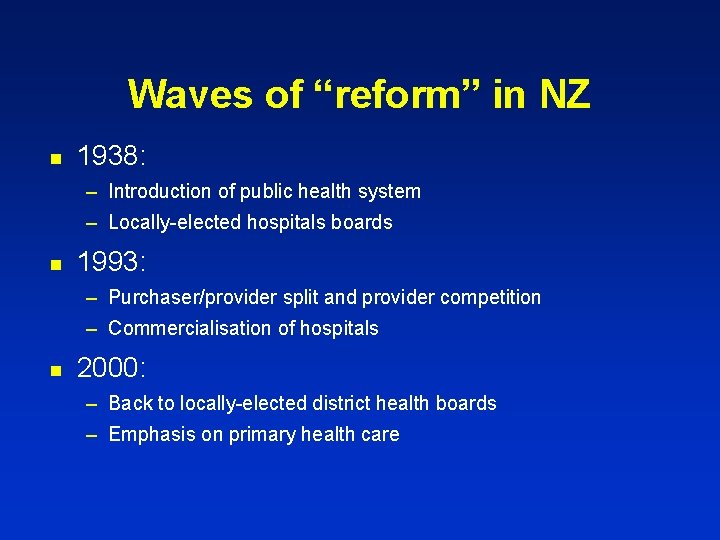
Waves of “reform” in NZ n 1938: – Introduction of public health system – Locally-elected hospitals boards n 1993: – Purchaser/provider split and provider competition – Commercialisation of hospitals n 2000: – Back to locally-elected district health boards – Emphasis on primary health care
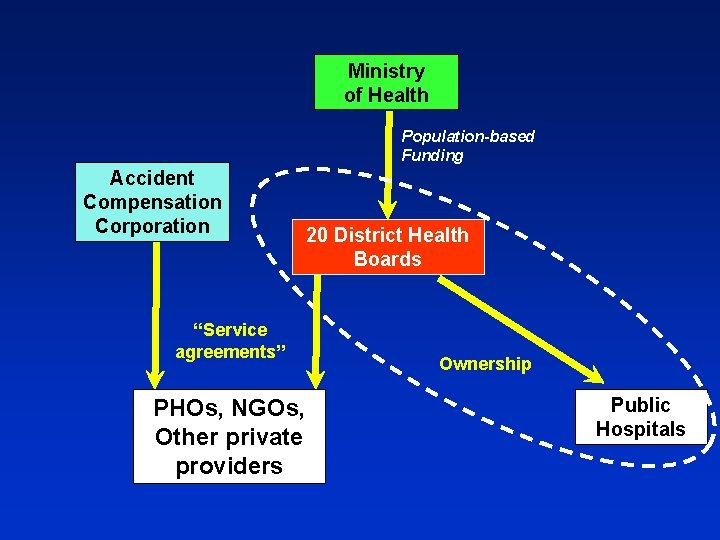
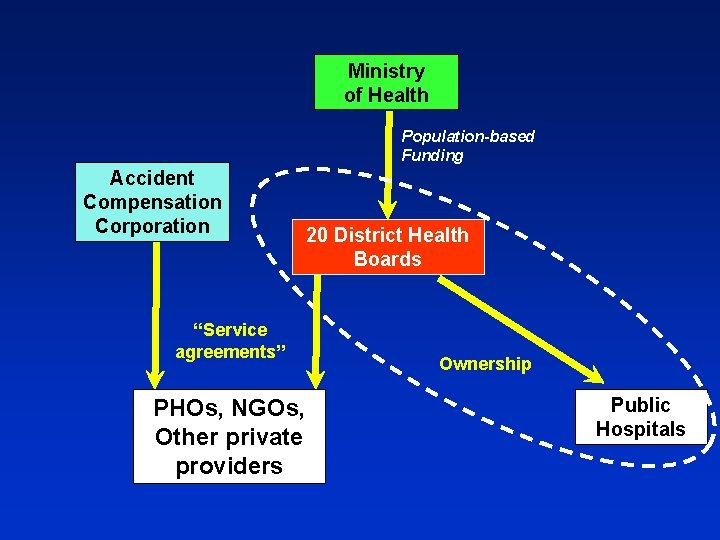
Ministry of Health Population-based Funding Accident Compensation Corporation “Service agreements” PHOs, NGOs, Other private providers 20 District Health Boards Ownership Public Hospitals

Budget May 16 2013 “While many developed countries are freezing or reducing health funding, this government is committed to protecting and growing our public health services. . ” NZ$1. 6 billion extra over next 4 years
“We need to see further improvement in efficiency gains and containing costs. . . We must do more with less”
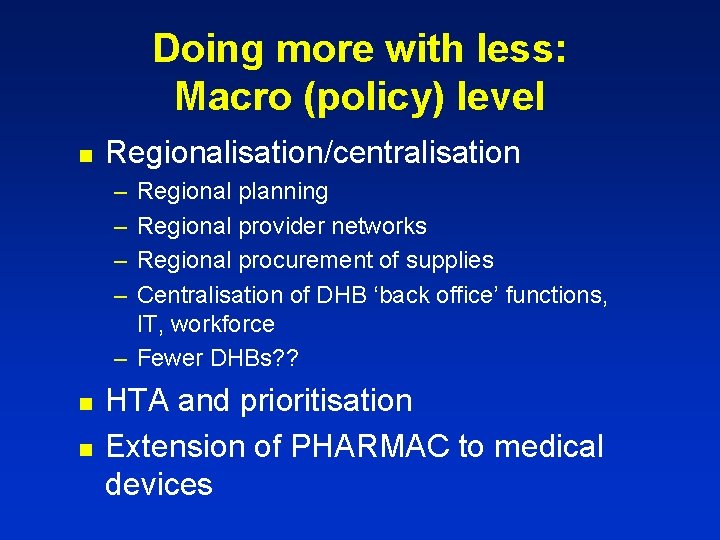
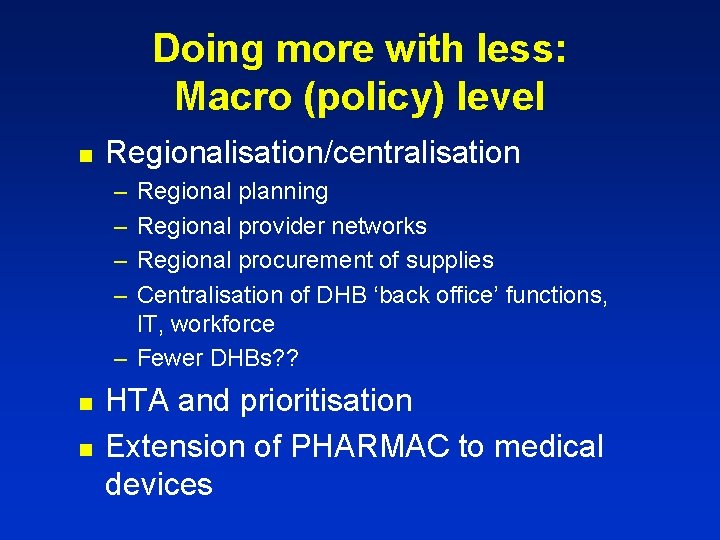
Doing more with less: Macro (policy) level n Regionalisation/centralisation – – Regional planning Regional provider networks Regional procurement of supplies Centralisation of DHB ‘back office’ functions, IT, workforce – Fewer DHBs? ? n n HTA and prioritisation Extension of PHARMAC to medical devices


Impact of PHARMAC on drug expenditure

Meso (organisational) level Concentration of specialised hospital services n Shift of care from hospitals into the community n Improved integration of services n
Integrated Family Health Centres: The vision Co-location of a wide range of services provided by multi-disciplinary teams – – – – Minor surgery Walk-in clinic Nurse-led clinics for chronic care Full diagnostics Specialist assessments Allied health services Some social care

Integrated Family Health Centres: The practice Development patchy – and slow n Lack of start-up capital n Collaboration more important than co-location n

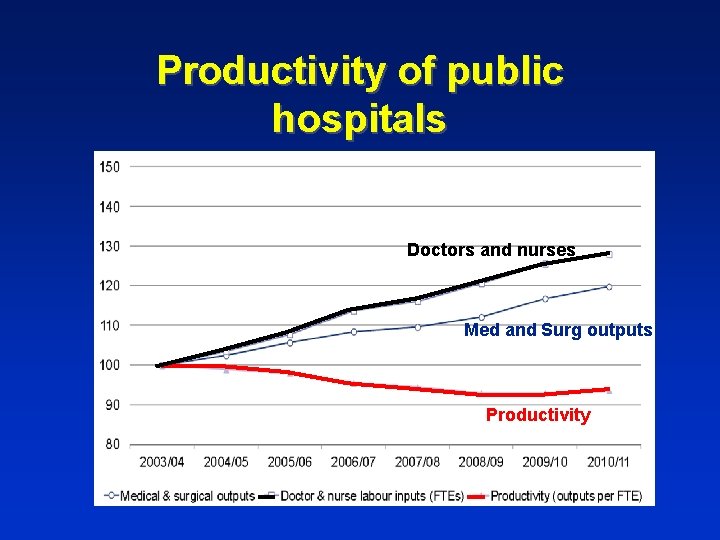
Meso (organisational) level Concentration of specialised hospital services n Shift of care from hospitals into the community n Improved integration of services n Productivity of hospital wards n
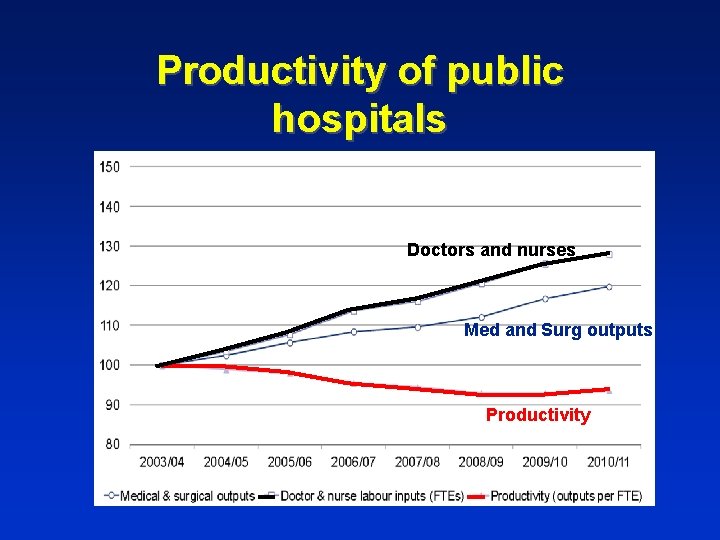
Productivity of public hospitals Doctors and nurses Med and Surg outputs Productivity
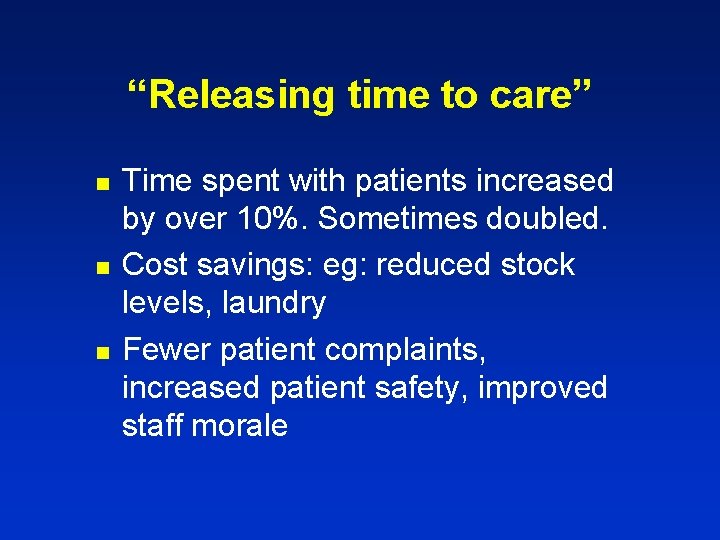
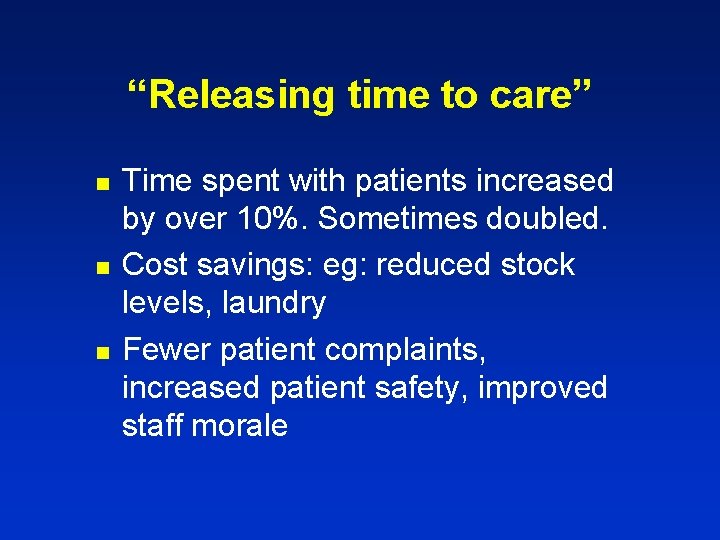
“Releasing time to care” n n n Time spent with patients increased by over 10%. Sometimes doubled. Cost savings: eg: reduced stock levels, laundry Fewer patient complaints, increased patient safety, improved staff morale

Meso (organisational) level Concentration of specialised hospital services n Shift of care from hospitals into the community n Improved integration of services n Productivity of hospital wards n Long term care n
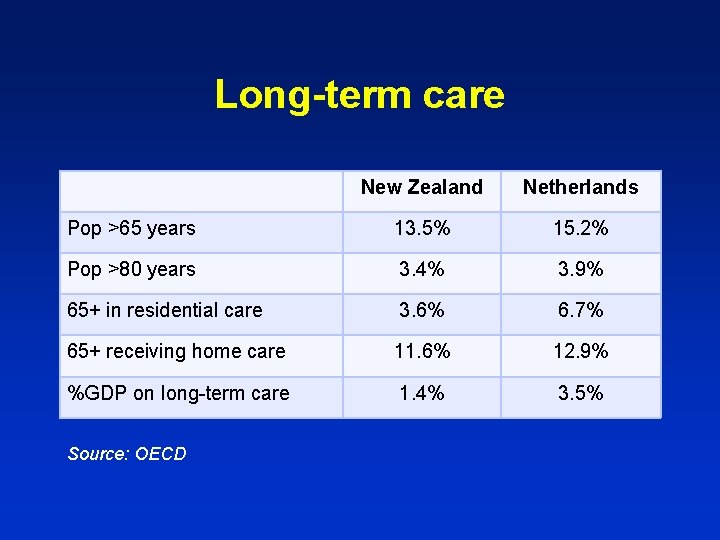
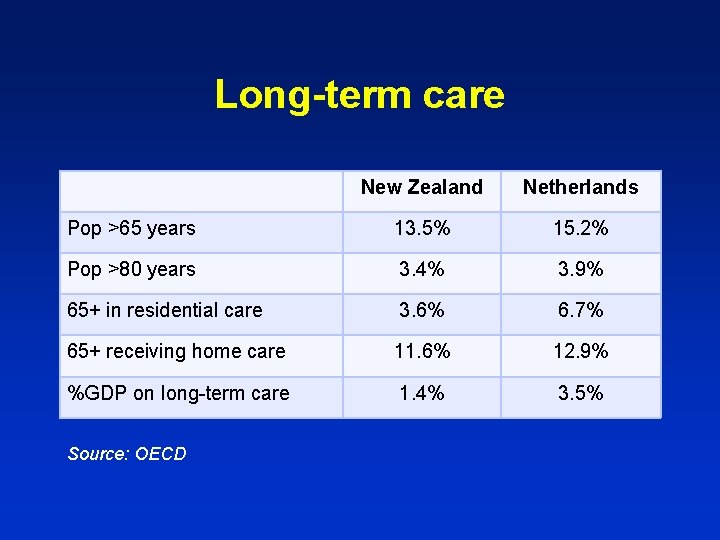
Long-term care New Zealand Netherlands Pop >65 years 13. 5% 15. 2% Pop >80 years 3. 4% 3. 9% 65+ in residential care 3. 6% 6. 7% 65+ receiving home care 11. 6% 12. 9% %GDP on long-term care 1. 4% 3. 5% Source: OECD
Long-term care “Aging in place” n Standardised needs-assessment n Assisted living arrangements? ? n Stricter income and asset testing? ? n Increase pre-funding? ? n – Compulsory insurance – Incentives for private saving

Micro-level (doctors and patients) n Task-shifting – Nurses, pharmacists, physician assistants Improve patient self-management n Prevention n – CVD and diabetes risk assessment – Immunisation – Smoking
What is NOT being discussed? Increasing copayments n Greater use of private insurance n Increasing competition and choice n Methods of reducing “unneccessary” care n

Dank u wel!
 More more more i want more more more more we praise you
More more more i want more more more more we praise you More more more i want more more more more we praise you
More more more i want more more more more we praise you New zealands tests positive
New zealands tests positive Less religious and less idealized than greek art
Less religious and less idealized than greek art Anything worth doing is not necessarily worth doing well
Anything worth doing is not necessarily worth doing well By doing nothing we learn to be ill
By doing nothing we learn to be ill Characteristics of the articles of confederation
Characteristics of the articles of confederation Neil thisse is a loyalist who fled the colonies
Neil thisse is a loyalist who fled the colonies Tweet less kiss more
Tweet less kiss more Le corbusier less is more
Le corbusier less is more Coco chanel less is more
Coco chanel less is more Propositional and expressive meaning
Propositional and expressive meaning More of this less of that
More of this less of that Regularly meaning
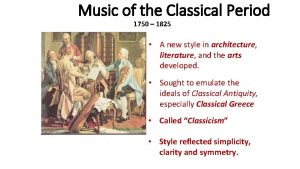
Regularly meaning The classical period started from 1750 to 1872
The classical period started from 1750 to 1872 What is the tone of “she walks in beauty”?
What is the tone of “she walks in beauty”? How to round decimals to the nearest hundredth
How to round decimals to the nearest hundredth Chapter 67 neo romantic evocations
Chapter 67 neo romantic evocations How youre
How youre “the more you save, the less you spend” describes
“the more you save, the less you spend” describes Explore more worry less
Explore more worry less Write less do more
Write less do more He must become greater; i must become less
He must become greater; i must become less Half life more than 2 less than 4
Half life more than 2 less than 4 Axe less is more
Axe less is more New ways of doing business
New ways of doing business