Does the Rate of Primary Series Vaccination Differ
- Slides: 1
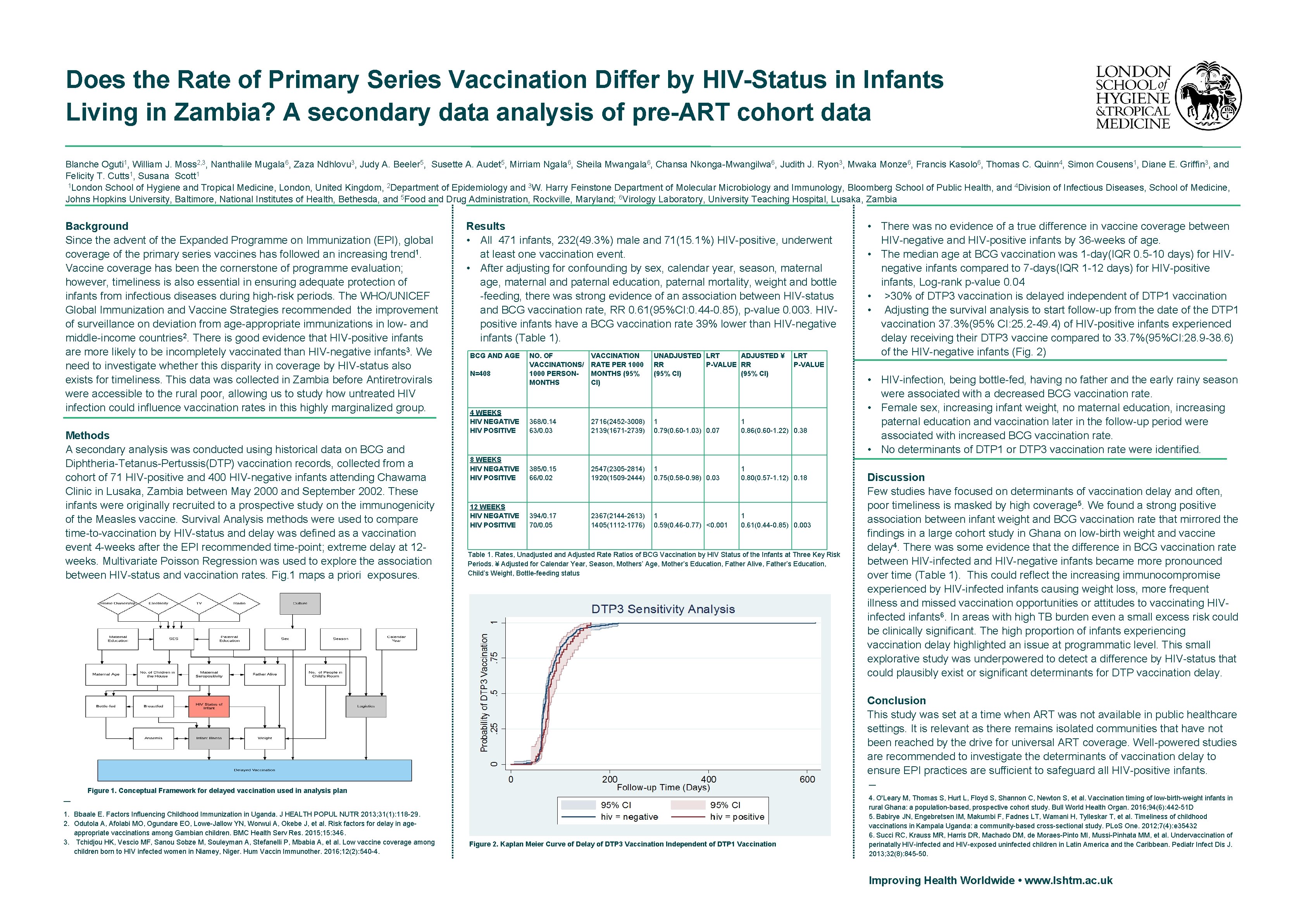
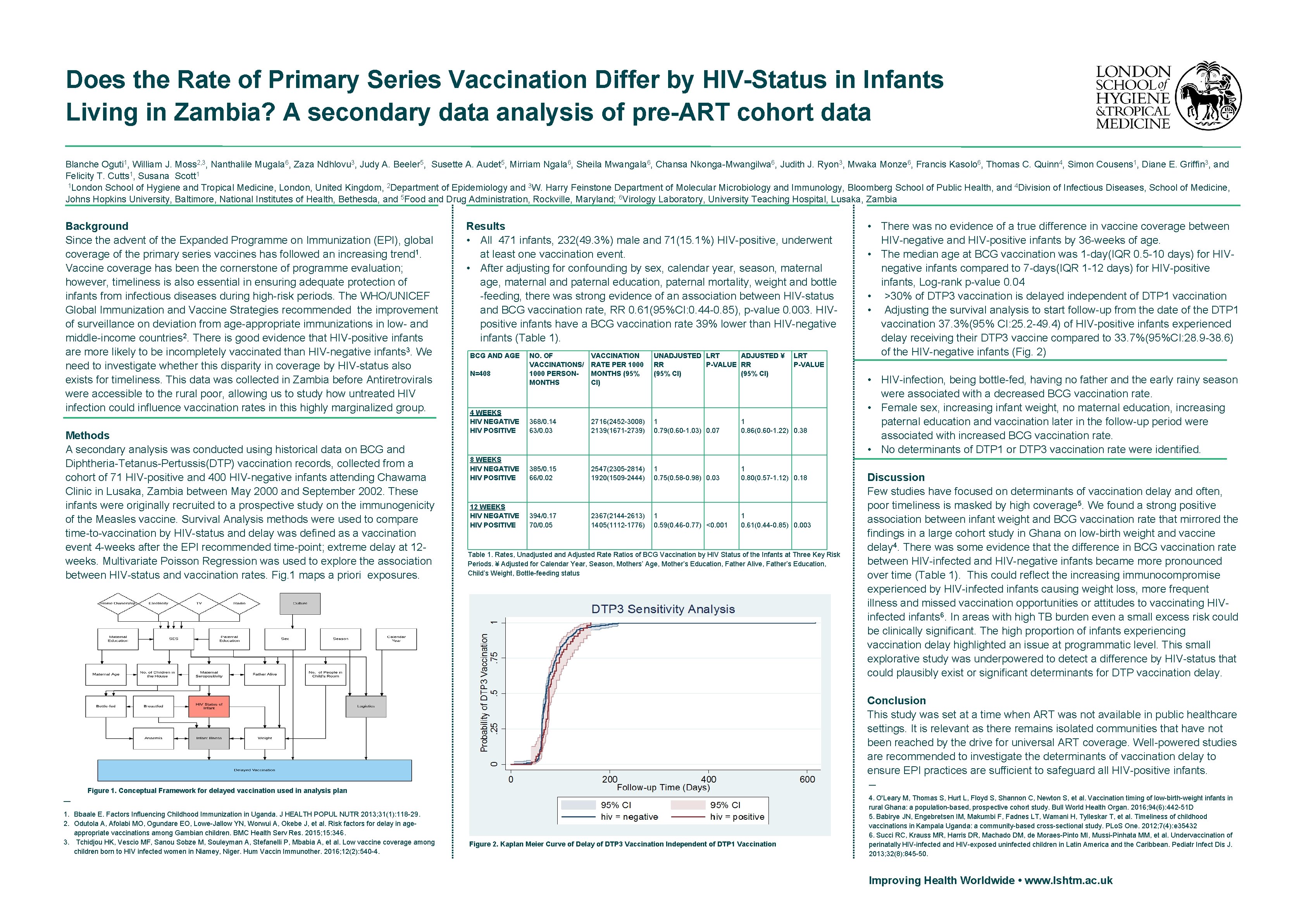
Does the Rate of Primary Series Vaccination Differ by HIV-Status in Infants Living in Zambia? A secondary data analysis of pre-ART cohort data Blanche Oguti 1, William J. Moss 2, 3, Nanthalile Mugala 6, Zaza Ndhlovu 3, Judy A. Beeler 5, Susette A. Audet 5, Mirriam Ngala 6, Sheila Mwangala 6, Chansa Nkonga-Mwangilwa 6, Judith J. Ryon 3, Mwaka Monze 6, Francis Kasolo 6, Thomas C. Quinn 4, Simon Cousens 1, Diane E. Griffin 3, and Felicity T. Cutts 1, Susana Scott 1 1 London School of Hygiene and Tropical Medicine, London, United Kingdom, 2 Department of Epidemiology and 3 W. Harry Feinstone Department of Molecular Microbiology and Immunology, Bloomberg School of Public Health, and 4 Division of Infectious Diseases, School of Medicine, Johns Hopkins University, Baltimore, National Institutes of Health, Bethesda, and 5 Food and Drug Administration, Rockville, Maryland; 6 Virology Laboratory, University Teaching Hospital, Lusaka, Zambia Background Since the advent of the Expanded Programme on Immunization (EPI), global coverage of the primary series vaccines has followed an increasing trend 1. Vaccine coverage has been the cornerstone of programme evaluation; however, timeliness is also essential in ensuring adequate protection of infants from infectious diseases during high-risk periods. The WHO/UNICEF Global Immunization and Vaccine Strategies recommended the improvement of surveillance on deviation from age-appropriate immunizations in low- and middle-income countries 2. There is good evidence that HIV-positive infants are more likely to be incompletely vaccinated than HIV-negative infants 3. We need to investigate whether this disparity in coverage by HIV-status also exists for timeliness. This data was collected in Zambia before Antiretrovirals were accessible to the rural poor, allowing us to study how untreated HIV infection could influence vaccination rates in this highly marginalized group. Methods A secondary analysis was conducted using historical data on BCG and Diphtheria-Tetanus-Pertussis(DTP) vaccination records, collected from a cohort of 71 HIV-positive and 400 HIV-negative infants attending Chawama Clinic in Lusaka, Zambia between May 2000 and September 2002. These infants were originally recruited to a prospective study on the immunogenicity of the Measles vaccine. Survival Analysis methods were used to compare time-to-vaccination by HIV-status and delay was defined as a vaccination event 4 -weeks after the EPI recommended time-point; extreme delay at 12 weeks. Multivariate Poisson Regression was used to explore the association between HIV-status and vaccination rates. Fig. 1 maps a priori exposures. Results • All 471 infants, 232(49. 3%) male and 71(15. 1%) HIV-positive, underwent at least one vaccination event. • After adjusting for confounding by sex, calendar year, season, maternal age, maternal and paternal education, paternal mortality, weight and bottle -feeding, there was strong evidence of an association between HIV-status and BCG vaccination rate, RR 0. 61(95%CI: 0. 44 -0. 85), p-value 0. 003. HIVpositive infants have a BCG vaccination rate 39% lower than HIV-negative infants (Table 1). BCG AND AGE NO. OF VACCINATIONS/ 1000 PERSONMONTHS VACCINATION RATE PER 1000 MONTHS (95% CI) UNADJUSTED LRT ADJUSTED ¥ RR P-VALUE RR (95% CI) 4 WEEKS HIV NEGATIVE HIV POSITIVE 368/0. 14 63/0. 03 2716(2452 -3008) 2139(1671 -2739) 1 0. 79(0. 60 -1. 03) 0. 07 1 0. 86(0. 60 -1. 22) 0. 38 8 WEEKS HIV NEGATIVE HIV POSITIVE 385/0. 15 66/0. 02 2547(2305 -2814) 1920(1509 -2444) 1 0. 75(0. 58 -0. 98) 0. 03 1 0. 80(0. 57 -1. 12) 0. 18 12 WEEKS HIV NEGATIVE HIV POSITIVE 394/0. 17 70/0. 05 2367(2144 -2613) 1405(1112 -1776) 1 0. 59(0. 46 -0. 77) <0. 001 1 0. 61(0. 44 -0. 85) 0. 003 N=408 LRT P-VALUE Table 1. Rates, Unadjusted and Adjusted Rate Ratios of BCG Vaccination by HIV Status of the Infants at Three Key Risk Periods. ¥ Adjusted for Calendar Year, Season, Mothers’ Age, Mother’s Education, Father Alive, Father’s Education, Child’s Weight, Bottle-feeding status • There was no evidence of a true difference in vaccine coverage between HIV-negative and HIV-positive infants by 36 -weeks of age. • The median age at BCG vaccination was 1 -day(IQR 0. 5 -10 days) for HIVnegative infants compared to 7 -days(IQR 1 -12 days) for HIV-positive infants, Log-rank p-value 0. 04 • >30% of DTP 3 vaccination is delayed independent of DTP 1 vaccination • Adjusting the survival analysis to start follow-up from the date of the DTP 1 vaccination 37. 3%(95% CI: 25. 2 -49. 4) of HIV-positive infants experienced delay receiving their DTP 3 vaccine compared to 33. 7%(95%CI: 28. 9 -38. 6) of the HIV-negative infants (Fig. 2) • HIV-infection, being bottle-fed, having no father and the early rainy season were associated with a decreased BCG vaccination rate. • Female sex, increasing infant weight, no maternal education, increasing paternal education and vaccination later in the follow-up period were associated with increased BCG vaccination rate. • No determinants of DTP 1 or DTP 3 vaccination rate were identified. Discussion Few studies have focused on determinants of vaccination delay and often, poor timeliness is masked by high coverage 5. We found a strong positive association between infant weight and BCG vaccination rate that mirrored the findings in a large cohort study in Ghana on low-birth weight and vaccine delay 4. There was some evidence that the difference in BCG vaccination rate between HIV-infected and HIV-negative infants became more pronounced over time (Table 1). This could reflect the increasing immunocompromise experienced by HIV-infected infants causing weight loss, more frequent illness and missed vaccination opportunities or attitudes to vaccinating HIVinfected infants 6. In areas with high TB burden even a small excess risk could be clinically significant. The high proportion of infants experiencing vaccination delay highlighted an issue at programmatic level. This small explorative study was underpowered to detect a difference by HIV-status that could plausibly exist or significant determinants for DTP vaccination delay. Conclusion This study was set at a time when ART was not available in public healthcare settings. It is relevant as there remains isolated communities that have not been reached by the drive for universal ART coverage. Well-powered studies are recommended to investigate the determinants of vaccination delay to ensure EPI practices are sufficient to safeguard all HIV-positive infants. — Figure 1. Conceptual Framework for delayed vaccination used in analysis plan — 1. Bbaale E. Factors Influencing Childhood Immunization in Uganda. J HEALTH POPUL NUTR 2013; 31(1): 118 -29. 2. Odutola A, Afolabi MO, Ogundare EO, Lowe-Jallow YN, Worwui A, Okebe J, et al. Risk factors for delay in ageappropriate vaccinations among Gambian children. BMC Health Serv Res. 2015; 15: 346. 3. Tchidjou HK, Vescio MF, Sanou Sobze M, Souleyman A, Stefanelli P, Mbabia A, et al. Low vaccine coverage among children born to HIV infected women in Niamey, Niger. Hum Vaccin Immunother. 2016; 12(2): 540 -4. Figure 2. Kaplan Meier Curve of Delay of DTP 3 Vaccination Independent of DTP 1 Vaccination 4. O'Leary M, Thomas S, Hurt L, Floyd S, Shannon C, Newton S, et al. Vaccination timing of low-birth-weight infants in rural Ghana: a population-based, prospective cohort study. Bull World Health Organ. 2016; 94(6): 442 -51 D 5. Babirye JN, Engebretsen IM, Makumbi F, Fadnes LT, Wamani H, Tylleskar T, et al. Timeliness of childhood vaccinations in Kampala Uganda: a community-based cross-sectional study. PLo. S One. 2012; 7(4): e 35432 6. Succi RC, Krauss MR, Harris DR, Machado DM, de Moraes-Pinto MI, Mussi-Pinhata MM, et al. Undervaccination of perinatally HIV-infected and HIV-exposed uninfected children in Latin America and the Caribbean. Pediatr Infect Dis J. 2013; 32(8): 845 -50. Improving Health Worldwide • www. lshtm. ac. uk