Documentation HPR 451 Where does documentation fit into
- Slides: 27
Documentation HPR 451
Where does documentation fit into the TR process? • • Assessment? Planning? ? Implementation? ? ? Evaluation? ? ? ? ? ? ? ? ? ? ?
Documentation – who needs it? • TR/RT – Basis for decisions, plan, results • TR/RT supervisor, manager – Evaluate TR/RT – Pass information to other TR/RT staff • Treatment team members – – Same as TR needs Avoid duplication Fill in gaps Changes, problems, etc.
Documentation – who needs it? • Insurers (include Medicare, Medicaid) – Need information to justify payment • Auditors, quality control personnel, accreditation agencies (JC, CARF) – What services are being provided – Services being provide appropriately • CEOs, Board of Directors, attorneys, etc. – Allegations of errors or omissions up to and including legal action
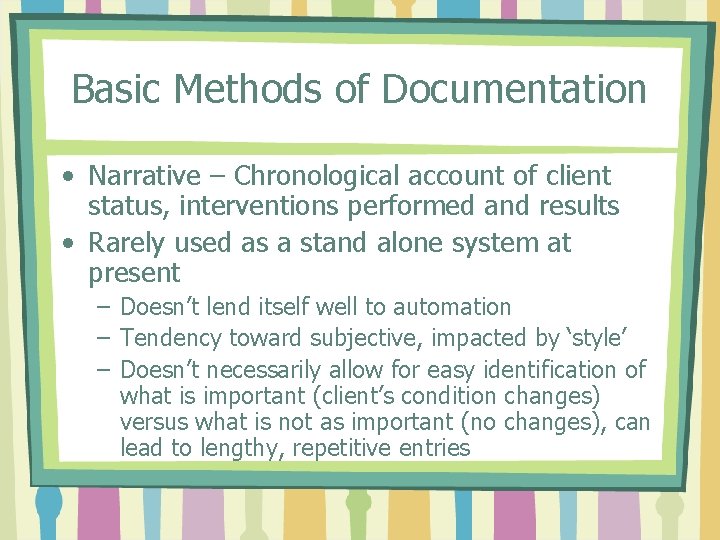
Basic Methods of Documentation • Narrative – Chronological account of client status, interventions performed and results • Rarely used as a stand alone system at present – Doesn’t lend itself well to automation – Tendency toward subjective, impacted by ‘style’ – Doesn’t necessarily allow for easy identification of what is important (client’s condition changes) versus what is not as important (no changes), can lead to lengthy, repetitive entries
Narrative Advantages • Flexible • Good for information gathered over a long period of time • May combine well some other methods (flow chart or graph for summary, narrative for detail) • Easy to train employees to use • Always in chronological order
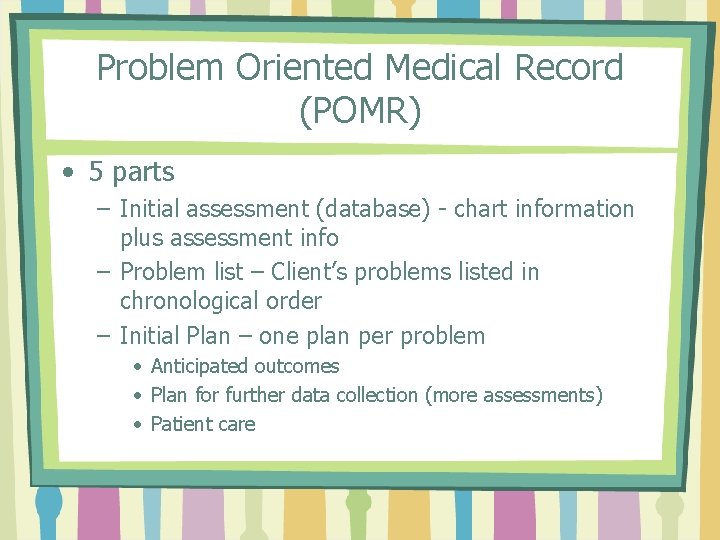
Problem Oriented Medical Record (POMR) • 5 parts – Initial assessment (database) - chart information plus assessment info – Problem list – Client’s problems listed in chronological order – Initial Plan – one plan per problem • Anticipated outcomes • Plan for further data collection (more assessments) • Patient care
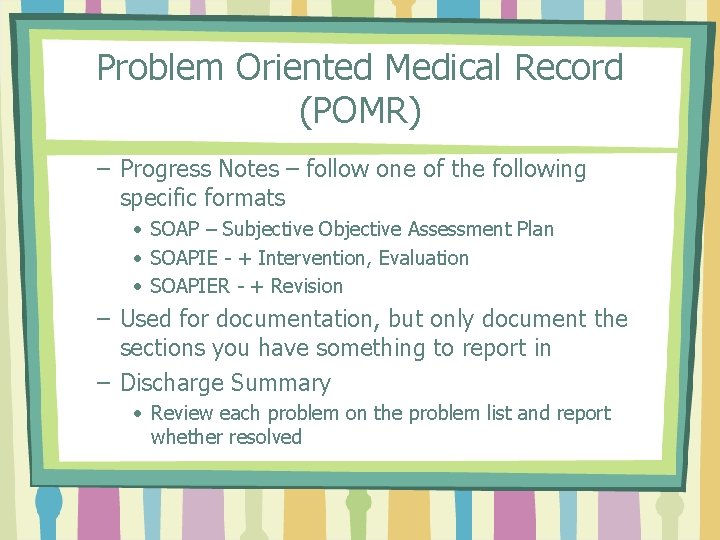
Problem Oriented Medical Record (POMR) – Progress Notes – follow one of the following specific formats • SOAP – Subjective Objective Assessment Plan • SOAPIE - + Intervention, Evaluation • SOAPIER - + Revision – Used for documentation, but only document the sections you have something to report in – Discharge Summary • Review each problem on the problem list and report whether resolved
Pluses of POMR • Standard organization • Shows care plan and delivery • Should emphasize charting only essential information • Provides an integrated medical record
Negatives of POMR • Chronology rather than priority • Possible duplication (assessments and interventions can apply to more than one problem) • Routine care may be undocumented • Does not work well in settings with high patient turnover • Training time for staff to use SOAP, etc. format
More on SOAP • S – Subjective – – What the client says (example? ) What the client thinks (example? ) How the client feels (example? ) What the client tells you about his or her illness, injury, disability, etc. (example? ) – What the client tells you about his/her medical or treatment history (example? ) – Same information from family members
More on SOAP • O – Objective – – – Everything observed or done by therapist Results of tests or assessments Vital signs Client’s demonstrated abilities or performance Medical chart information
More on SOAP • A – Assessment – Your conclusions based on S and O • P – Plan – – Immediate treatment Specific, measurable Expected outcomes In POMR, relates to one problem, concern, complaint
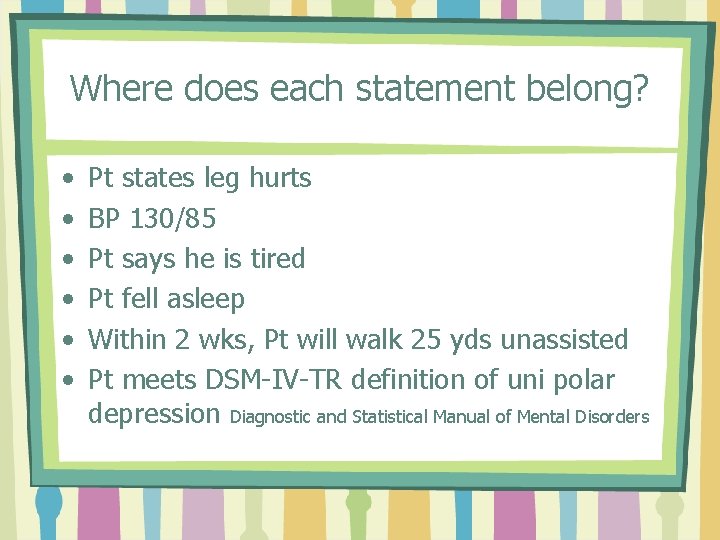
Where does each statement belong? • • • Pt states leg hurts BP 130/85 Pt says he is tired Pt fell asleep Within 2 wks, Pt will walk 25 yds unassisted Pt meets DSM-IV-TR definition of uni polar depression Diagnostic and Statistical Manual of Mental Disorders
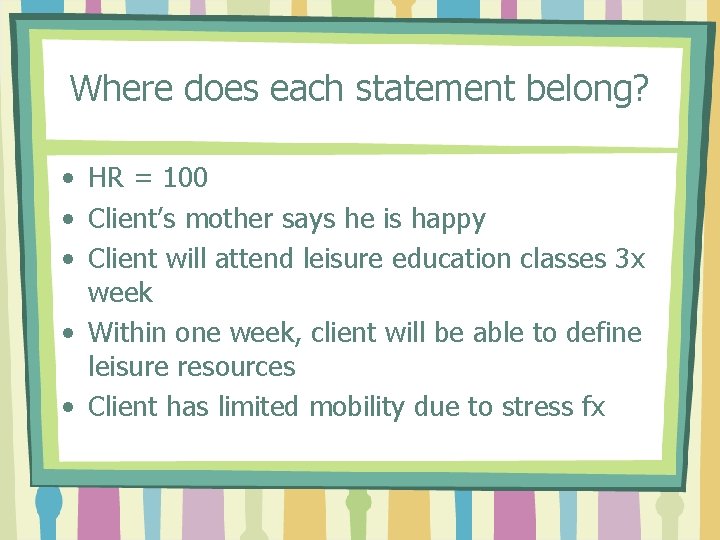
Where does each statement belong? • HR = 100 • Client’s mother says he is happy • Client will attend leisure education classes 3 x week • Within one week, client will be able to define leisure resources • Client has limited mobility due to stress fx
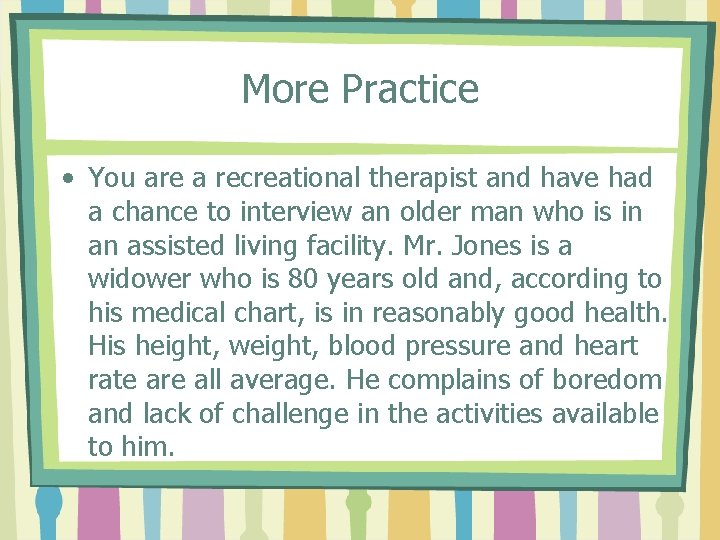
More Practice • You are a recreational therapist and have had a chance to interview an older man who is in an assisted living facility. Mr. Jones is a widower who is 80 years old and, according to his medical chart, is in reasonably good health. His height, weight, blood pressure and heart rate are all average. He complains of boredom and lack of challenge in the activities available to him.
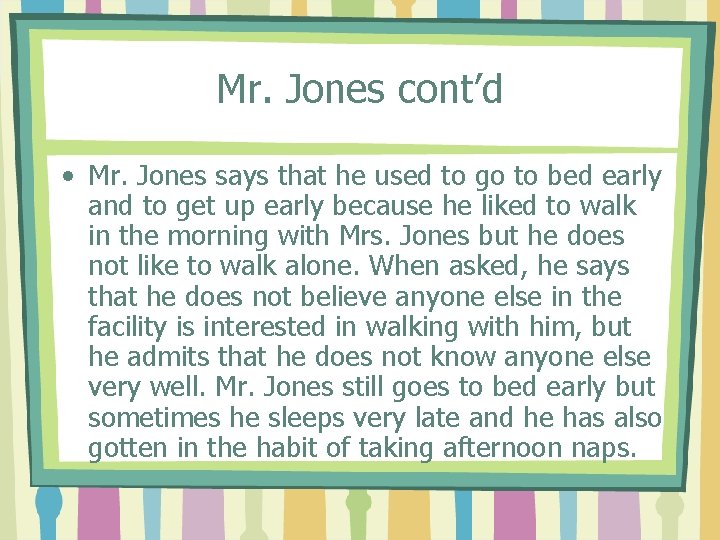
Mr. Jones cont’d • Mr. Jones says that he used to go to bed early and to get up early because he liked to walk in the morning with Mrs. Jones but he does not like to walk alone. When asked, he says that he does not believe anyone else in the facility is interested in walking with him, but he admits that he does not know anyone else very well. Mr. Jones still goes to bed early but sometimes he sleeps very late and he has also gotten in the habit of taking afternoon naps.
Mr. Jones cont’d • • Subjective? Objective? Assessment? Plan?
SOAPIE, SOAPIER • I – Intervention (implementing the plan) • E - Evaluation • R – Revision • It starts to get more and more complicated…
Other types of documentation or charting • Focus – developed in part in response to SOAP • Each series (DAR following) refers to a ‘focus’ • A ‘focus’ can be a sign or symptom, a diagnosis, patient behavior, special need, change in patient’s condition, significant event
FOCUS – D –Data – subjective and objective – Action – immediate and future actions (assessment + plan) – R – response – patient/client response to care (evaluation in SOAPIE or SOAPIER notes) – Example
Focus/DAR • Flexible • Process-oriented • Some of the same problems as with SOAP – lengthy, duplication, difficult to sort out what is REALLY important, etc.
CBE – Charting By Exception • Goals: – Eliminate lengthy and repetitive notes – Eliminate poorly organized information (how to determine what is important? ) – Eliminate possibility of overlooking the really important things
CBE – Charting By Exception • Facilities that use CBE will have explicit guidelines – – Diagnosis based standardized care plans Patient care guidelines – individualized per patient Prescribed medical interventions (physician orders) Incidental orders – one time or infrequent things • Standards of ordinary care spelled out (no need to chart everything) • Acceptable level of routine care is spelled out
CBE – Charting By Exception • To simplify – charting/documenting is centered on things that are wrong, abnormal, out of the ordinary • Time and space is not taken up to write normal care, of course, this assumes that normal care is always done • May be brief, lack some of the information provided by other forms • Development of standards of care is time consuming; standards must be clearly understood before this method can be used
Automated Systems • Vary by organization (+ or – depending on ease of use of system) • Immediate retrieval/sharing of information by all members of treatment team (+) • May need to share equipment (-) • Has some built in programming and prompts (+ for standards and accreditation, things can’t get left out; - for flexibility, some things cannot be put in)
Automated Systems • Advantages probably outweigh disadvantages • Immediate retrieval/sharing of pt/client information with any other facility in the world, storage far more simple than paper records – Obvious concerns about privacy apply • Should simplify billing, scheduling, treatment, etc. • Clients/patients can become more involved in care if they can access systems from home (outpatient care)