Do SpeechLanguage Pathology Graduate Students Obtain the Knowledge
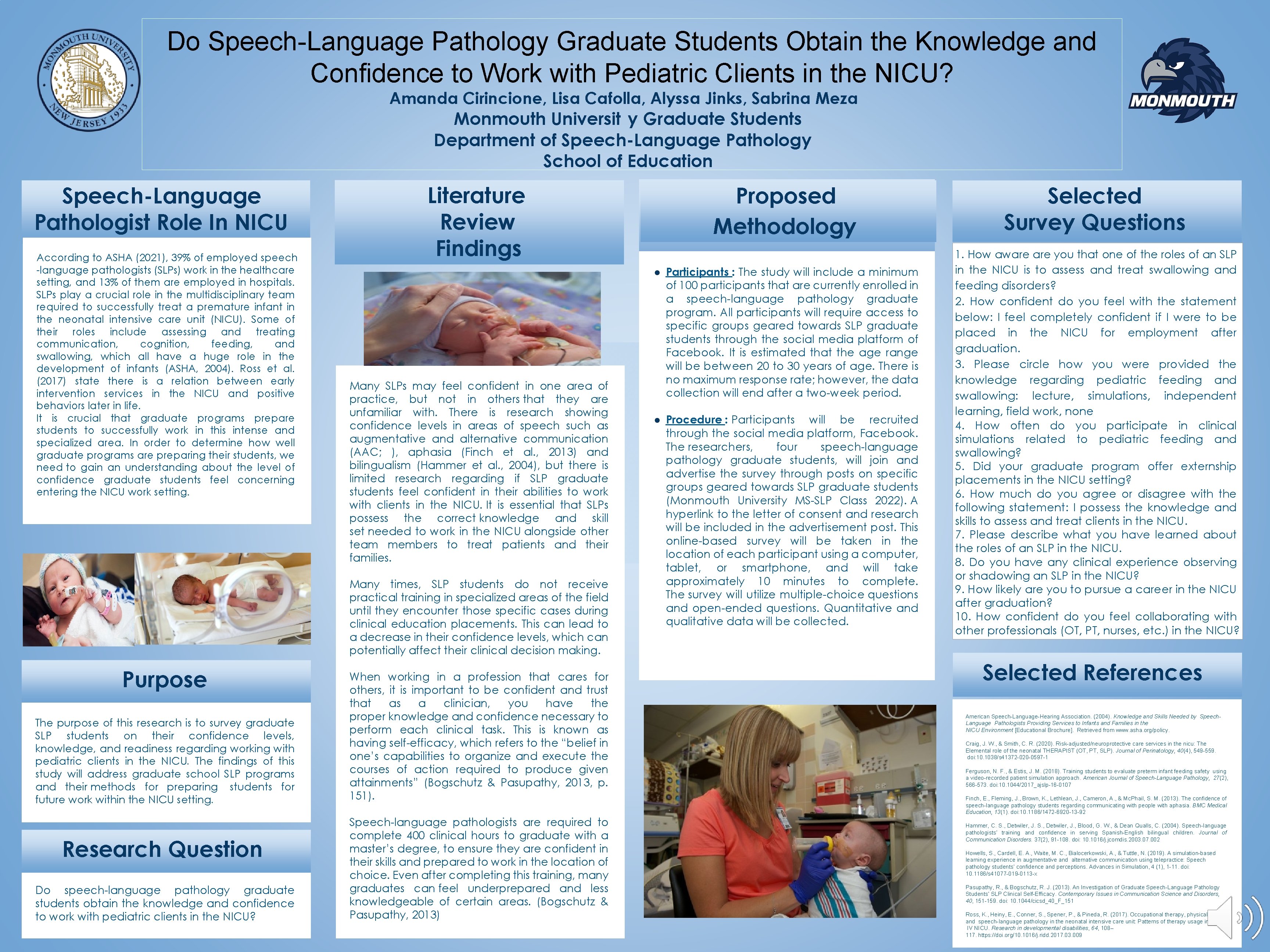
Do Speech-Language Pathology Graduate Students Obtain the Knowledge and Confidence to Work with Pediatric Clients in the NICU? Amanda Cirincione, Lisa Cafolla, Alyssa Jinks, Sabrina Meza Monmouth Universit y Graduate Students Department of Speech-Language Pathology School of Education Speech-Language Pathologist Role In NICU According to ASHA (2021), 39% of employed speech -language pathologists (SLPs) work in the healthcare setting, and 13% of them are employed in hospitals. SLPs play a crucial role in the multidisciplinary team required to successfully treat a premature infant in the neonatal intensive care unit (NICU). Some of their roles include assessing and treating communication, cognition, feeding, and swallowing, which all have a huge role in the development of infants (ASHA, 2004). Ross et al. (2017) state there is a relation between early intervention services in the NICU and positive behaviors later in life. It is crucial that graduate programs prepare students to successfully work in this intense and specialized area. In order to determine how well graduate programs are preparing their students, we need to gain an understanding about the level of confidence graduate students feel concerning entering the NICU work setting. Literature Review Findings Many SLPs may feel confident in one area of practice, but not in others that they are unfamiliar with. There is research showing confidence levels in areas of speech such as augmentative and alternative communication (AAC; ), aphasia (Finch et al. , 2013) and bilingualism (Hammer et al. , 2004), but there is limited research regarding if SLP graduate students feel confident in their abilities to work with clients in the NICU. It is essential that SLPs possess the correct knowledge and skill set needed to work in the NICU alongside other team members to treat patients and their families. Many times, SLP students do not receive practical training in specialized areas of the field until they encounter those specific cases during clinical education placements. This can lead to a decrease in their confidence levels, which can potentially affect their clinical decision making. Purpose The purpose of this research is to survey graduate SLP students on their confidence levels, knowledge, and readiness regarding working with pediatric clients in the NICU. The findings of this study will address graduate school SLP programs and their methods for preparing students for future work within the NICU setting. Research Question Do speech-language pathology graduate students obtain the knowledge and confidence to work with pediatric clients in the NICU? When working in a profession that cares for others, it is important to be confident and trust that as a clinician, you have the proper knowledge and confidence necessary to perform each clinical task. This is known as having self-efficacy, which refers to the “belief in one’s capabilities to organize and execute the courses of action required to produce given attainments” (Bogschutz & Pasupathy, 2013, p. 151). Speech-language pathologists are required to complete 400 clinical hours to graduate with a master’s degree, to ensure they are confident in their skills and prepared to work in the location of choice. Even after completing this training, many graduates can feel underprepared and less knowledgeable of certain areas. (Bogschutz & Pasupathy, 2013) Proposed Methodology ● Participants : The study will include a minimum of 100 participants that are currently enrolled in a speech-language pathology graduate program. All participants will require access to specific groups geared towards SLP graduate students through the social media platform of Facebook. It is estimated that the age range will be between 20 to 30 years of age. There is no maximum response rate; however, the data collection will end after a two-week period. ● Procedure : Participants will be recruited through the social media platform, Facebook. The researchers, four speech-language pathology graduate students, will join and advertise the survey through posts on specific groups geared towards SLP graduate students (Monmouth University MS-SLP Class 2022). A hyperlink to the letter of consent and research will be included in the advertisement post. This online-based survey will be taken in the location of each participant using a computer, tablet, or smartphone, and will take approximately 10 minutes to complete. The survey will utilize multiple-choice questions and open-ended questions. Quantitative and qualitative data will be collected. Selected Survey Questions 1. How aware you that one of the roles of an SLP in the NICU is to assess and treat swallowing and feeding disorders? 2. How confident do you feel with the statement below: I feel completely confident if I were to be placed in the NICU for employment after graduation. 3. Please circle how you were provided the knowledge regarding pediatric feeding and swallowing: lecture, simulations, independent learning, field work, none 4. How often do you participate in clinical simulations related to pediatric feeding and swallowing? 5. Did your graduate program offer externship placements in the NICU setting? 6. How much do you agree or disagree with the following statement: I possess the knowledge and skills to assess and treat clients in the NICU. 7. Please describe what you have learned about the roles of an SLP in the NICU. 8. Do you have any clinical experience observing or shadowing an SLP in the NICU? 9. How likely are you to pursue a career in the NICU after graduation? 10. How confident do you feel collaborating with other professionals (OT, PT, nurses, etc. ) in the NICU? Selected References American Speech-Language-Hearing Association. (2004). Knowledge and Skills Needed by Speech. Language Pathologists Providing Services to Infants and Families in the NICU Environment [Educational Brochure]. Retrieved from www. asha. org/policy. Craig, J. W. , & Smith, C. R. (2020). Risk-adjusted/neuroprotective care services in the nicu: The Elemental role of the neonatal THERAPIST (OT, PT, SLP). Journal of Perinatology, 40(4), 549 -559. doi: 10. 1038/s 41372 -020 -0597 -1 Ferguson, N. F. , & Estis, J. M. (2018). Training students to evaluate preterm infant feeding safety using a video-recorded patient simulation approach. American Journal of Speech-Language Pathology, 27(2), 566 -573. doi: 10. 1044/2017_ajslp-16 -0107 Finch, E. , Fleming, J. , Brown, K. , Lethlean, J. , Cameron, A. , & Mc. Phail, S. M. (2013). The confidence of speech-language pathology students regarding communicating with people with aphasia. BMC Medical Education, 13(1). doi: 10. 1186/1472 -6920 -13 -92 Hammer, C. S. , Detwiler, J. , Blood, G. W. , & Dean Qualls, C. (2004). Speech-language pathologists’ training and confidence in serving Spanish-English bilingual children. Journal of Communication Disorders. 37(2), 91 -108. doi: 10. 1016/j. jcomdis. 2003. 07. 002 Howells, S. , Cardell, E. A. , Waite, M. C. , Bialocerkowski, A. , & Tuttle, N. (2019). A simulation-based learning experience in augmentative and alternative communication using telepractice: Speech pathology students’ confidence and perceptions. Advances in Simulation, 4 (1), 1 -11. doi: 10. 1186/s 41077 -019 -0113 -x Pasupathy, R. , & Bogschutz, R. J. (2013). An Investigation of Graduate Speech-Language Pathology Students’ SLP Clinical Self-Efficacy. Contemporary Issues in Communication Science and Disorders, 40, 151 -159. doi: 10. 1044/cicsd_40_F_151 Ross, K. , Heiny, E. , Conner, S. , Spener, P. , & Pineda, R. (2017). Occupational therapy, physical therapy and speech-language pathology in the neonatal intensive care unit: Patterns of therapy usage in a level IV NICU. Research in developmental disabilities, 64, 108– 117. https: //doi. org/10. 1016/j. ridd. 2017. 03. 009
- Slides: 1