Do Not Attempt CardioPulmonary Resuscitation DNACPR Update on
- Slides: 15
Do Not Attempt Cardio-Pulmonary Resuscitation (DNACPR) Update on National Changes 2016
Do Not Attempt Cardio-Pulmonary Resuscitation (DNACPR) • • Background Key messages DNACPR within the wider context of ACP Person Centred Care
Background • 13 -17% of patients who have a cardiac arrest in hospital will survive to discharge (Ferguson et al 2008) • Living and Dying Well (SG 2008, 2011) • DNACPR Policy 2010 • Tracey Judgement June 2014 • BMA/RCN/RC(UK) – “Decisions Relating to CPR” 3 rd ed. – July 2014 • Caring for people in the last days and hours (SG 2014)
Background / Context • SG Health and Sport Committee Enquiry into Palliative Care • Strategic Framework For Palliative Care (SG/2015) • Montgomery vs Lanarkshire Health Board - Judgement (2015) • Winspear vs Sunderland NHS Foundation Trust - Judgement (2015) • BMA/RCN/RC(UK) – “Decisions Relating to CPR” revised 3 rd ed. – July 2016
Summary of progress to date. . . • SG set up a group to perform a Light Touch Review of the DNACPR adult Policy and CYPADM Oct 2014 • Representation across Scotland services • Recognition that DNAPCR is everyone’s business • Acknowledgement that conversations about DNAPCR do not sit in isolation – should be sensitively facilitated within the wider context of Advance/Anticipatory Care Planning (ACP) • Consultation process August –September 2015 • Review following further legislative changes Jan-Aug 2016 • Launch of updated policy & documentation – August 2016 • Shared approach to dissemination of information – everyones’ responsibility
The culture shift in communication - DNACPR as a prompt not a focus? Puts death on the horizon for clinicians Prompts escalation planning What if they were to suddenly collapse? - would CPR work? , - would ITU/HDU be appropriate? - would they be for any resuscitative measures ? (fluids, blood, NIV etc) Prompts goals of care discussions - out of possible realistic treatments what would the patient want?
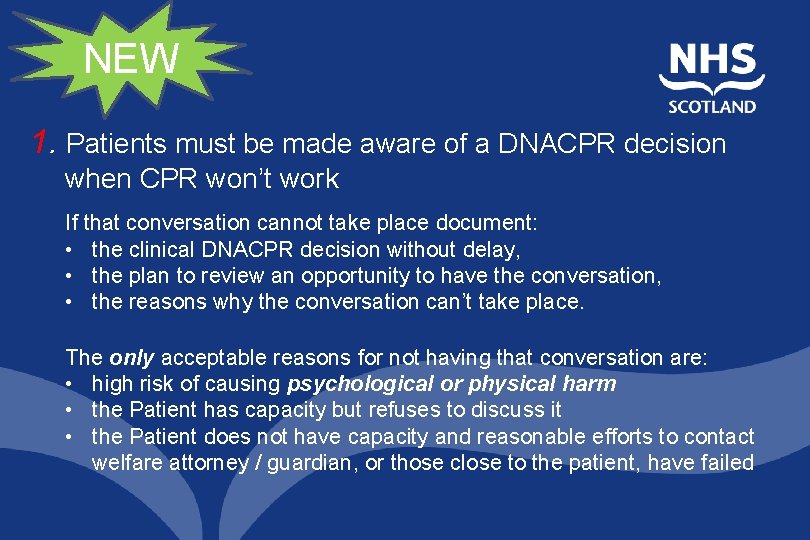
NEW 1. Patients must be made aware of a DNACPR decision when CPR won’t work If that conversation cannot take place document: • the clinical DNACPR decision without delay, • the plan to review an opportunity to have the conversation, • the reasons why the conversation can’t take place. The only acceptable reasons for not having that conversation are: • high risk of causing psychological or physical harm • the Patient has capacity but refuses to discuss it • the Patient does not have capacity and reasonable efforts to contact welfare attorney / guardian, or those close to the patient, have failed
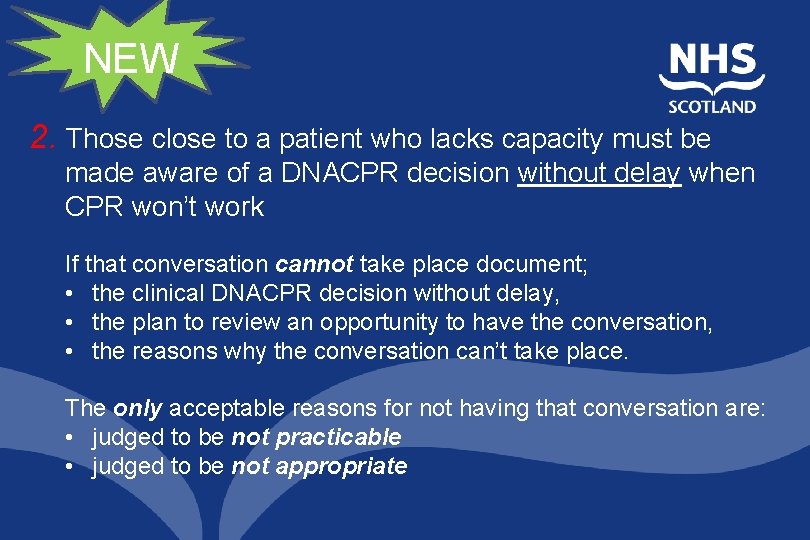
NEW 2. Those close to a patient who lacks capacity must be made aware of a DNACPR decision without delay when CPR won’t work If that conversation cannot take place document; • the clinical DNACPR decision without delay, • the plan to review an opportunity to have the conversation, • the reasons why the conversation can’t take place. The only acceptable reasons for not having that conversation are: • judged to be not practicable • judged to be not appropriate
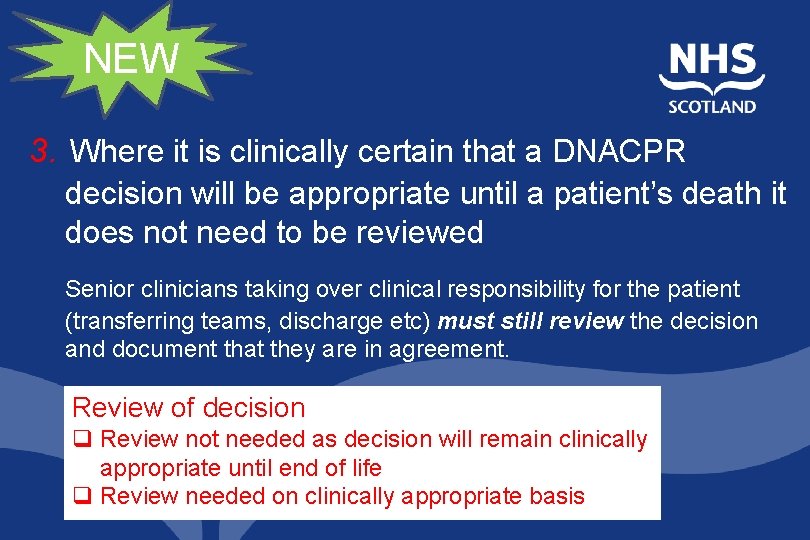
NEW 3. Where it is clinically certain that a DNACPR decision will be appropriate until a patient’s death it does not need to be reviewed Senior clinicians taking over clinical responsibility for the patient (transferring teams, discharge etc) must still review the decision and document that they are in agreement. Review of decision q Review not needed as decision will remain clinically appropriate until end of life q Review needed on clinically appropriate basis
Key messages • The death rate is 100%! • Almost 30% of people in a hospital bed today will die within a year (Clark et al 2014) • A DNACPR decision is intended to prevent inappropriate attempts at CPR where it clearly will not work or would not be wanted by a patient • The DNACPR form is not a legal document and is not a decision –it is a record of a decision made in advance to provide guidance which can inform clinicians who do not know the patient and who may be summoned to assess an emergency situation • Documented evidence of communication is essential • If conversation does not take place: document rationale
Key messages cont’d. • Where a patient’s natural death is anticipated by the clinical team, and they are obviously imminently dying (within hours to several days), CPR is clearly contraindicated as it would not work and would only cause harm. If a DNACPR form has been overlooked in this situation the decision not to initiate CPR can be made by a nurse or junior doctor who is with the patient when this type of expected death occurs. • DNACPR forms completed prior to the launch of the new NHS Scotland DNACPR Policy (2016) will remain valid and a completed 2010 form does not need to be replaced with a new form. • Review should take place at transitions of care.
DNACPR…made easy • D • N • A • • • Decision making that is responsive to individual… Needs and is discussed within the wider context of. . . Advance care planning that includes realistic goals of care with sensitive. . . C Communication to facilitate compassionate care by. . . P Preparing people in a. . . R Respectful manner to reduce the risk of an undignified death, support bereavement care, and may also reduce the risk of possible complaint NB. The consequences of not having a form signed when a natural death is expected are: - undignified death; - unnecessary stress for families (especially at home); - potential conflict between teams leading to stress for staff.
Person Centred Care. . . • • • What matters to you? Who matters to you? What information do you need? Personalised contact Nothing about me without me
DNACPR Education Resources • ACP toolkit and DNACPR information www. palliativecareinpractice. nes. scot. nhs. uk • Video developed for online hospital consultants’ module – open access http: //www. mystar. org. uk/dnacpr/start. asp • Online module for Foundation Year Doctors www. nhseportfolios. org • Communication aspects of DNACPR discussions - videos available via palliative care in practice website www. palliativecareinpractice. nes. scot. nhs. uk/advanceanticipatory-care-planning-toolkit/dnacpr. aspx
DNACPR Document links • Living and Dying Well (SG 2008, 2011) http: //www. gov. scot/Resource/Doc/340076/0112559. pdf • Are we Living and Dying Well https: //www. mariecurie. org. uk/globalassets/media/images/blog/2014/05/are-we-living-a -dying-well-yet-final-report. pdf • DNACPR Policy 2016 www. scotland. gov. uk/dnacpr • Tracey Judgement June 2015 http: //www. 39 essex. com/docs/cases/tracey_final_2. pdf • BMA/RC(UK)/RCN (June 2016) https: //www. resus. org. uk/dnacpr/decisions-relating-to-cpr/ • Caring for people in the last days and hours (SG 2014) http: //www. gov. scot/Resource/00466779. pdf • Person Centred Care Strategy http: //nhsforthvalley. com/wp-content/uploads/2014/01/NHS-Forth. Valley. Person Centred Care-Strategy. pdf • Realistic Medicine http: //www. gov. scot/Resource/00492520. pdf • A National Clinical Strategy for Scotland http: //www. gov. scot/Resource/00494144. pdf • Atul Gawande – “Being Mortal” http: //atulgawande. com/book/being-mortal/