DNP Project Formal Review Rachel Livingston CPNP DNP
- Slides: 42
DNP Project Formal Review Rachel Livingston, CPNP DNP Candidate May 2018
The Journey • Journey suggests travel or passage from one place to another such as the journey from youth to maturity. • a journey through time. • JOURNEY usually means traveling a long distance and often in dangerous or difficult circumstances. https: //www. merriam-webster. com/dictionary/journey
The Journey
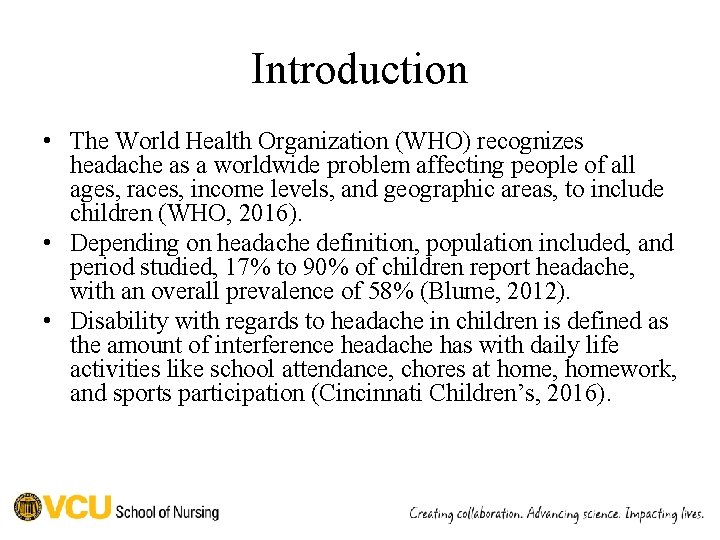
Introduction • The World Health Organization (WHO) recognizes headache as a worldwide problem affecting people of all ages, races, income levels, and geographic areas, to include children (WHO, 2016). • Depending on headache definition, population included, and period studied, 17% to 90% of children report headache, with an overall prevalence of 58% (Blume, 2012). • Disability with regards to headache in children is defined as the amount of interference headache has with daily life activities like school attendance, chores at home, homework, and sports participation (Cincinnati Children’s, 2016).
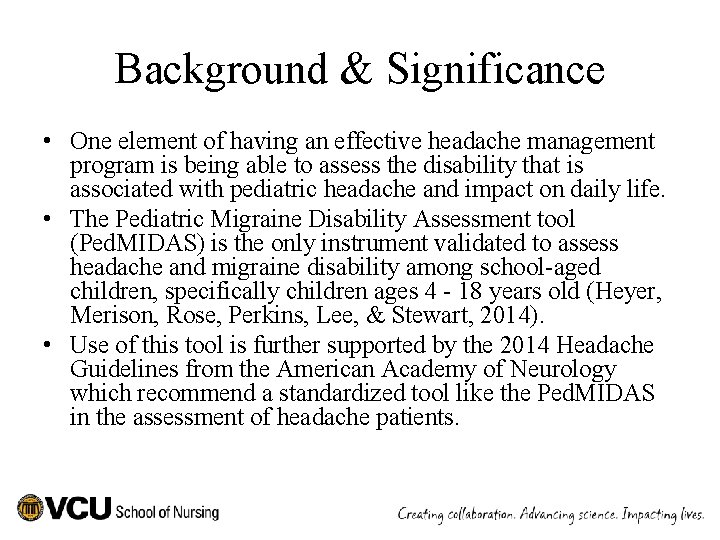
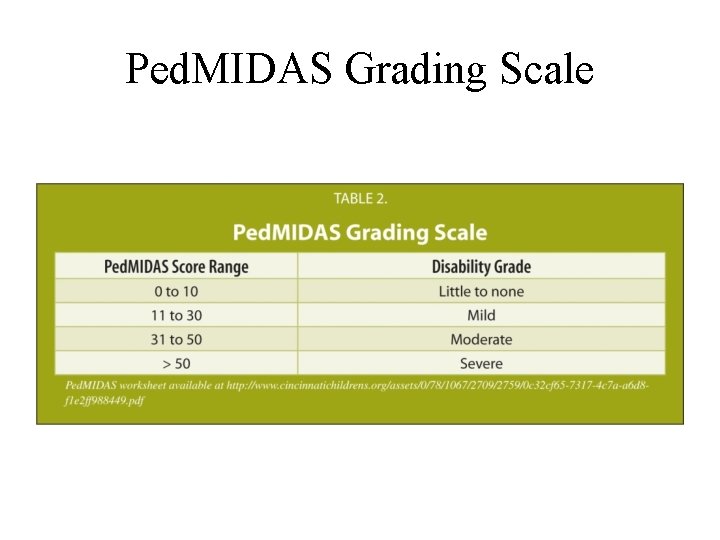
Background & Significance • One element of having an effective headache management program is being able to assess the disability that is associated with pediatric headache and impact on daily life. • The Pediatric Migraine Disability Assessment tool (Ped. MIDAS) is the only instrument validated to assess headache and migraine disability among school-aged children, specifically children ages 4 - 18 years old (Heyer, Merison, Rose, Perkins, Lee, & Stewart, 2014). • Use of this tool is further supported by the 2014 Headache Guidelines from the American Academy of Neurology which recommend a standardized tool like the Ped. MIDAS in the assessment of headache patients.
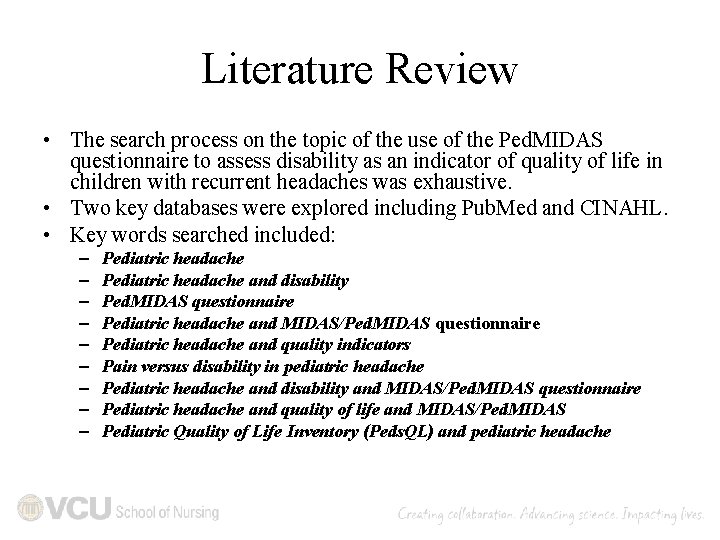
Literature Review • The search process on the topic of the use of the Ped. MIDAS questionnaire to assess disability as an indicator of quality of life in children with recurrent headaches was exhaustive. • Two key databases were explored including Pub. Med and CINAHL. • Key words searched included: – – – – – Pediatric headache and disability Ped. MIDAS questionnaire Pediatric headache and MIDAS/Ped. MIDAS questionnaire Pediatric headache and quality indicators Pain versus disability in pediatric headache Pediatric headache and disability and MIDAS/Ped. MIDAS questionnaire Pediatric headache and quality of life and MIDAS/Ped. MIDAS Pediatric Quality of Life Inventory (Peds. QL) and pediatric headache
Analysis of the Literature • There were only 8 studies found that included the Ped. MIDAS. • These studies addressed either the Ped. MIDAS or the Ped. MIDAS and the Peds. QL together. • Studies that addressed the Peds. QL alone were not included for further analysis as use of the Ped. MIDAS is the focus of this quality initiative.
Key Points from Literature Analysis • This literature review and analysis demonstrates the usefulness of standardized questionnaires in assessing childhood headache as it relates to disability and quality of life • The Ped. MIDAS questionnaire as a validated tool is the main focus for this research question because it is well-known and recognized in the pediatric headache field and is easy to use in the clinical setting • This review supports the implementation and use of this questionnaire, while at the same time cautioning that function related to headache on non-school days may be underestimated
Key Points from Literature Analysis • Use of this tool is further supported by the 2014 Headache Guidelines from the American Academy of Neurology which recommend a standardized tool like the Ped. MIDAS in the assessment of headache patients. • This review of the literature and analysis of the evidence does not specifically address if use of this questionnaire transforms practice by generating practice changes based on questionnaire scores.
PURPOSE • Due to the prevalence of pediatric headache and the associated cost, child neurology groups are establishing headache programs to help manage this disorder. • One element of having an effective headache management program is being able to assess the disability that is associated with pediatric headache to understand the impact on quality of life and determine appropriate treatment needs.
Problem Statement • Research question: In providing care for pediatric patients with headaches, how does implementation of the Ped. MIDAS disability scale impact practice with regards to tool use and provider perspective of helpfulness over a one-year period?
Project Description • This question directs a program evaluation of a practice change, where use of the tool, which is new to the provider group, will be reviewed for consistency of use, effectiveness, and successful implementation. • If this program evaluation reveals that the use of the Ped. MIDAS tool is a positive practice change in assessing pediatric headache, continued use (through comparison with baseline scores), could subsequently help guide standardization of headache management for these children.
Ped. MIDAS
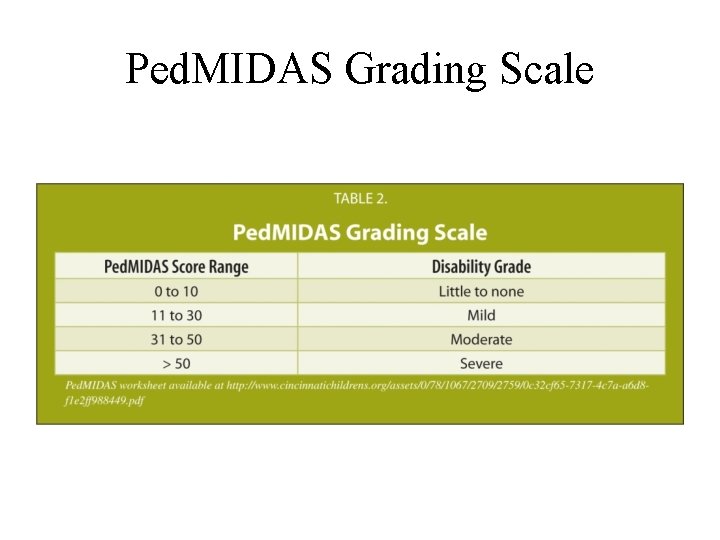
Ped. MIDAS Grading Scale
Theoretical Framework • The model used to support evidence-based practice through research at VCUHS is the Johns Hopkins Nursing Evidence-Based Practice model (JHNEBP). • The goal of this model is to transform knowledge into practice by allowing research to take place at the patient care level and have a direct impact on nursing practice.
Theoretical Framework • When research is undertaken using this change model, implementation is based on the process of looking at a practice question, analyzing the evidence, and then translating the evidence into practice (Dang et al. , 2015). • Since this practice change is taking place at VCUHS and the program evaluation will have a direct impact on VCUHS, it makes sense to use theoretical framework that is already supported within this health system.
Theoretical Framework • This project focuses on a program evaluation to see if this practice change implementation was successful, helps identify treatment and testing commonalities, and if providers found this practice change helpful.
Theoretical Framework • Plan-Do-Study-Act (PDSA) was also an integral part of this project. (ihi. org) • The Ped. MIDAS tool was used in several different forms during this project to try and increase use. (dryerase, paper with scanning, electronic) • Re-education was also provided based on the monitoring of tool use in an effort to increase its use. (July 2016, Oct. 2016, Jan. 2017, July 2017, October 2017)
Project Design • Retrospective chart review (11 -21 -16 to 11 -3017) following provider/staff education regarding the Ped. MIDAS. • All charts were reviewed by the primary investigator (PI). • Provider satisfaction with the Ped. MIDAS was evaluated separately through a PI created, four item survey questionnaire.
Project Implementation • Use of the Ped. MIDAS tool was instituted within the child neurology clinic at VCU in July 2016. • Providers, medical assistants, and nursing staff were educated about use of the tool prior to initiation of its use through inservice training within the clinic. • All in-services were provided by the PI of this study. • Data collection for this study began in November 2016 with this start date being chosen to allow staff to complete training practice with the tool prior to analyzing implementation. • Re-education was provided in October 2016, January 2017, July 2017, and October 2017 in an effort to further promote survey use.
Project Implementation • This project was reviewed by the VCU IRB and found to be exempt as a quality improvement initiative. • Cost: – Since this study represents a retrospective chart review, the cost is minimal. – The questionnaire is available free of charge from the Cincinnati Children’s website with permission to duplicate for patient use.
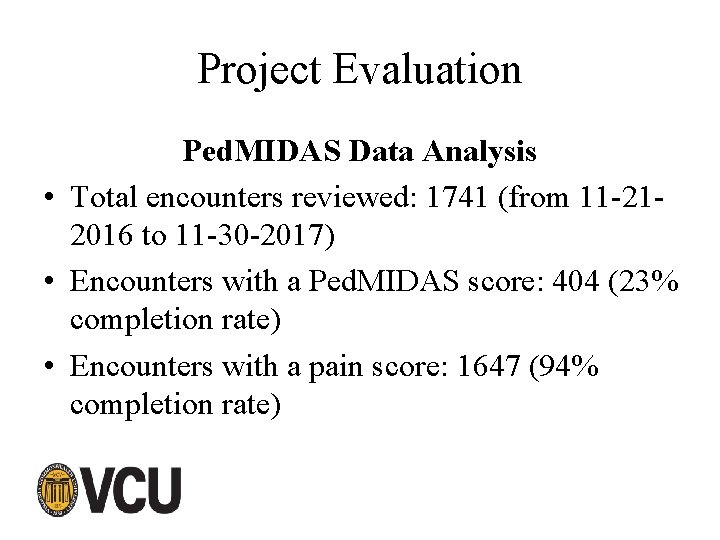
Project Evaluation Ped. MIDAS Data Analysis • Total encounters reviewed: 1741 (from 11 -212016 to 11 -30 -2017) • Encounters with a Ped. MIDAS score: 404 (23% completion rate) • Encounters with a pain score: 1647 (94% completion rate)
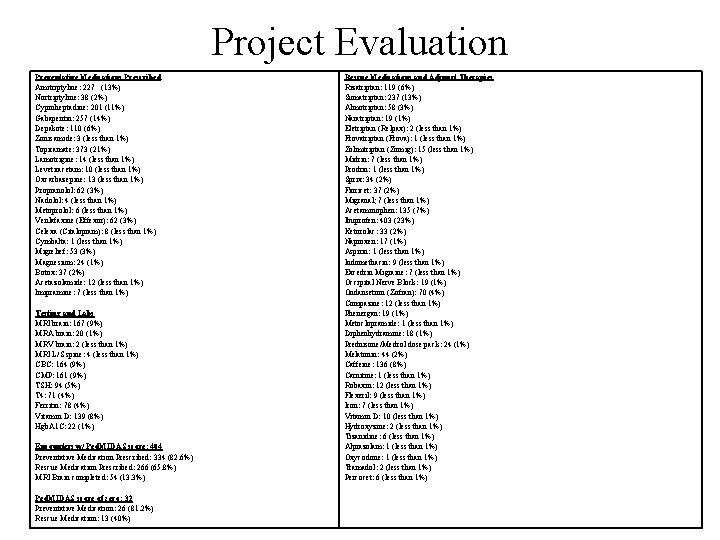
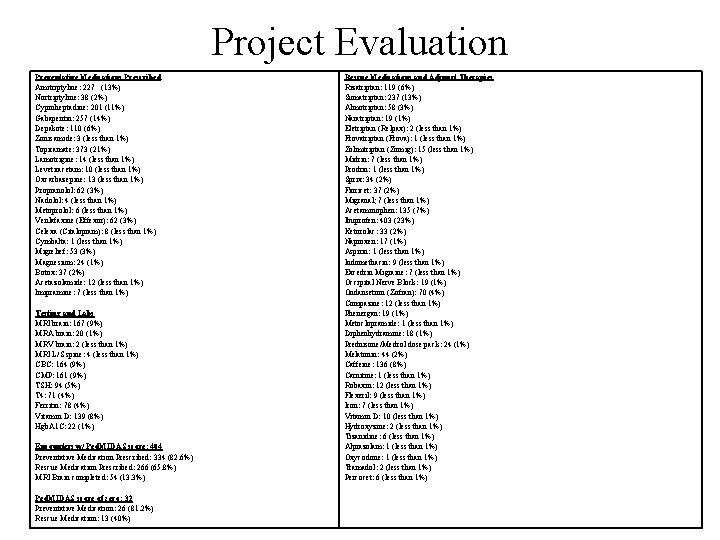
Project Evaluation Preventative Medications Prescribed Amitriptyline: 227 (13%) Nortriptyline: 38 (2%) Cyproheptadine: 201 (11%) Gabapentin: 257 (14%) Depakote: 110 (6%) Zonisamide: 3 (less than 1%) Topiramate: 373 (21%) Lamotrigine: 14 (less than 1%) Levetiracetam: 10 (less than 1%) Oxcarbazepine: 13 (less than 1%) Propranolol: 62 (3%) Nadolol: 4 (less than 1%) Metoprolol: 6 (less than 1%) Venlafaxine (Effexor): 62 (3%) Celexa (Citalopram): 8 (less than 1%) Cymbalta: 1 (less than 1%) Migrelief: 53 (3%) Magnesium: 24 (1%) Botox: 37 (2%) Acetazolamide: 12 (less than 1%) Imipramine: 7 (less than 1%) Testing and Labs MRI brain: 167 (9%) MRA brain: 20 (1%) MRV brain: 2 (less than 1%) MRI L/S spine: 4 (less than 1%) CBC: 164 (9%) CMP: 161 (9%) TSH: 94 (5%) T 4: 71 (4%) Ferritin: 78 (4%) Vitamin D: 139 (8%) Hgb. A 1 C: 22 (1%) Encounters w/ Ped. MIDAS score: 404 Preventative Medication Prescribed: 334 (82. 6%) Rescue Medication Prescribed: 266 (65. 8%) MRI Brain completed: 54 (13. 3%) Ped. MIDAS score of zero: 32 Preventative Medication: 26 (81. 2%) Rescue Medication: 13 (40%) Rescue Medications and Adjunct Therapies Rizatriptan: 119 (6%) Sumatriptan: 237 (13%) Almotriptan: 58 (3%) Naratriptan: 19 (1%) Eletriptan (Relpax): 2 (less than 1%) Frovatriptan (Frova): 1 (less than 1%) Zolmitriptan (Zomig): 15 (less than 1%) Midrin: 7 (less than 1%) Prodrin: 1 (less than 1%) Sprix: 34 (2%) Fioricet: 37 (2%) Migranal; 7 (less than 1%) Acetaminophen: 135 (7%) Ibuprofen: 403 (23%) Ketorolac: 33 (2%) Naproxen: 17 (1%) Aspirin: 1 (less than 1%) Indomethacin: 9 (less than 1%) Excedrin Migraine: 7 (less than 1%) Occipital Nerve Block: 19 (1%) Ondansetron (Zofran): 70 (4%) Compazine: 12 (less than 1%) Phenergan: 19 (1%) Metoclopramide: 1 (less than 1%) Diphenhydramine: 18 (1%) Prednisone/Medrol dose pack: 24 (1%) Melatonin: 44 (2%) Caffeine: 136 (8%) Carnitine: 1 (less than 1%) Robaxin: 12 (less than 1%) Flexeril: 9 (less than 1%) Iron: 7 (less than 1%) Vitamin D: 10 (less than 1%) Hydroxyzine: 2 (less than 1%) Tizanidine: 6 (less than 1%) Alprazolam: 1 (less than 1%) Oxycodone: 1 (less than 1%) Tramadol: 2 (less than 1%) Percocet: 6 (less than 1%)
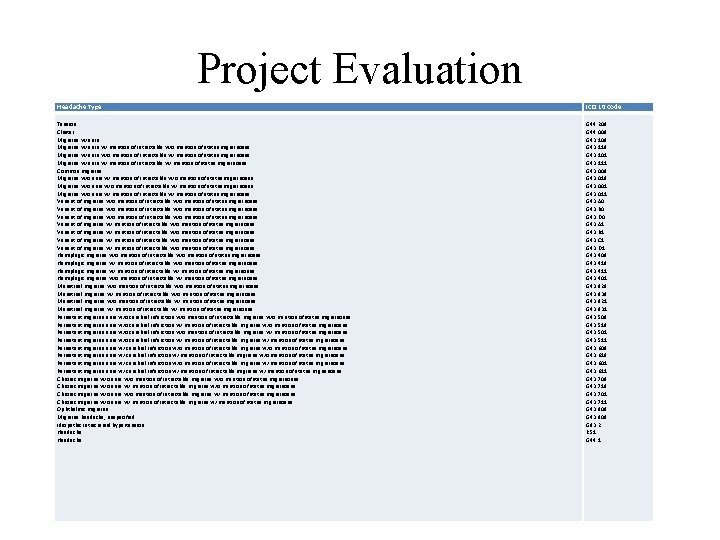
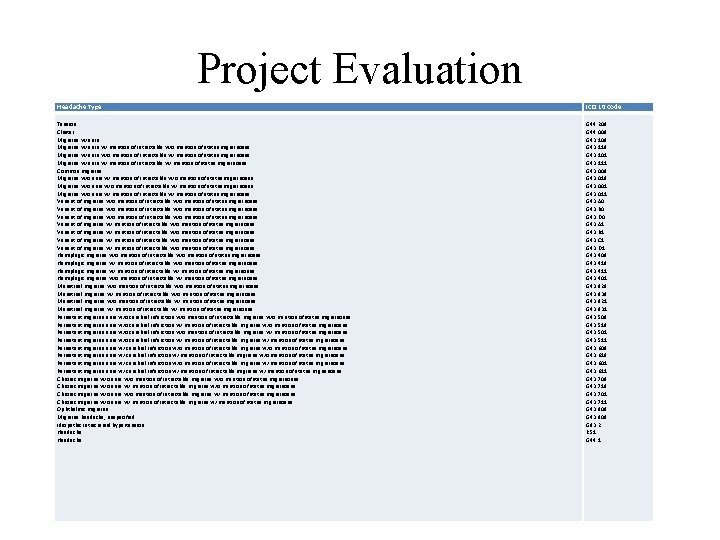
Project Evaluation Headache Type ICD 10 Code Tension Cluster Migraine w/ aura w/ mention of intractable w/o mention of status migrainosus Migraine w/ aura w/o mention of intractable w/ mention of status migrainosus Migraine w/ aura w/ mention of intractable w/ mention of status migrainosus Common migraine Migraine w/o aura w/ mention of intractable w/o mention of status migrainosus Migraine w/o aura w/o mention of intractable w/ mention of status migrainosus Migraine w/o aura w/ mention of intractable w/ mention of status migrainosus Variant of migraine w/o mention of intractable w/o mention of status migrainosus Variant of migraine w/ mention of intractable w/o mention of status migrainosus Hemiplegic migraine w/o mention of intractable w/o mention of status migrainosus Hemiplegic migraine w/ mention of intractable w/ mention of status migrainosus Hemiplegic migraine w/o mention of intractable w/ mention of status migrainosus Menstrual migraine w/o mention of intractable w/o mention of status migrainosus Menstrual migraine w/o mention of intractable w/ mention of status migrainosus Menstrual migraine w/ mention of intractable w/ mention of status migrainosus Persistent migraine aura w/o cerebral infarction w/o mention of intractable migraine w/o mention of status migrainosus Persistent migraine aura w/o cerebral infarction w/o mention of intractable migraine w/ mention of status migrainosus Persistent migraine aura w/o cerebral infarction w/ mention of intractable migraine w/ mention of status migrainosus Persistent migraine aura w/ cerebral infarction w/o mention of intractable migraine w/o mention of status migrainosus Persistent migraine aura w/ cerebral infarction w/o mention of intractable migraine w/ mention of status migrainosus Persistent migraine aura w/ cerebral infarction w/ mention of intractable migraine w/ mention of status migrainosus Chronic migraine w/o aura w/o mention of intractable migraine w/o mention of status migrainosus Chronic migraine w/o aura w/o mention of intractable migraine w/ mention of status migrainosus Chronic migraine w/o aura w/ mention of intractable migraine w/ mention of status migrainosus Ophthalmic migraine Migraine headache, unspecified Idiopathic intracranial hypertension Headache G 44. 209 G 44. 009 G 43. 119 G 43. 101 G 43. 111 G 43. 009 G 43. 019 G 43. 001 G 43. 011 G 43. A 0 G 43. B 0 G 43. D 0 G 43. A 1 G 43. B 1 G 43. C 1 G 43. D 1 G 43. 409 G 43. 411 G 43. 401 G 43. 829 G 43. 839 G 43. 821 G 43. 831 G 43. 509 G 43. 519 G 43. 501 G 43. 511 G 43. 609 G 43. 619 G 43. 601 G 43. 611 G 43. 709 G 43. 719 G 43. 701 G 43. 711 G 43. 809 G 43. 909 G 93. 2 R 51 G 44. 1
Project Evaluation Provider Survey 1. Has use of the Ped. MIDAS questionnaire been useful to your practice? Yes or No 2. If the questionnaire was helpful, how did it help? 3. If the questionnaire was not helpful, why not? 4. Additional comments:
Project Evaluation Provider survey – 55% response rate – 75% of respondents found the Ped. MIDAS to be useful – Helps quantify the disability experienced by the child related to headache which can be used to guide treatment – Helps to differentiate headache frequency from disability
Project Evaluation Secondary Gains – Upon examination of practice among the child neurology providers at VCU, the use of Topiramate and Amitriptyline is evidence-based and consistent with the AAN guideline. – The use of Ibuprofen as first-line followed by triptans, specifically Sumatriptan and Rizatriptan, is evidence-based, and prescribed consistently within the child neurology clinic at VCU. – During this chart review, MRI was only ordered 9% of the time which was consistent with addressing those patients with concern for secondary etiology. – Specific laboratory testing was completed 8 -9% of the time and is not specifically addressed in the literature as an integral part of headache management.
Project Evaluation Implications for Nursing – Assessing disability through the use of the Ped. MIDAS is a beneficial practice change for: v Helping with evaluating headache interventions v Differentiating headache frequency from disability v Clarifying the severity of pain related to headache that affects daily life.
Dissemination Plan Research outcomes will be shared as follows: – Defense presentation for the DNP program – Poster presentation on 5 -11 -18 hosted by the VCU School of Nursing for DNP students – Poster presentation at the Child Neurology Society meeting in October 2018 (applied/not yet accepted) – Journal manuscript submission to the Journal of Doctoral Nursing Practice – Power. Point presentation of information at local chapter NAPNAP meeting (no date scheduled) – May also post data on some form of social media (i. e. twitter and on my Rampages e-portfolio)
DNP Essentials DNP Essential I: Scientific Underpinnings for Practice • This essential calls for integrating knowledge into practice to effect a positive change in health status. • The practice change with instituting the Ped. MIDAS is aimed at improving quality of care for children with headache, understanding that the disability caused by headache supports looking at more effective treatment.
DNP Essentials DNP Essential II: Organizational and Systems Leadership for Quality Improvement and Systems Thinking • This essential focuses on making a difference for a target population and the need within the community. • In this case, the target population is pediatric patients with headache in the greater Richmond, Virginia and surrounding areas who need better headache management to improve quality of life. • Establishing a specific headache program at the VCUHS supports this need and use of the Ped. MIDAS is one of the first steps in standardizing headache care.
DNP Essentials DNP Essential III: Clinical Scholarship and Analytical Methods for Evidence-Based Practice • Scholarship and research are hallmarks of a doctoral degree. • Making a practice change and the evaluation of this change supports this essential.
DNP Essentials DNP Essential IV: Information Systems/Technology and Patient Care Technology for the Improvement and Transformation of Health Care • This essential involves using information technology to move patient care and promote quality. • This program evaluation relies on data from the electronic medical record for successful implementation and evaluation.
DNP Essentials DNP Essential V: Health Care Policy for Advocacy in Health Care • DNP prepared nurses are called to advocate for practice and policy change that help patients. • In this case, an institutional level practice change is being made to help the children in the Richmond, Virginia and surrounding areas to receive headache management that is evidence -based and aimed at improving quality of care.
DNP Essentials DNP Essential VI: • Patient-centered care Interprofessional Collaboration requires professionals of all for Improving Patient and disciplines to work together. Population Health Outcomes • Instituting the Ped. MIDAS has involved physicians, nurse practitioners, medical assistants, clinic-level personnel, and departmentlevel personnel all collaborating and communicating in a variety of ways.
DNP Essentials DNP Essential VII: Clinical Prevention and Population Health for Improving the Nation’s Health • The implementation of population health activities is centered on achieving the national goal of improving the health status of the population of the United States. • This project and program evaluation are occurring on a local level within the United States, with the goal of improving the health of pediatric patients with headache. • Change must start somewhere and can spread on a larger scale if successful.
DNP Essentials DNP Essential VIII: Advanced Nursing Practice • DNP prepared nurses are expected to practice at an advanced level, including the advancement of nursing science. • Implementing a practice change and evaluating this change are advanced nursing skills.
The Journey Two roads diverged in a wood, and II took the one less traveled by, And that has made all the difference
The Journey • Lessons Learned – See the big picture – Understand Systems – Be a catalyst for change E-portfolio link: https: //rampages. us/rlivingston/
Thank You!
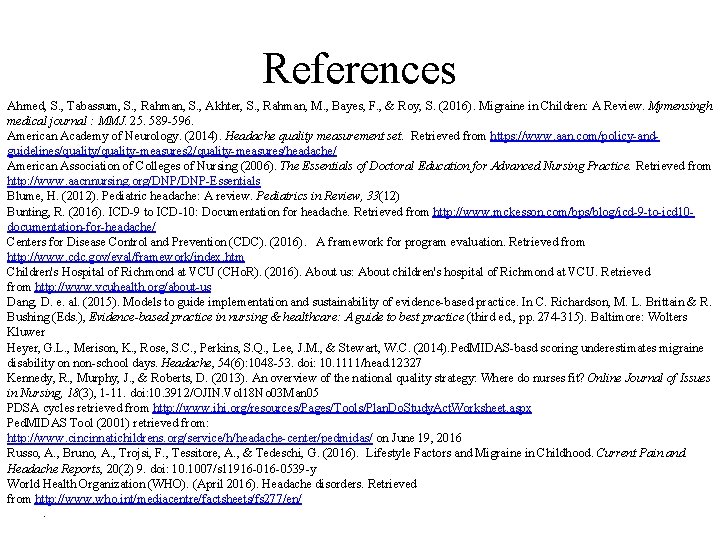
References Ahmed, S. , Tabassum, S. , Rahman, S. , Akhter, S. , Rahman, M. , Bayes, F. , & Roy, S. (2016). Migraine in Children: A Review. Mymensingh medical journal : MMJ. 25. 589 -596. American Academy of Neurology. (2014). Headache quality measurement set. Retrieved from https: //www. aan. com/policy-andguidelines/quality-measures 2/quality-measures/headache/ American Association of Colleges of Nursing (2006). The Essentials of Doctoral Education for Advanced Nursing Practice. Retrieved from http: //www. aacnnursing. org/DNP-Essentials Blume, H. (2012). Pediatric headache: A review. Pediatrics in Review, 33(12) Bunting, R. (2016). ICD-9 to ICD-10: Documentation for headache. Retrieved from http: //www. mckesson. com/bps/blog/icd-9 -to-icd 10 documentation-for-headache/ Centers for Disease Control and Prevention (CDC). (2016). A framework for program evaluation. Retrieved from http: //www. cdc. gov/eval/framework/index. htm Children's Hospital of Richmond at VCU (CHo. R). (2016). About us: About children's hospital of Richmond at VCU. Retrieved from http: //www. vcuhealth. org/about-us Dang, D. e. al. (2015). Models to guide implementation and sustainability of evidence-based practice. In C. Richardson, M. L. Brittain & R. Bushing (Eds. ), Evidence-based practice in nursing & healthcare: A guide to best practice (third ed. , pp. 274 -315). Baltimore: Wolters Kluwer Heyer, G. L. , Merison, K. , Rose, S. C. , Perkins, S. Q. , Lee, J. M. , & Stewart, W. C. (2014). Ped. MIDAS-basd scoring underestimates migraine disability on non-school days. Headache, 54(6): 1048 -53. doi: 10. 1111/head. 12327 Kennedy, R. , Murphy, J. , & Roberts, D. (2013). An overview of the national quality strategy: Where do nurses fit? Online Journal of Issues in Nursing, 18(3), 1 -11. doi: 10. 3912/OJIN. Vol 18 No 03 Man 05 PDSA cycles retrieved from http: //www. ihi. org/resources/Pages/Tools/Plan. Do. Study. Act. Worksheet. aspx Ped. MIDAS Tool (2001) retrieved from: http: //www. cincinnatichildrens. org/service/h/headache-center/pedmidas/ on June 19, 2016 Russo, A. , Bruno, A. , Trojsi, F. , Tessitore, A. , & Tedeschi, G. (2016). Lifestyle Factors and Migraine in Childhood. Current Pain and Headache Reports, 20(2) 9. doi: 10. 1007/s 11916 -0539 -y World Health Organization (WHO). (April 2016). Headache disorders. Retrieved from http: //www. who. int/mediacentre/factsheets/fs 277/en/.
Questions ?
 Saas cpnp
Saas cpnp Eu cosmetic product notification portal (cpnp)
Eu cosmetic product notification portal (cpnp) Sicodis ultima doceava 2020
Sicodis ultima doceava 2020 Chamberlain practicum handbook
Chamberlain practicum handbook Uca dnp
Uca dnp Ciclo de vida de un proyecto de inversión
Ciclo de vida de un proyecto de inversión Galeb jonathan livingston kratki sadržaj
Galeb jonathan livingston kratki sadržaj Livingston county veterans services
Livingston county veterans services Coles livingston
Coles livingston Jennifer livingston
Jennifer livingston Galeb jonathan livingston alegorija
Galeb jonathan livingston alegorija Citati galeb jonathan livingston
Citati galeb jonathan livingston Conforred
Conforred Sramota božidar prosenjak
Sramota božidar prosenjak Midas east livingston
Midas east livingston Livingston federal employee retirement planning
Livingston federal employee retirement planning Dylan livingston
Dylan livingston Citizen advice livingston
Citizen advice livingston Il gabbiano jonathan livingston attività didattiche
Il gabbiano jonathan livingston attività didattiche Coles livingston
Coles livingston Trish livingston deakin
Trish livingston deakin Richard bach galeb jonathan livingston
Richard bach galeb jonathan livingston Richard bach galeb jonathan livingston
Richard bach galeb jonathan livingston Ben livingston weather
Ben livingston weather Galeb jonathan livingston ppt
Galeb jonathan livingston ppt Lets livingston county
Lets livingston county David livingston seagull
David livingston seagull Richard bach galeb jonathan livingston
Richard bach galeb jonathan livingston Nec semiconductors livingston
Nec semiconductors livingston Norma inculta informal ejemplos
Norma inculta informal ejemplos Merits of formal education
Merits of formal education Unit 3 formal informal and nonformal education
Unit 3 formal informal and nonformal education Falsafah pendidikan khas
Falsafah pendidikan khas Karangan formal
Karangan formal Difference between als and formal education
Difference between als and formal education Komunikasi atas ke bawah
Komunikasi atas ke bawah Falasi formal dan tidak formal
Falasi formal dan tidak formal Definisi kepimpinan
Definisi kepimpinan Aap1 - linguagem e oralidade
Aap1 - linguagem e oralidade Fungsi manajemen paud
Fungsi manajemen paud Formal design reviews
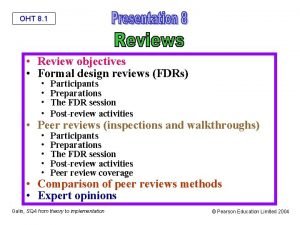
Formal design reviews Formal technical review
Formal technical review Oht design
Oht design