Dizziness Vertigo Tom Heaps Consultant Acute Physician What


- Slides: 26
Dizziness | Vertigo Tom Heaps Consultant Acute Physician
What is Dizziness? Panicky Fuzzy-head Giddy Dizzy Off-balance Light-headed Room spinning Unsteady Faint Vertigo
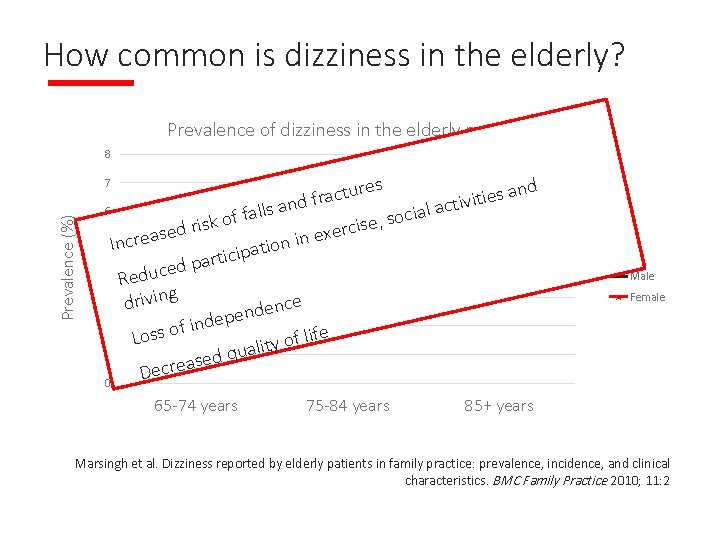
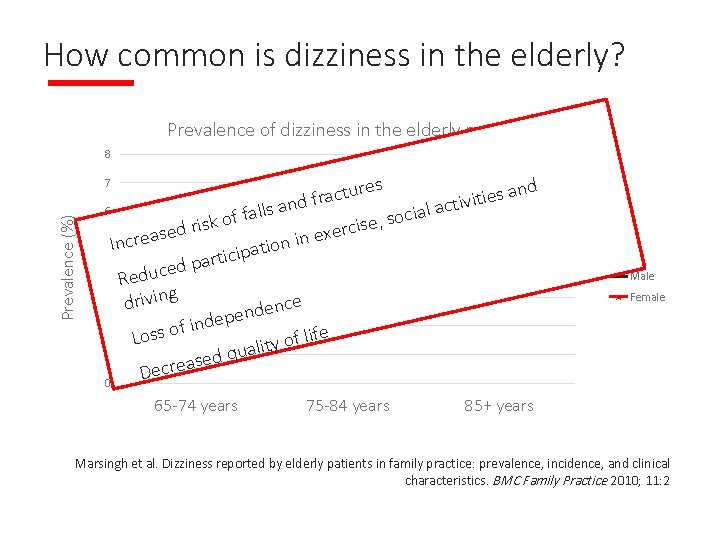
How common is dizziness in the elderly? Prevalence of dizziness in the elderly population 8 es r u and t s c a e i r t f i and activ 6 s l l l a i a f c f o ko e, s s s i i r c r d e e x 5 creas in e n In o i t icipa t r a p 4 ed Reduc g 3 drivin ence d n e p 2 nde i f o s life f Los o y t uali 1 q d e s crea e D 0 Prevalence (%) 7 65 -74 years 75 -84 years Male Female 85+ years Marsingh et al. Dizziness reported by elderly patients in family practice: prevalence, incidence, and clinical characteristics. BMC Family Practice 2010; 11: 2
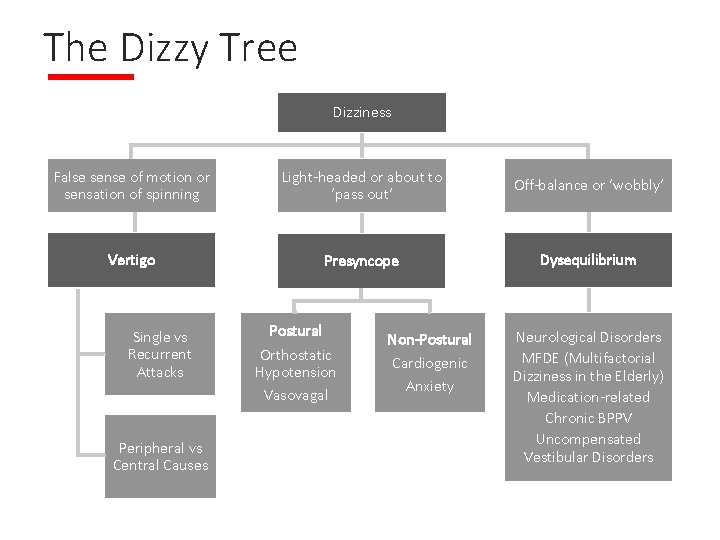
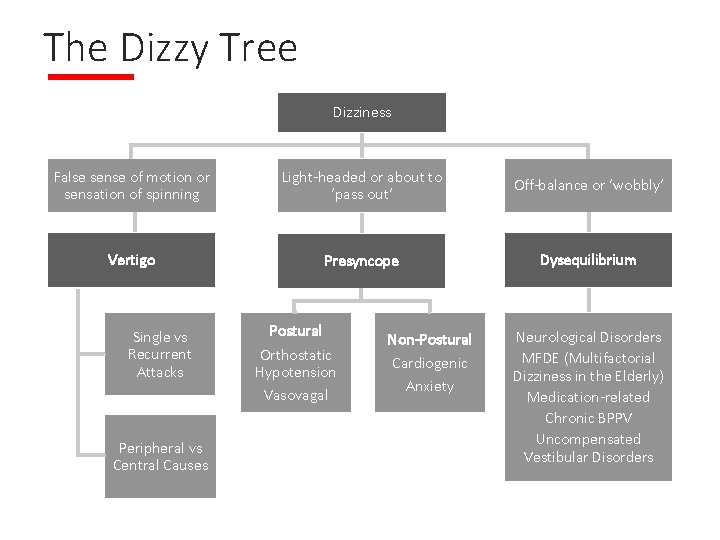
The Dizzy Tree Dizziness False sense of motion or sensation of spinning Light-headed or about to ‘pass out’ Off-balance or ‘wobbly’ Vertigo Presyncope Dysequilibrium Single vs Recurrent Attacks Peripheral vs Central Causes Postural Orthostatic Hypotension Vasovagal Non-Postural Cardiogenic Anxiety Neurological Disorders MFDE (Multifactorial Dizziness in the Elderly) Medication-related Chronic BPPV Uncompensated Vestibular Disorders

Vertigo ‘an illusory sensation of movement’ - mismatch between visual input and sensory information from the vestibular labyrinths - abnormal central processing of vestibular input (brainstem vestibular nuclei / cerebellum) Rotational Swaying Rocking Tilting Translational
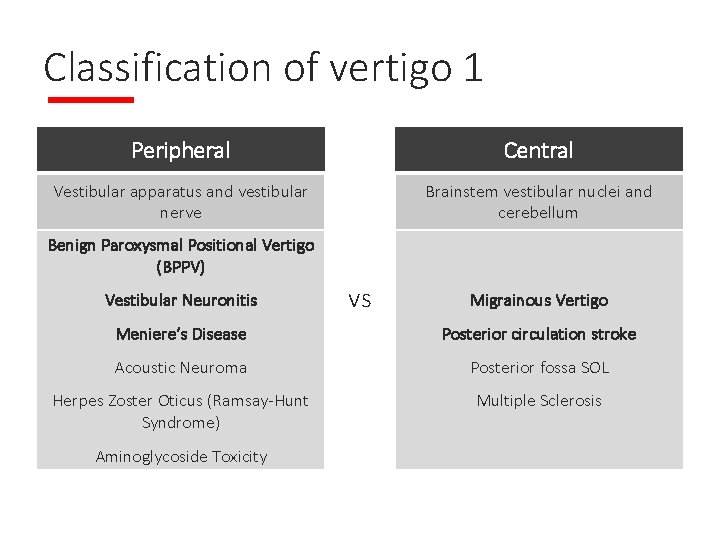
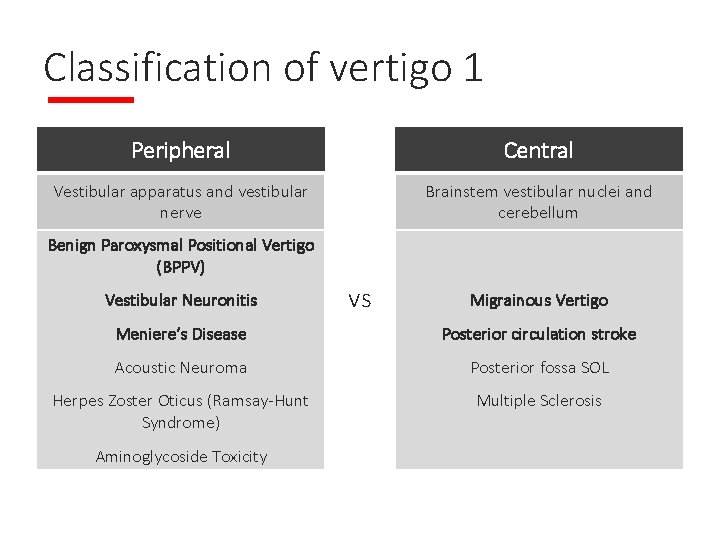
Classification of vertigo 1 Peripheral Central Vestibular apparatus and vestibular nerve Brainstem vestibular nuclei and cerebellum Benign Paroxysmal Positional Vertigo (BPPV) Vestibular Neuronitis vs Migrainous Vertigo Meniere’s Disease Posterior circulation stroke Acoustic Neuroma Posterior fossa SOL Herpes Zoster Oticus (Ramsay-Hunt Syndrome) Multiple Sclerosis Aminoglycoside Toxicity
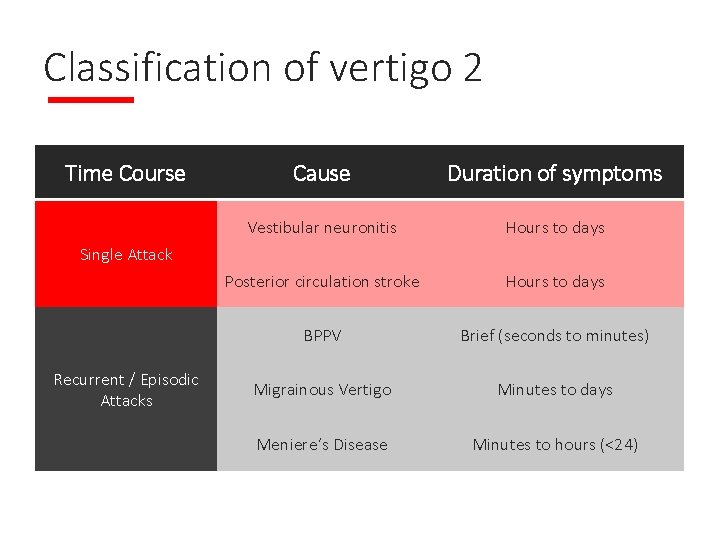
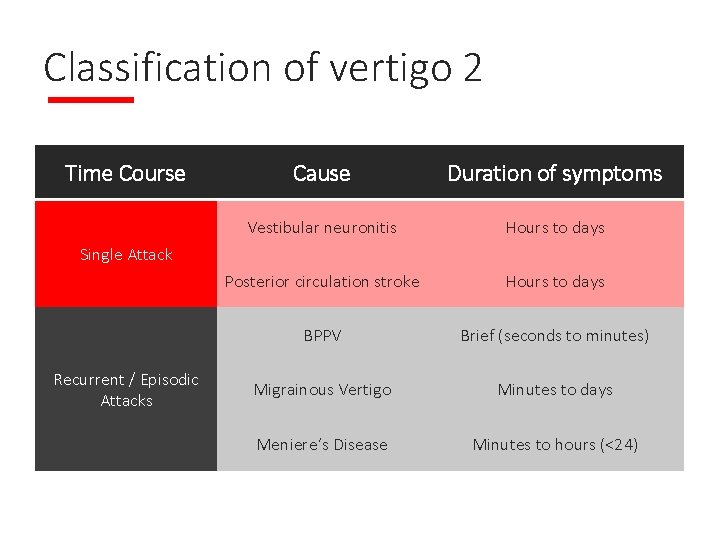
Classification of vertigo 2 Time Course Cause Duration of symptoms Vestibular neuronitis Hours to days Posterior circulation stroke Hours to days BPPV Brief (seconds to minutes) Migrainous Vertigo Minutes to days Meniere’s Disease Minutes to hours (<24) Single Attack Recurrent / Episodic Attacks
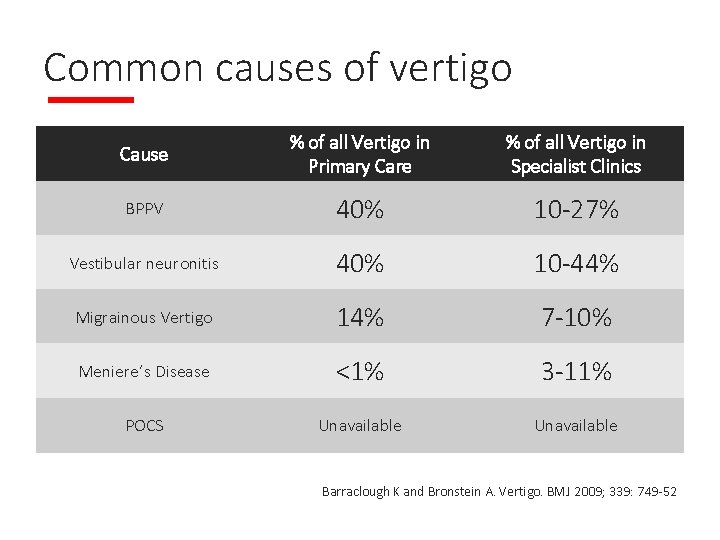
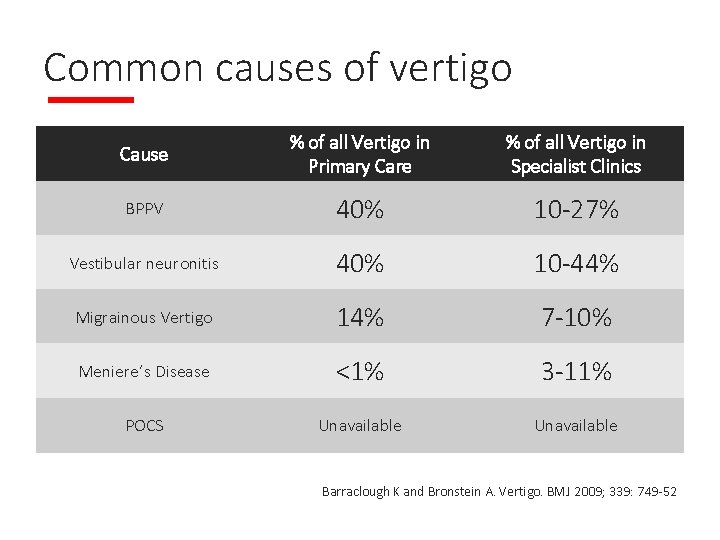
Common causes of vertigo Cause % of all Vertigo in Primary Care % of all Vertigo in Specialist Clinics BPPV 40% 10 -27% Vestibular neuronitis 40% 10 -44% Migrainous Vertigo 14% 7 -10% Meniere’s Disease <1% 3 -11% POCS Unavailable Barraclough K and Bronstein A. Vertigo. BMJ 2009; 339: 749 -52
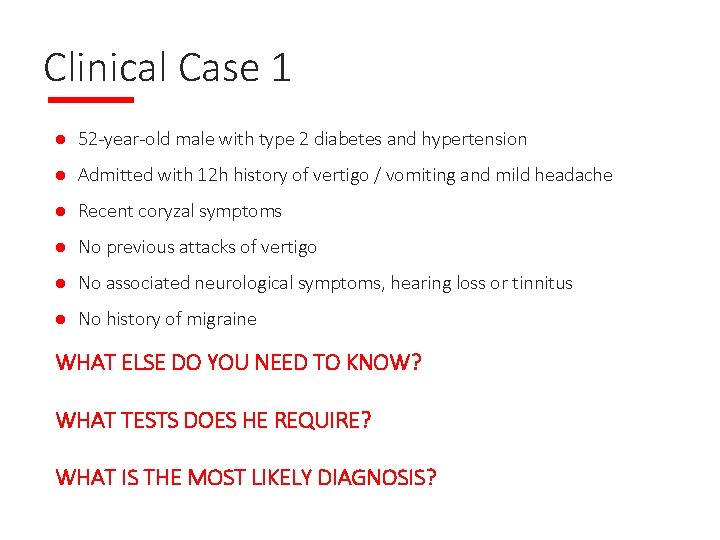
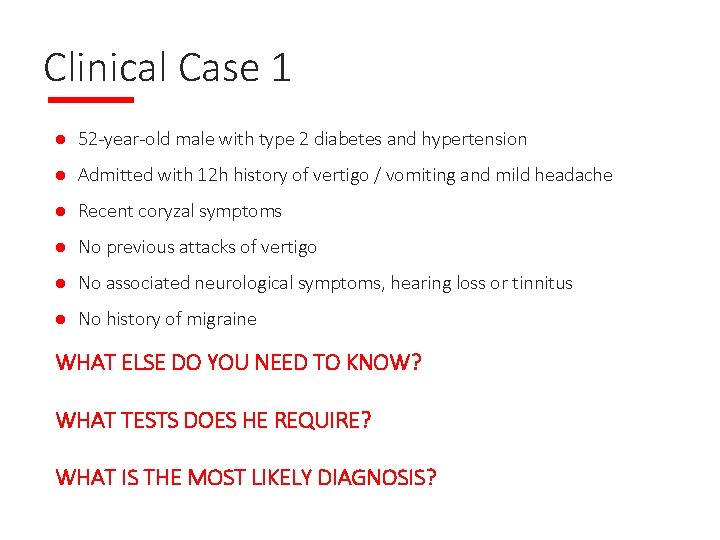
Clinical Case 1 l 52 -year-old male with type 2 diabetes and hypertension l Admitted with 12 h history of vertigo / vomiting and mild headache l Recent coryzal symptoms l No previous attacks of vertigo l No associated neurological symptoms, hearing loss or tinnitus l No history of migraine WHAT ELSE DO YOU NEED TO KNOW? WHAT TESTS DOES HE REQUIRE? WHAT IS THE MOST LIKELY DIAGNOSIS?
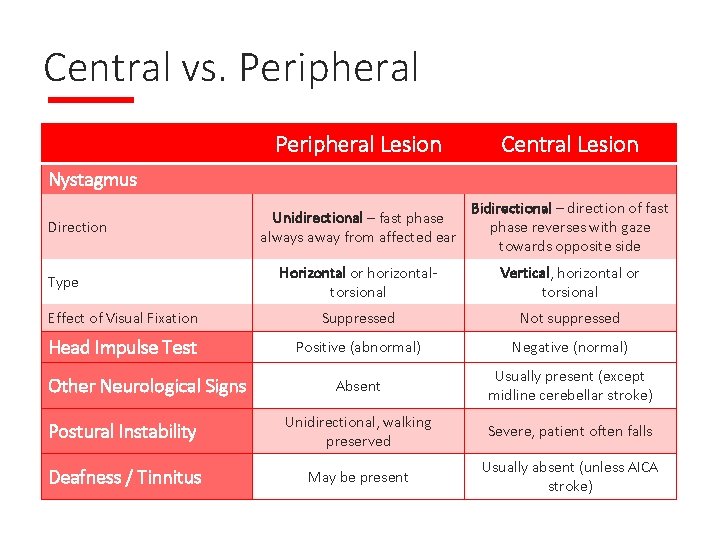
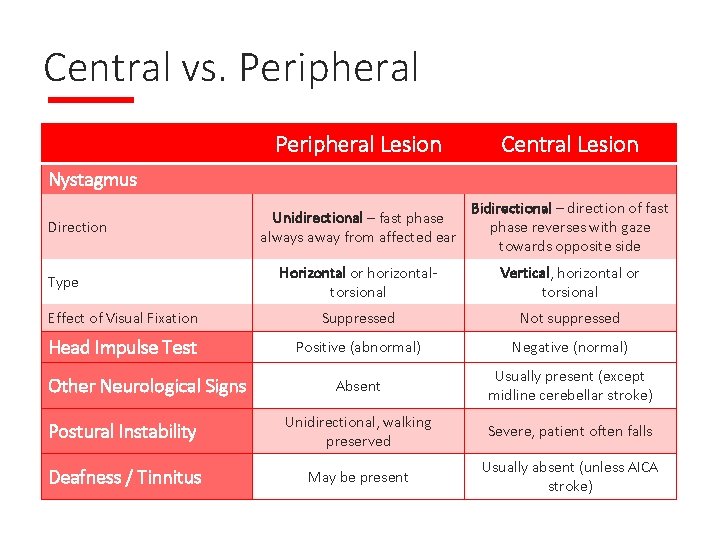
Central vs. Peripheral Lesion Central Lesion Unidirectional – fast phase always away from affected ear Bidirectional – direction of fast phase reverses with gaze towards opposite side Horizontal or horizontaltorsional Vertical, horizontal or torsional Effect of Visual Fixation Suppressed Not suppressed Head Impulse Test Positive (abnormal) Negative (normal) Absent Usually present (except midline cerebellar stroke) Postural Instability Unidirectional, walking preserved Severe, patient often falls Deafness / Tinnitus May be present Usually absent (unless AICA stroke) Nystagmus Direction Type Other Neurological Signs
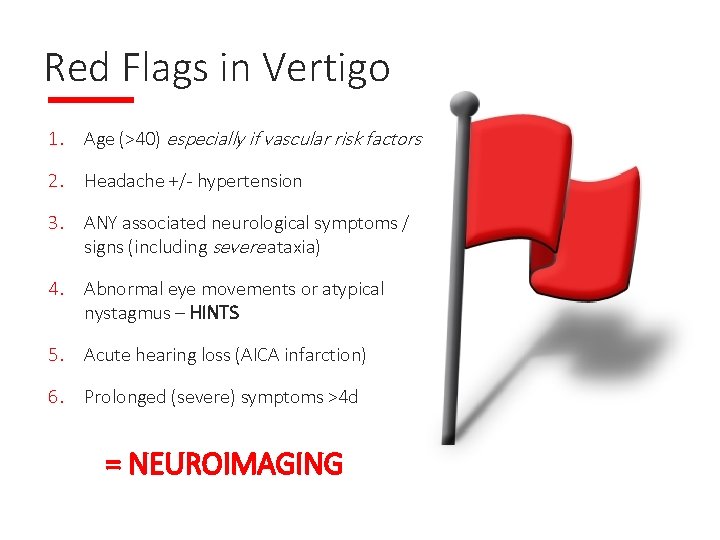
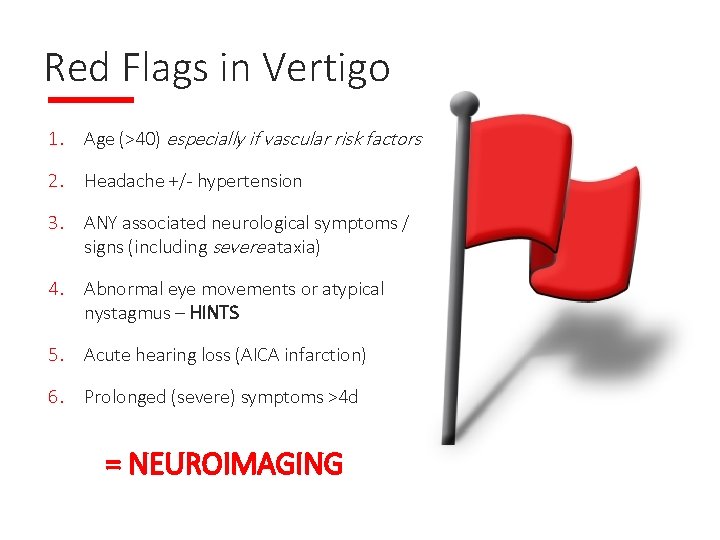
Red Flags in Vertigo 1. Age (>40) especially if vascular risk factors 2. Headache +/- hypertension 3. ANY associated neurological symptoms / signs (including severe ataxia) 4. Abnormal eye movements or atypical nystagmus – HINTS 5. Acute hearing loss (AICA infarction) 6. Prolonged (severe) symptoms >4 d = NEUROIMAGING
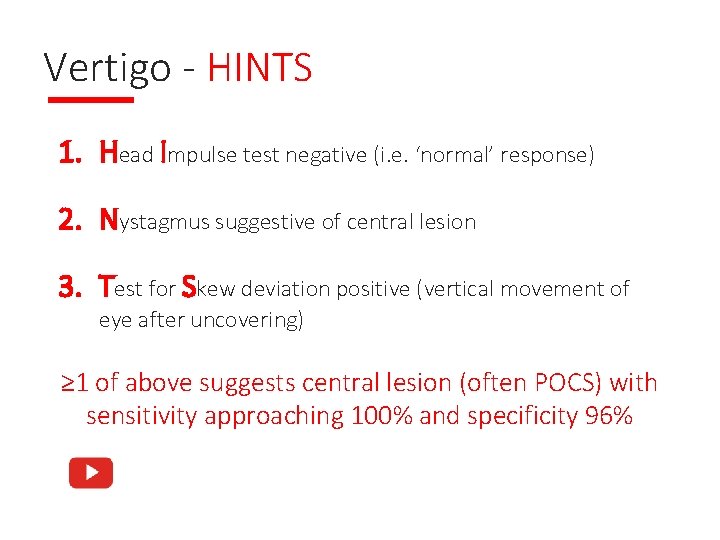
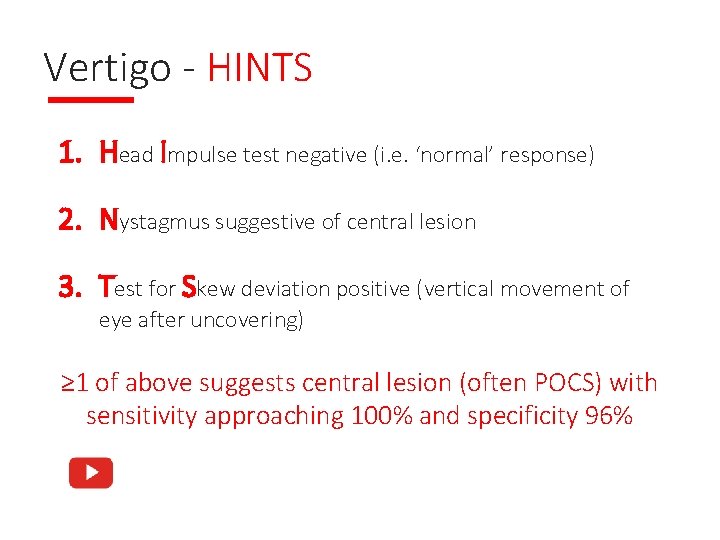
Vertigo - HINTS 1. Head Impulse test negative (i. e. ‘normal’ response) 2. Nystagmus suggestive of central lesion 3. Test for Skew deviation positive (vertical movement of eye after uncovering) ≥ 1 of above suggests central lesion (often POCS) with sensitivity approaching 100% and specificity 96%
BPPV l affects almost 1: 10 older people, women 2 x men l displacement of otoconia (otoliths) from utricle / saccule into semicircular canals l usually idiopathic (age-related vestibular membrane degeneration) l may occur after minor head trauma or other vestibular insults l brief episodes of vertigo ≤ 60 seconds l precipitated by certain head movements - looking upwards (posterior canalithiasis) e. g. hanging out the washing - turning over in bed (horizontal canalithiasis) l recurrent episodes over weeks to months l more persistent dysequilibrium may occur in chronic cases
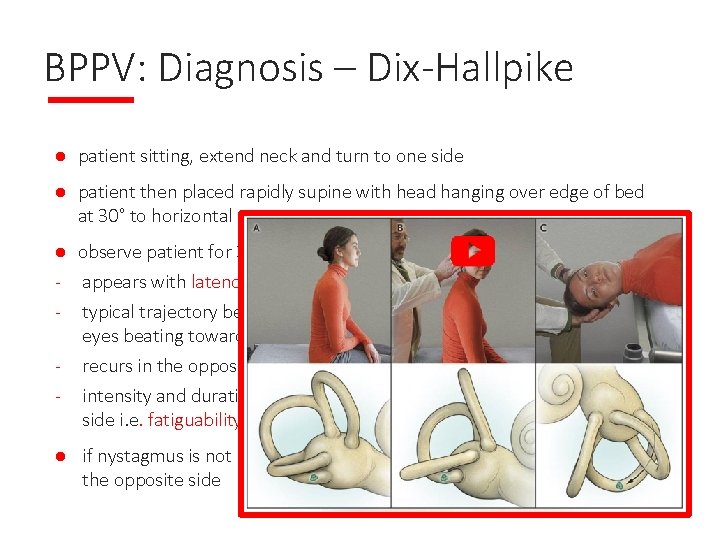
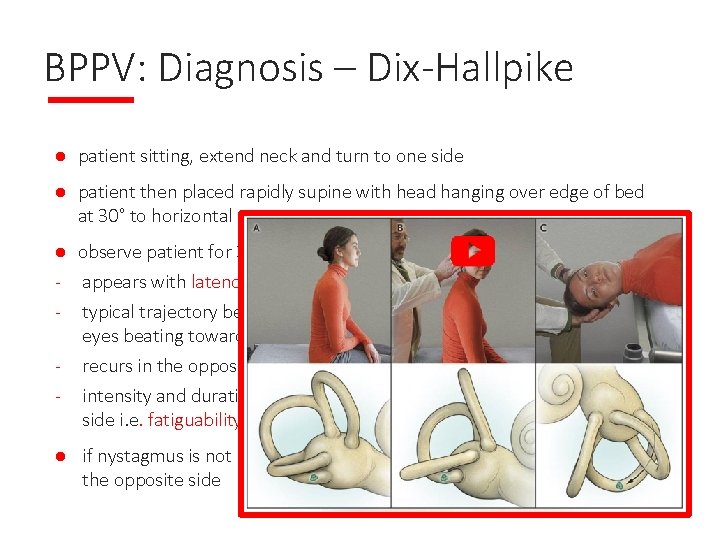
BPPV: Diagnosis – Dix-Hallpike l patient sitting, extend neck and turn to one side l patient then placed rapidly supine with head hanging over edge of bed at 30° to horizontal l observe patient for 30 seconds for nystagmus appears with latency of a few seconds and lasts < 30 seconds typical trajectory beating upward and torsionally, with upper poles of eyes beating toward the ground recurs in the opposite direction on sitting the patient up intensity and duration decreases with each repetition to the provoked side i. e. fatiguability l if nystagmus is not provoked, repeat manoeuvre with head turned to the opposite side
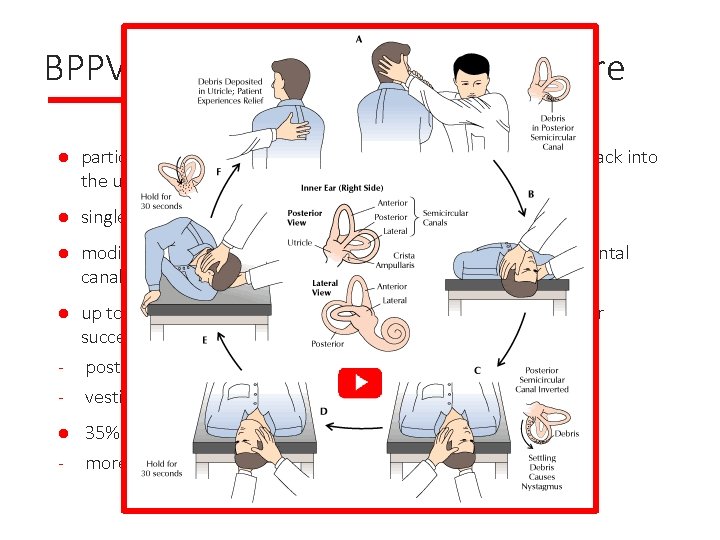
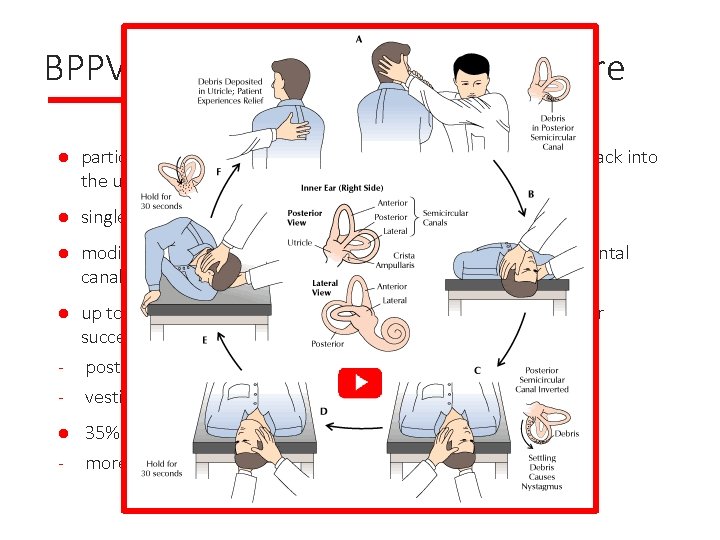
BPPV Treatment – Epley Manouevre l particle repositioning manoeuvre - encourages debris to move back into the utricular cavity l single manoeuvre effective in 85% of patients l modified manoeuvres (Lempert roll, Gufoni) for anterior / horizontal canalithiasis up to 1/3 have vague imbalance and dizziness for 2 -3 weeks after successful treatment - postural restriction (cervical collar / upright posture) for 2 days? - vestibular suppressants for 1 week? l l - 35% recurrence rate at 5 years more likely if older with chronic symptoms
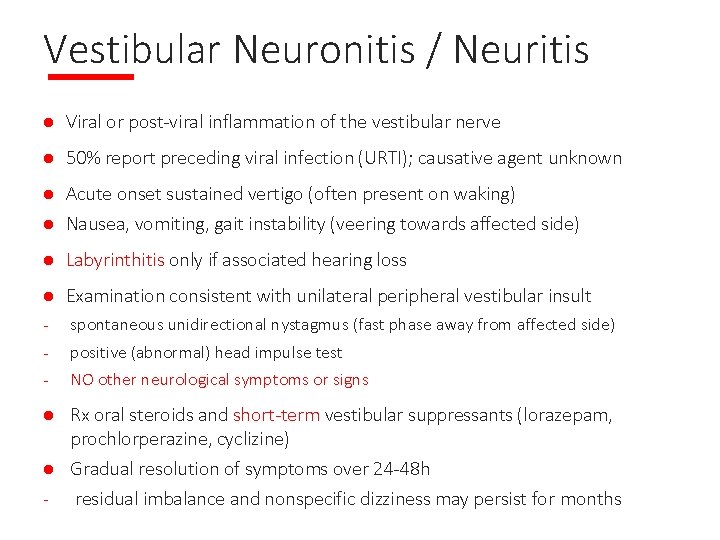
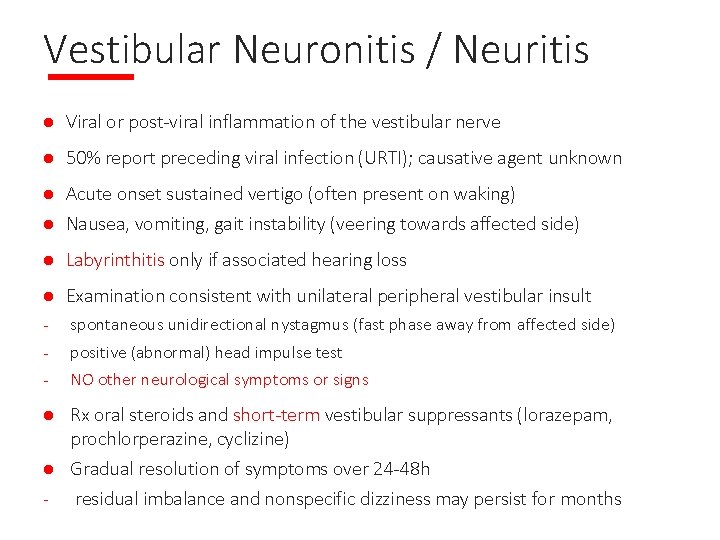
Vestibular Neuronitis / Neuritis l Viral or post-viral inflammation of the vestibular nerve l 50% report preceding viral infection (URTI); causative agent unknown Acute onset sustained vertigo (often present on waking) l Nausea, vomiting, gait instability (veering towards affected side) l l Labyrinthitis only if associated hearing loss l Examination consistent with unilateral peripheral vestibular insult - spontaneous unidirectional nystagmus (fast phase away from affected side) - positive (abnormal) head impulse test - NO other neurological symptoms or signs Rx oral steroids and short-term vestibular suppressants (lorazepam, prochlorperazine, cyclizine) l Gradual resolution of symptoms over 24 -48 h residual imbalance and nonspecific dizziness may persist for months l
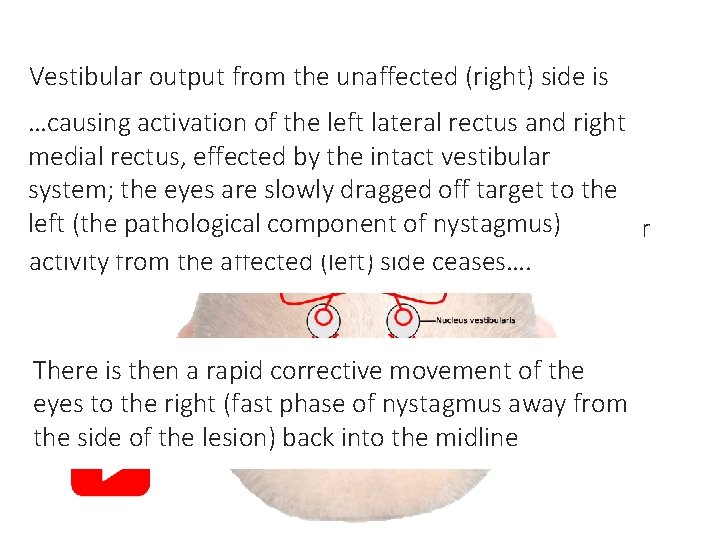
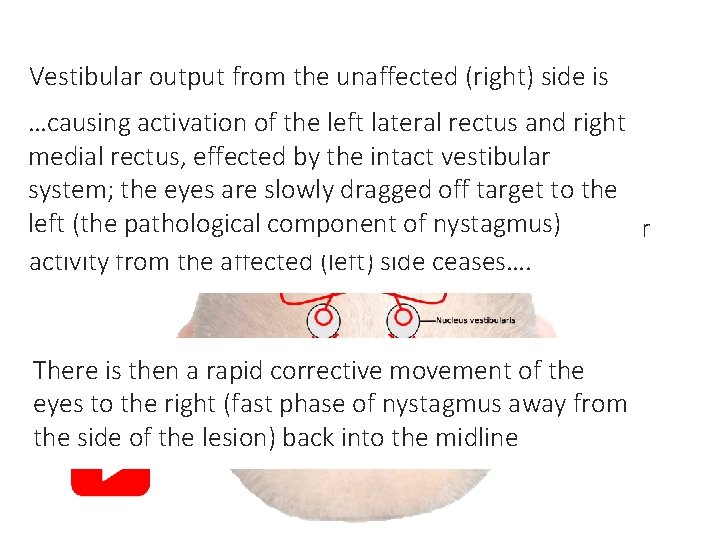
In the resting state, low-level baseline activity fromis Vestibular output from the unaffected (right) side both vestibular systems stimulates medial and lateral now unopposed and the brain misinterprets this as if …causing activation of the left lateral rectus and right recti on both sides equally, maintaining forward gaze the head is turning towards the right… medial rectus, effected by the intact vestibular system; the eyes are slowly dragged off target to the left pathological component of nystagmus) With(the a unilateral peripheral vestibular lesion, vestibular activity from the affected (left) side ceases…. There is then a rapid corrective movement of the eyes to the right (fast phase of nystagmus away from the side of the lesion) back into the midline
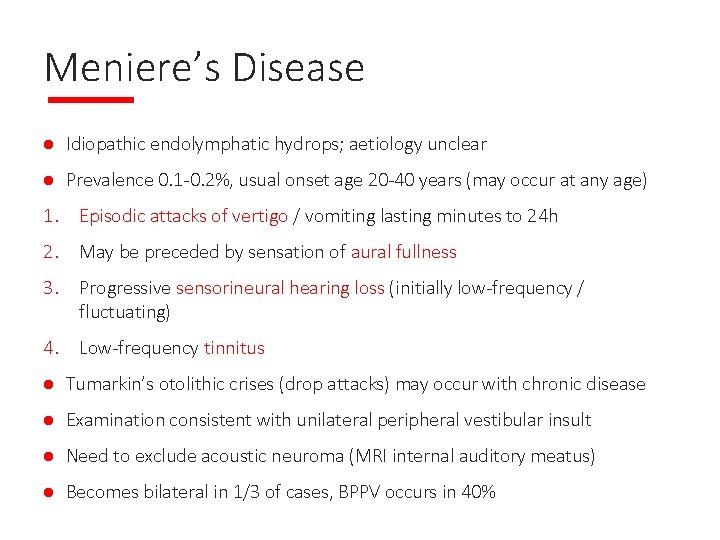
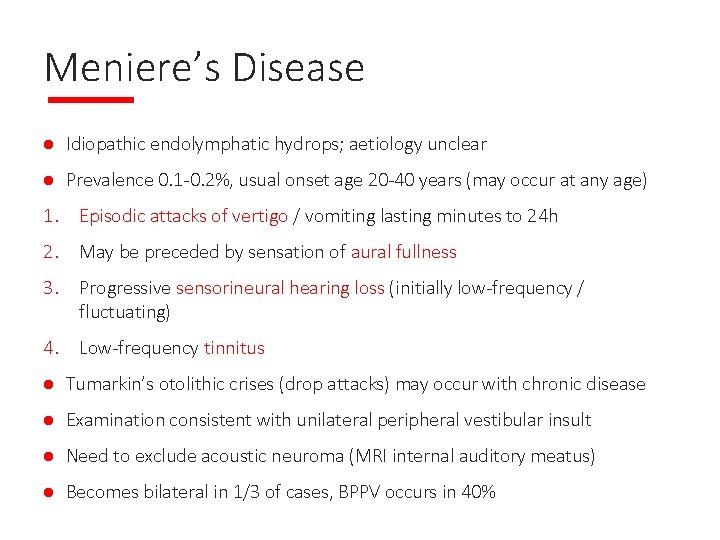
Meniere’s Disease l Idiopathic endolymphatic hydrops; aetiology unclear l Prevalence 0. 1 -0. 2%, usual onset age 20 -40 years (may occur at any age) 1. Episodic attacks of vertigo / vomiting lasting minutes to 24 h 2. May be preceded by sensation of aural fullness 3. Progressive sensorineural hearing loss (initially low-frequency / fluctuating) 4. Low-frequency tinnitus l Tumarkin’s otolithic crises (drop attacks) may occur with chronic disease l Examination consistent with unilateral peripheral vestibular insult l Need to exclude acoustic neuroma (MRI internal auditory meatus) l Becomes bilateral in 1/3 of cases, BPPV occurs in 40%
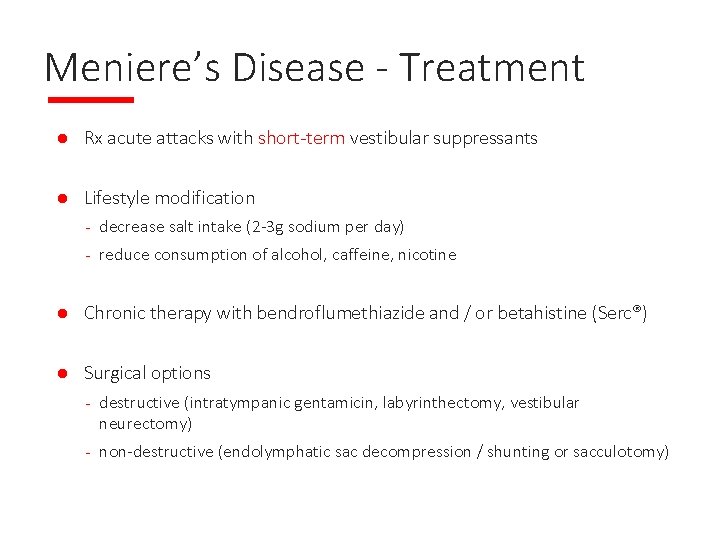
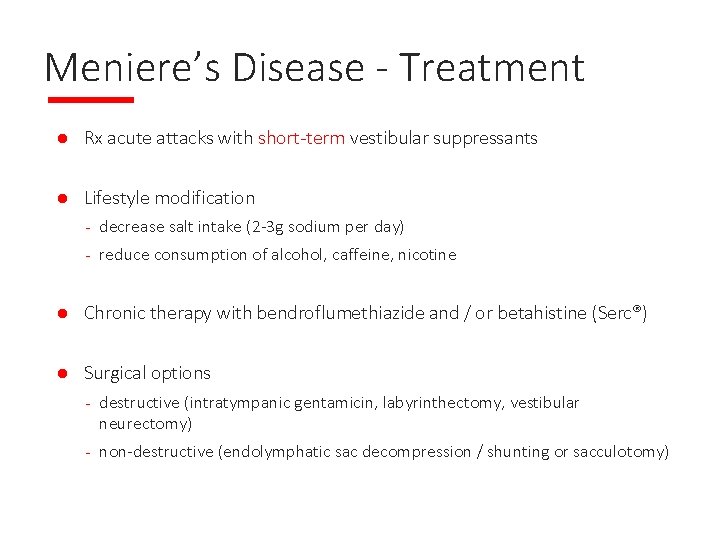
Meniere’s Disease - Treatment l Rx acute attacks with short-term vestibular suppressants l Lifestyle modification - decrease salt intake (2 -3 g sodium per day) - reduce consumption of alcohol, caffeine, nicotine l Chronic therapy with bendroflumethiazide and / or betahistine (Serc®) l Surgical options - destructive (intratympanic gentamicin, labyrinthectomy, vestibular neurectomy) - non-destructive (endolymphatic sac decompression / shunting or sacculotomy)
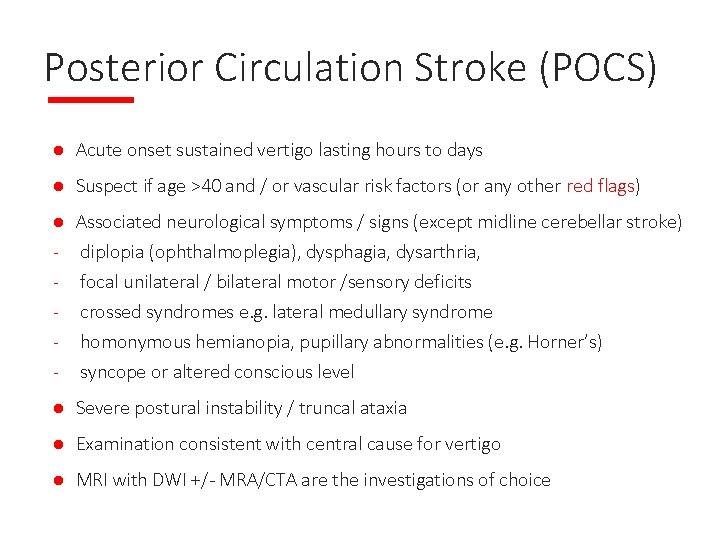
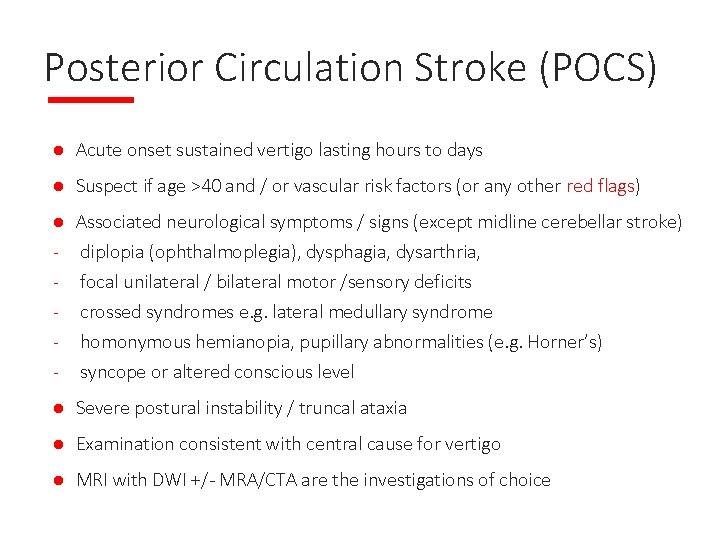
Posterior Circulation Stroke (POCS) l Acute onset sustained vertigo lasting hours to days l Suspect if age >40 and / or vascular risk factors (or any other red flags) l - Associated neurological symptoms / signs (except midline cerebellar stroke) diplopia (ophthalmoplegia), dysphagia, dysarthria, focal unilateral / bilateral motor /sensory deficits crossed syndromes e. g. lateral medullary syndrome homonymous hemianopia, pupillary abnormalities (e. g. Horner’s) syncope or altered conscious level l Severe postural instability / truncal ataxia l Examination consistent with central cause for vertigo l MRI with DWI +/- MRA/CTA are the investigations of choice -
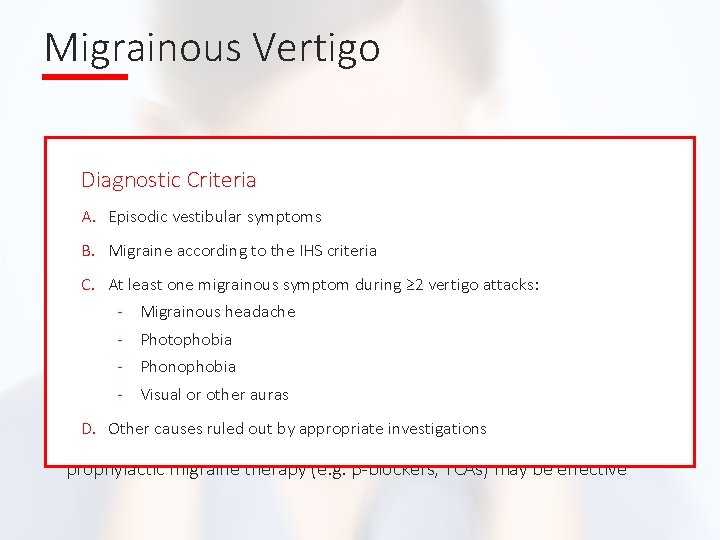
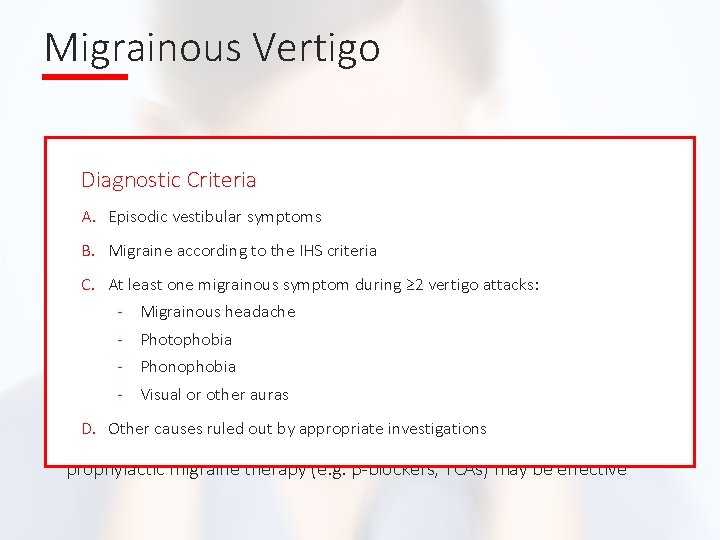
Migrainous Vertigo l aka vestibular migraine (NOT the same as basilar migraine) l higher incidence of vertigo, travel-sickness, BPPV and Meniere’s in A. Episodic vestibular symptoms migraineurs l B. Migraine according to thewith IHS acriteria episodic vertigo in patients history of migraine or with other clinical features of migraine C. At least one migrainous symptom during ≥ 2 vertigo attacks: l - Migrainous headache episodes last seconds to days (≤ 72 h) and may recur several times per day or only a -few. Photophobia times every year Diagnostic Criteria l - neurological Phonophobia symptoms, headache often absent no other l no confirmatory tests (diagnosis of exclusion) l acute migraine treatments (e. g. triptans), vestibular suppressants and prophylactic migraine therapy (e. g. β-blockers, TCAs) may be effective - Visual or other auras D. Other causes ruled out by appropriate investigations
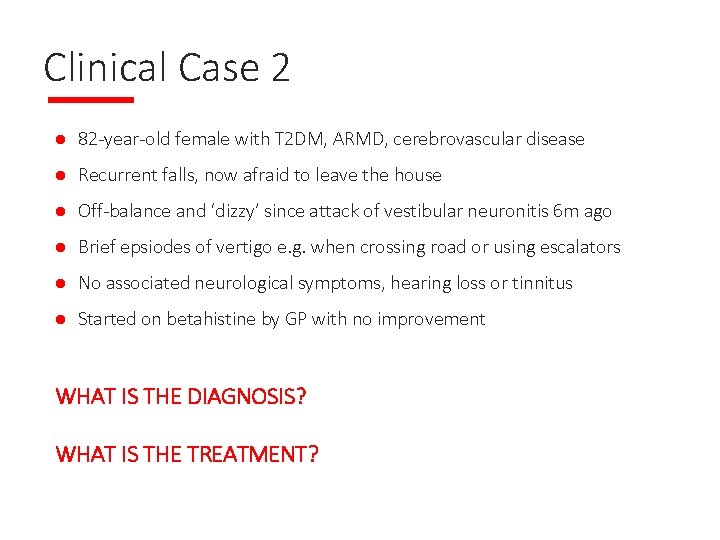
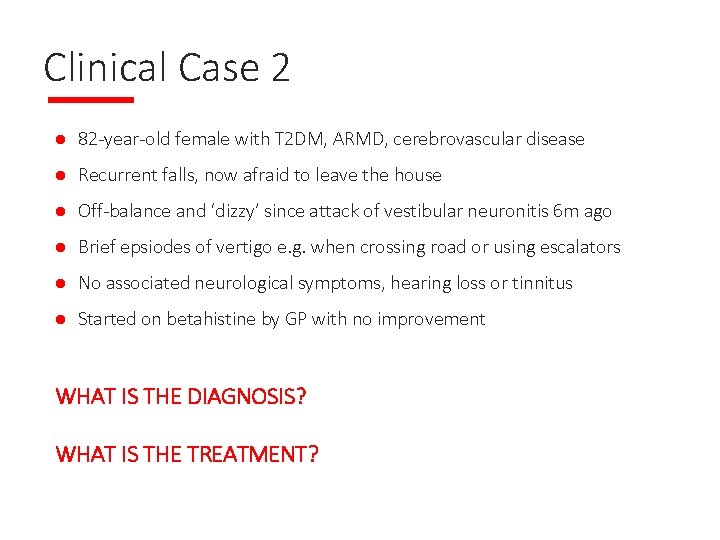
Clinical Case 2 l 82 -year-old female with T 2 DM, ARMD, cerebrovascular disease l Recurrent falls, now afraid to leave the house l Off-balance and ‘dizzy’ since attack of vestibular neuronitis 6 m ago l Brief epsiodes of vertigo e. g. when crossing road or using escalators l No associated neurological symptoms, hearing loss or tinnitus l Started on betahistine by GP with no improvement WHAT IS THE DIAGNOSIS? WHAT IS THE TREATMENT?

Uncompensated Vestibular Hypofunction Vestibular sedatives Cerebral Restriction Pathology an acute unilateral peripheral of activityvestibular insult l Usually occurs following - Vestibular neuronitis, Meniere’s disease, BPPV Ototoxic medication, trauma, surgery l Cognitive Failure (or absence) of central compensatory recalibration mechanisms Peripheral - Impairment neuropathy Failure of l Persistent imbalance (dysequilibrium) centraland vague dizziness compensation Brief attacks of vertigo may occur - With sudden head movements Poly- environments - In visually ‘rich’ l Anxiety and fear pharmacy l Stop vestibular sedatives and optimize other sensory inputs l Vestibular Rehabilitation. Visual Therapy (VRT) Abnormal is the cornerstone of Rx impairment posturing
Assessment of Vertigo: History l Clarify exactly what patient means by ‘dizziness’ l Previous episodes , duration / frequency / triggers, normal in between attacks? l - Associated symptoms Recent viral URTI you say ‘dizzy’ do you mean light. When Neurological headed, off-balance or are things moving Tinnitus / hearing loss around like you’ve just stepped off a Migrainous symptoms l PMHx esp. vascular risk factors, migraine, ENT l DHx esp. exposure to ototoxics, prolonged use of vestibular sedatives - roundabout?
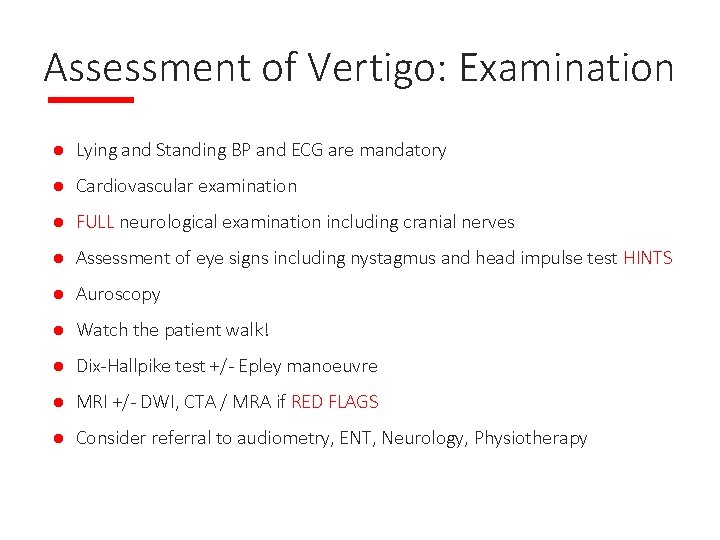
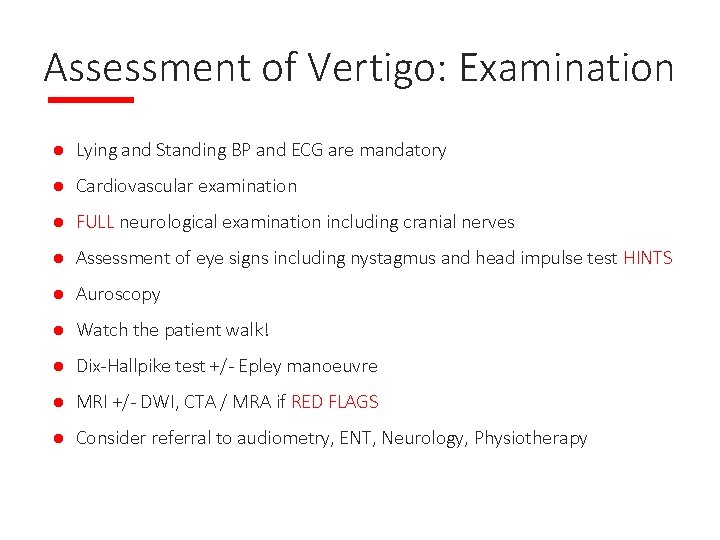
Assessment of Vertigo: Examination l Lying and Standing BP and ECG are mandatory l Cardiovascular examination l FULL neurological examination including cranial nerves l Assessment of eye signs including nystagmus and head impulse test HINTS l Auroscopy l Watch the patient walk! l Dix-Hallpike test +/- Epley manoeuvre l MRI +/- DWI, CTA / MRA if RED FLAGS l Consider referral to audiometry, ENT, Neurology, Physiotherapy
Questions?