Diuretics 2011 10 19 R 3 Introduction among






- Slides: 26
Diuretics 2011. 10. 19 R 3 주혜영
Introduction § among the most commonly used drugs § diminish sodium reabsorption at different sites in the nephron → increase urinary sodium and water losses → negative fluid balance § in the treatment of edematous states(heart failure, cirrhosis, nephrotic syndrome, renal failure), hypertension, electrolyte imbalance
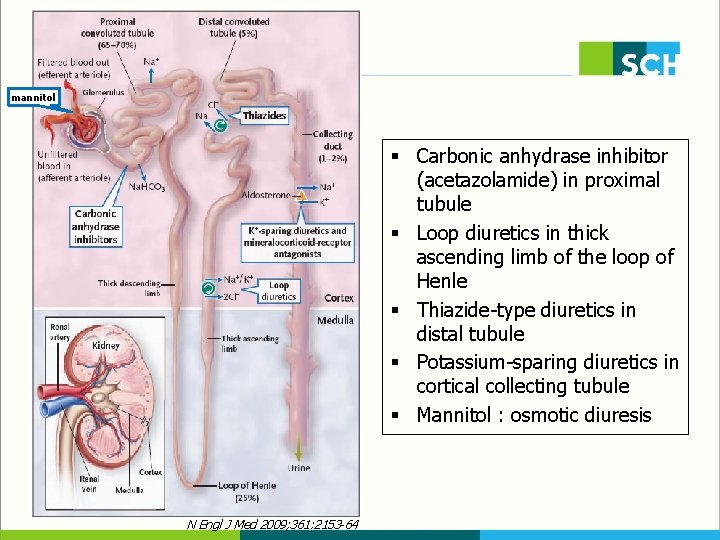
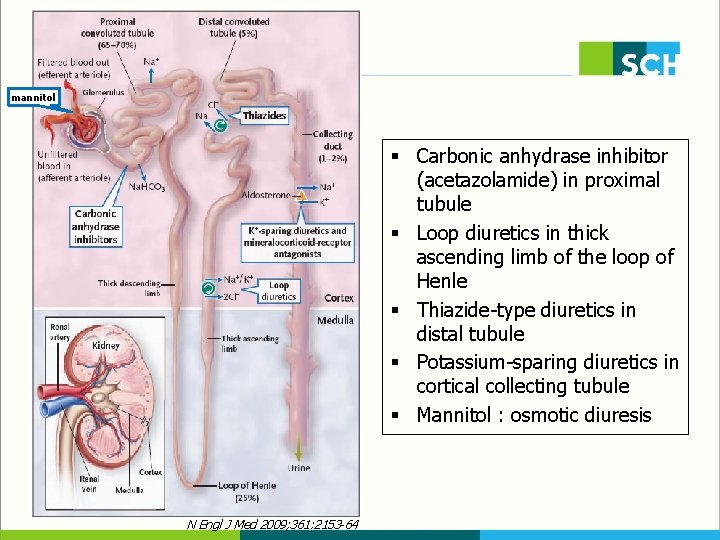
mannitol § Carbonic anhydrase inhibitor (acetazolamide) in proximal tubule § Loop diuretics in thick ascending limb of the loop of Henle § Thiazide-type diuretics in distal tubule § Potassium-sparing diuretics in cortical collecting tubule § Mannitol : osmotic diuresis N Engl J Med 2009; 361: 2153 -64
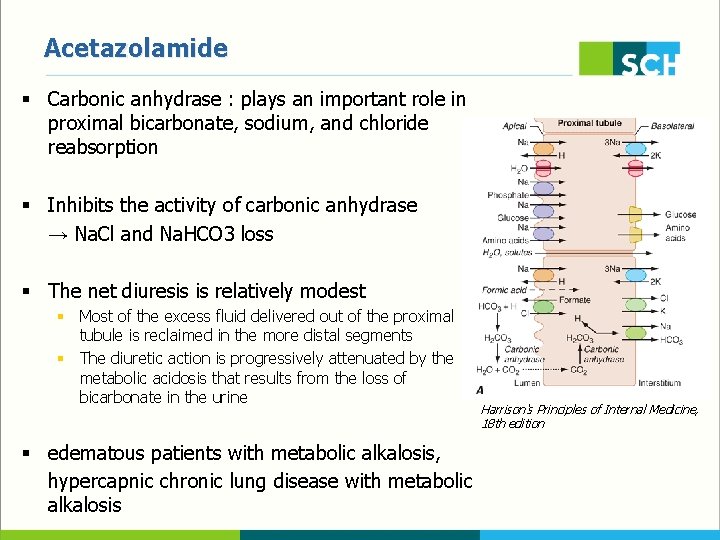
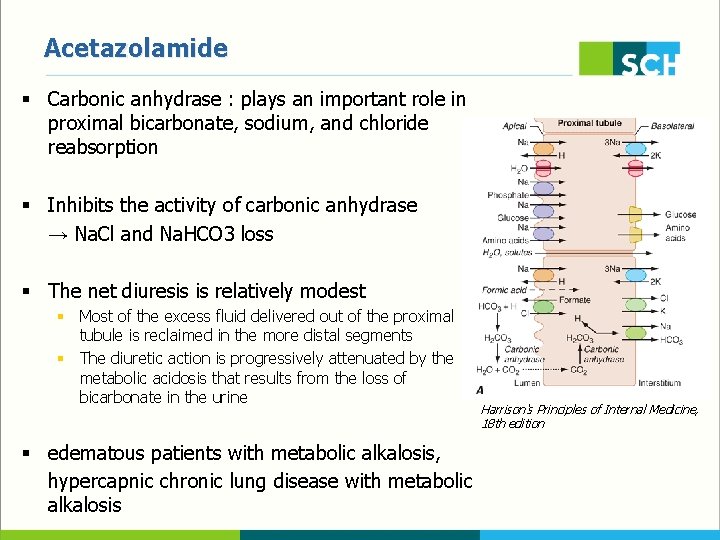
Acetazolamide § Carbonic anhydrase : plays an important role in proximal bicarbonate, sodium, and chloride reabsorption § Inhibits the activity of carbonic anhydrase → Na. Cl and Na. HCO 3 loss § The net diuresis is relatively modest § Most of the excess fluid delivered out of the proximal tubule is reclaimed in the more distal segments § The diuretic action is progressively attenuated by the metabolic acidosis that results from the loss of bicarbonate in the urine § edematous patients with metabolic alkalosis, hypercapnic chronic lung disease with metabolic alkalosis Harrison's Principles of Internal Medicine, 18 th edition
Mannitol § a nonreabsorbable sugar alcohol § filtered by glomerulus but not reabsorbed by the proximal tubule → osmotic diuresis § half-life : 1 to 36 hr(may be retained in renal failure) § preferential water diuresis → water defecit, Hypernatremia, plasma osmolarity ↑ § treatment of cerebral edema, elevated ICP

Loop diuretics § the most potent diuretics (lead to the excretion of up to 20~25% of filtered Na) § furosemide, bumetanide, torsemide, ethacrynic acid (Sulfonamide derivatives except for ethacrynic acid) § Inhibits the Na-K-2 Cl cotransporter (compete for the chloride site on this carrier) Harrison's Principles of Internal Medicine, § reabsorption of Ca in the loop of Henle 18 th edition : passive, driven by the electrochemical gradient created by Na. Cl transport, paracellular pathway § → increase Ca excretion : treatment of hypercalcemia
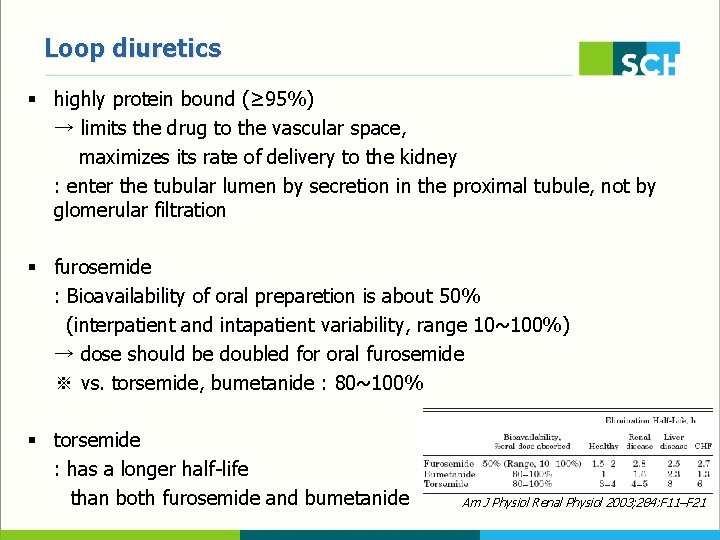
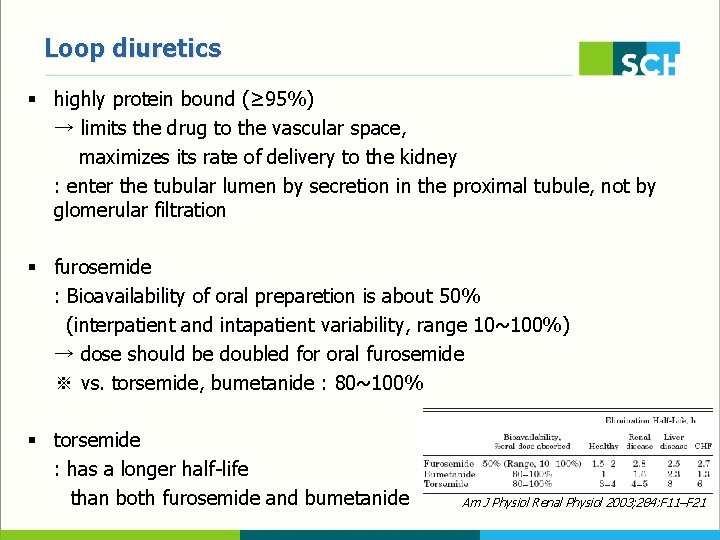
Loop diuretics § highly protein bound (≥ 95%) → limits the drug to the vascular space, maximizes its rate of delivery to the kidney : enter the tubular lumen by secretion in the proximal tubule, not by glomerular filtration § furosemide : Bioavailability of oral preparetion is about 50% (interpatient and intapatient variability, range 10~100%) → dose should be doubled for oral furosemide ※ vs. torsemide, bumetanide : 80~100% § torsemide : has a longer half-life than both furosemide and bumetanide Am J Physiol Renal Physiol 2003; 284: F 11–F 21
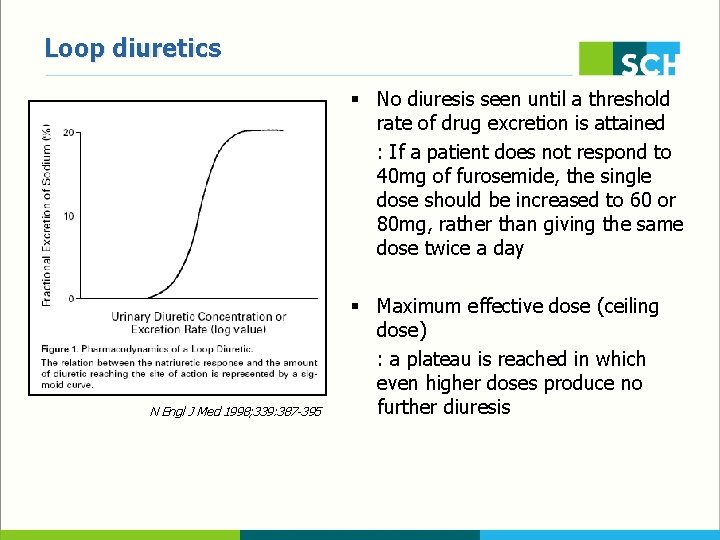
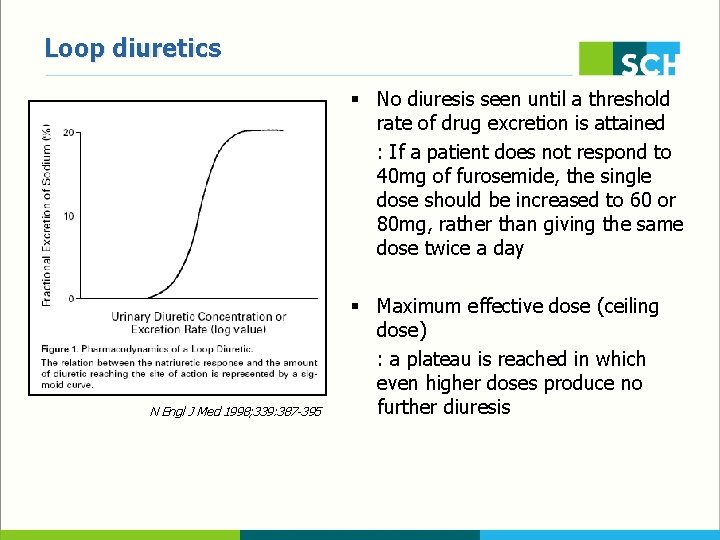
Loop diuretics § No diuresis seen until a threshold rate of drug excretion is attained : If a patient does not respond to 40 mg of furosemide, the single dose should be increased to 60 or 80 mg, rather than giving the same dose twice a day N Engl J Med 1998; 339: 387 -395 § Maximum effective dose (ceiling dose) : a plateau is reached in which even higher doses produce no further diuresis

Loop diuretics § The maximum effective diuretic dose is higher in patients with heart failure, cirrhosis, or renal failure : d/t decreased renal perfusion (and therefore decreased drug delivery to the kidney), diminished proximal secretion (d/t the retention of competing anions in renal failure), renal vasoconstriction(cirrhosis), and enhanced activity of sodium-retaining forces (such as the RAAS) N Engl J Med 1998; 339: 387 -395
Loop diuretics § Diuresis-related : hypokalemia, metabolic alkalosis, signs of decreased tissue perfusion (hypotension, BUN↑, Cr↑, hyperuricemia, hyponatremia) § Hypersensitivity reaction § rash, acute interstitial nephritis(rarely) § similar to those produced by other sulfonamide drugs § Ototoxicity § inhibition of an isoform of this cotransporter in the inner ear § decreased hearing, tinnitus, deafness(may be permanent) § occur with high-dose IV therapy

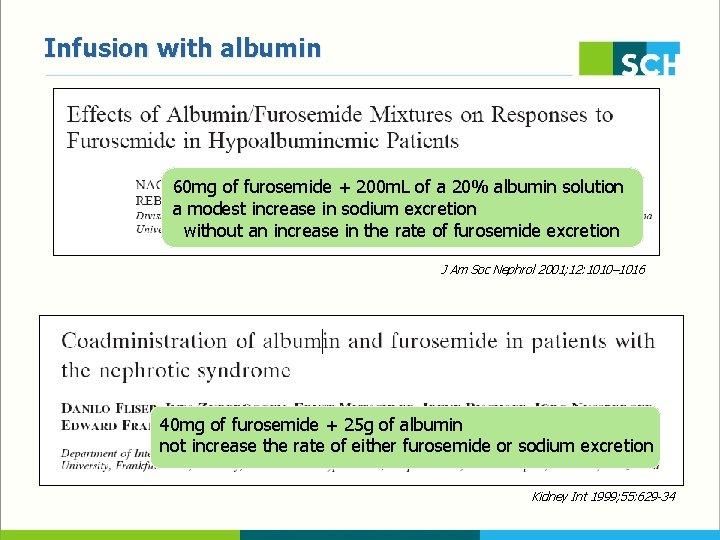
Refractory to loop diuretics § High salt intake : 24 hour urine Na > 100 meq/day → adequate diuretic response & high salt intake § Infusion with albumin § administration of 40 to 80 mg of furosemide added to 6. 25 to 12. 5 g of salt-poor albumin § increasing diuretic delivery to the kidney by keeping furosemide within the vascular space § But, lack of efficacy. . § Posture : supine position § Renal perfusion ↑ → urinary diuretic delivery ↑ § Upright position : increases in plasma norepinephrine, renin, aldosterone
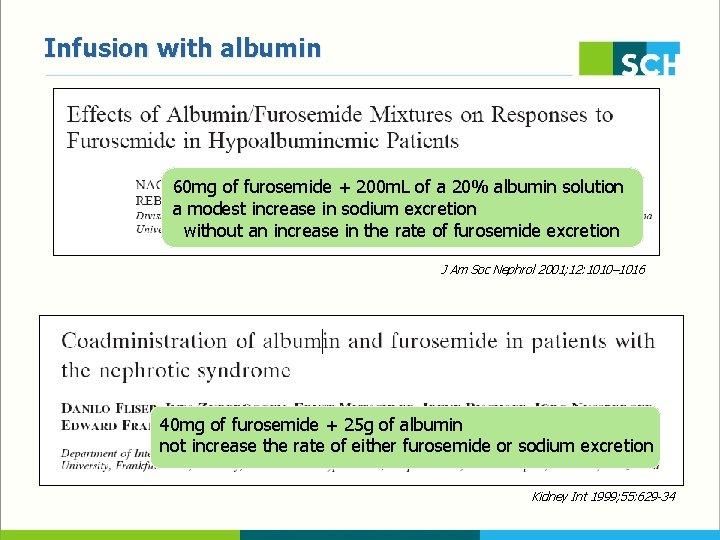
Infusion with albumin 60 mg of furosemide + 200 m. L of a 20% albumin solution a modest increase in sodium excretion without an increase in the rate of furosemide excretion J Am Soc Nephrol 2001; 12: 1010– 1016 40 mg of furosemide + 25 g of albumin not increase the rate of either furosemide or sodium excretion Kidney Int 1999; 55: 629 -34
Refractory to loop diuretics § continuous infusion § safer (less ototoxicity) and more effective than bolus injections § maintenance of an effective rate of drug excretion § bolus therapy results in higher initial serum concentrations and higher initial rates of urinary diuretic excretion than a continuous infusion ☞ continuous infusion should not be tried in patients who have not responded to the maximum bolus doses § Regimen - renal insufficiency : initial furosemide infusion rate of 20 mg/h, higher of 40 mg/h - reasonable renal function : initial infusion rate of 5 mg/h, higher of 10 mg/h § The literature has reports of higher infusion rates of up to 240 mg/h But, ototoxicity and other side effects → the addition of a thiazide-type diuretic or fluid removal via ultrafltration

Diuretic tolerance § a decrease in the response to a diuretic after the first dose § Short-term tolerance § initial reduction in extracellular fluid volume → decline in the drug level in plasma and tubular fluid to below the diuretic threshold § activation of the RAAS and the sympathetic nervous system § Long-term tolerance (diuretic braking phenomenon) § activation of the RAAS → circulating angiotensin II ↑ → promotes increased proximal sodium reabsorption § the up-regulation of sodium transporters downstream from the primary site of diuretic action § structural hypertrophy of distal nephron segments § Sodium restriction, repeated or higher doses, combinations of diuretics
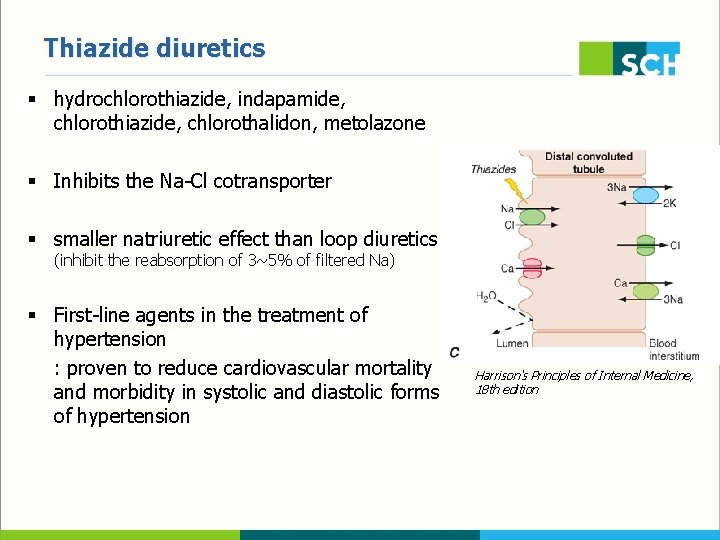
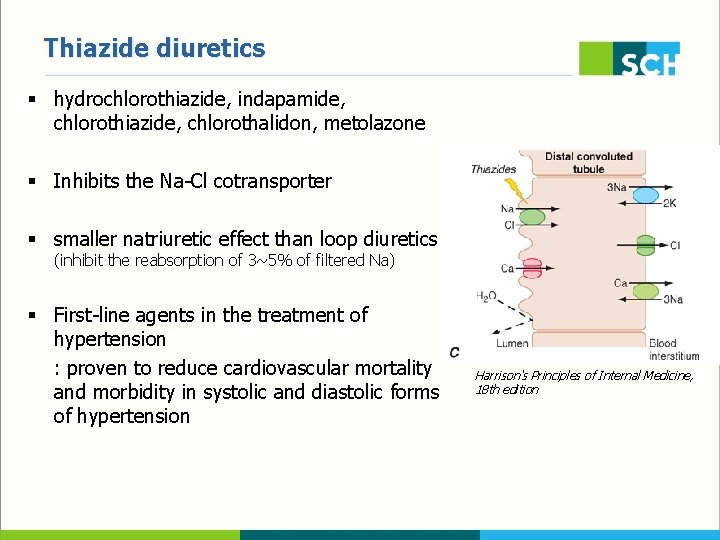
Thiazide diuretics § hydrochlorothiazide, indapamide, chlorothiazide, chlorothalidon, metolazone § Inhibits the Na-Cl cotransporter § smaller natriuretic effect than loop diuretics (inhibit the reabsorption of 3~5% of filtered Na) § First-line agents in the treatment of hypertension : proven to reduce cardiovascular mortality and morbidity in systolic and diastolic forms of hypertension Harrison's Principles of Internal Medicine, 18 th edition
Thiazide diuretics § ineffective at GFR <30 ml/min § Metolazone : efficacy in patients who have renal insufficiency § The distal tubule is the major site of active Ca reabsorption : thiazides increase the reabsorption of Ca → treatment of recurrent kidney stones d/t hypercalciuria
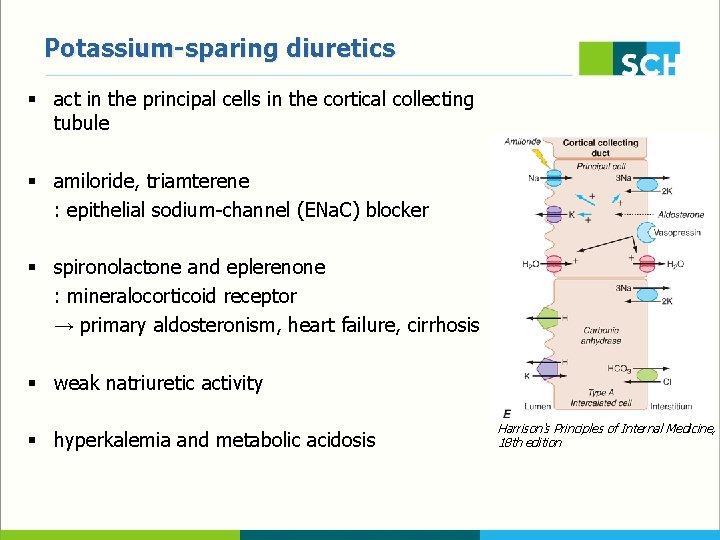
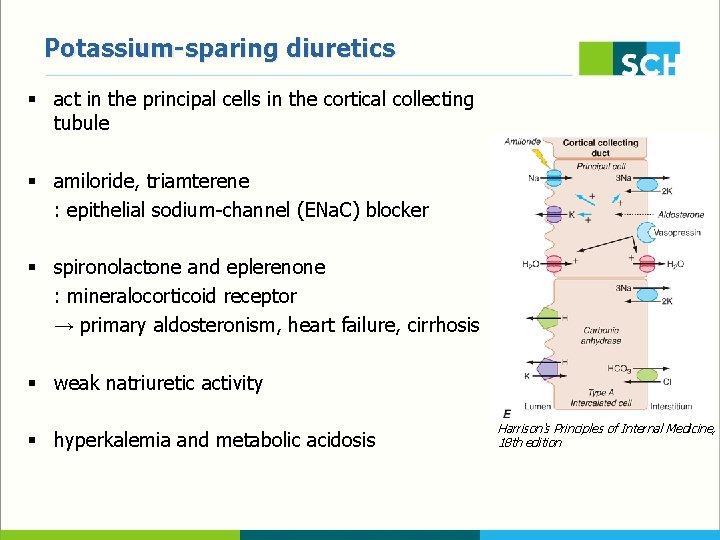
Potassium-sparing diuretics § act in the principal cells in the cortical collecting tubule § amiloride, triamterene : epithelial sodium-channel (ENa. C) blocker § spironolactone and eplerenone : mineralocorticoid receptor → primary aldosteronism, heart failure, cirrhosis § weak natriuretic activity § hyperkalemia and metabolic acidosis Harrison's Principles of Internal Medicine, 18 th edition

Potassium-sparing diuretics § Trimethoprim : can act as a potassium-sparing diuretic when given in high doses → nephrotoxicity, hyperkalemia § Eplerenone : more selective for aldosterone less endocrine side effects (eg, gynecomastia, menstrual abnormalities, impotence, and decreased libido)
Treatment of edema § Edema = a palpable swelling produced by expansion of the interstitial fluid volume § massive and generalized → anasarca § heart failure, cirrhosis, and the nephrotic syndrome, renal failure as well as local conditions (venous and lymphatic disease) § When diuretics are administered, the fluid that is lost initially comes from the intravascular space → venous pressure and capillary hydraulic pressure ↓ → restoration of the plasma volume by the mobilization of edema fluid into the vascular space
Treatment of edema § In heart failure or nephrotic syndrome : since most capillary beds are involved, the edema fluid can be mobilized rapidly → removal of ≥ 2~3 L of edema fluid in 24 hours § But, cirrhosis - ascites and no peripheral edema : the excess ascitic fluid can only be mobilized via the peritoneal capillaries → 300~500 m. L/day is the maximum amount that can be mobilized by most patients § If the diuresis proceeds more rapidly, the ascitic fluid will be unable to completely replenish the plasma volume → resulting in azotemia and possible precipitation of the hepatorenal syndrome
Treatment of edema § In venous insufficiency, lymphedema, or ascites due to peritoneal malignancy “ fluid removal → reduction in venous and intracapillary pressure → edema fluid to be mobilized and the plasma volume to be maintained ” ☞ not occurred § So, diuretics should be used with caution and monitoring of the serum creatinine monitored in such patients § The mainstays of therapy of lower extremity edema d/t venous insufficiency : leg elevation well-fitted, knee-high compression stockings
Use of diuretics in heart failure § Evaluation and optimization of volume status is an essential component of treatment in patients with HF § In contrast to ACEi, beta blockers, and aldosterone antagonist, limited outcomes data are available for diuretic therapy § 3 major manifestations of volume overload : pulmonary congestion, pph edema, and elevated JVP § combination of an oral loop diuretic and low sodium diet

Use of diuretics in heart failure § IV administration of loop diuretics is generally required for acute decompensation or severe disease § decreased intestinal perfusion § reduced intestinal motility § mucosal edema reduce the rate of diuretic absorption § bolus vs. continuous infusion high dose vs. low dose
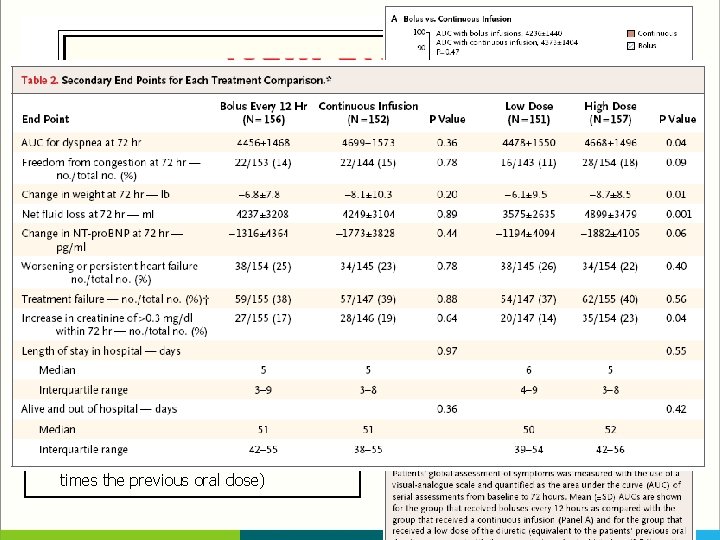
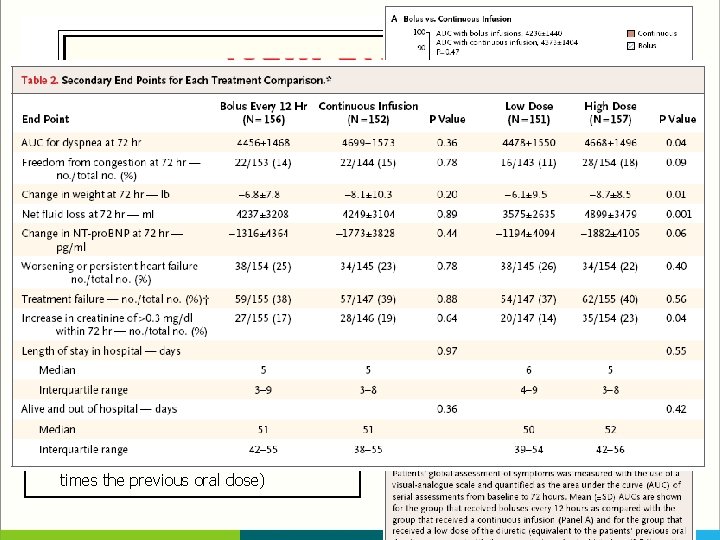
< Diuretic Optimization Strategies Evaluation (DOSE) trial > § 308 pts with acute decompensated heart failure § prospective, double-blind, randomized trial § bolus every 12 hours or continuous infusion § low dose (equivalent to the patient’s previous oral dose) or high dose (2. 5 times the previous oral dose)
Use of diuretics in heart failure § Daily assessment of patient weight - the most effective method for documenting effective diuresis : use the same scale, performed at the same time each day (in the morning, prior to eating, after voiding) § decrease in intracardiac filling pressure induced by the diuresis → lower the cardiac output → reduced tissue perfusion → unexplained rise in serum Cr (reflects a reduction in GFR) : worse prognosis § IV furosemide in acute pulmonary edema § venodilatory effect → cardiac filling pr ↓ → pulmonary congestion ↓ § renal production of PG ↑
Reference § § § N Engl J Med 2009; 361: 2153 -64 N Engl J Med 1998; 339: 387 -395 Am J Physiol Renal Physiol 2003; 284: F 11 -F 21 N Engl J Med 2011; 364: 797 -805 Crit Care Med 2008; 36[Suppl. ]: S 89 -S 94 Clin J Am Soc Nephrol 2010; 5: 1893 -1903 J Clin Hypertens 2011; 13: 639 -643 J Am Soc Nephrol 2001; 12: 1010– 1016 Kidney Int 1999; 55: 629 -34 Korean J Med 2011; 80: 8 -14 Harrison's Principles of Internal Medicine, 18 th edition www. uptodate. com