Distal tibial fractures AO Trauma Basic Principles Course
Distal tibial fractures AO Trauma Basic Principles Course
Learning objectives • Describe the anatomical characteristics of the distal tibia and why injuries of the distal tibia are unique • Define fractures requiring absolute stability and those amenable to relative stability, focusing on different fracture patterns • Recall techniques of internal fixation that avoid soft-tissue damage while preserving blood supply to the bone • Describe the role of the fibula in the operative treatment of distal tibial fractures

Objectives By the end of this talk you should be able to: • Appreciate the significance of this injury • Understand the fracture characteristics • Describe the treatment principles • Avoid the potential complications
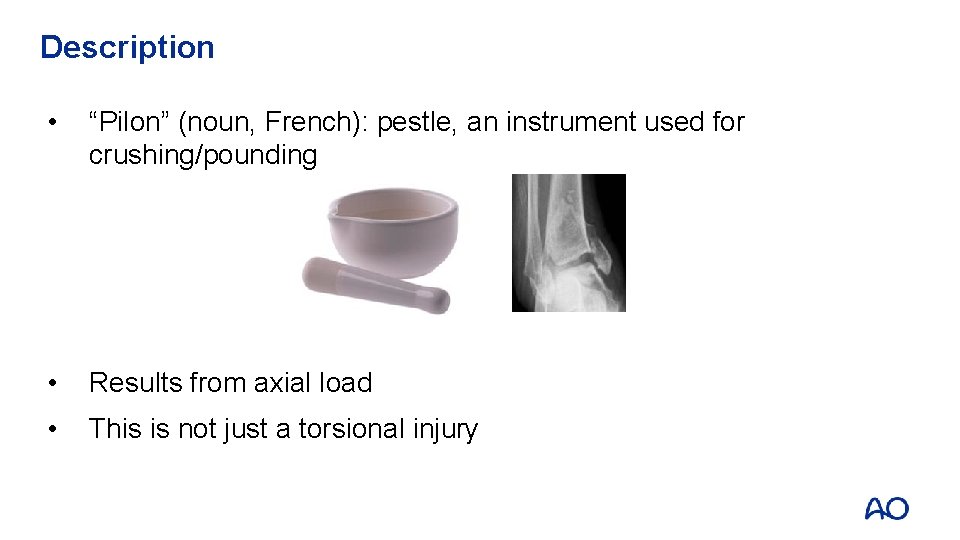
Description • “Pilon” (noun, French): pestle, an instrument used for crushing/pounding • Results from axial load • This is not just a torsional injury
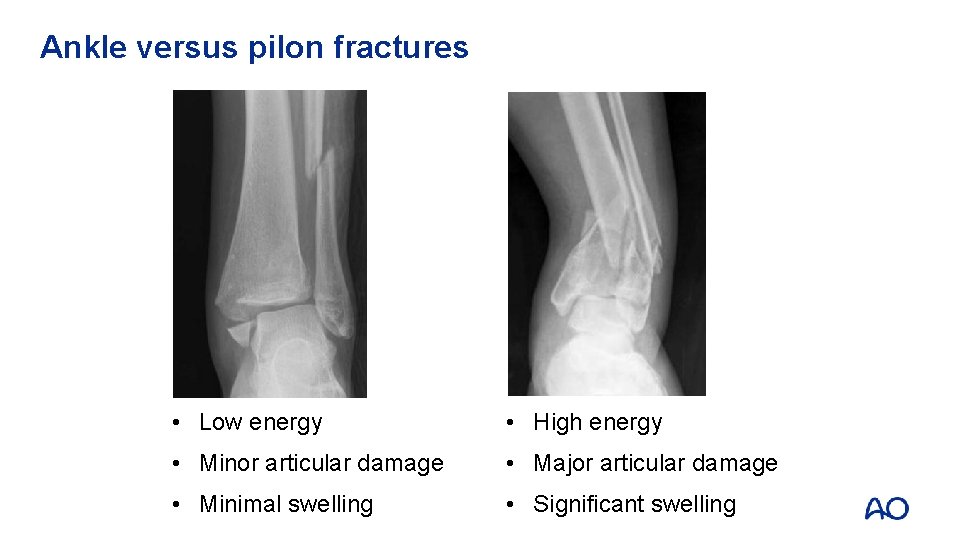
Ankle versus pilon fractures • Low energy • High energy • Minor articular damage • Major articular damage • Minimal swelling • Significant swelling

Respect the pilon • Complications: • Wound breakdown • Infection • Malunion • Nonunion • Arthritis • Stiffness • Amputation

Problem: soft-tissue injury!
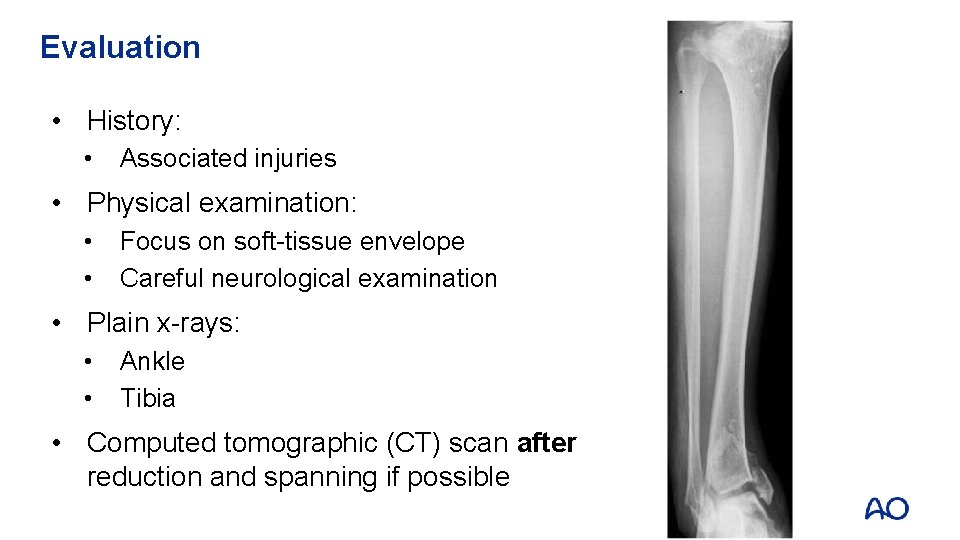
Evaluation • History: • Associated injuries • Physical examination: • • Focus on soft-tissue envelope Careful neurological examination • Plain x-rays: • • Ankle Tibia • Computed tomographic (CT) scan after reduction and spanning if possible
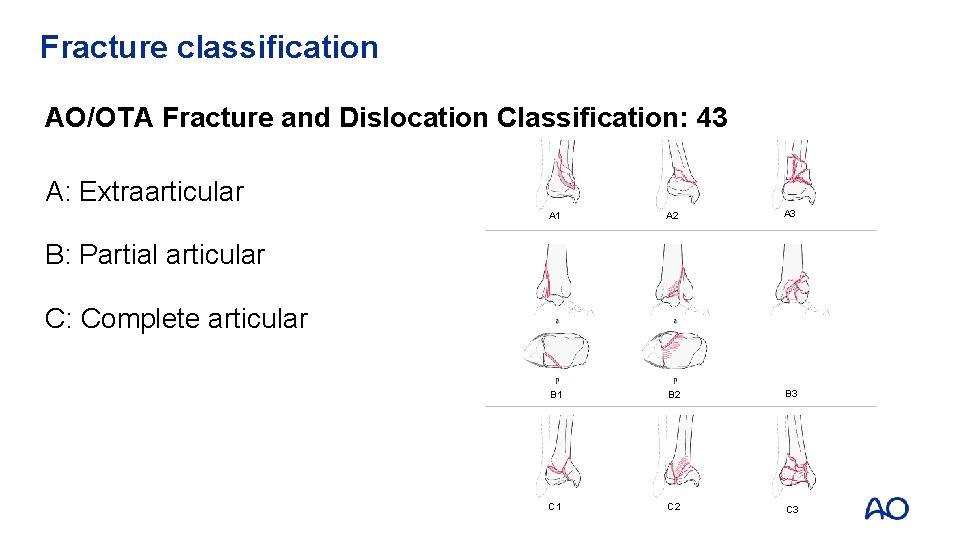
Fracture classification AO/OTA Fracture and Dislocation Classification: 43 A: Extraarticular A 1 A 2 A 3 B 1 B 2 B 3 C 1 C 2 C 3 B: Partial articular C: Complete articular
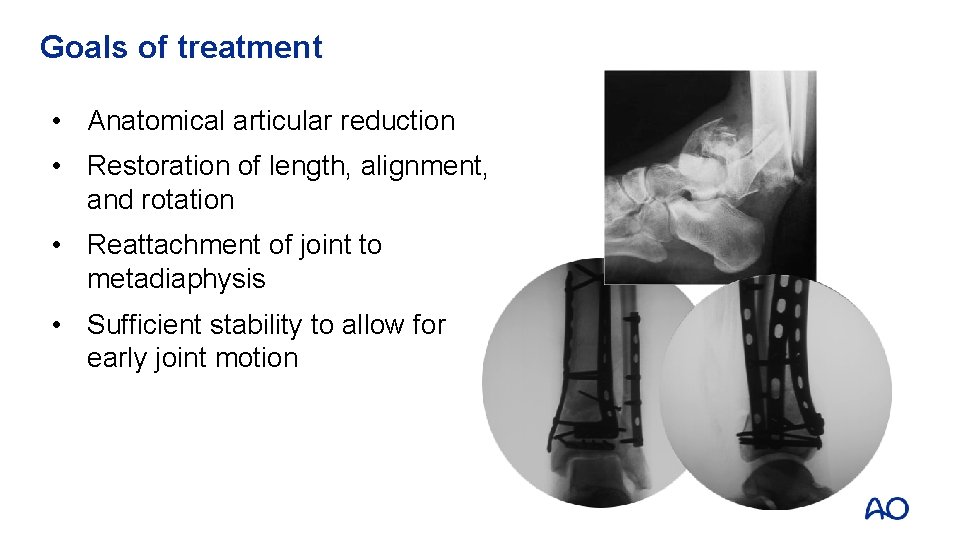
Goals of treatment • Anatomical articular reduction • Restoration of length, alignment, and rotation • Reattachment of joint to metadiaphysis • Sufficient stability to allow for early joint motion
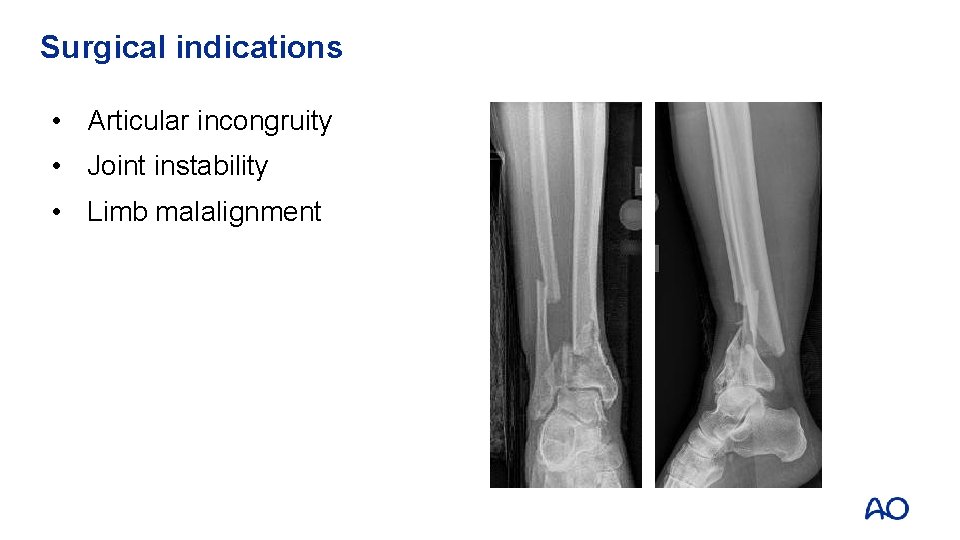
Surgical indications • Articular incongruity • Joint instability • Limb malalignment
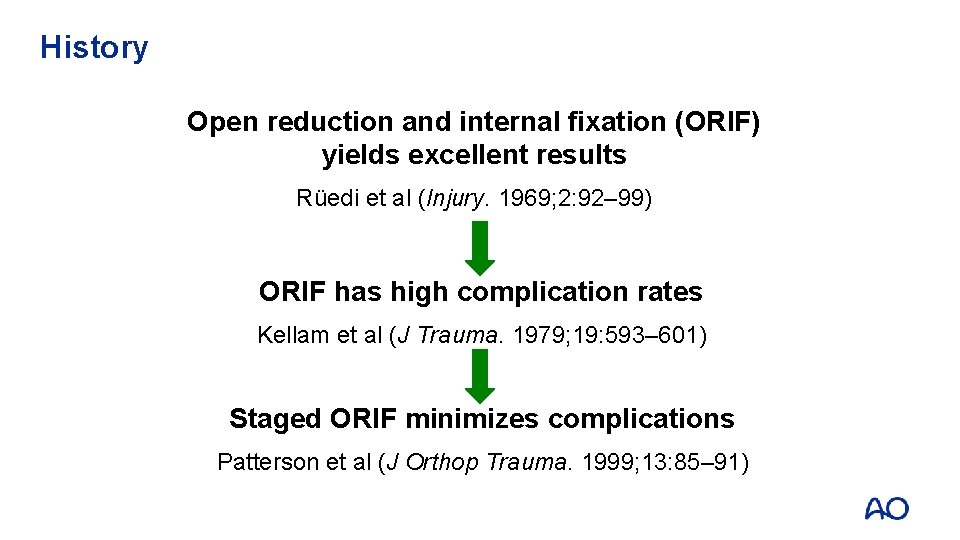
History Open reduction and internal fixation (ORIF) yields excellent results Rüedi et al (Injury. 1969; 2: 92– 99) ORIF has high complication rates Kellam et al (J Trauma. 1979; 19: 593– 601) Staged ORIF minimizes complications Patterson et al (J Orthop Trauma. 1999; 13: 85– 91)
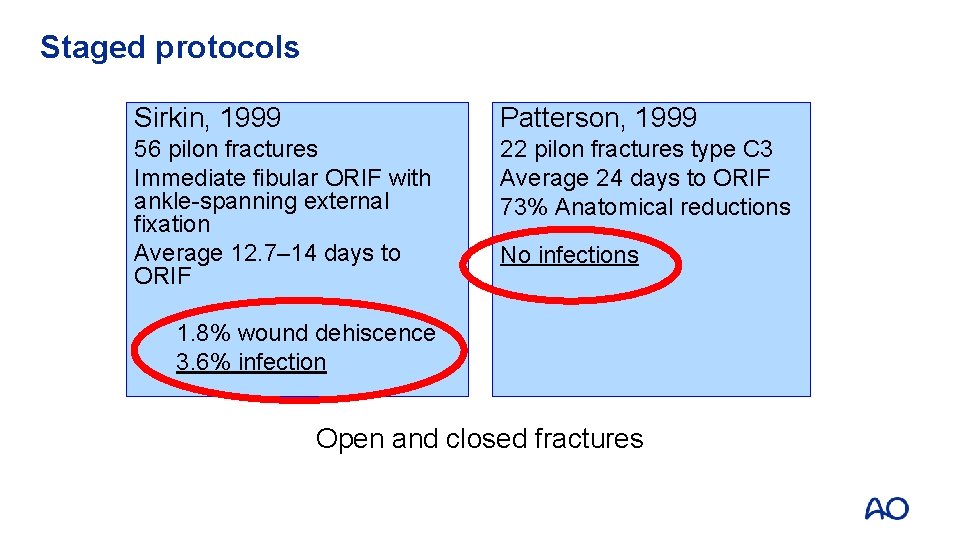
Staged protocols Sirkin, 1999 Patterson, 1999 56 pilon fractures Immediate fibular ORIF with ankle-spanning external fixation Average 12. 7– 14 days to ORIF 22 pilon fractures type C 3 Average 24 days to ORIF 73% Anatomical reductions No infections 1. 8% wound dehiscence 3. 6% infection Open and closed fractures
Staged protocol 1. Temporary limb stabilization 2. Await resolution of soft-tissue swelling 3. Study the injury 4. Staged reconstruction Sirkin et al (J Orthop Trauma. 1999; 13: 78– 84)
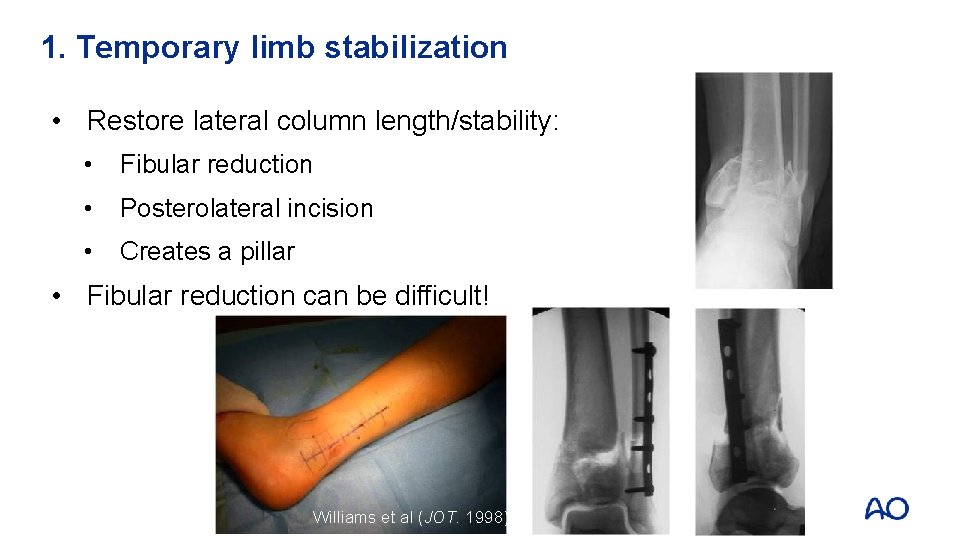
1. Temporary limb stabilization • Restore lateral column length/stability: • Fibular reduction • Posterolateral incision • Creates a pillar • Fibular reduction can be difficult! Williams et al (JOT. 1998)
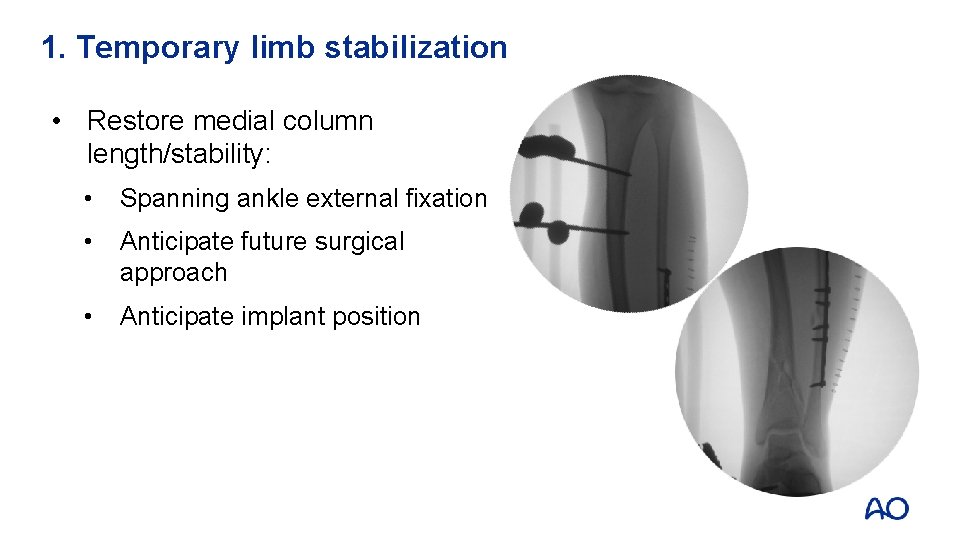
1. Temporary limb stabilization • Restore medial column length/stability: • Spanning ankle external fixation • Anticipate future surgical approach • Anticipate implant position
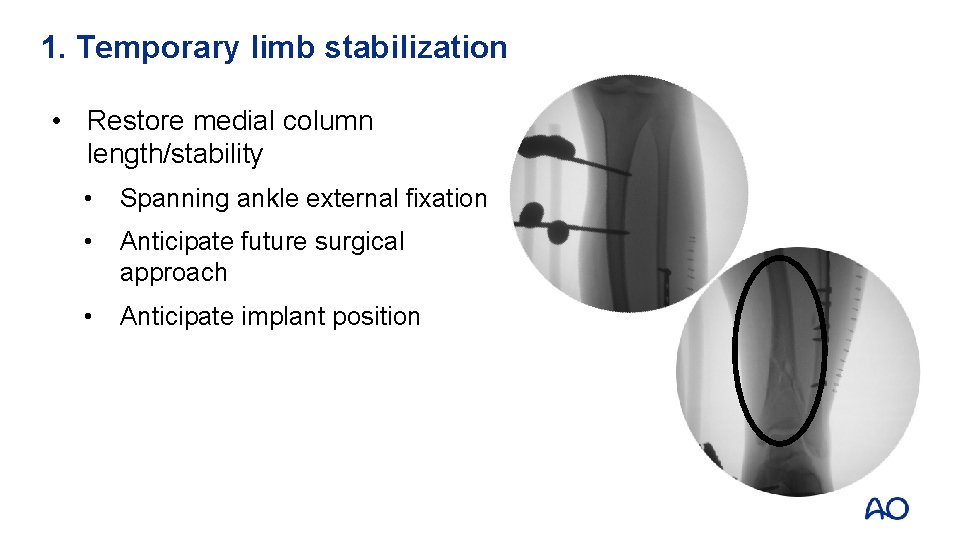
1. Temporary limb stabilization • Restore medial column length/stability • Spanning ankle external fixation • Anticipate future surgical approach • Anticipate implant position
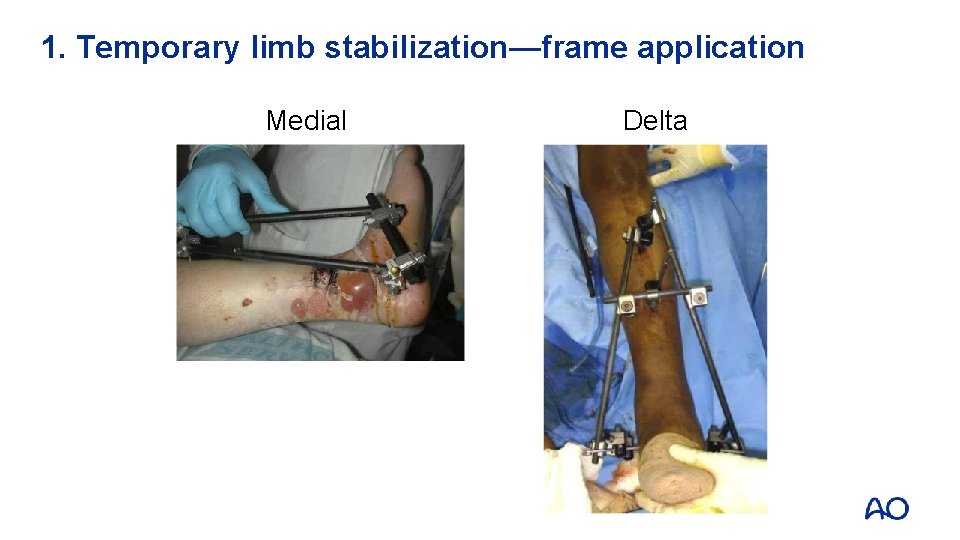
1. Temporary limb stabilization—frame application Medial Delta
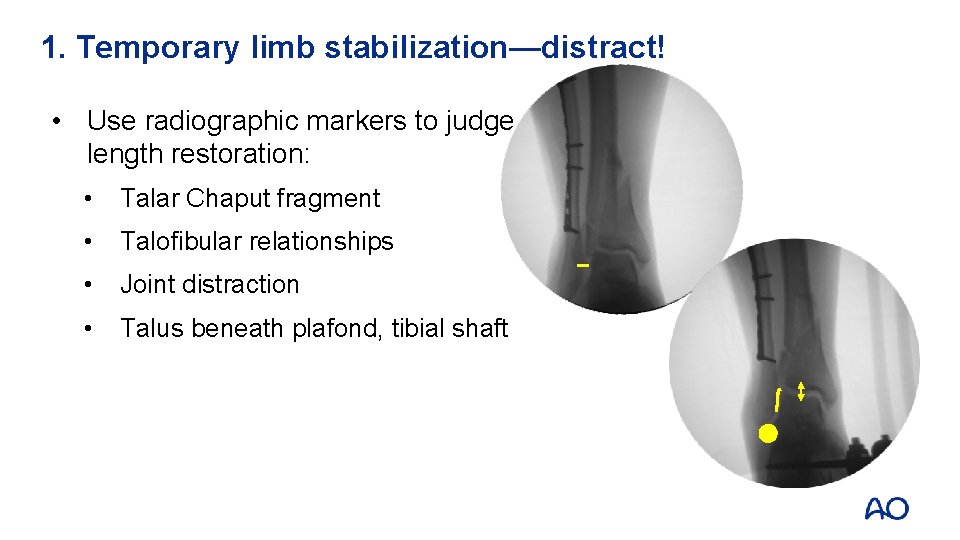
1. Temporary limb stabilization—distract! • Use radiographic markers to judge length restoration: • Talar Chaput fragment • Talofibular relationships • Joint distraction • Talus beneath plafond, tibial shaft
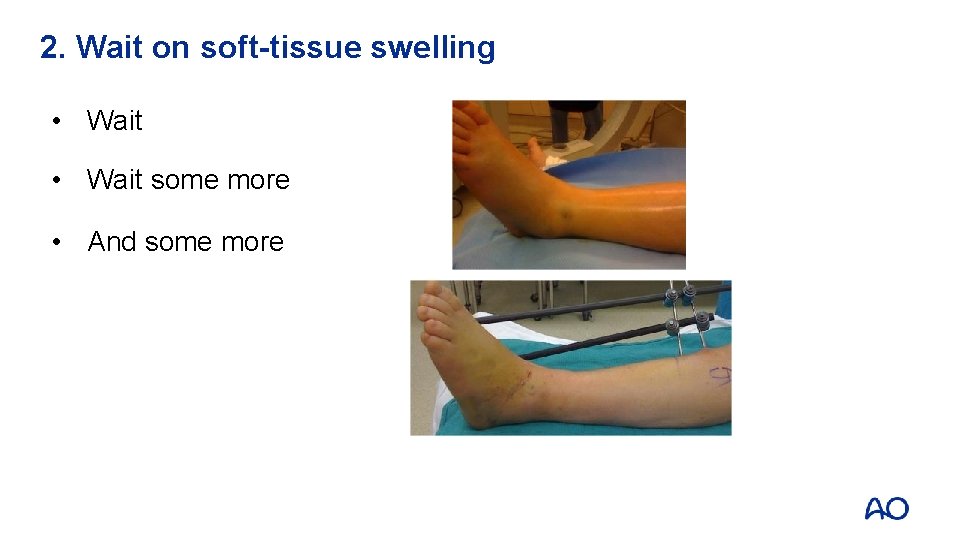
2. Wait on soft-tissue swelling • Wait some more • And some more
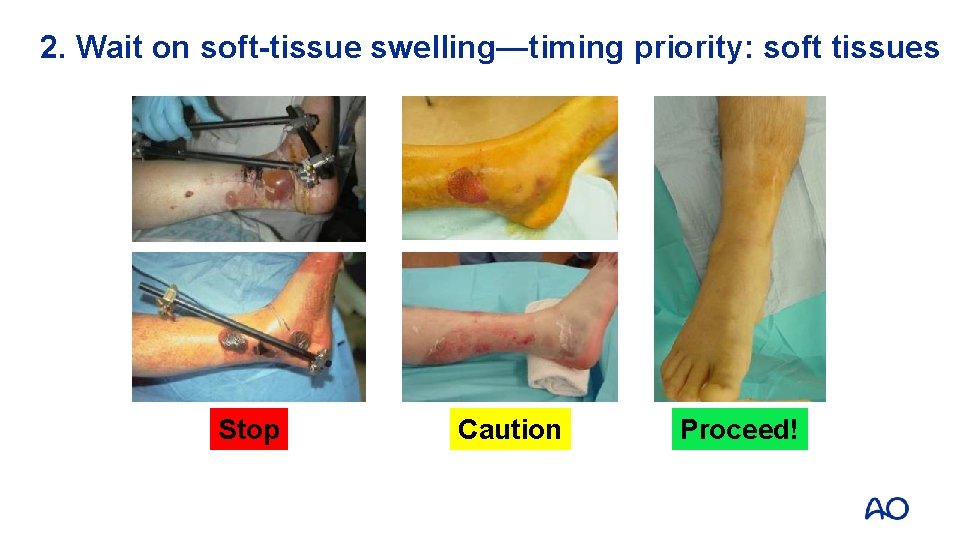
2. Wait on soft-tissue swelling—timing priority: soft tissues Stop Caution Proceed!

2. Wait on soft-tissue swelling—surgical timing • Correct timing is critical • Patience! • Rarely day 1– 6 • Often day 14– 21 • Wrinkles
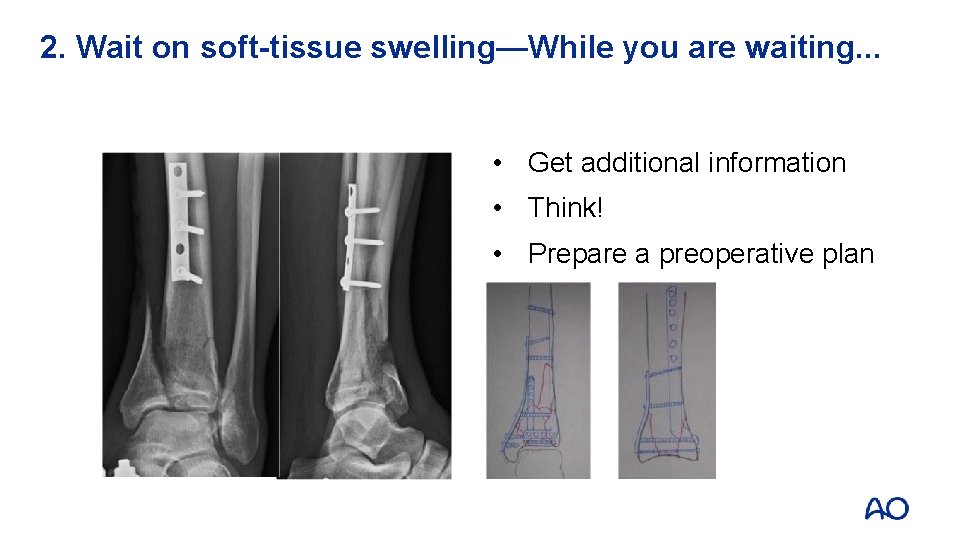
2. Wait on soft-tissue swelling—While you are waiting. . . • Get additional information • Think! • Prepare a preoperative plan
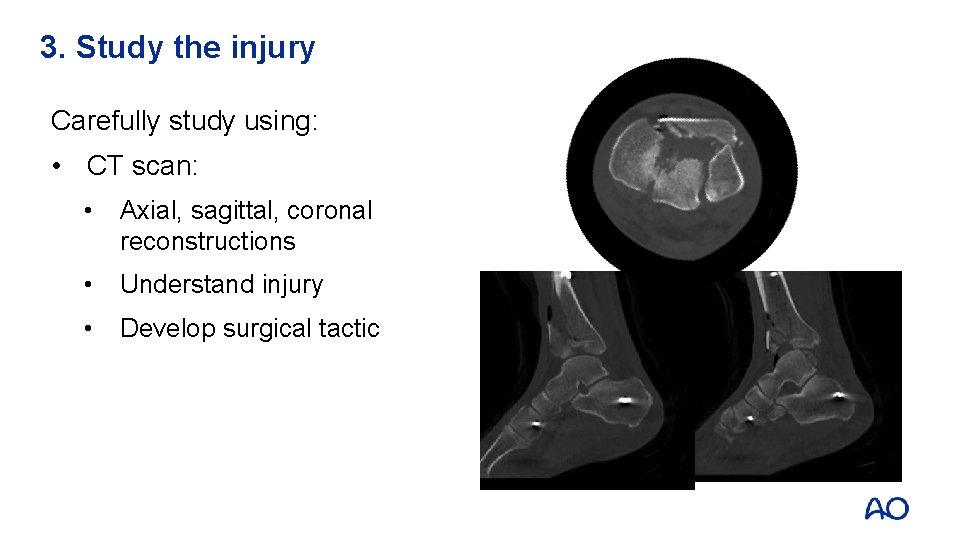
3. Study the injury Carefully study using: • CT scan: • Axial, sagittal, coronal reconstructions • Understand injury • Develop surgical tactic
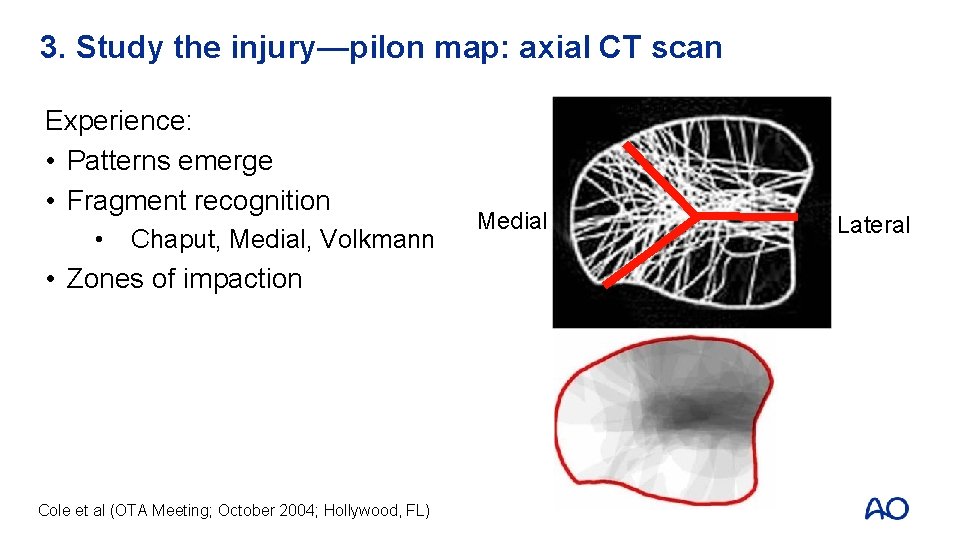
3. Study the injury—pilon map: axial CT scan Experience: • Patterns emerge • Fragment recognition • Chaput, Medial, Volkmann Anterior Medial Lateral • Zones of impaction Posterior Cole et al (OTA Meeting; October 2004; Hollywood, FL)
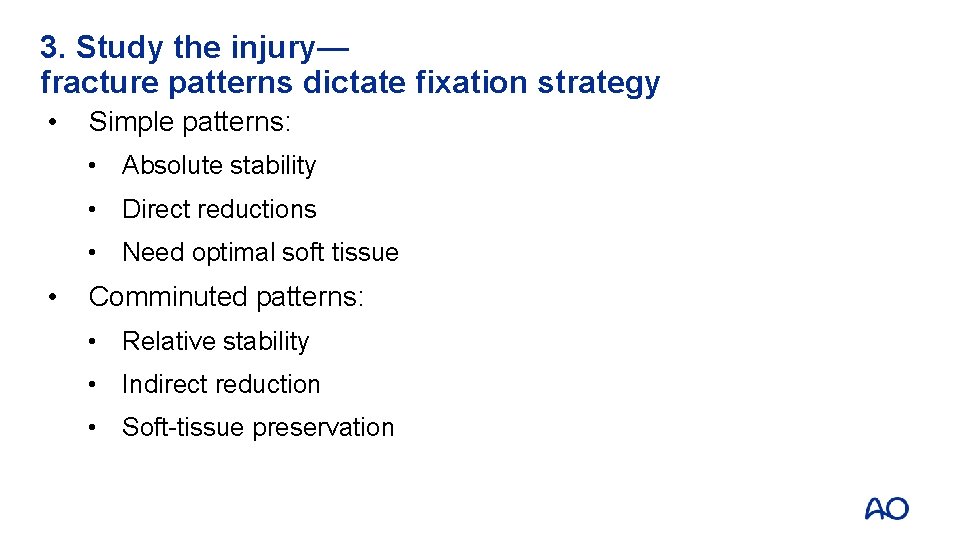
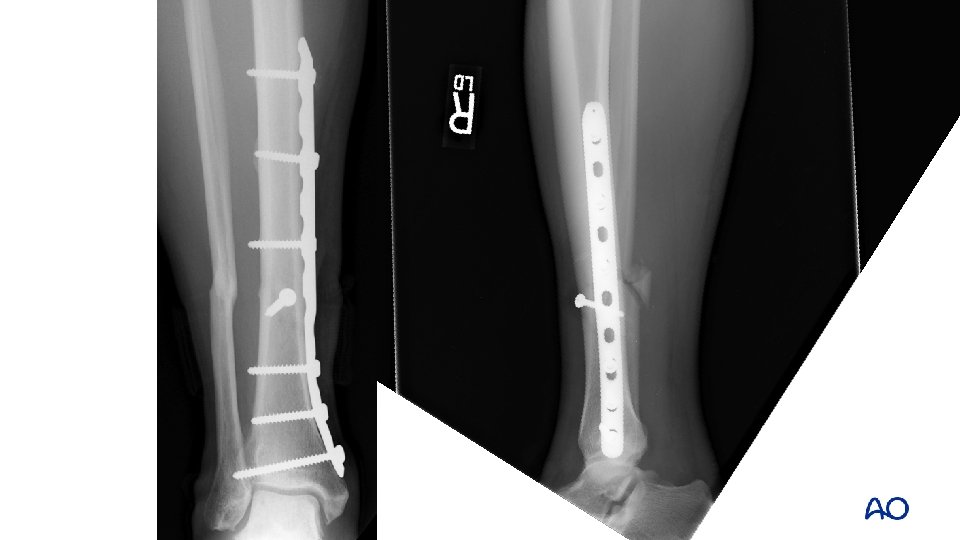
3. Study the injury— fracture patterns dictate fixation strategy • Simple patterns: • Absolute stability • Direct reductions • Need optimal soft tissue • Comminuted patterns: • Relative stability • Indirect reduction • Soft-tissue preservation






3. Study the injury—respect distal tibial fractures • Complications: • Wound breakdown • Infection • Malunion • Nonunion • Arthritis • Joint stiffness • Amputation
3. Study the injury—avoid complications! • Soft tissues: • Patience: wait • Meticulous handling • Careful closure • Bone: • Anatomical reconstruction of joint surface • Restore alignment • Preserve blood supply
3. Study the injury—treatment algorithm • Stabilize the soft tissues • Wait for soft tissues to recover • Understand the injury: • Create a surgical tactic • Reconstruct articular surface and secure to metadiaphysis • Use implants that neutralize the deforming forces and fixation strategies optimal for fracture patterns

Take-home messages • Axial loading injuries are a distinct high-energy fracture type • High-energy distal tibial fractures have severe soft-tissue injuries • Staged protocols can reduce complications • Fracture patterns dictate fixation strategy
- Slides: 37