Disorders of Water Balance Hyponatremia and Hypernatremia Zewdu
Disorders of Water Balance: Hyponatremia and Hypernatremia Zewdu Haile, MD Suneel Udani, MD
Key Learning Points • Electrolyte disorders are common in clinical practice and are mainly encountered in hospital populations. • The evaluation of the etiology of electrolyte disorders is mandatory before initiating specific therapy. • Hyponatremia, hypernatremia, hypokalemia and hyperkalemia are the most common electrolyte abnormalities encountered in clinical practice.
Disorders of Water Balance • Objectives: • Identify the disorders of serum sodium and the underlying water balance disorder. • Perform a concise history and physical exam with an emphasis on stimulus for ADH and volume status. • Interpret lab results to assess the kidneys' water handling and volume status. • Develop an impression and recommendations for management.
Disorders of Water Balance: A Nephron’s Perspective Goal: Apply the knowledge of renal water handling in evaluating disorders of water balance (hyponatremia and hypernatremia).
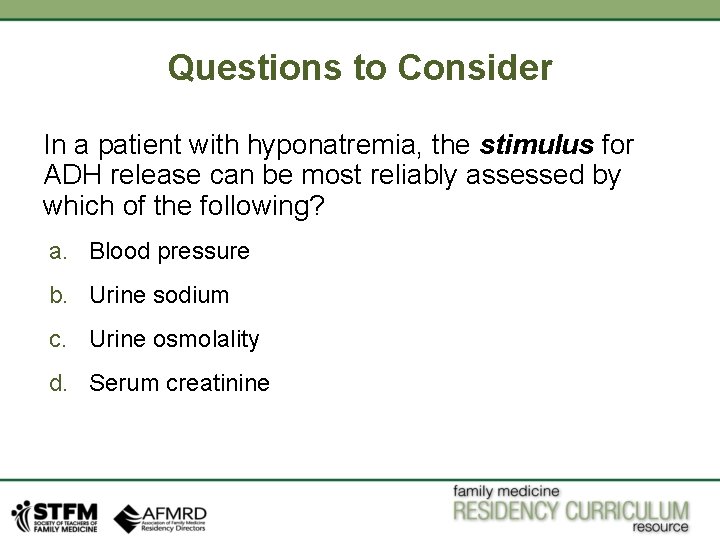
Questions to Consider In a patient with hyponatremia, the stimulus for ADH release can be most reliably assessed by which of the following? a. Blood pressure b. Urine sodium c. Urine osmolality d. Serum creatinine
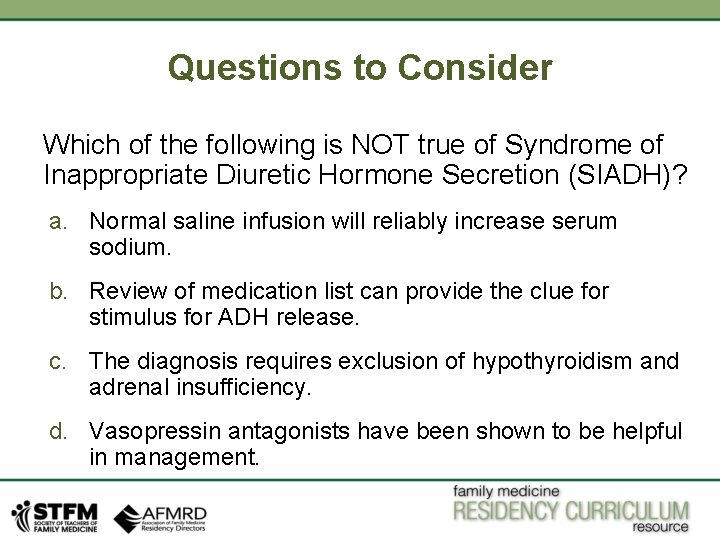
Questions to Consider Which of the following is NOT true of Syndrome of Inappropriate Diuretic Hormone Secretion (SIADH)? a. Normal saline infusion will reliably increase serum sodium. b. Review of medication list can provide the clue for stimulus for ADH release. c. The diagnosis requires exclusion of hypothyroidism and adrenal insufficiency. d. Vasopressin antagonists have been shown to be helpful in management.
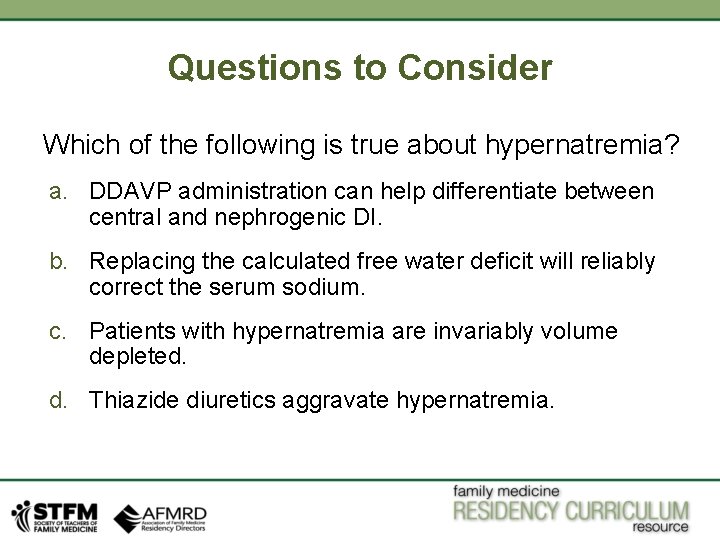
Questions to Consider Which of the following is true about hypernatremia? a. DDAVP administration can help differentiate between central and nephrogenic DI. b. Replacing the calculated free water deficit will reliably correct the serum sodium. c. Patients with hypernatremia are invariably volume depleted. d. Thiazide diuretics aggravate hypernatremia.
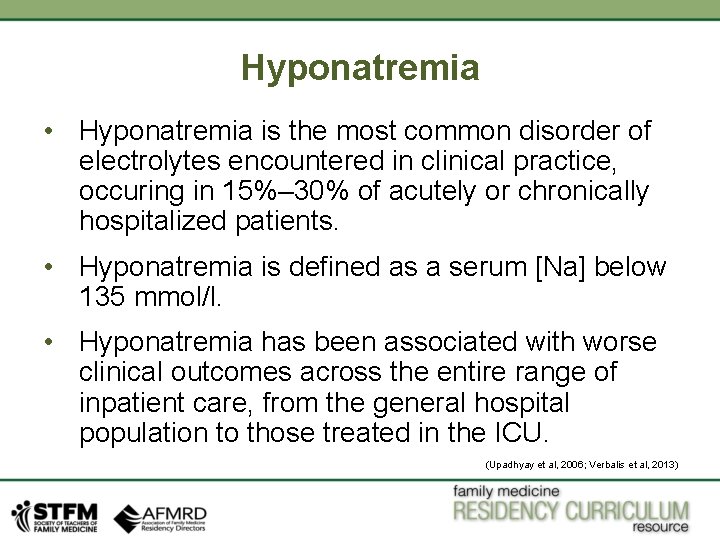
Hyponatremia • Hyponatremia is the most common disorder of electrolytes encountered in clinical practice, occuring in 15%– 30% of acutely or chronically hospitalized patients. • Hyponatremia is defined as a serum [Na] below 135 mmol/l. • Hyponatremia has been associated with worse clinical outcomes across the entire range of inpatient care, from the general hospital population to those treated in the ICU. (Upadhyay et al, 2006; Verbalis et al, 2013)
Hyponatremia—Overview • When hyponatremia develops rapidly (within 48 hours) and is severe (<120 m. Eq/l), initial symptoms of nausea and headache may progress to lethargy, psychosis, seizures, coma, brainstem herniation, and death. • In elderly patients, mild hyponatremia (125– 135 m. Eq/l) can be an important cause of frequent falls and attention deficits.
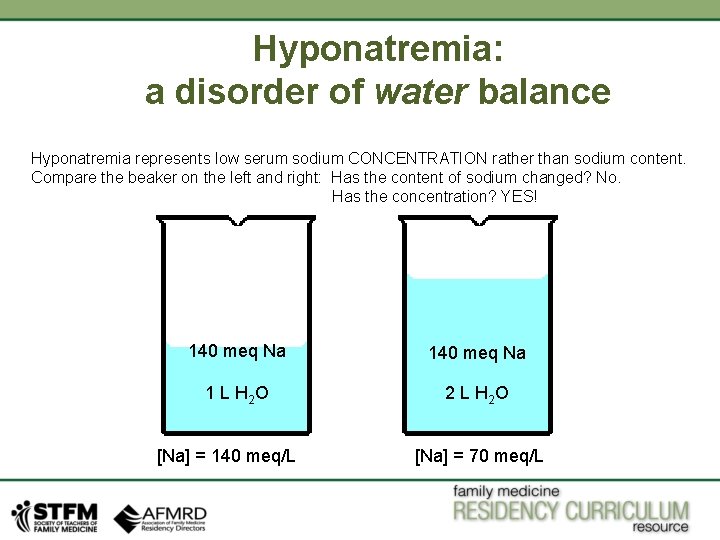
Hyponatremia: a disorder of water balance Hyponatremia represents low serum sodium CONCENTRATION rather than sodium content. Compare the beaker on the left and right: Has the content of sodium changed? No. Has the concentration? YES! 140 meq Na 1 L H 2 O 2 L H 2 O [Na] = 140 meq/L [Na] = 70 meq/L
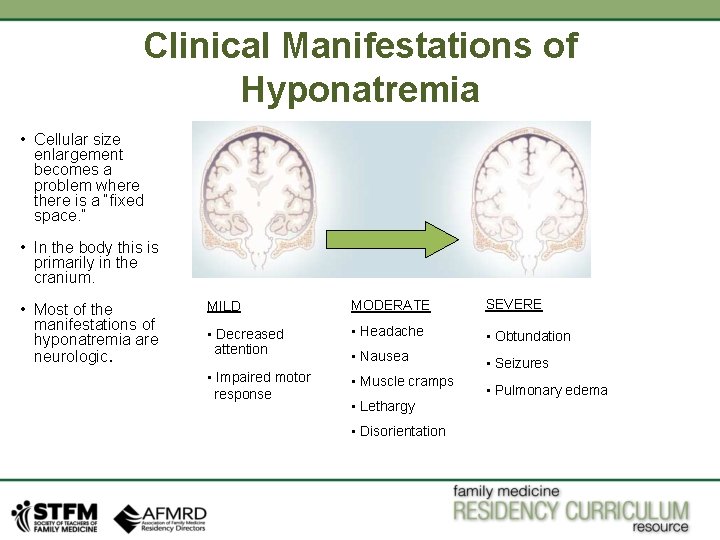
Clinical Manifestations of Hyponatremia • Cellular size enlargement becomes a problem where there is a “fixed space. ” • In the body this is primarily in the cranium. • Most of the manifestations of hyponatremia are neurologic. MILD MODERATE SEVERE • Decreased attention • Headache • Obtundation • Nausea • Impaired motor response • Seizures • Muscle cramps • Lethargy • Disorientation • Pulmonary edema
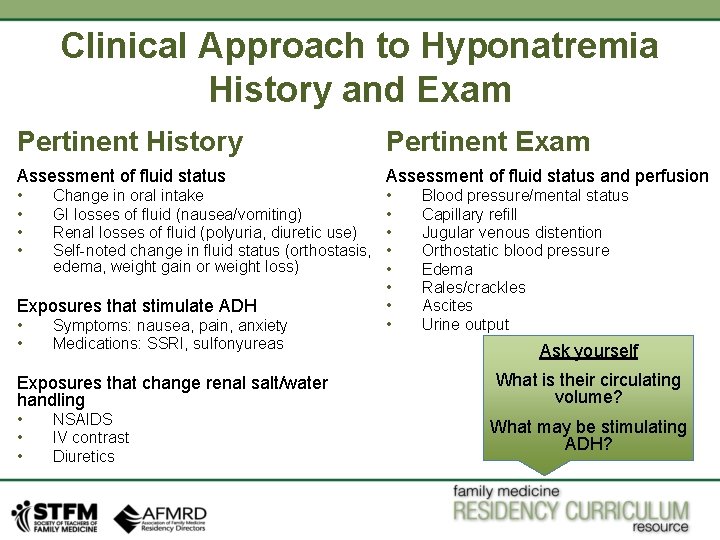
Clinical Approach to Hyponatremia History and Exam Pertinent History Pertinent Exam Assessment of fluid status and perfusion • • Change in oral intake GI losses of fluid (nausea/vomiting) Renal losses of fluid (polyuria, diuretic use) Self-noted change in fluid status (orthostasis, edema, weight gain or weight loss) Exposures that stimulate ADH • • Symptoms: nausea, pain, anxiety Medications: SSRI, sulfonyureas Exposures that change renal salt/water handling • • • NSAIDS IV contrast Diuretics • • Blood pressure/mental status Capillary refill Jugular venous distention Orthostatic blood pressure Edema Rales/crackles Ascites Urine output Ask yourself What is their circulating volume? What may be stimulating ADH?
Clinical Approach to Hyponatremia Laboratory • Plasma osmolality • Plasma concentration of Na, K, CL, Hco 3, urea, glucose • Urine Na concentration • Urine osmolality • TSH • AM cortisol (Braun et al, 2015)
![Clinical Approach to Hyponatremia Laboratory Low EABV High RAAS High ADH Yes [Na] < Clinical Approach to Hyponatremia Laboratory Low EABV High RAAS High ADH Yes [Na] <](http://slidetodoc.com/presentation_image_h2/bb755ec661c2345e256ccd10d3e744b4/image-14.jpg)
Clinical Approach to Hyponatremia Laboratory Low EABV High RAAS High ADH Yes [Na] < 135 meq/L P Osm < 285 m. Osm/L? No Check blood glucose, evaluate for alternative osmotically active solutes Yes Is ADH active? (i. e Uosm > 100) No Primary Polydipsia Yes Physiologic reason for ADH release? No Nl/High EABV Nl/low RAAS High ADH (inappropriate)
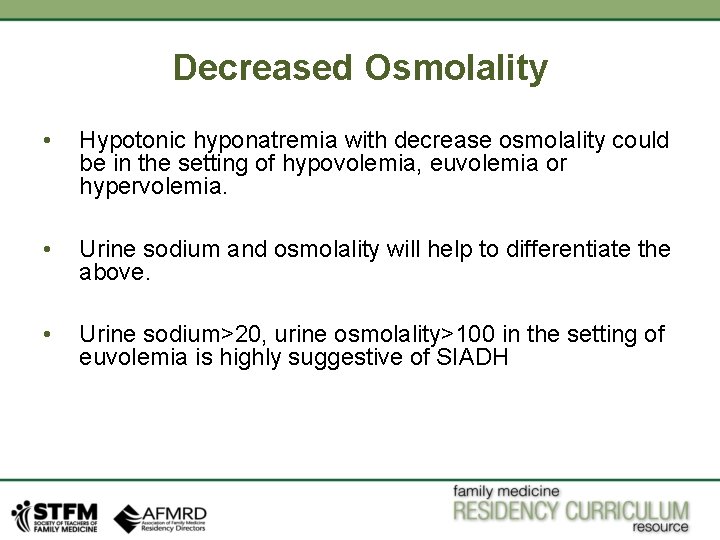
Decreased Osmolality • Hypotonic hyponatremia with decrease osmolality could be in the setting of hypovolemia, euvolemia or hypervolemia. • Urine sodium and osmolality will help to differentiate the above. • Urine sodium>20, urine osmolality>100 in the setting of euvolemia is highly suggestive of SIADH
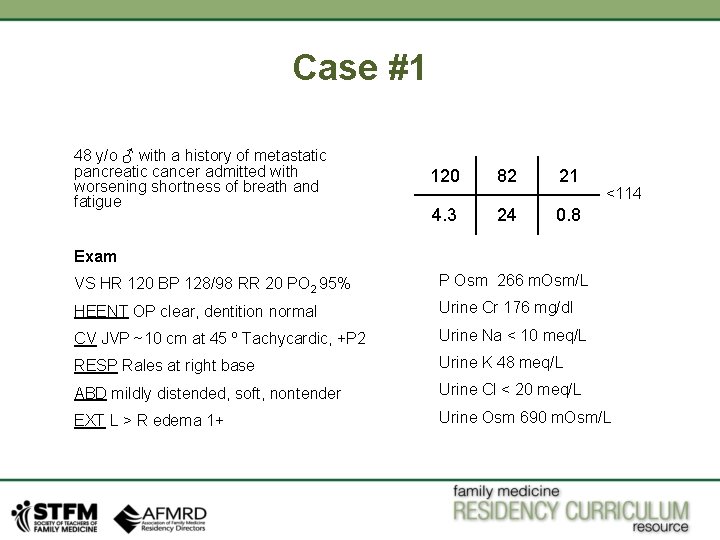
Case #1 48 y/o ♂ with a history of metastatic pancreatic cancer admitted with worsening shortness of breath and fatigue 120 82 21 4. 3 24 0. 8 <114 Exam VS HR 120 BP 128/98 RR 20 PO 2 95% P Osm 266 m. Osm/L HEENT OP clear, dentition normal Urine Cr 176 mg/dl CV JVP ~10 cm at 45 º Tachycardic, +P 2 Urine Na < 10 meq/L RESP Rales at right base Urine K 48 meq/L ABD mildly distended, soft, nontender Urine Cl < 20 meq/L EXT L > R edema 1+ Urine Osm 690 m. Osm/L
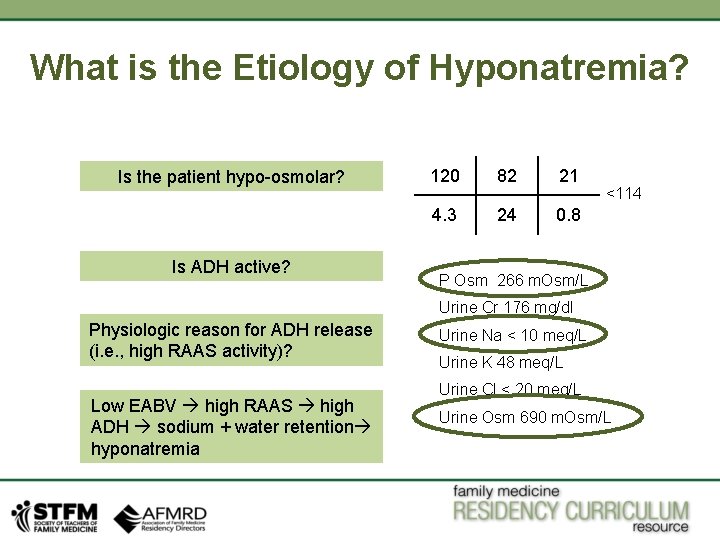
What is the Etiology of Hyponatremia? Is the patient hypo-osmolar? Is ADH active? 120 82 21 4. 3 24 0. 8 <114 P Osm 266 m. Osm/L Urine Cr 176 mg/dl Physiologic reason for ADH release (i. e. , high RAAS activity)? Low EABV high RAAS high ADH sodium + water retention hyponatremia Urine Na < 10 meq/L Urine K 48 meq/L Urine Cl < 20 meq/L Urine Osm 690 m. Osm/L
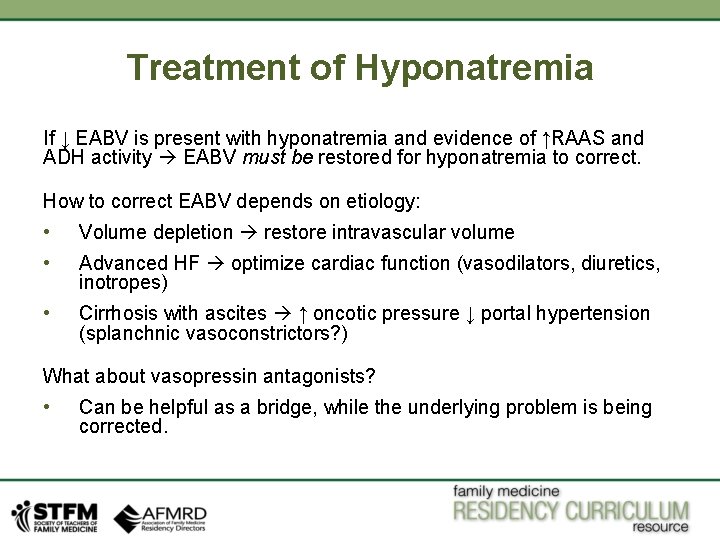
Treatment of Hyponatremia If ↓ EABV is present with hyponatremia and evidence of ↑RAAS and ADH activity EABV must be restored for hyponatremia to correct. How to correct EABV depends on etiology: • Volume depletion restore intravascular volume • Advanced HF optimize cardiac function (vasodilators, diuretics, inotropes) • Cirrhosis with ascites ↑ oncotic pressure ↓ portal hypertension (splanchnic vasoconstrictors? ) What about vasopressin antagonists? • Can be helpful as a bridge, while the underlying problem is being corrected.
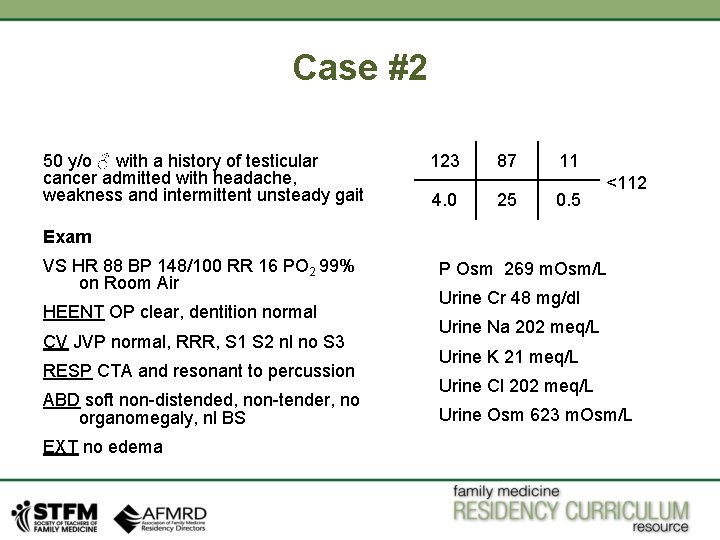
Case #2 50 y/o ♂ with a history of testicular cancer admitted with headache, weakness and intermittent unsteady gait 123 4. 0 87 25 11 0. 5 <112 Exam VS HR 88 BP 148/100 RR 16 PO 2 99% on Room Air HEENT OP clear, dentition normal CV JVP normal, RRR, S 1 S 2 nl no S 3 RESP CTA and resonant to percussion ABD soft non-distended, non-tender, no organomegaly, nl BS EXT no edema P Osm 269 m. Osm/L Urine Cr 48 mg/dl Urine Na 202 meq/L Urine K 21 meq/L Urine Cl 202 meq/L Urine Osm 623 m. Osm/L
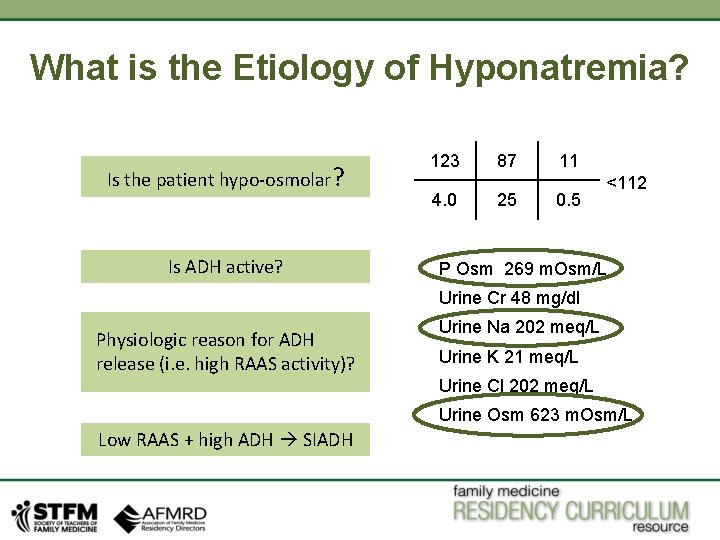
What is the Etiology of Hyponatremia? Is the patient hypo-osmolar? Is ADH active? 123 4. 0 87 25 11 0. 5 <112 P Osm 269 m. Osm/L Urine Cr 48 mg/dl Physiologic reason for ADH release (i. e. high RAAS activity)? Urine Na 202 meq/L Urine K 21 meq/L Urine Cl 202 meq/L Urine Osm 623 m. Osm/L Low RAAS + high ADH SIADH
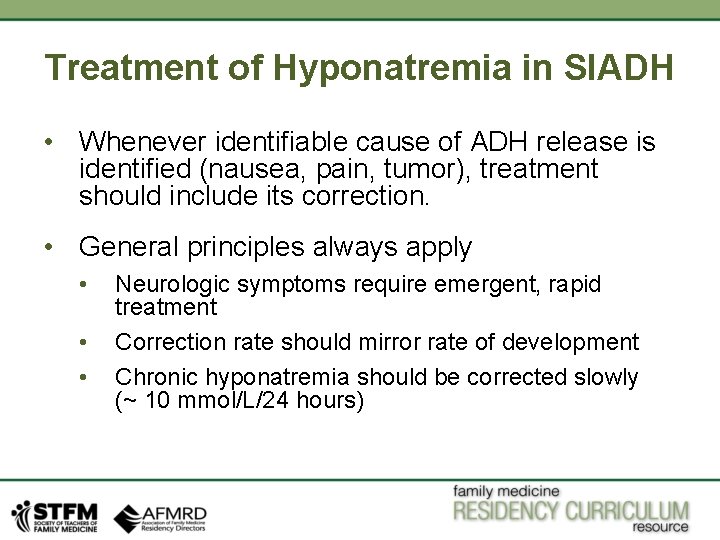
Treatment of Hyponatremia in SIADH • Whenever identifiable cause of ADH release is identified (nausea, pain, tumor), treatment should include its correction. • General principles always apply • • • Neurologic symptoms require emergent, rapid treatment Correction rate should mirror rate of development Chronic hyponatremia should be corrected slowly (~ 10 mmol/L/24 hours)
Treatment of Hyponatremia • Fluid restriction • • Difficult due to sensation of thirst All fluid is hypotonic! • Salt tablets (in concert with fluid restriction) • Potassium replacement (often concomitant hypokalemia or total body K deficit) • • Exchangeable Na = (Na + K)/Total body H 2 O KCL “rider” = 20 meq/100 ml = 400 m. Osm/L

Urea Supplementation • Urea had been used for many years as treatment for hyponatremia due to SIADH and hypervolemic states • Urea acts as an osmotic diuretic and increases free water excretion without significant effect on natriuresis or kaliuresis • Recently it has been reformulated with a more palatable flavor with an associated resurgence in use • Urea has been included in the European Society of Endocrinology guidelines for treatment • The usual dose is 7. 5 grams twice daily escalating to 15 grams twice daily as needed
Vasopressin Antagonists • Indicated for treatment of “euvolemic” and “hypervolemic” hyponatremia (NOT hypovolemic hyponatremia) • Oral—Tonivaptan • IV—Conivaptan • Appear to be effective and safe, but use is on case-by-case basis
Treatment of Hyponatremia Special Circumstances Acute hyponatremia with neurologic dysfunction must be treated emergently. • 3% saline solution 100 ml administered over 15 minutes (can be repeated up to three times) • Raise [Na] to safe level in first few hours then slow correction to 24 -hour goal
Treatment of Hyponatremia Special Circumstances • Individuals with chronic hyponatremia with readily correctable underlying cause (e. g. , volume depletion, adrenal insufficiency) are at highest risk for CPM. • These patients may require administration of DDAVP to limit water diuresis.
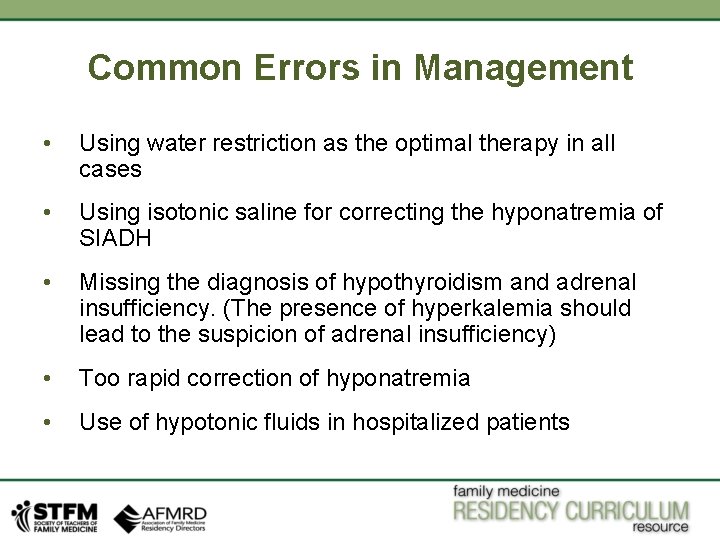
Common Errors in Management • Using water restriction as the optimal therapy in all cases • Using isotonic saline for correcting the hyponatremia of SIADH • Missing the diagnosis of hypothyroidism and adrenal insufficiency. (The presence of hyperkalemia should lead to the suspicion of adrenal insufficiency) • Too rapid correction of hyponatremia • Use of hypotonic fluids in hospitalized patients
Hypernatremia • Defined as serum sodium>145 m. Eq/l • In adults, hypernatremia is almost exclusively due to a TBW (total body water) deficit. (Huang et al, 2007)
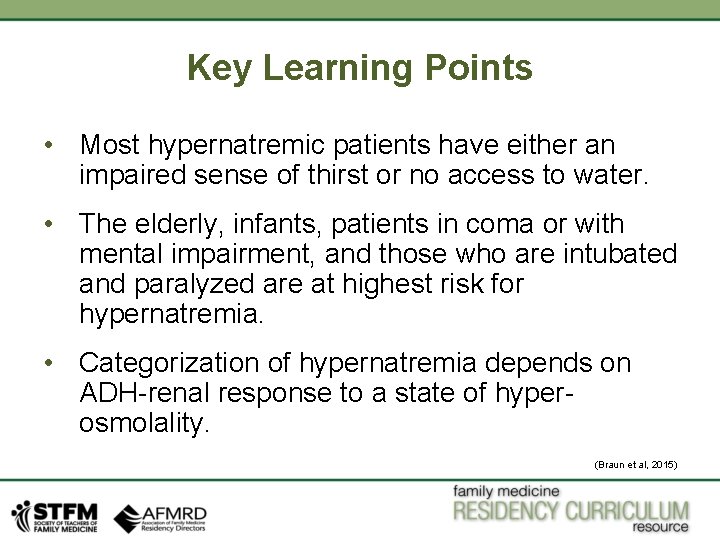
Key Learning Points • Most hypernatremic patients have either an impaired sense of thirst or no access to water. • The elderly, infants, patients in coma or with mental impairment, and those who are intubated and paralyzed are at highest risk for hypernatremia. • Categorization of hypernatremia depends on ADH-renal response to a state of hyperosmolality. (Braun et al, 2015)
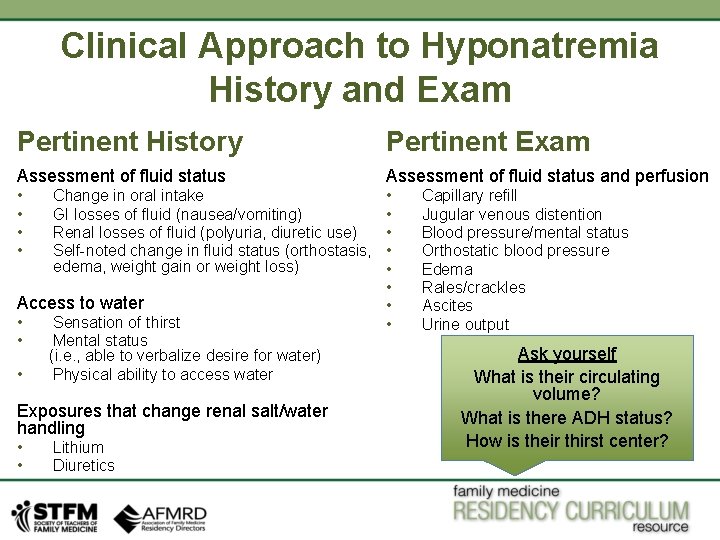
Clinical Approach to Hyponatremia History and Exam Pertinent History Pertinent Exam Assessment of fluid status and perfusion • • Change in oral intake GI losses of fluid (nausea/vomiting) Renal losses of fluid (polyuria, diuretic use) Self-noted change in fluid status (orthostasis, edema, weight gain or weight loss) Access to water • • • Sensation of thirst Mental status (i. e. , able to verbalize desire for water) Physical ability to access water Exposures that change renal salt/water handling • • Lithium Diuretics • • Capillary refill Jugular venous distention Blood pressure/mental status Orthostatic blood pressure Edema Rales/crackles Ascites Urine output Ask yourself What is their circulating volume? What is there ADH status? How is their thirst center?
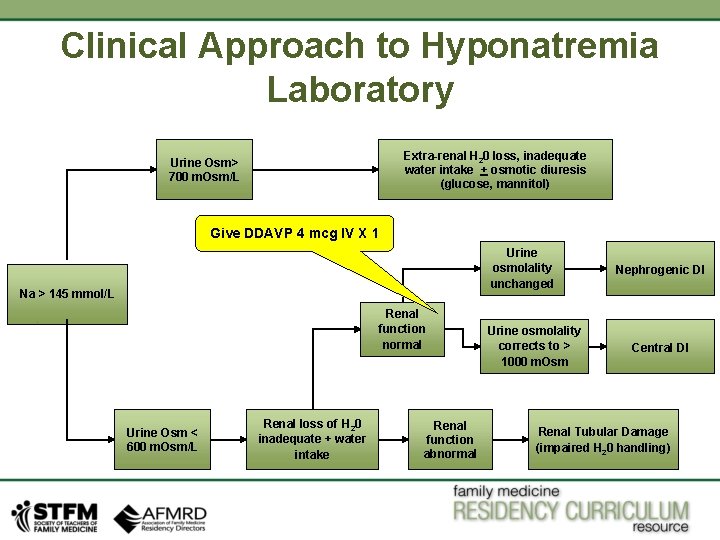
Clinical Approach to Hyponatremia Laboratory Extra-renal H 20 loss, inadequate water intake + osmotic diuresis (glucose, mannitol) Urine Osm> 700 m. Osm/L Give DDAVP 4 mcg IV X 1 Urine osmolality unchanged Na > 145 mmol/L Renal function normal Urine Osm < 600 m. Osm/L Renal loss of H 20 inadequate + water intake Renal function abnormal Urine osmolality corrects to > 1000 m. Osm Nephrogenic DI Central DI Renal Tubular Damage (impaired H 20 handling)
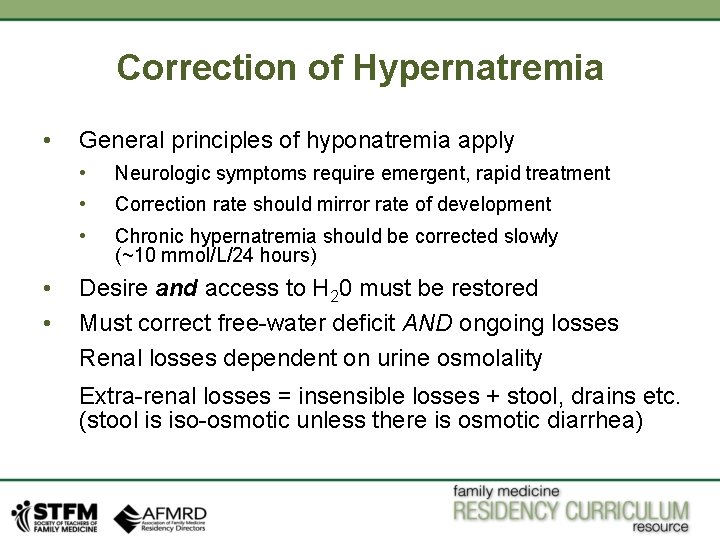
Correction of Hypernatremia • • • General principles of hyponatremia apply • Neurologic symptoms require emergent, rapid treatment • Correction rate should mirror rate of development • Chronic hypernatremia should be corrected slowly (~10 mmol/L/24 hours) Desire and access to H 20 must be restored Must correct free-water deficit AND ongoing losses Renal losses dependent on urine osmolality Extra-renal losses = insensible losses + stool, drains etc. (stool is iso-osmotic unless there is osmotic diarrhea)
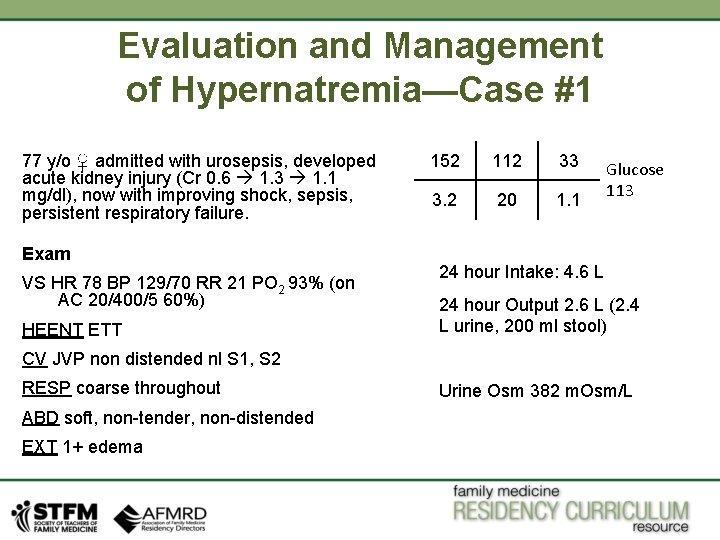
Evaluation and Management of Hypernatremia—Case #1 77 y/o ♀ admitted with urosepsis, developed acute kidney injury (Cr 0. 6 1. 3 1. 1 mg/dl), now with improving shock, sepsis, persistent respiratory failure. Exam VS HR 78 BP 129/70 RR 21 PO 2 93% (on AC 20/400/5 60%) HEENT ETT 152 112 33 3. 2 20 1. 1 Glucose 113 24 hour Intake: 4. 6 L 24 hour Output 2. 6 L (2. 4 L urine, 200 ml stool) CV JVP non distended nl S 1, S 2 RESP coarse throughout ABD soft, non-tender, non-distended EXT 1+ edema Urine Osm 382 m. Osm/L
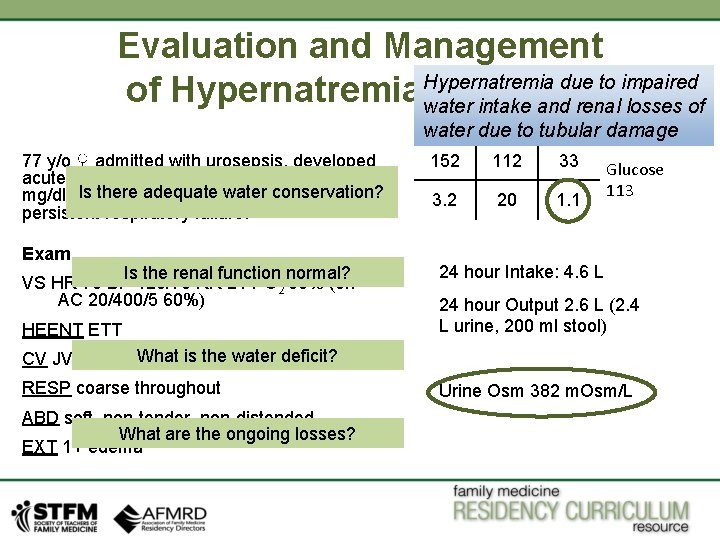
Evaluation and Management Hypernatremia due to impaired of Hypernatremia—Case #1 water intake and renal losses of water due to tubular damage 77 y/o ♀ admitted with urosepsis, developed acute kidney injury (Cr 0. 6 1. 3 1. 1 there water conservation? mg/dl), Is now withadequate improving shock, sepsis, persistent respiratory failure. Exam Is the renal function normal? VS HR 78 BP 129/70 RR 21 PO 2 93% (on AC 20/400/5 60%) HEENT ETT 152 112 33 3. 2 20 1. 1 Glucose 113 24 hour Intake: 4. 6 L 24 hour Output 2. 6 L (2. 4 L urine, 200 ml stool) What is the water CV JVP non distended nl S 1, S 2 deficit? RESP coarse throughout ABD soft, non-tender, non-distended What are the ongoing losses? EXT 1+ edema Urine Osm 382 m. Osm/L
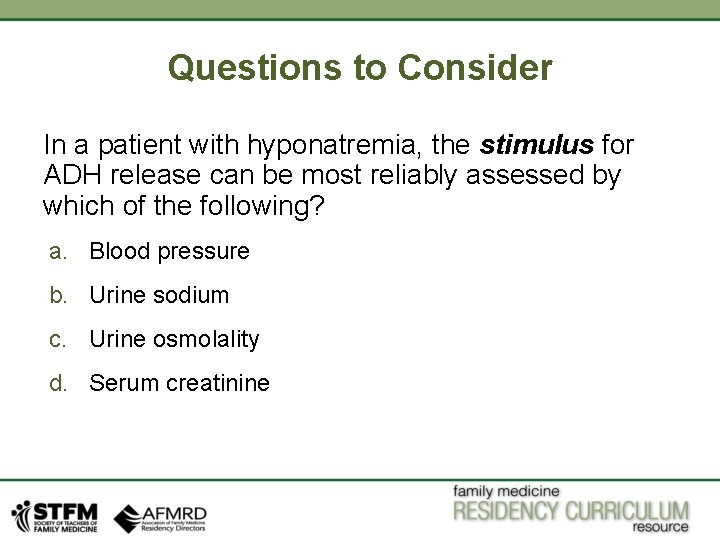
Questions to Consider In a patient with hyponatremia, the stimulus for ADH release can be most reliably assessed by which of the following? a. Blood pressure b. Urine sodium c. Urine osmolality d. Serum creatinine
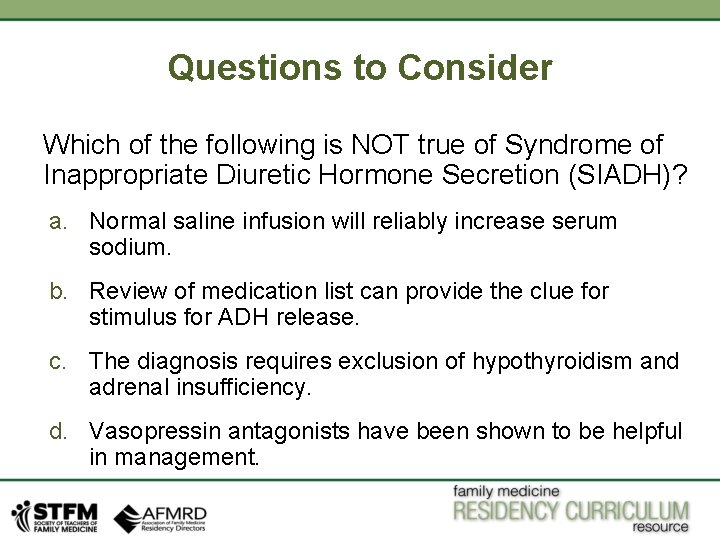
Questions to Consider Which of the following is NOT true of Syndrome of Inappropriate Diuretic Hormone Secretion (SIADH)? a. Normal saline infusion will reliably increase serum sodium. b. Review of medication list can provide the clue for stimulus for ADH release. c. The diagnosis requires exclusion of hypothyroidism and adrenal insufficiency. d. Vasopressin antagonists have been shown to be helpful in management.
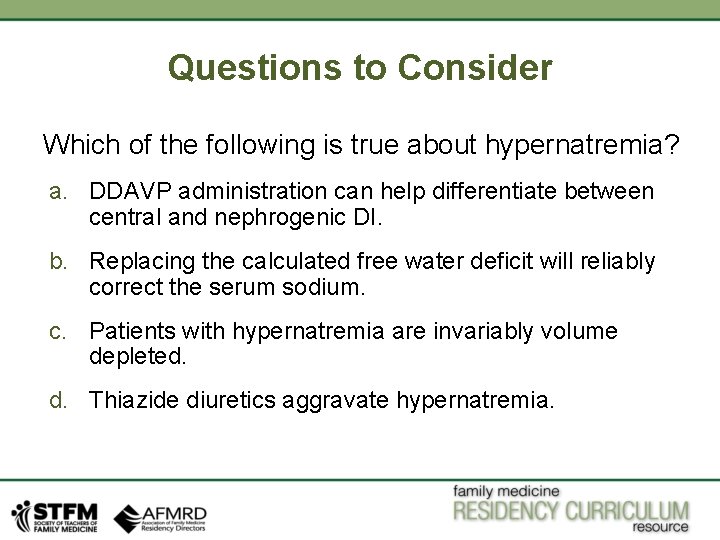
Questions to Consider Which of the following is true about hypernatremia? a. DDAVP administration can help differentiate between central and nephrogenic DI. b. Replacing the calculated free water deficit will reliably correct the serum sodium. c. Patients with hypernatremia are invariably volume depleted. d. Thiazide diuretics aggravate hypernatremia.
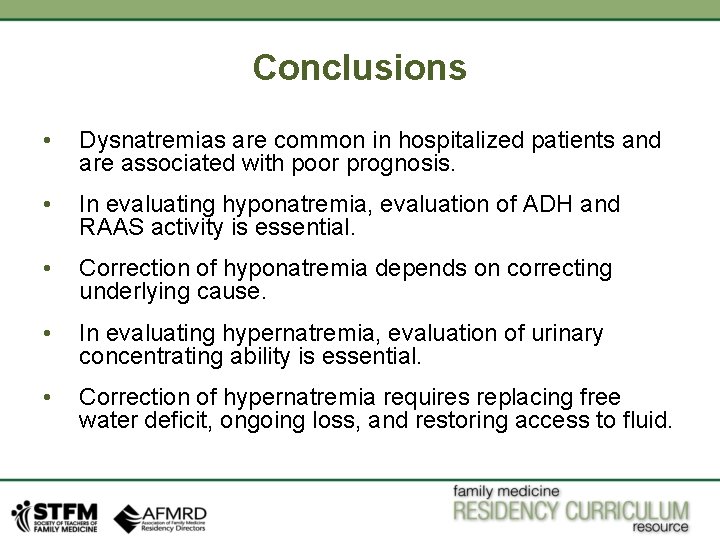
Conclusions • Dysnatremias are common in hospitalized patients and are associated with poor prognosis. • In evaluating hyponatremia, evaluation of ADH and RAAS activity is essential. • Correction of hyponatremia depends on correcting underlying cause. • In evaluating hypernatremia, evaluation of urinary concentrating ability is essential. • Correction of hypernatremia requires replacing free water deficit, ongoing loss, and restoring access to fluid.
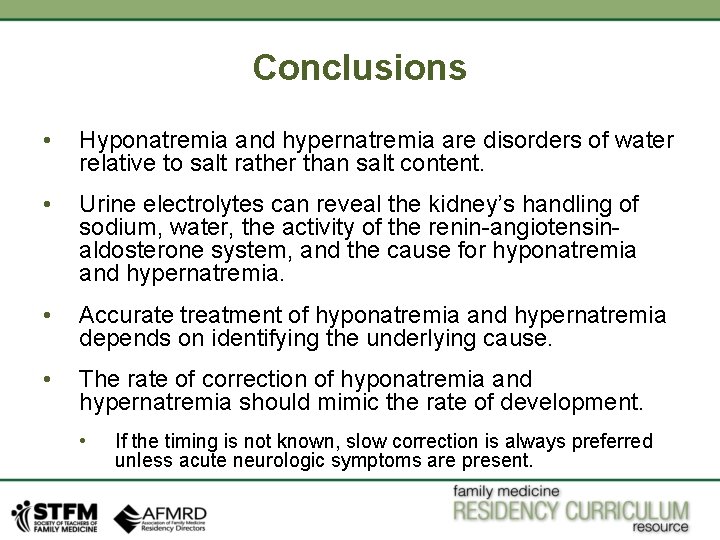
Conclusions • Hyponatremia and hypernatremia are disorders of water relative to salt rather than salt content. • Urine electrolytes can reveal the kidney’s handling of sodium, water, the activity of the renin-angiotensinaldosterone system, and the cause for hyponatremia and hypernatremia. • Accurate treatment of hyponatremia and hypernatremia depends on identifying the underlying cause. • The rate of correction of hyponatremia and hypernatremia should mimic the rate of development. • If the timing is not known, slow correction is always preferred unless acute neurologic symptoms are present.

References Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and Management of Sodium Disorders: Hyponatremia and Hypernatremia. Am Fam Physician. 2015 Mar 1; 91(5): 299– 307 Goh KP. Management of Hyponatremia. Am Fam Physician, 2004 May 15; 69 (10): 2387– 2394. Huang WY, Weng WC, Peng TL, et al. Central Pontine and extrapontine myelinolysis after rapid correction of hyponatremia by hemodialysis in a uremic patient. Ren Fail. 2007; 29 (5): 635– 638. Pepin J, Shields C. Advances in Diagnosis and Management of Hypokalemic and Hyperkalemic Emergencies. EBMedicine. net. 2012 February (14): 1– 20. Pfenning C, Slovis C. Sodium Disorders In The Emergency Department: A Review of Hyponatremia and Hypernatremia. EBMedicine. net. 2012 October (14): 1– 12. Reddy P, Mooradian AD. Diagnosis and Management of hyponatraemia in hospitalized patients, Int J Clin Pract, 2009 October; 63, 10, 1494– 1508. Upadhyay A, Jaber BL, Madias NE. Incidence and Prevalence of Hyponatremia, Am J Med. 2006; 119: S 30–S 35. Viera AJ, Wouk N. Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician. 2015 Sep 15; 92(6): 487– 495 Verbalis JG, Goldsmith SR, Greenberg A, et al. Diagnosis, Evaluation, and Treatment of Hyponatremia: Expert Panel Recommendations, Am J Med. 2013 October(126): S 5–S 41.
- Slides: 40