Disorders of the Pancreas Nrsg 407 PANCREAS Exocrine












- Slides: 47

Disorders of the Pancreas Nrsg 407

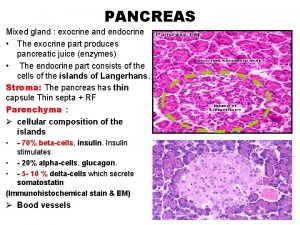
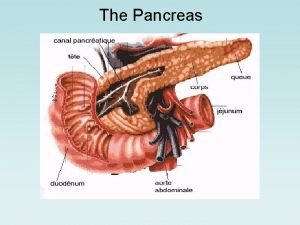
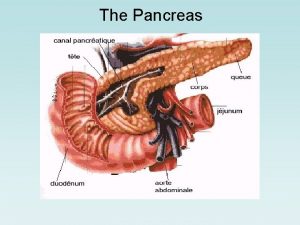
PANCREAS ¡ Exocrine l Secretes digestive enzymes into the small intestines l Breakdown of CHO, protein, and fats ¡ Endocrine l Produces hormones l Insulin l Glucagon
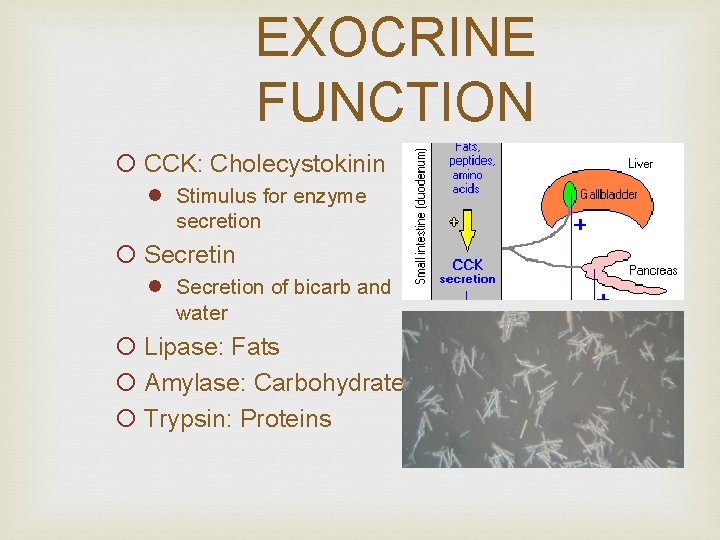
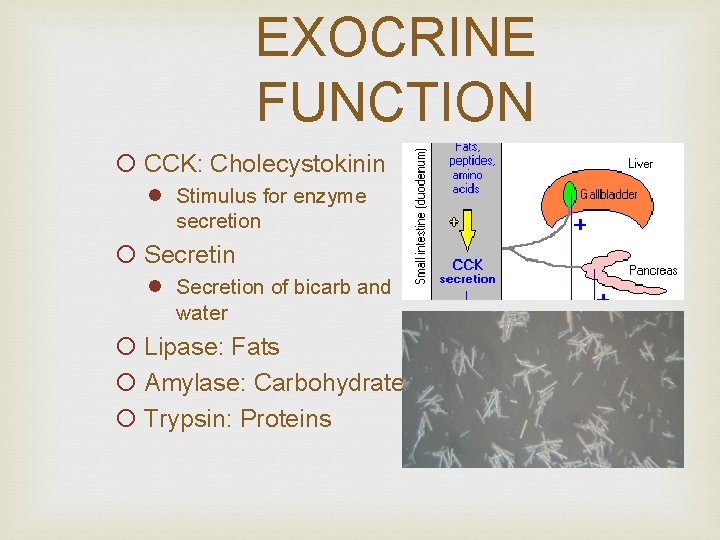
EXOCRINE FUNCTION ¡ CCK: Cholecystokinin l Stimulus for enzyme secretion ¡ Secretin l Secretion of bicarb and water ¡ Lipase: Fats ¡ Amylase: Carbohydrates ¡ Trypsin: Proteins
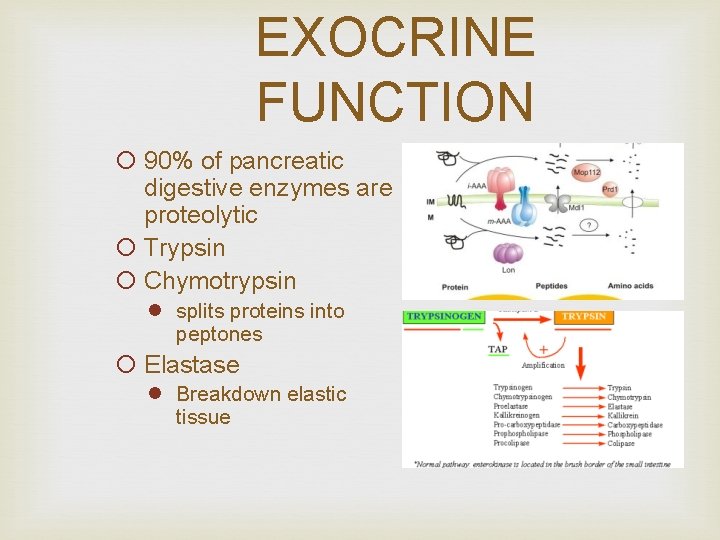
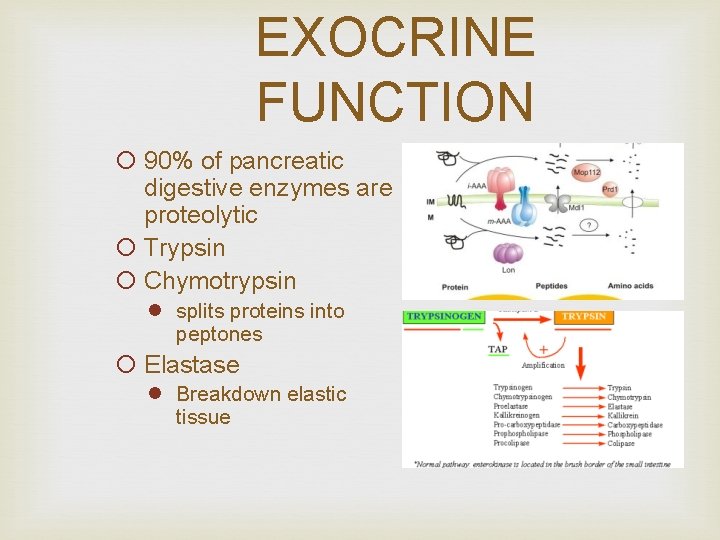
EXOCRINE FUNCTION ¡ 90% of pancreatic digestive enzymes are proteolytic ¡ Trypsin ¡ Chymotrypsin l splits proteins into peptones ¡ Elastase l Breakdown elastic tissue

EXOCRINE FUNCTION ¡ Amylolytic l Breakdown of carbohydrates l Amylase ¡ Lipolytic l Breakdown of fats l Lipase l Phospholipase A
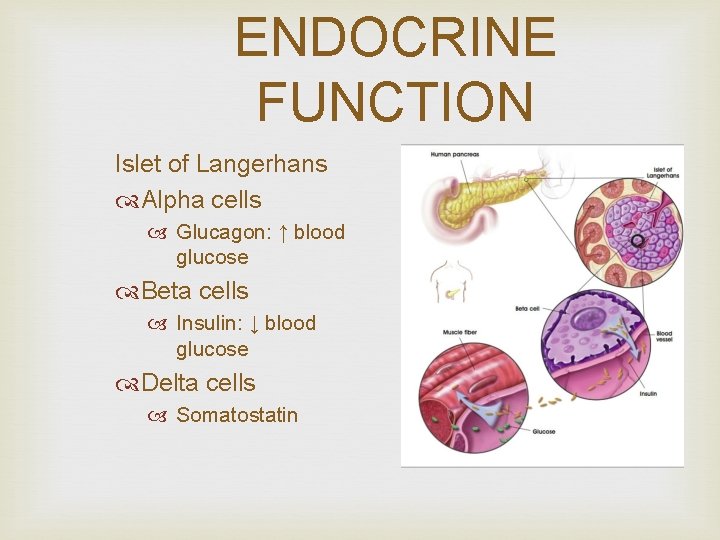
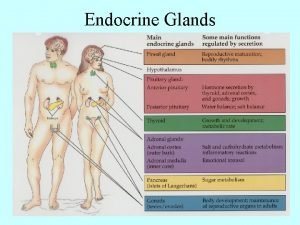
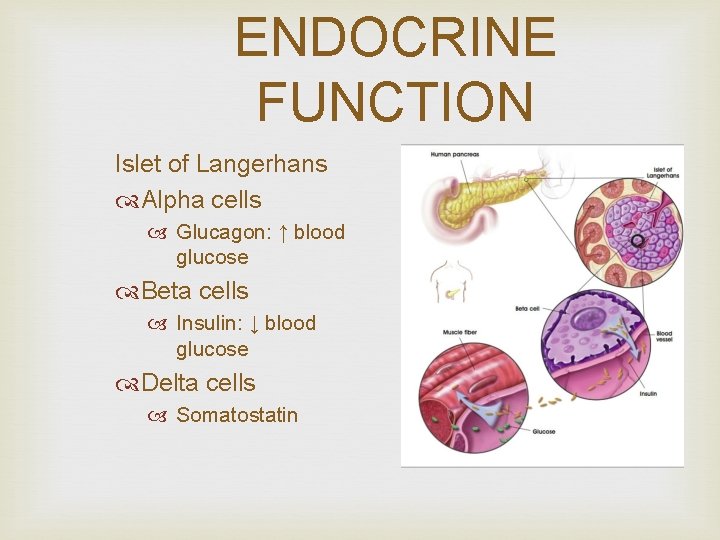
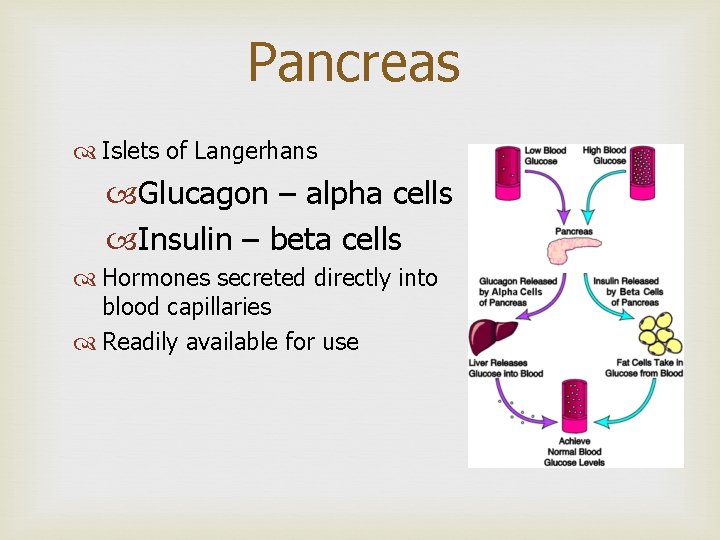
ENDOCRINE FUNCTION Islet of Langerhans Alpha cells Glucagon: ↑ blood glucose Beta cells Insulin: ↓ blood glucose Delta cells Somatostatin
PANCREATITIS ¡ Inflammation of the pancreas ¡ Autodigestion of the pancreas by pancreatic enzymes ¡ Cellular destruction and organ damage
ACUTE PANCREATITS ¡ Acute l Mild or Nonhemorrhagic l Severe or Hemorrhagic l Fulminant
EPIDEMIOLOGY 185, 000 cases each year 150, 000 cholelithiasis or sustained alcohol abuse African-Americans are at ↑ risk
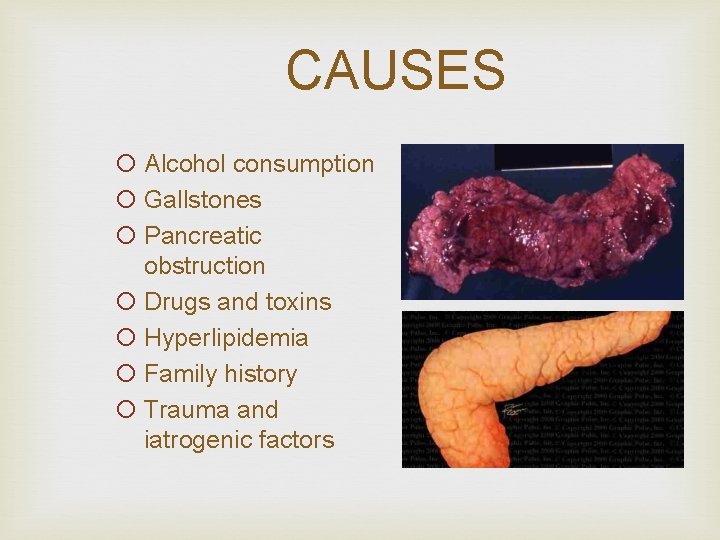
CAUSES ¡ Alcohol consumption ¡ Gallstones ¡ Pancreatic obstruction ¡ Drugs and toxins ¡ Hyperlipidemia ¡ Family history ¡ Trauma and iatrogenic factors
SIGNS and SYMPTOMS ¡ Severe abdominal pain l Epigastrium radiating to midback l Not relieved by vomiting ¡ Fever, malaise ¡ Nausea, vomiting ¡ Rigid and distended ¡ Rebound tenderness ¡ Absent or diminished bowel sounds

SIGNS and SYMPTOMS Dyspnea and Tachypnea Pulmonary infiltrates Grey Turner’s sign Large ecchymosis appearing in the flanks Cullen’s sign Ecchymosis in umbilical area Hypovolemic Shock
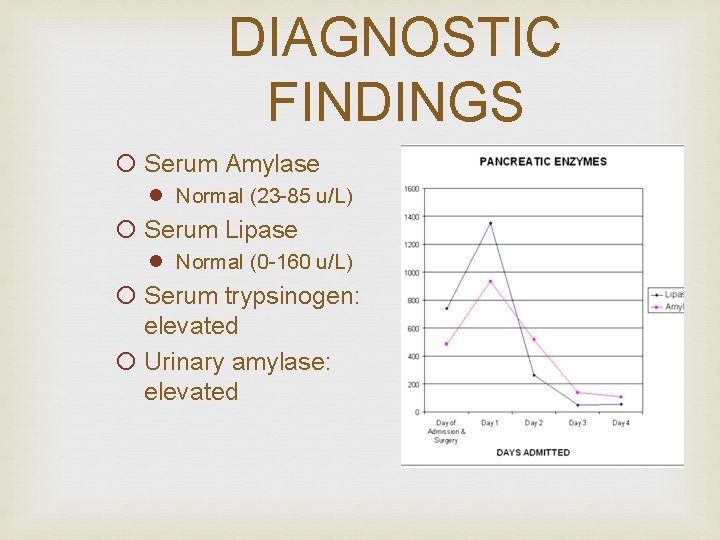
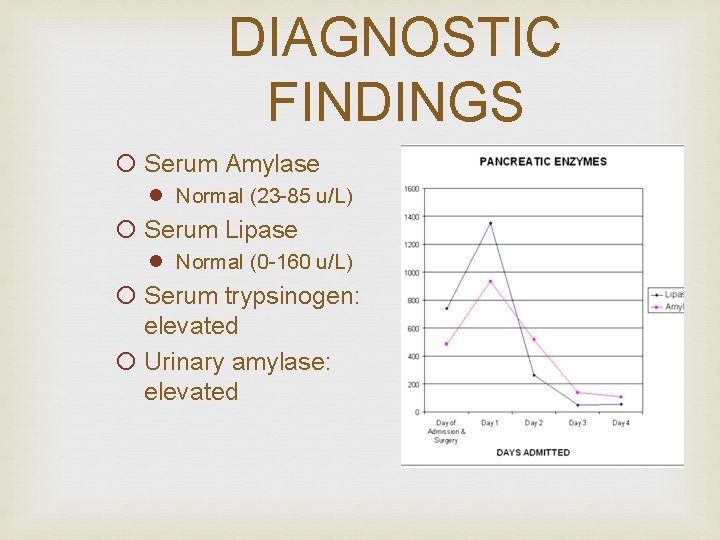
DIAGNOSTIC FINDINGS ¡ Serum Amylase l Normal (23 -85 u/L) ¡ Serum Lipase l Normal (0 -160 u/L) ¡ Serum trypsinogen: elevated ¡ Urinary amylase: elevated
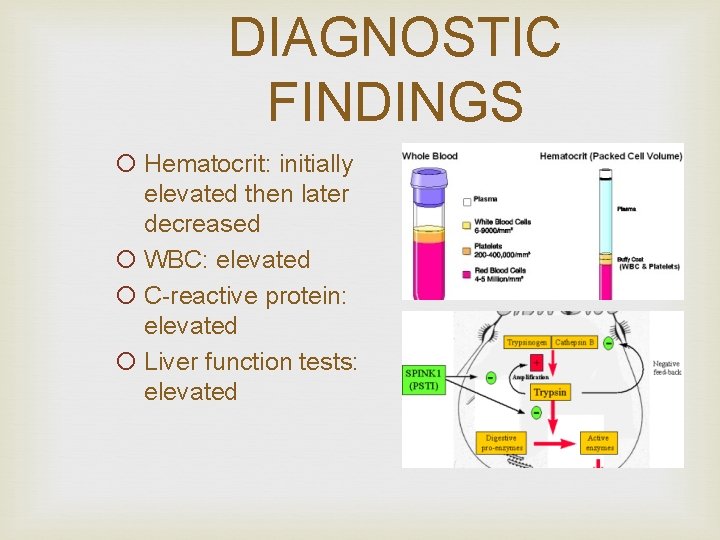
DIAGNOSTIC FINDINGS ¡ Hematocrit: initially elevated then later decreased ¡ WBC: elevated ¡ C-reactive protein: elevated ¡ Liver function tests: elevated
DIAGNOSTIC FINDINGS ¡ Sodium and Potassium: decreased ¡ Blood glucose: elevated ¡ Serum Calcium: decreased ¡ Albumin and Magnesium: decreased

DIAGNOSTIC FINDINGS ¡ Abdominal and Chest X-ray ¡ CT scan, Ultrasound, MRI ¡ Endoscopic Retrograde Cholangiopancreatography (ERCP) ¡ Aspiration biopsy ¡ Stool studies: steatorrhea
COMPLICATIONS ¡ Hypovolemic shock l l 3 rd spacing Hemorrhage Vomiting Decreased protein intake
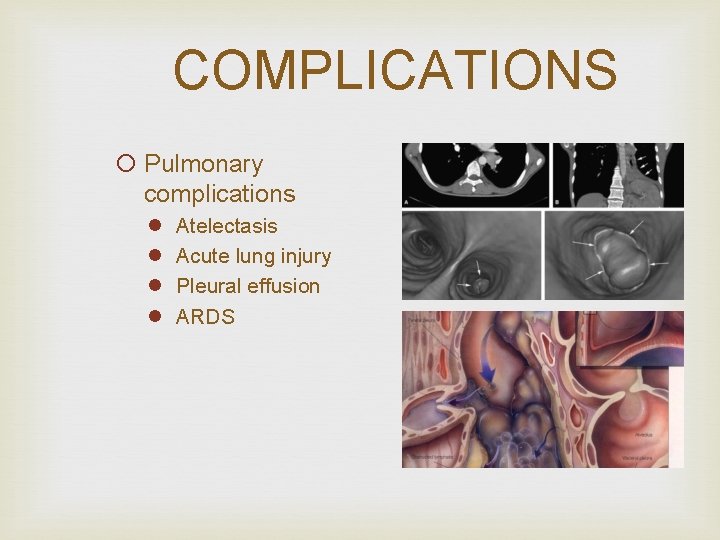
COMPLICATIONS ¡ Pulmonary complications l l Atelectasis Acute lung injury Pleural effusion ARDS
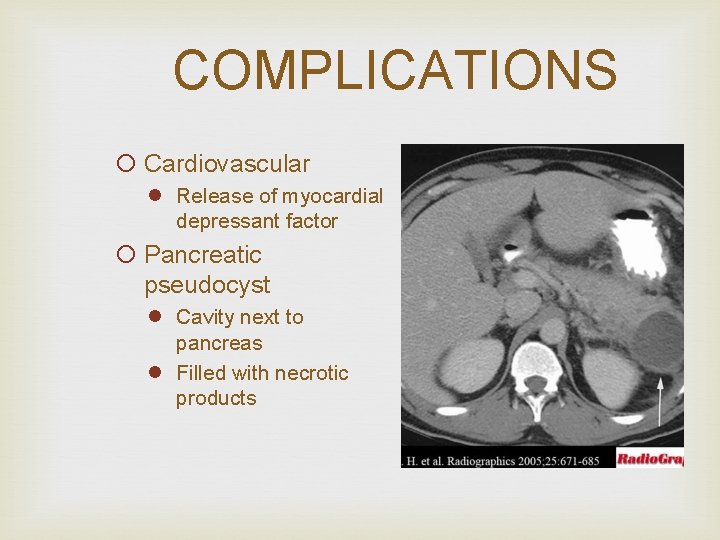
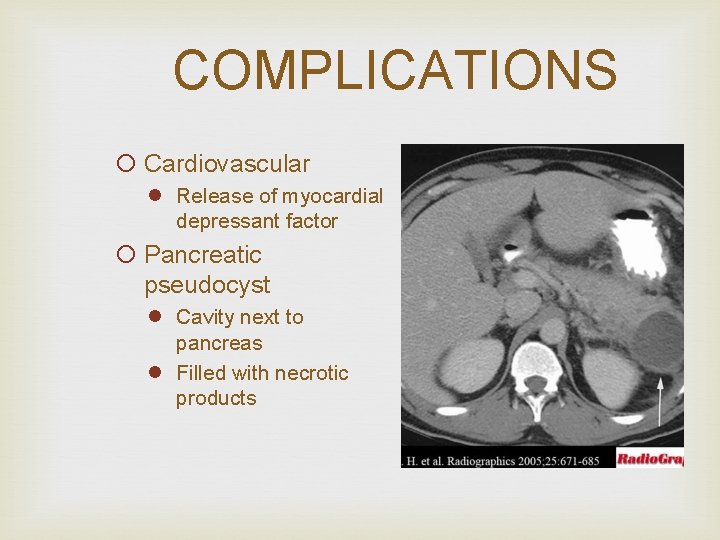
COMPLICATIONS ¡ Cardiovascular l Release of myocardial depressant factor ¡ Pancreatic pseudocyst l Cavity next to pancreas l Filled with necrotic products
COMPLICATIONS ¡ Pancreatic abscess l 2 -4 weeks after episode l Necrosis of tissue l Relocation of bacteria ¡ Hypocalcaemia can occur with severe disease
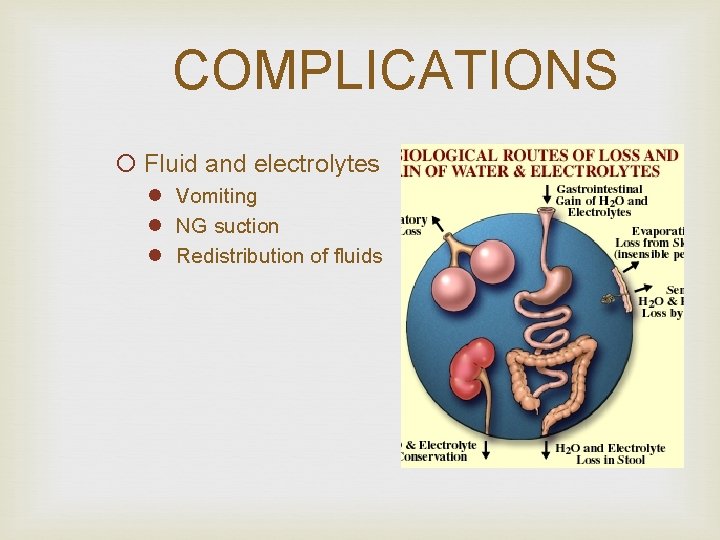
COMPLICATIONS ¡ Fluid and electrolytes l Vomiting l NG suction l Redistribution of fluids
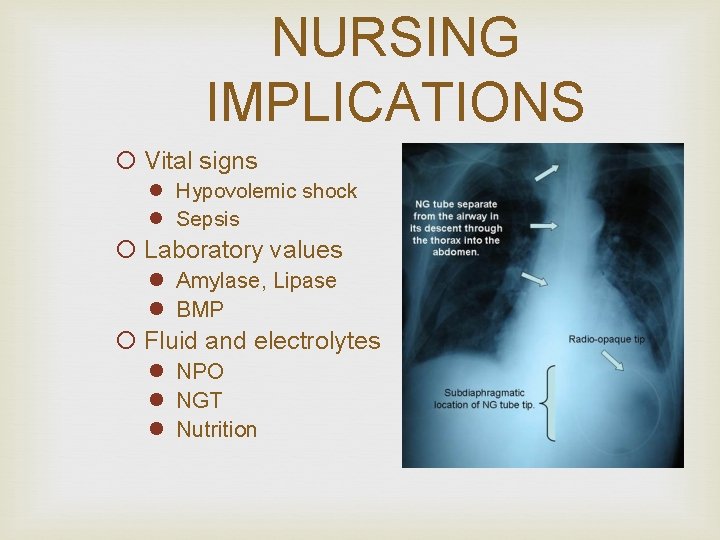
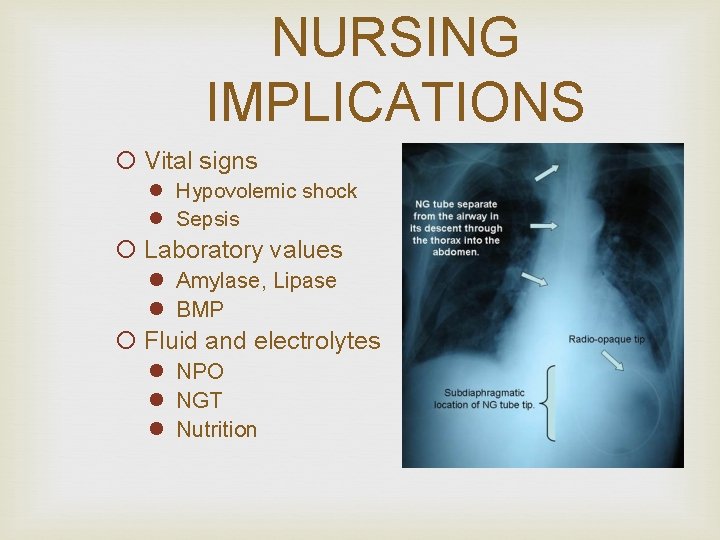
NURSING IMPLICATIONS ¡ Vital signs l Hypovolemic shock l Sepsis ¡ Laboratory values l Amylase, Lipase l BMP ¡ Fluid and electrolytes l NPO l NGT l Nutrition
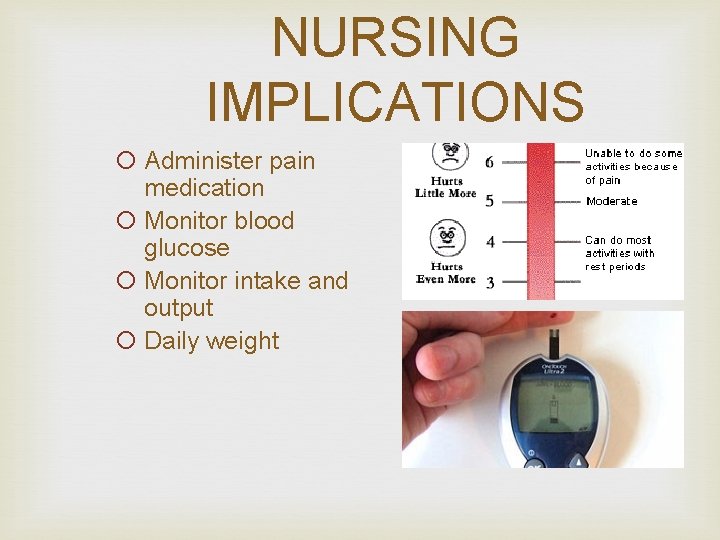
NURSING IMPLICATIONS ¡ Administer pain medication ¡ Monitor blood glucose ¡ Monitor intake and output ¡ Daily weight

CHRONIC PANCREATITIS ¡ Persistent inflammation of the pancreas ¡ Scarring and calcification of the pancreatic ducts
CAUSES ¡ 70% is caused by alcohol abuse ¡ 20% is caused by obstruction, trauma, metabolic disturbances
SIGNS & SYMPTOMS ¡ 80% of pancreatic destruction causes l Malabsorption resulting in nutritional deficits l Diarrhea and steatorrhea l Impaired glucose regulation
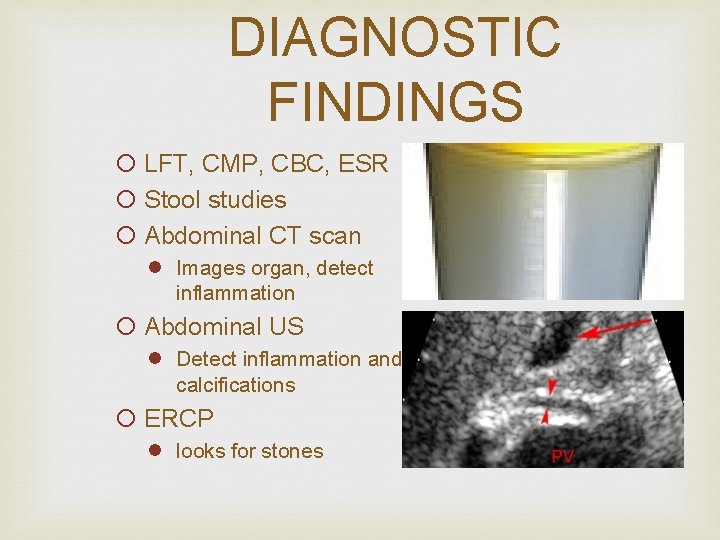
DIAGNOSTIC FINDINGS ¡ LFT, CMP, CBC, ESR ¡ Stool studies ¡ Abdominal CT scan l Images organ, detect inflammation ¡ Abdominal US l Detect inflammation and calcifications ¡ ERCP l looks for stones
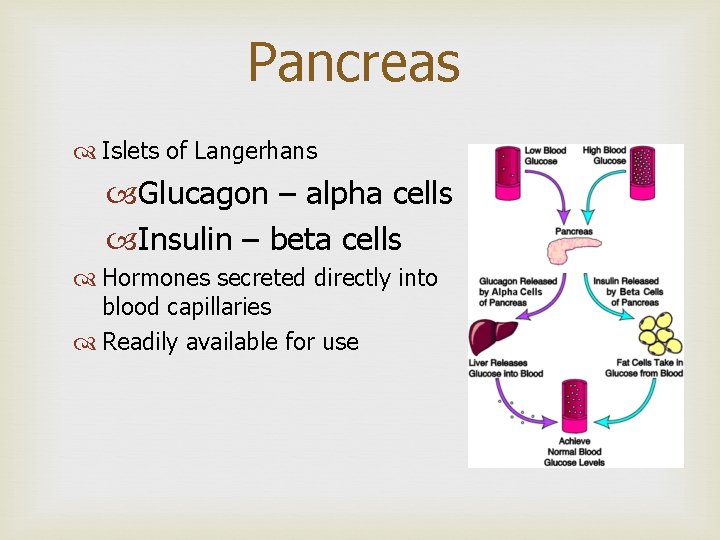
Pancreas Islets of Langerhans Glucagon – alpha cells Insulin – beta cells Hormones secreted directly into blood capillaries Readily available for use
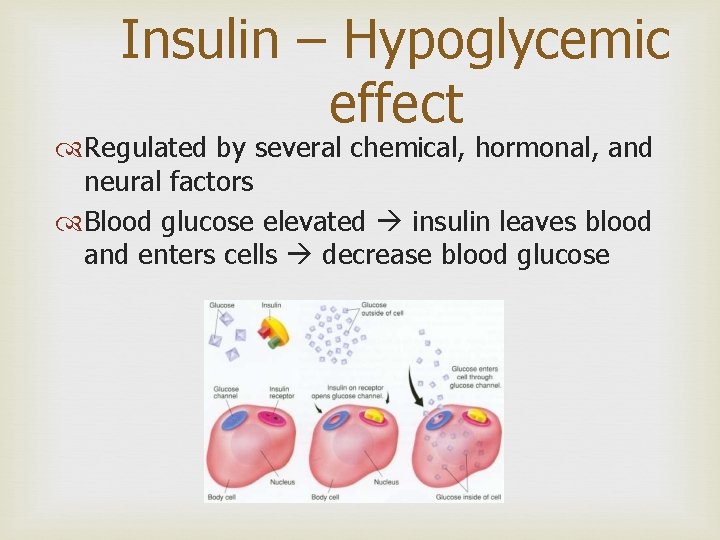
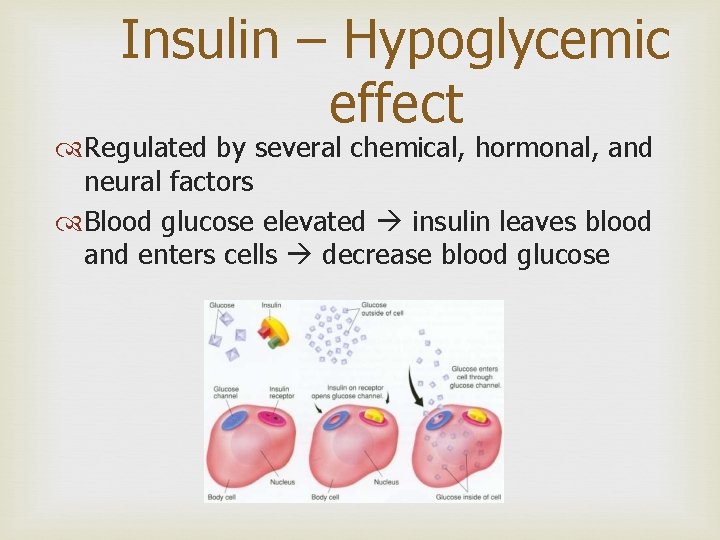
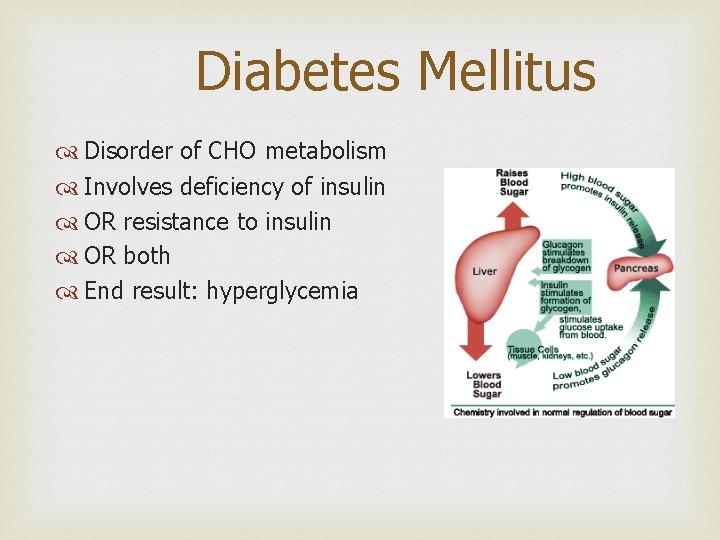
Insulin – Hypoglycemic effect Regulated by several chemical, hormonal, and neural factors Blood glucose elevated insulin leaves blood and enters cells decrease blood glucose

Insulin Affects CHO, lipid, and protein metabolism Assists in glucose transport Causes glucose to leave blood Serum glucose will fall
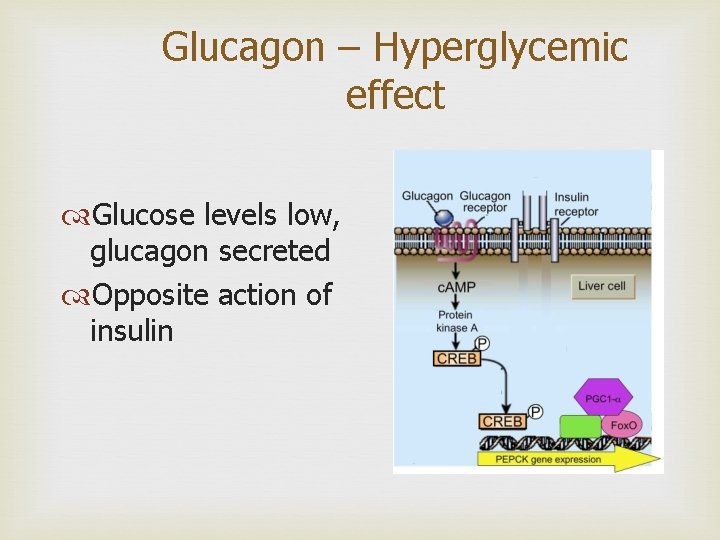
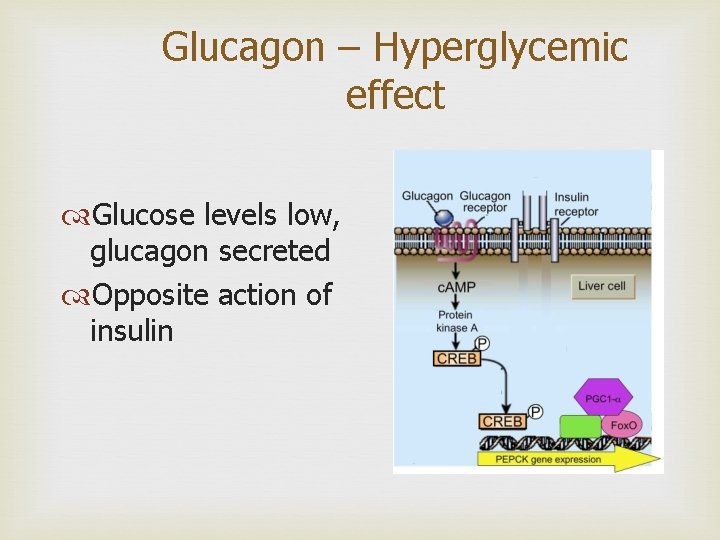
Glucagon – Hyperglycemic effect Glucose levels low, glucagon secreted Opposite action of insulin

DIABETES Disorder of insulin action or secretion (usually both) Results in high blood glucose Two different types of diabetes: Type I Autoimmune disorder Type II Multifactorial disease
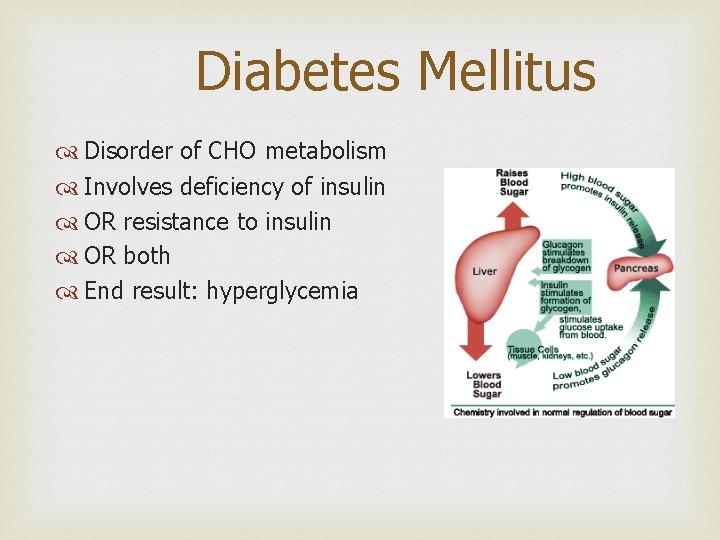
Diabetes Mellitus Disorder of CHO metabolism Involves deficiency of insulin OR resistance to insulin OR both End result: hyperglycemia
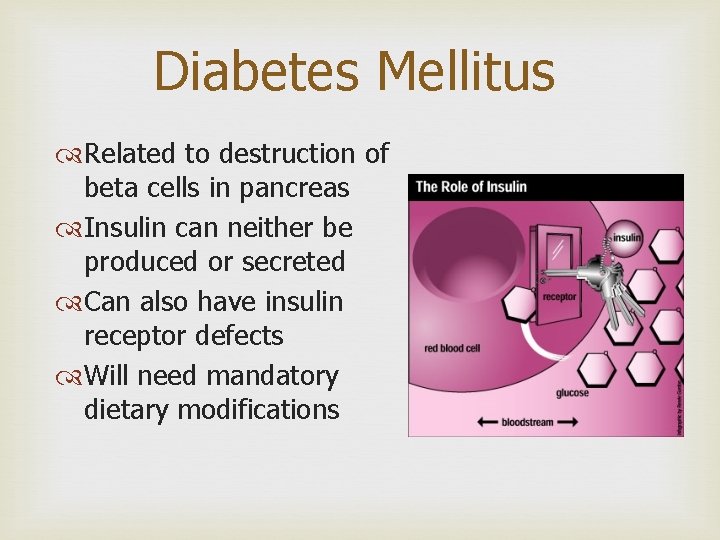
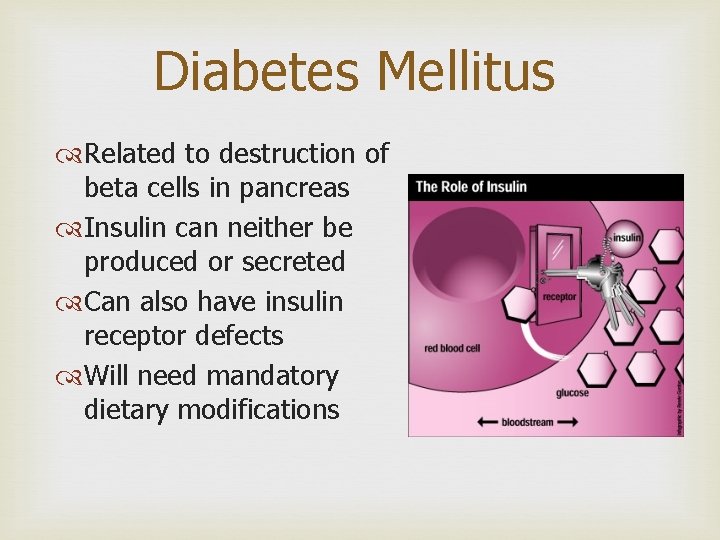
Diabetes Mellitus Related to destruction of beta cells in pancreas Insulin can neither be produced or secreted Can also have insulin receptor defects Will need mandatory dietary modifications

Type I DM Considered juvenile – usually under 30 y/o Sudden onset of symptoms Usually not obese Autoimmune response destroys beta cells
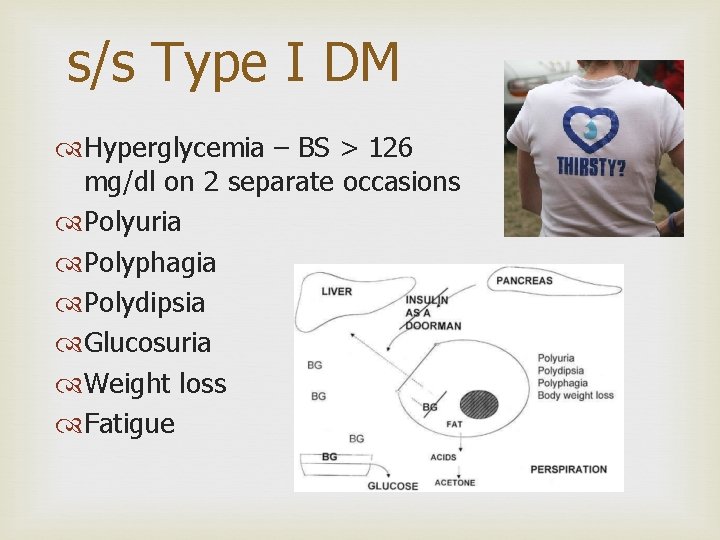
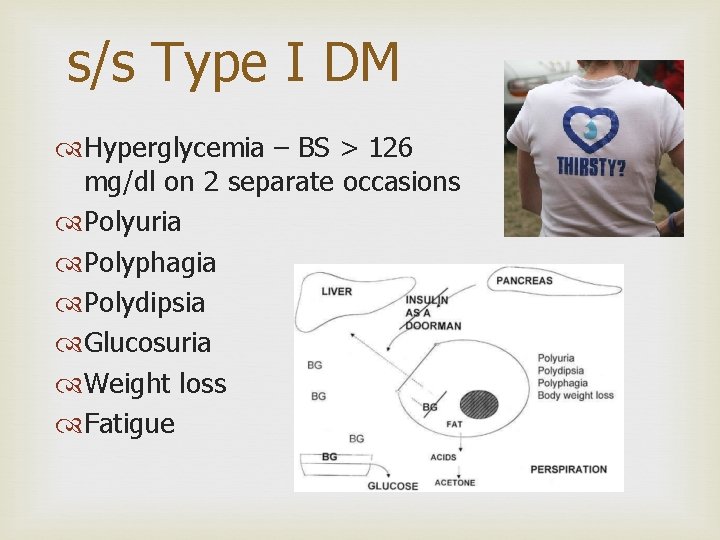
s/s Type I DM Hyperglycemia – BS > 126 mg/dl on 2 separate occasions Polyuria Polyphagia Polydipsia Glucosuria Weight loss Fatigue
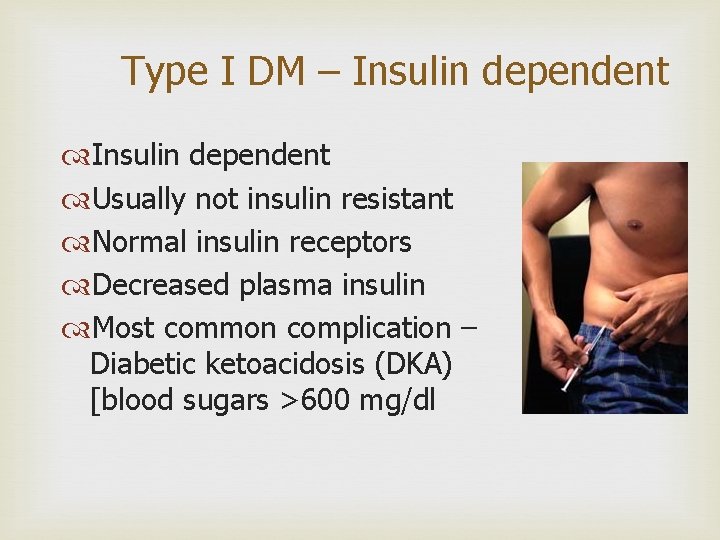
Type I DM – Insulin dependent Usually not insulin resistant Normal insulin receptors Decreased plasma insulin Most common complication – Diabetic ketoacidosis (DKA) [blood sugars >600 mg/dl

Untreated DM Long-term damage to arteries Heart disease Stroke Kidney disease Blindness Peripheral neuropathy

Diagnosis Classic symptoms: Increased urination, increased thirst, and unexplained weight loss plus random blood glucose ≥ 200 mg/d. L OR Fasting (8 hours+) ≥ 126 mg/d. L OR Blood glucose ≥ 200 mg/d. L two hours after a standard carbohydrate load Oral Glucose tolerance (OGTT) Any glucose ≥ 200 mg/d. L Exception: someone receiving IV infusion of glucose
Type I Autoimmune destruction of beta cells causes a decrease in or absence of insulin production by islets of Langerhans Islets are infiltrated by T lymphocytes Has genetic component Environmental factors also play a role
Type II Mixture of genetic and environmental factors Obesity is the underlying cause of most type II diabetes Also lifestyle factors play an important role Is characterized by: Decreased sensitivity of peripheral cells to the effect of insulin (insulin resistance) Beta-cell dysfunction that prevents adequate insulin response to decreased peripheral cell sensitivity and high blood glucose
Secondary Type II Due to causes other than obesity Pregnancy Drug therapy (steroids, Cushing disease) Diabetes usually will disappear when underlying condition is corrected
Diabetic Complications Excessive glucose binds to extracellular proteins to form abnormal glycoproteins that negatively impact vascular endothelium Increases inflammation Promotes thrombosis Loosens endothelial cells Stimulates proliferation of vascular smooth muscle cells (atherosclerosis) Promotes vascular disease
Complications cont’d High intracellular glucose results in increased oxidative stress (diabetic neuropathy) Also stimulates production of mediators that: Stimulate growth of new blood vessels (diabetic retinal disease) Promote thrombosis Promotes vascular inflammation Promotes vasoconstriction
Diabetic Ketoacidosis Acidosis occurs due to absence of insulin because in the absence of glucose, body must burn fat for fuel Fat is broken down into fatty acids-transported to liver and converted into ketones to be burned for fuel Lowers blood p. H Present mainly with Type I diabetes

Long-Term Complications of DM Usually seen 15 -20 years after onset of hyperglycemia Infections: due to impaired neutrophil & macrophage function and impaired delivery of circulating cells and molecules necessary for host defense Vascular disease relating complications: Atherosclerosis (increases risk of MI, stroke, lower extremity gangrene) Diabetic retinopathy Diabetic nephropathy Diabetic neuropathy
Treatment Lifestyle changes Type I: insulin replacement Type II: oral hypoglycemic drug to increase insulin secretion, insulin or both
 Nrsg 374 assignment 1
Nrsg 374 assignment 1 Intraductal papillary mucinous neoplasm
Intraductal papillary mucinous neoplasm Is bile in pancreatic juice
Is bile in pancreatic juice Emirates 407
Emirates 407 Csc 407
Csc 407 Frases indicativas
Frases indicativas Ent407
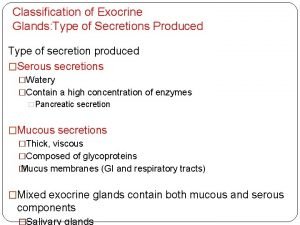
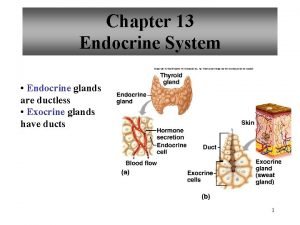
Ent407 Exocrine glands
Exocrine glands Exocrine cell signaling
Exocrine cell signaling Glandes tubuleuses droites
Glandes tubuleuses droites Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands Kelenjar endokrin
Kelenjar endokrin Kliere
Kliere Exocrine glands function
Exocrine glands function Endocrine exocrine
Endocrine exocrine Acinar alveolar
Acinar alveolar Ap biology chapter 40
Ap biology chapter 40 Difference between endocrine and exocrine glands
Difference between endocrine and exocrine glands The only example of unicellular exocrine glands are
The only example of unicellular exocrine glands are Canine exocrine pancreatic insufficiency
Canine exocrine pancreatic insufficiency Classification of exocrine glands
Classification of exocrine glands Exocrine glands
Exocrine glands Glande endocrine exocrine
Glande endocrine exocrine Are endocrine glands ductless
Are endocrine glands ductless Endocrine vs exocrine
Endocrine vs exocrine Cardiac muscle striations
Cardiac muscle striations Merocrine gland
Merocrine gland Tissue
Tissue Multicellular exocrine glands can be classified
Multicellular exocrine glands can be classified điện thế nghỉ
điện thế nghỉ Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Chó sói
Chó sói Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Tia chieu sa te
Tia chieu sa te Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Ng-html
Ng-html Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết Số nguyên tố là số gì
Số nguyên tố là số gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Thang điểm glasgow
Thang điểm glasgow ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin