Disorders of Hemostasis Sultana Qureshi PGY2 Resident Rounds
















- Slides: 57
Disorders of Hemostasis Sultana Qureshi, PGY-2 Resident Rounds March 1, 2007 Thanks to Adam Oster for some slides!

Goals Approach and when to be suspicious n Pattern of presentation n ED Management – when to use blood products n

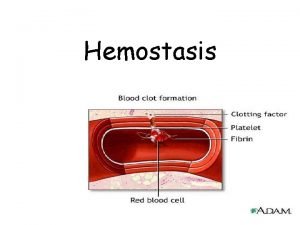
Hemostasis Endothelial cells n Platelets n Blood flow & vasoconstrictors n Clotting cascade n Fibrinolysis n

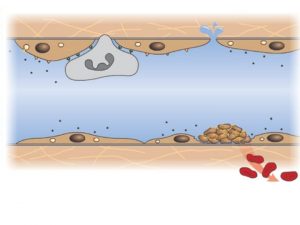
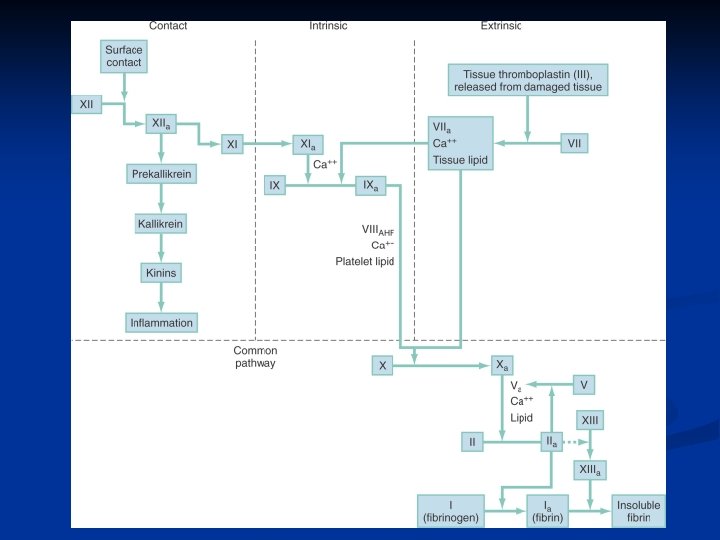
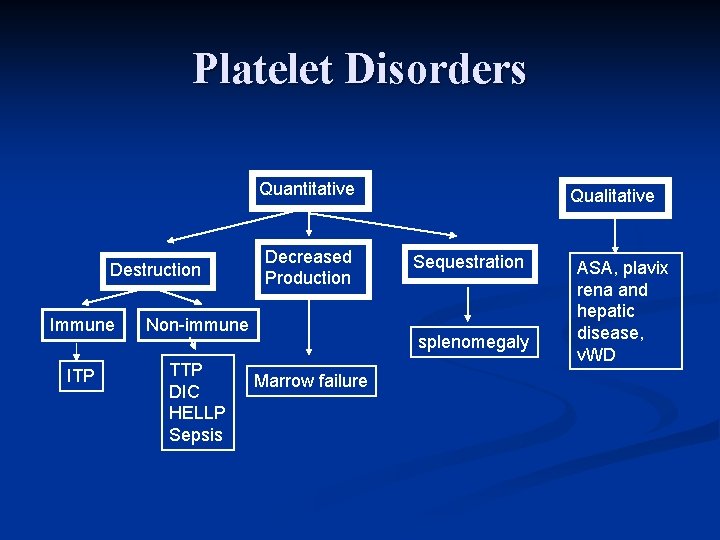
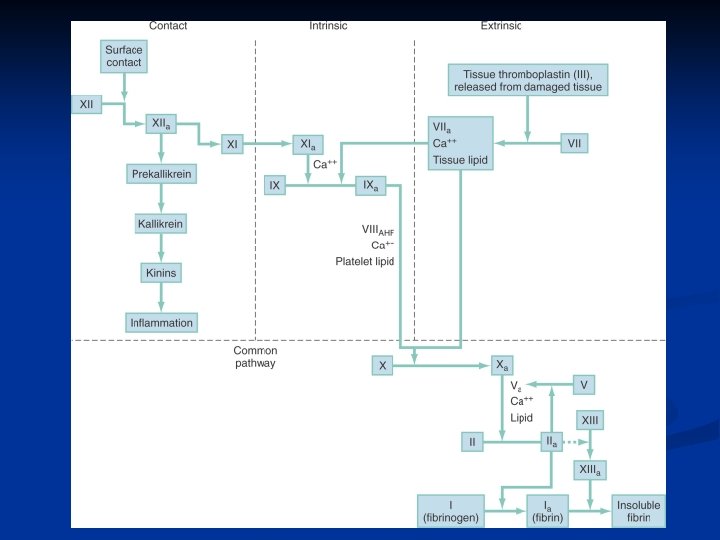
Approach to Bleeding Disorders n Primary Hemostasis n n Exposed endothelial cells cause platelets to aggregate and form plug Platelet Disorders n n n ITP TTP Also partially in liver disease, v. WD n Secondary Hemostasis n n n Tissue factor iniates coagulation cascade eventually leading to fibrinogen forming fibrin cross links Extrinsic starts pathway, intrinsic sustains Coagulation Disorders n n n v. WD Hemophilia A & B Other – consumptive (DIC)

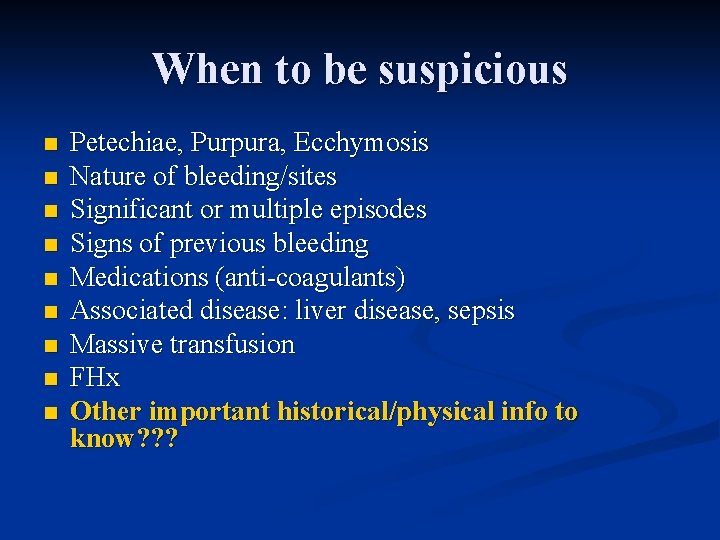
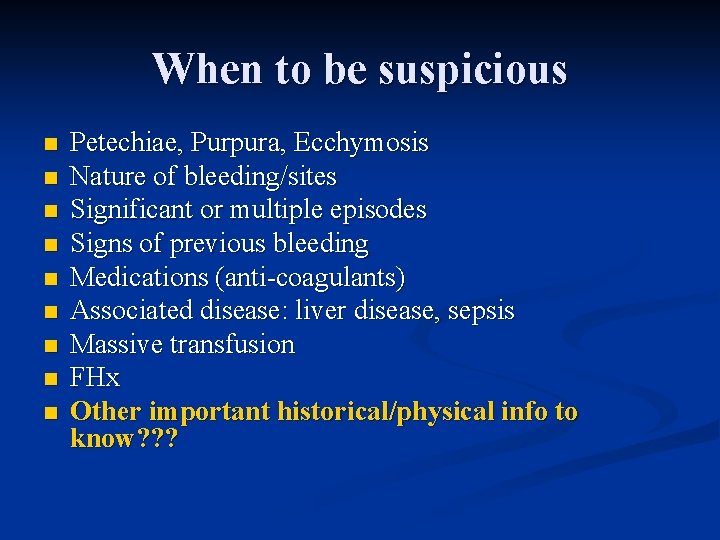
When to be suspicious n n n n n Petechiae, Purpura, Ecchymosis Nature of bleeding/sites Significant or multiple episodes Signs of previous bleeding Medications (anti-coagulants) Associated disease: liver disease, sepsis Massive transfusion FHx Other important historical/physical info to know? ? ?
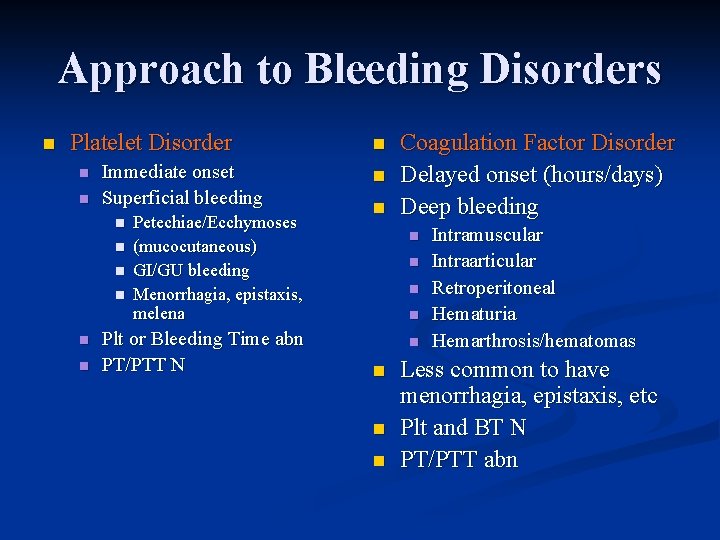
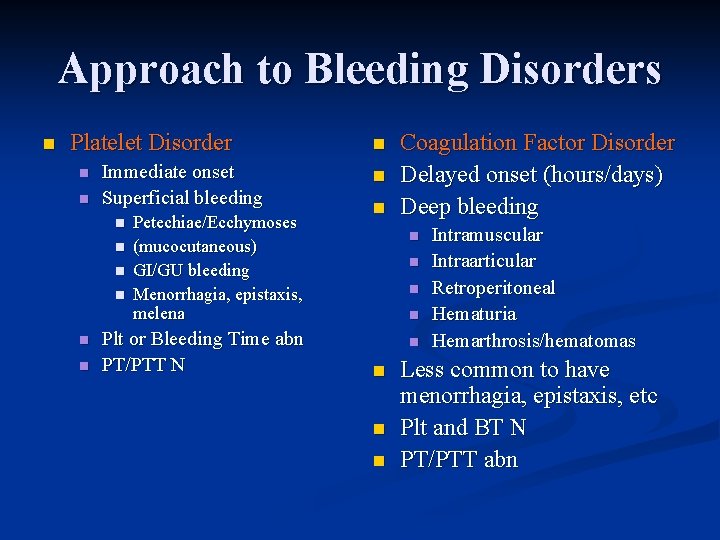
Approach to Bleeding Disorders n Platelet Disorder n n Immediate onset Superficial bleeding n n n Petechiae/Ecchymoses (mucocutaneous) GI/GU bleeding Menorrhagia, epistaxis, melena Plt or Bleeding Time abn PT/PTT N n n n Coagulation Factor Disorder Delayed onset (hours/days) Deep bleeding n n n n Intramuscular Intraarticular Retroperitoneal Hematuria Hemarthrosis/hematomas Less common to have menorrhagia, epistaxis, etc Plt and BT N PT/PTT abn
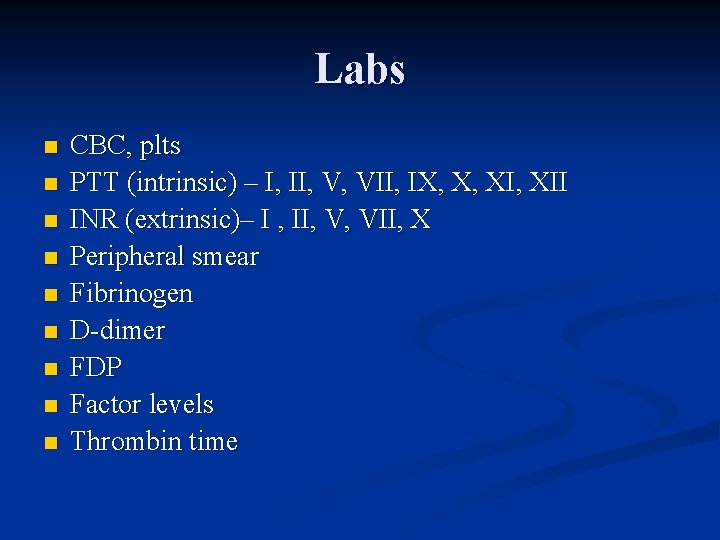
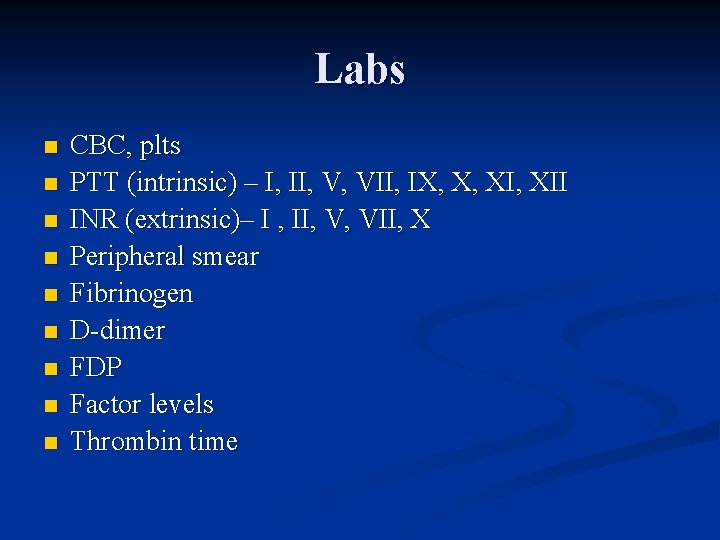
Labs n n n n n CBC, plts PTT (intrinsic) – I, II, V, VII, IX, X, XII INR (extrinsic)– I , II, V, VII, X Peripheral smear Fibrinogen D-dimer FDP Factor levels Thrombin time
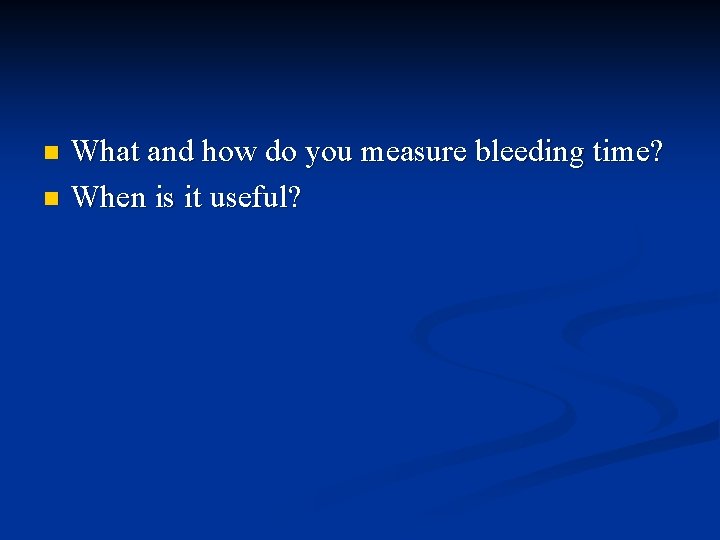
What and how do you measure bleeding time? n When is it useful? n

Blood Products Platelets – 1 unit raise value by 5 -10 n Cryoprecipitate – FVIII, v. WF, fibrinogen, fibronectin n FFP – contains all coagulation factors (about 7% of a 70 kg person) n

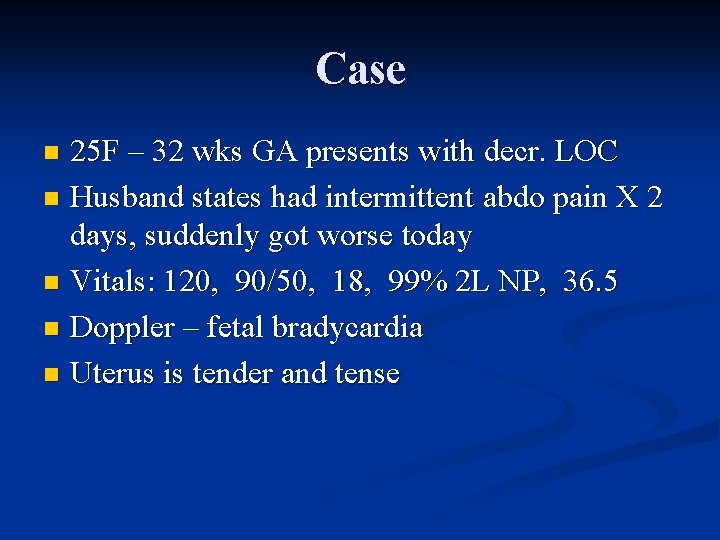
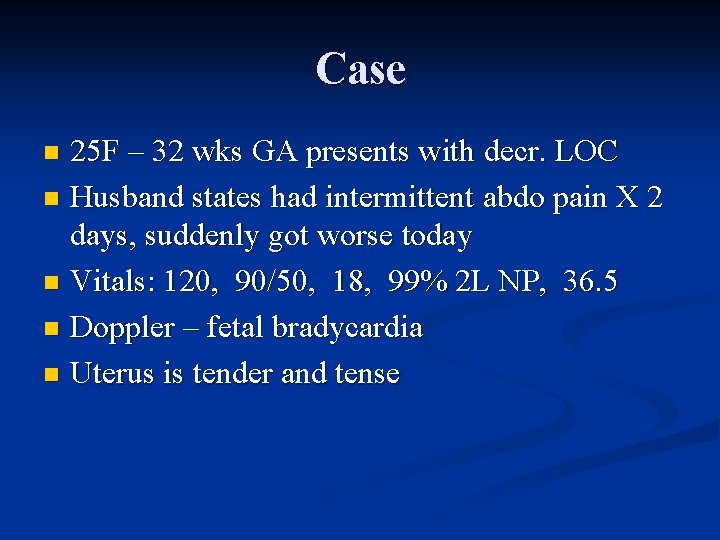
Case 25 F – 32 wks GA presents with decr. LOC n Husband states had intermittent abdo pain X 2 days, suddenly got worse today n Vitals: 120, 90/50, 18, 99% 2 L NP, 36. 5 n Doppler – fetal bradycardia n Uterus is tender and tense n

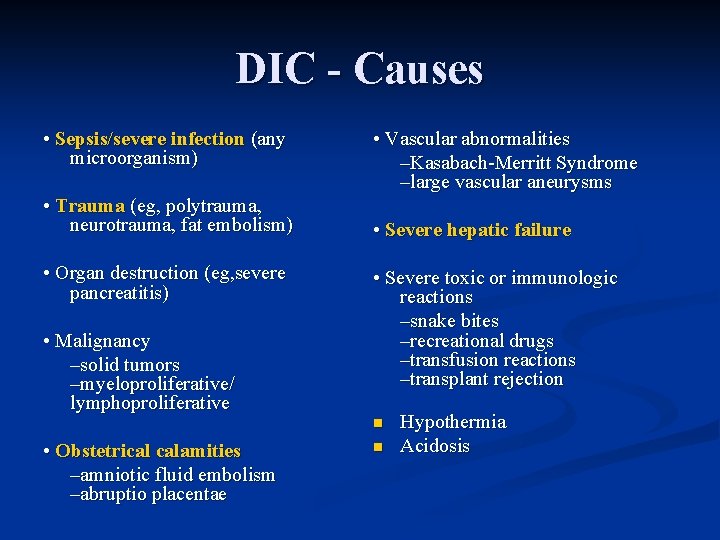
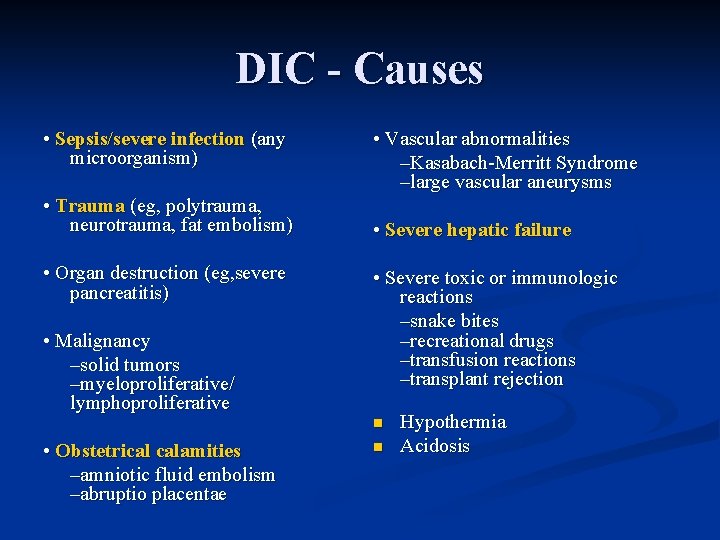
DIC - Causes • Sepsis/severe infection (any microorganism) • Trauma (eg, polytrauma, neurotrauma, fat embolism) • Organ destruction (eg, severe pancreatitis) • Malignancy –solid tumors –myeloproliferative/ lymphoproliferative • Vascular abnormalities –Kasabach-Merritt Syndrome –large vascular aneurysms • Severe hepatic failure • Severe toxic or immunologic reactions –snake bites –recreational drugs –transfusion reactions –transplant rejection n • Obstetrical calamities –amniotic fluid embolism –abruptio placentae n Hypothermia Acidosis
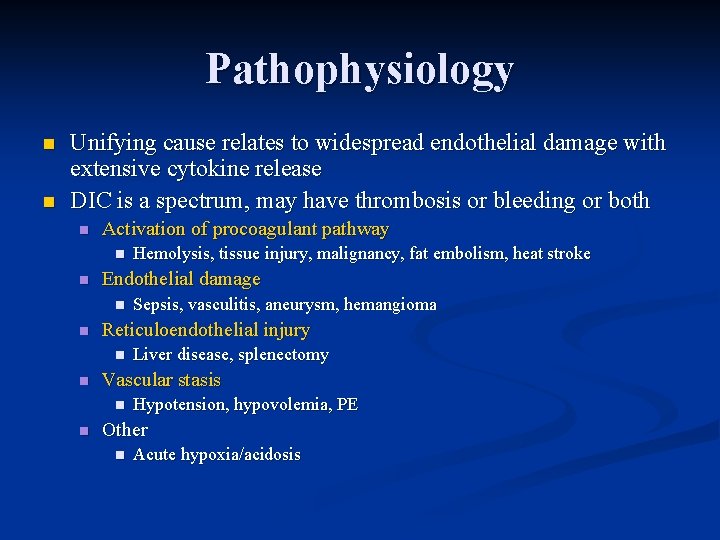
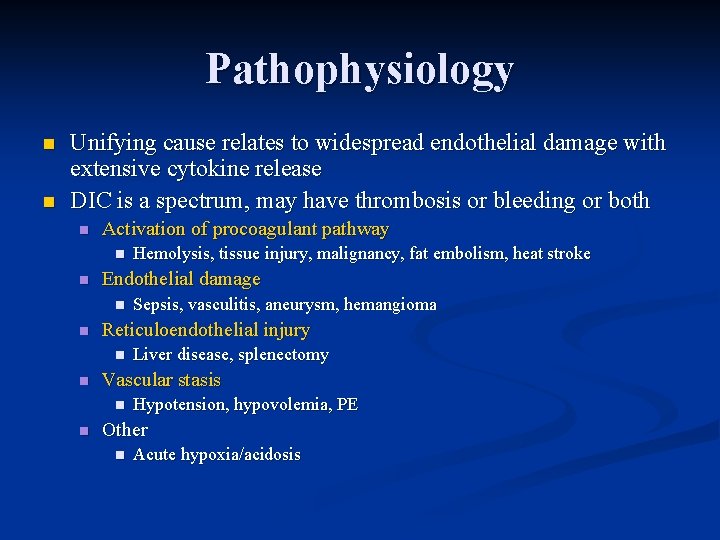
Pathophysiology n n Unifying cause relates to widespread endothelial damage with extensive cytokine release DIC is a spectrum, may have thrombosis or bleeding or both n Activation of procoagulant pathway n n Endothelial damage n n Liver disease, splenectomy Vascular stasis n n Sepsis, vasculitis, aneurysm, hemangioma Reticuloendothelial injury n n Hemolysis, tissue injury, malignancy, fat embolism, heat stroke Hypotension, hypovolemia, PE Other n Acute hypoxia/acidosis
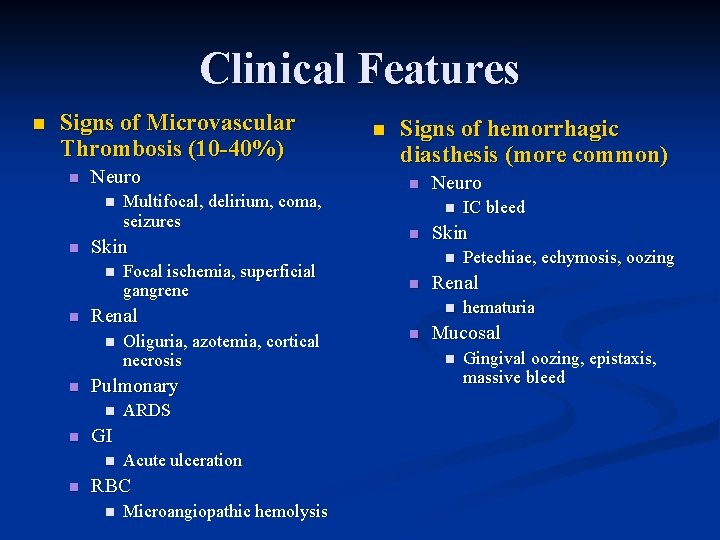
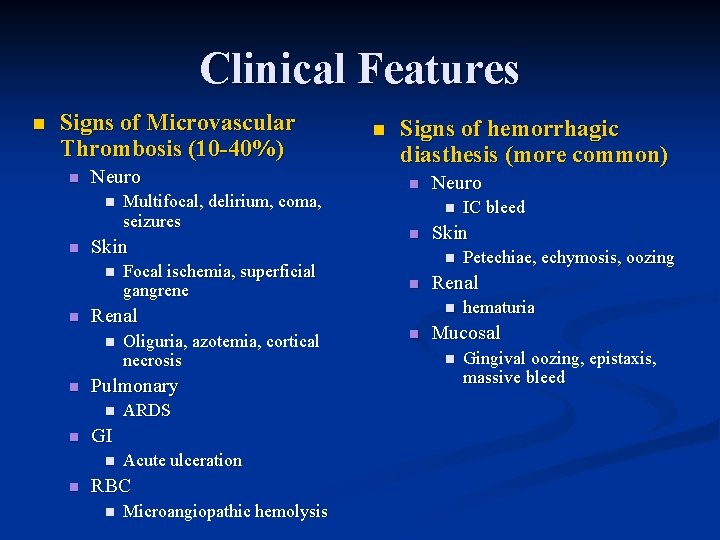
Clinical Features n Signs of Microvascular Thrombosis (10 -40%) n Neuro n n Skin n n ARDS GI n n Oliguria, azotemia, cortical necrosis Pulmonary n n Focal ischemia, superficial gangrene Renal n n Multifocal, delirium, coma, seizures Acute ulceration RBC n Microangiopathic hemolysis n Signs of hemorrhagic diasthesis (more common) n Neuro n n Skin n n Petechiae, echymosis, oozing Renal n n IC bleed hematuria Mucosal n Gingival oozing, epistaxis, massive bleed
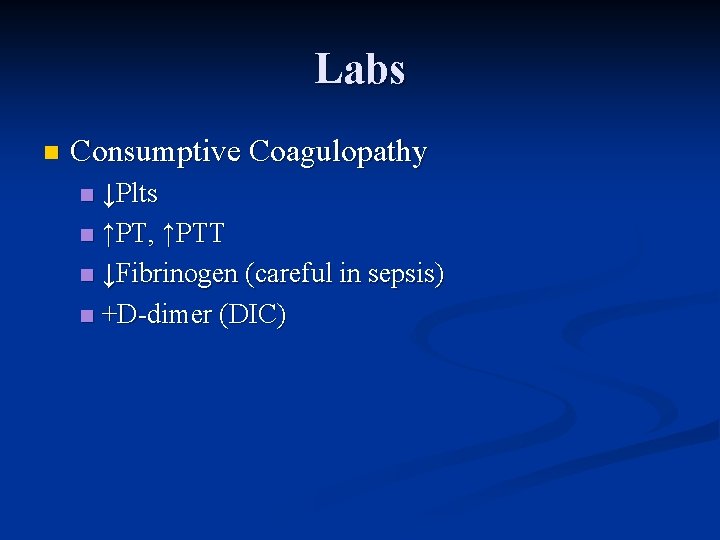
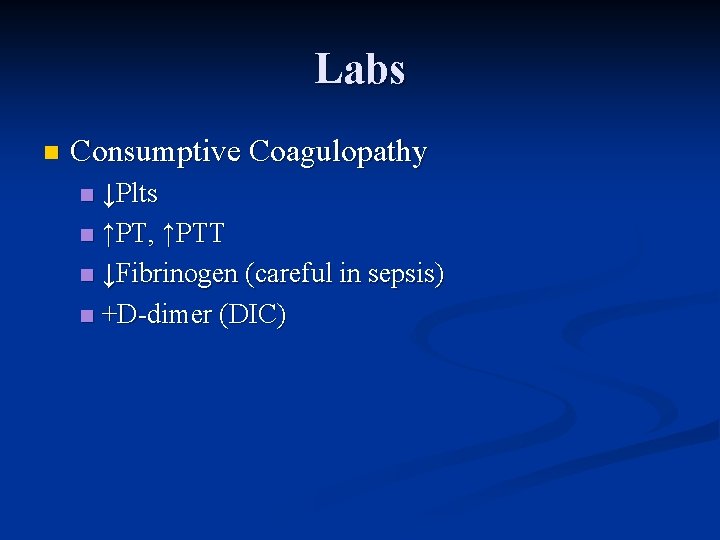
Labs n Consumptive Coagulopathy ↓Plts n ↑PT, ↑PTT n ↓Fibrinogen (careful in sepsis) n +D-dimer (DIC) n
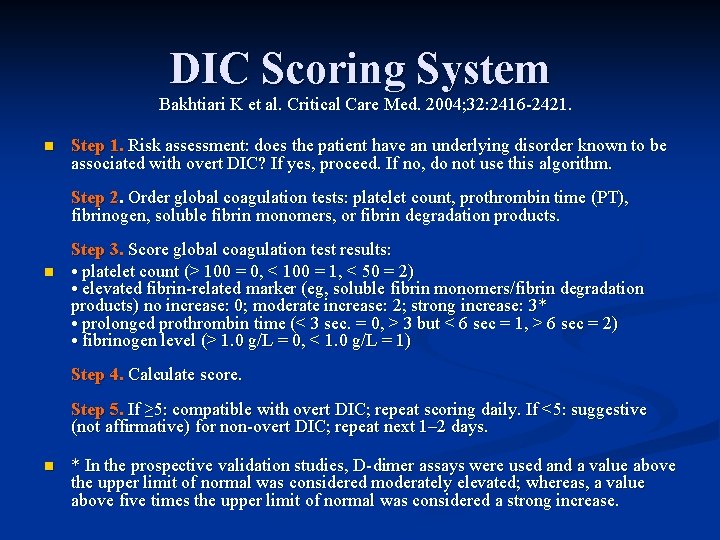
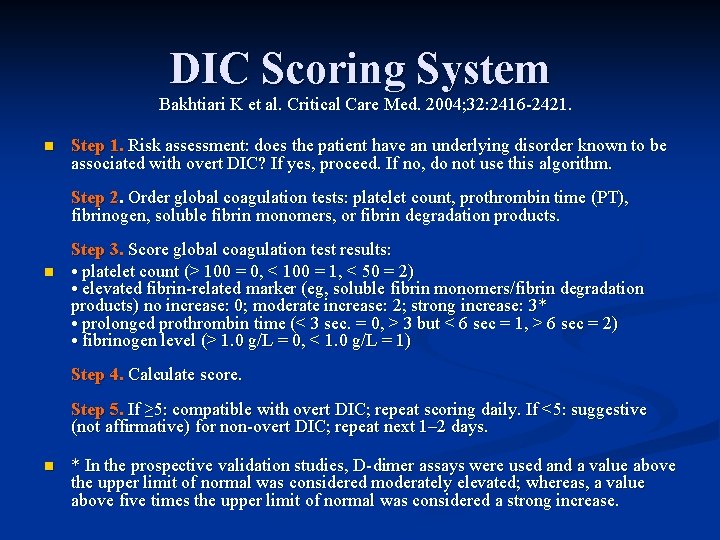
DIC Scoring System Bakhtiari K et al. Critical Care Med. 2004; 32: 2416 -2421. n Step 1. Risk assessment: does the patient have an underlying disorder known to be associated with overt DIC? If yes, proceed. If no, do not use this algorithm. Step 2. Order global coagulation tests: platelet count, prothrombin time (PT), fibrinogen, soluble fibrin monomers, or fibrin degradation products. n Step 3. Score global coagulation test results: • platelet count (> 100 = 0, < 100 = 1, < 50 = 2) • elevated fibrin-related marker (eg, soluble fibrin monomers/fibrin degradation products) no increase: 0; moderate increase: 2; strong increase: 3* • prolonged prothrombin time (< 3 sec. = 0, > 3 but < 6 sec = 1, > 6 sec = 2) • fibrinogen level (> 1. 0 g/L = 0, < 1. 0 g/L = 1) Step 4. Calculate score. Step 5. If ≥ 5: compatible with overt DIC; repeat scoring daily. If <5: suggestive (not affirmative) for non-overt DIC; repeat next 1– 2 days. n * In the prospective validation studies, D-dimer assays were used and a value above the upper limit of normal was considered moderately elevated; whereas, a value above five times the upper limit of normal was considered a strong increase.

DIC Scoring System Bakhtiari K et al. Critical Care Med. 2004; 32: 2416 -2421. n n Sens 93% Spec 96%
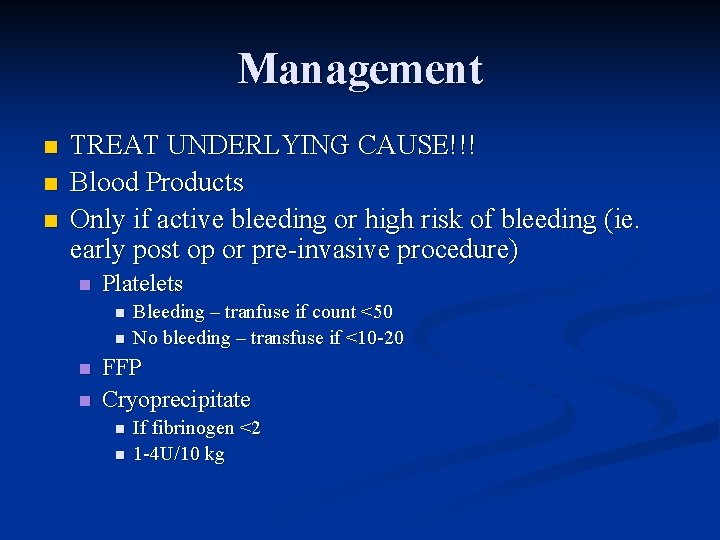
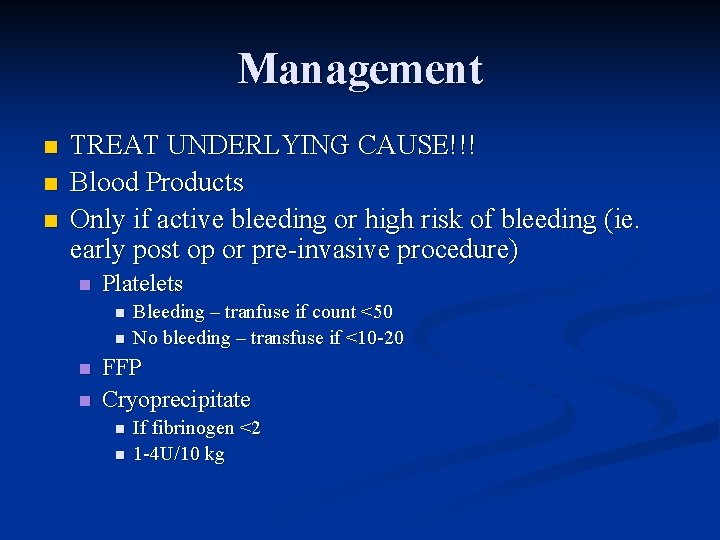
Management n n n TREAT UNDERLYING CAUSE!!! Blood Products Only if active bleeding or high risk of bleeding (ie. early post op or pre-invasive procedure) n Platelets n n Bleeding – tranfuse if count <50 No bleeding – transfuse if <10 -20 FFP Cryoprecipitate n n If fibrinogen <2 1 -4 U/10 kg

Novel treatments APC – up to Phase III trials show benefit in septic DIC n TFPI – promising n ATIII- RCT promising n Heparin n Only case series. Controversial n Therapeutically if overt venous TE or purpura fulminans n
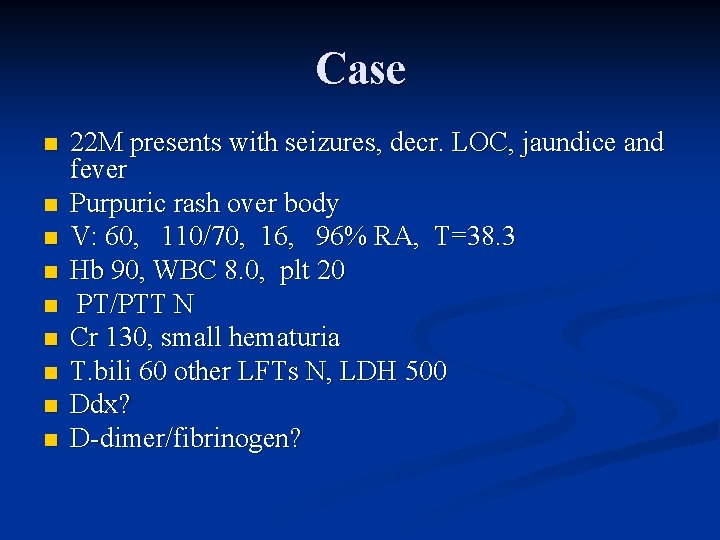
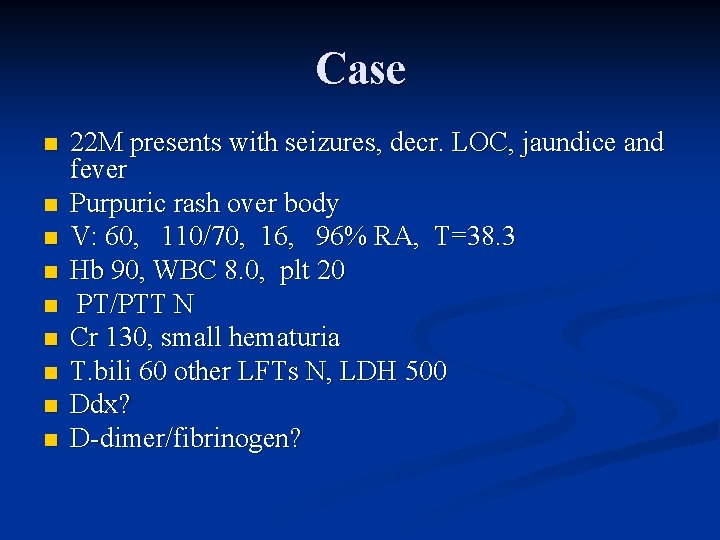
Case n n n n n 22 M presents with seizures, decr. LOC, jaundice and fever Purpuric rash over body V: 60, 110/70, 16, 96% RA, T=38. 3 Hb 90, WBC 8. 0, plt 20 PT/PTT N Cr 130, small hematuria T. bili 60 other LFTs N, LDH 500 Ddx? D-dimer/fibrinogen?
TTP n Main ED mgmt point: n NO platelet transfusion unless life threatening hemorrhage
Liver Disease What mechanisms of coagulopathy? n What blood products to use? n
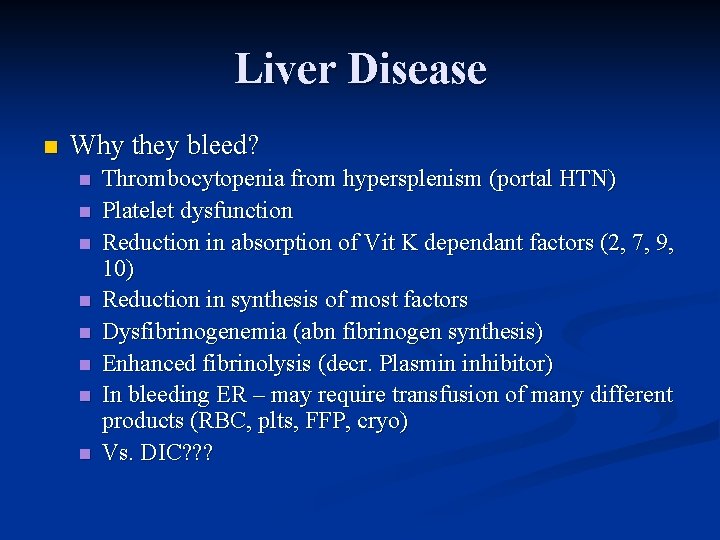
Liver Disease n Why they bleed? n n n n Thrombocytopenia from hypersplenism (portal HTN) Platelet dysfunction Reduction in absorption of Vit K dependant factors (2, 7, 9, 10) Reduction in synthesis of most factors Dysfibrinogenemia (abn fibrinogen synthesis) Enhanced fibrinolysis (decr. Plasmin inhibitor) In bleeding ER – may require transfusion of many different products (RBC, plts, FFP, cryo) Vs. DIC? ? ?
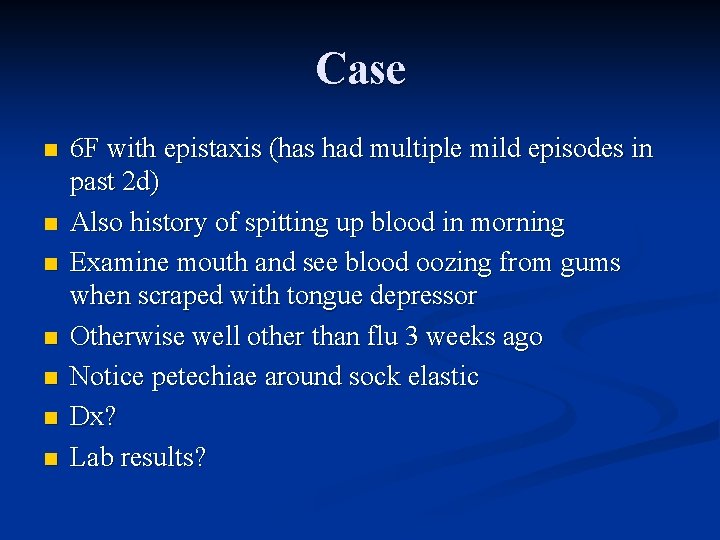
Case n n n n 6 F with epistaxis (has had multiple mild episodes in past 2 d) Also history of spitting up blood in morning Examine mouth and see blood oozing from gums when scraped with tongue depressor Otherwise well other than flu 3 weeks ago Notice petechiae around sock elastic Dx? Lab results?
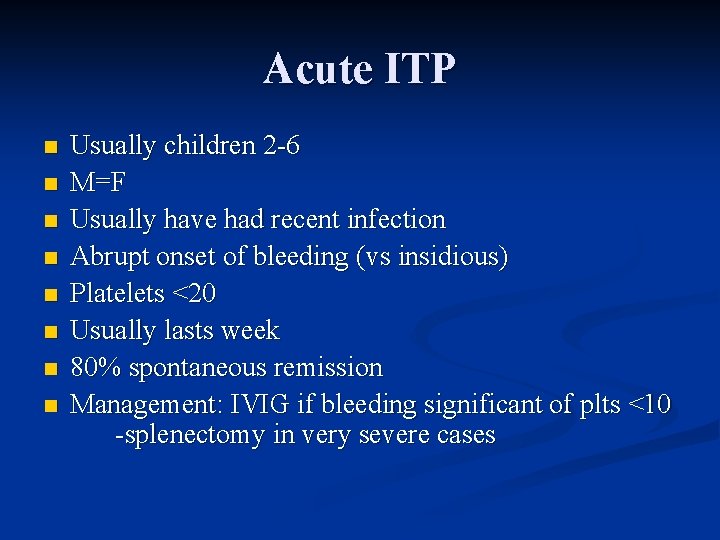
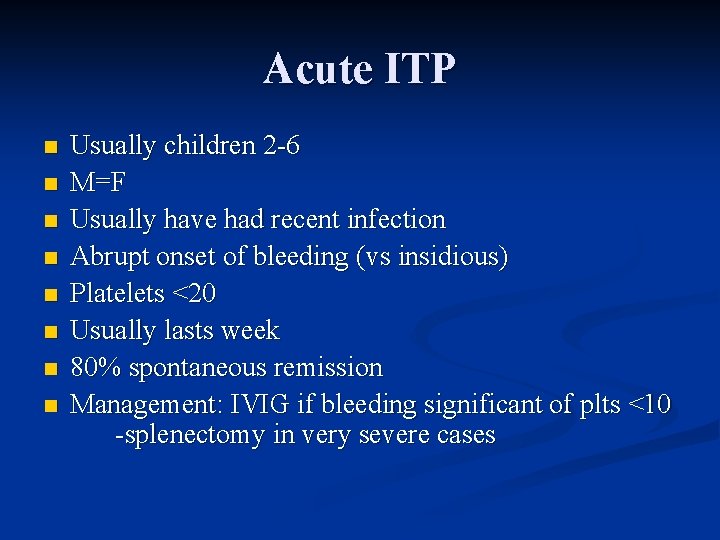
Acute ITP n n n n Usually children 2 -6 M=F Usually have had recent infection Abrupt onset of bleeding (vs insidious) Platelets <20 Usually lasts week 80% spontaneous remission Management: IVIG if bleeding significant of plts <10 -splenectomy in very severe cases
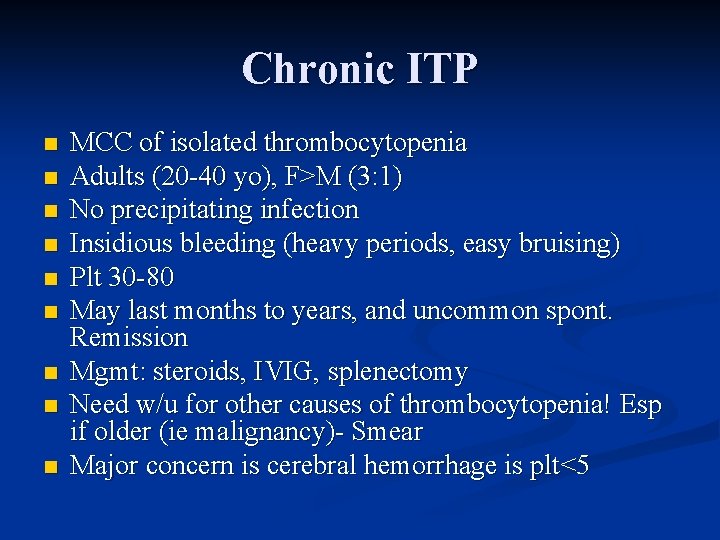
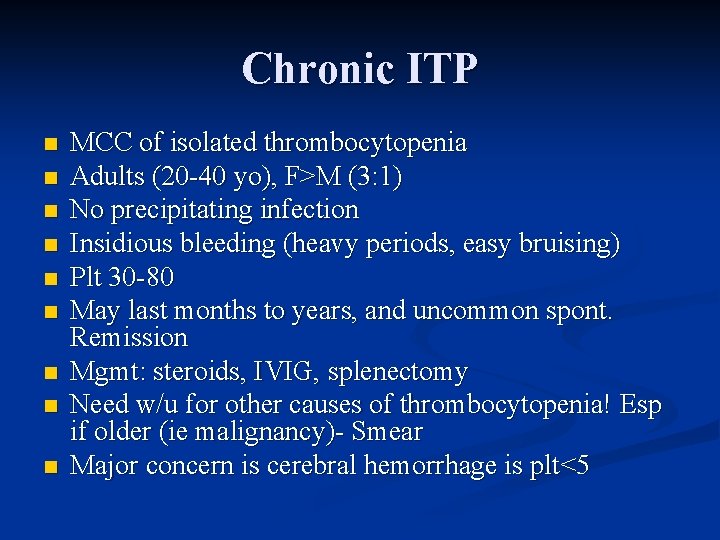
Chronic ITP n n n n n MCC of isolated thrombocytopenia Adults (20 -40 yo), F>M (3: 1) No precipitating infection Insidious bleeding (heavy periods, easy bruising) Plt 30 -80 May last months to years, and uncommon spont. Remission Mgmt: steroids, IVIG, splenectomy Need w/u for other causes of thrombocytopenia! Esp if older (ie malignancy)- Smear Major concern is cerebral hemorrhage is plt<5
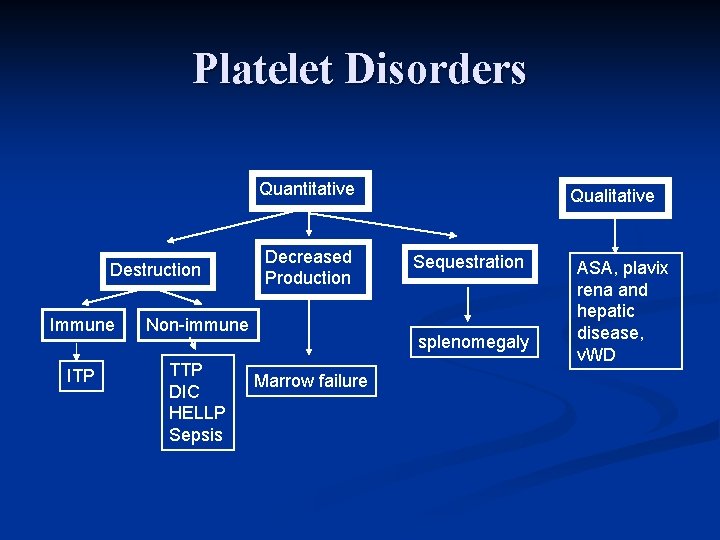
Platelet Disorders Quantitative Destruction Immune Non-immune ITP TTP DIC HELLP Sepsis Decreased Production Qualitative Sequestration splenomegaly Marrow failure ASA, plavix rena and hepatic disease, v. WD

Case 12 F hx of VWD n Presents with heavy menarche (ongoing bleeding for >7 days) n Pale, asymptomatic n Hb = 60 n Mgmt? n
Erik Adolf von Willebrand n n 1870 -1949 Finnish Pediatrician “known for integrity and modesty” Hjordis – 5 yo girl with FHx of bleeding disorders
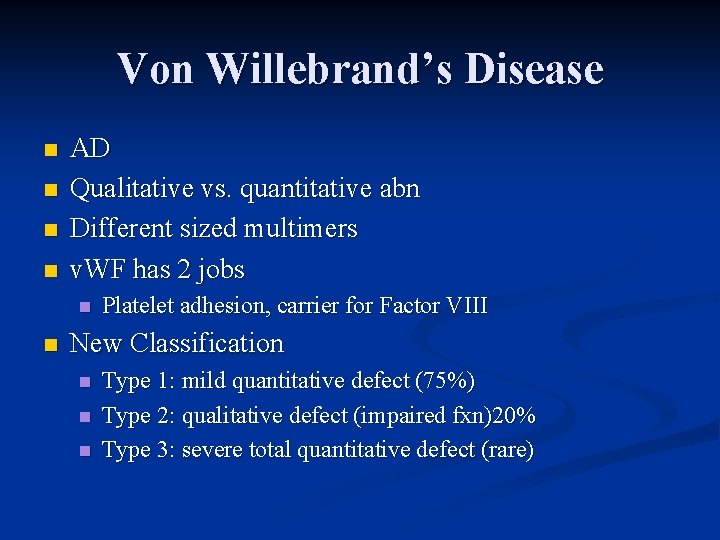
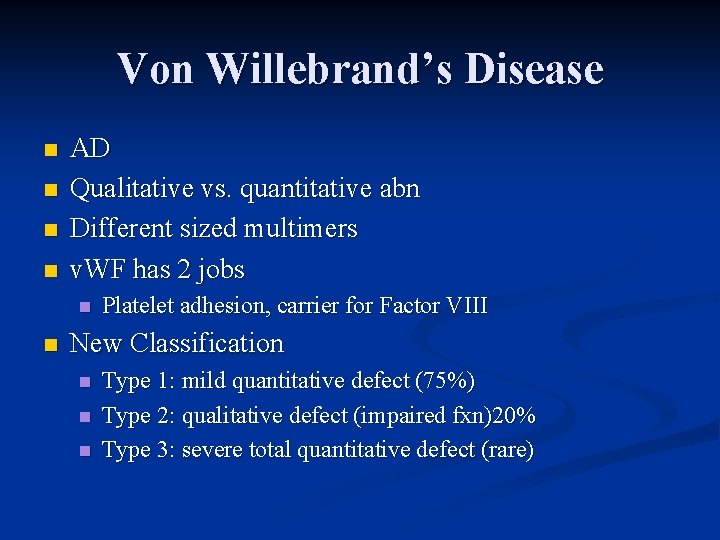
Von Willebrand’s Disease n n AD Qualitative vs. quantitative abn Different sized multimers v. WF has 2 jobs n n Platelet adhesion, carrier for Factor VIII New Classification n Type 1: mild quantitative defect (75%) Type 2: qualitative defect (impaired fxn)20% Type 3: severe total quantitative defect (rare)
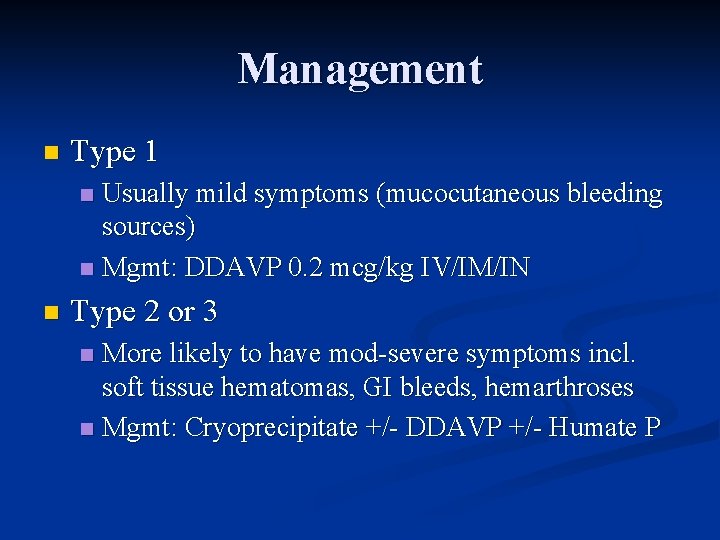
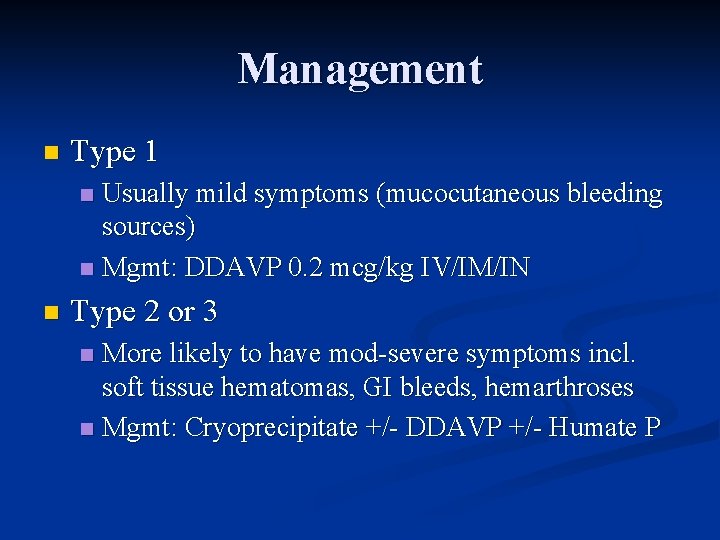
Management n Type 1 Usually mild symptoms (mucocutaneous bleeding sources) n Mgmt: DDAVP 0. 2 mcg/kg IV/IM/IN n n Type 2 or 3 More likely to have mod-severe symptoms incl. soft tissue hematomas, GI bleeds, hemarthroses n Mgmt: Cryoprecipitate +/- DDAVP +/- Humate P n
Case 50 M slipped on ice and twisted R knee n On exam: large hemarthrosis n What is most likely hemostatic disorder? n Management? n

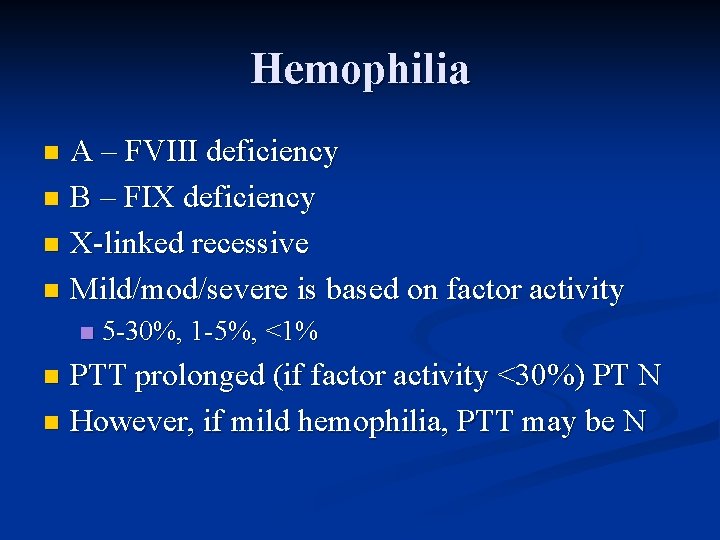
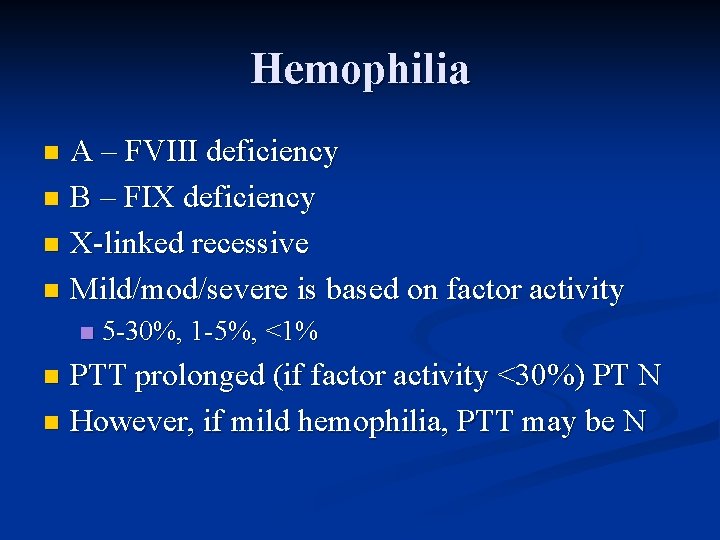
Hemophilia A – FVIII deficiency n B – FIX deficiency n X-linked recessive n Mild/mod/severe is based on factor activity n n 5 -30%, 1 -5%, <1% PTT prolonged (if factor activity <30%) PT N n However, if mild hemophilia, PTT may be N n
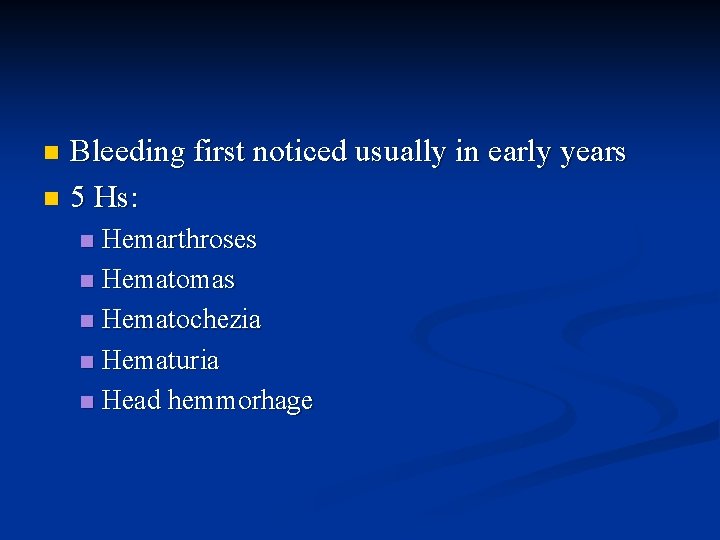
Bleeding first noticed usually in early years n 5 Hs: n Hemarthroses n Hematomas n Hematochezia n Hematuria n Head hemmorhage n
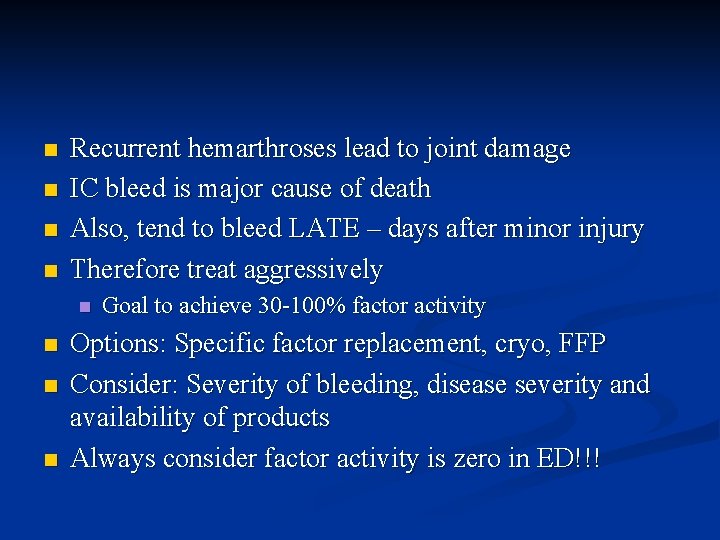
n n Recurrent hemarthroses lead to joint damage IC bleed is major cause of death Also, tend to bleed LATE – days after minor injury Therefore treat aggressively n n Goal to achieve 30 -100% factor activity Options: Specific factor replacement, cryo, FFP Consider: Severity of bleeding, disease severity and availability of products Always consider factor activity is zero in ED!!!

Factor Replacement Is ideal if available in ED, otherwise cryo n 1 U/kg will increase factor by 2% n May develop alloantibodies and need 3 -4 X predicted dose n Goals: n Mild: 5 -10% activity desired -initial dose 12. 5 U/kg n Mod 20 -30% - 25 U/kg n Severe >50% - 50 U/kg n

Cryoprecipitate n Contains 80 - 100 U FVIII (als contains v. WF, fibrinogen, FXIII and fibronectin) Considered a second line agent for Hem A n Dose = 2 bags/10 kg to raise FVIII to hemostatic levels n T ½ = 8 hrs n
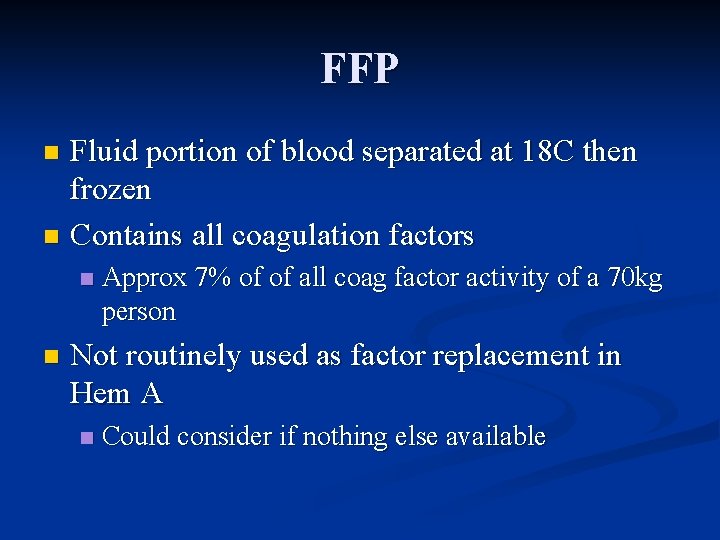
FFP Fluid portion of blood separated at 18 C then frozen n Contains all coagulation factors n n n Approx 7% of of all coag factor activity of a 70 kg person Not routinely used as factor replacement in Hem A n Could consider if nothing else available
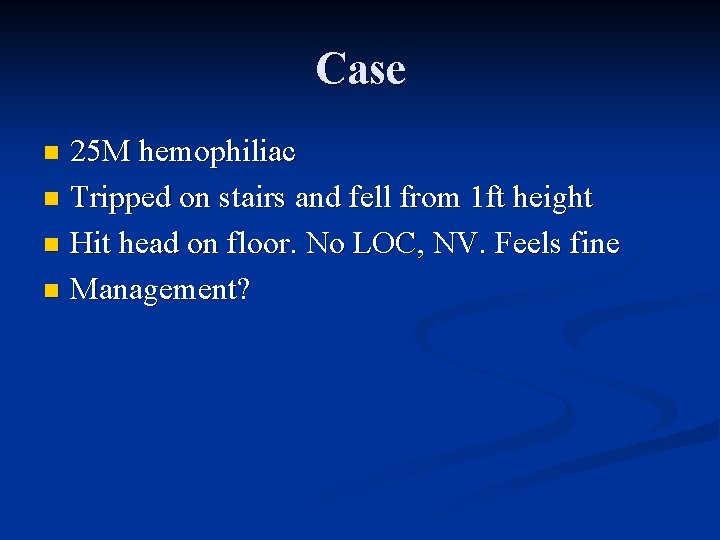
Case 25 M hemophiliac n Tripped on stairs and fell from 1 ft height n Hit head on floor. No LOC, NV. Feels fine n Management? n
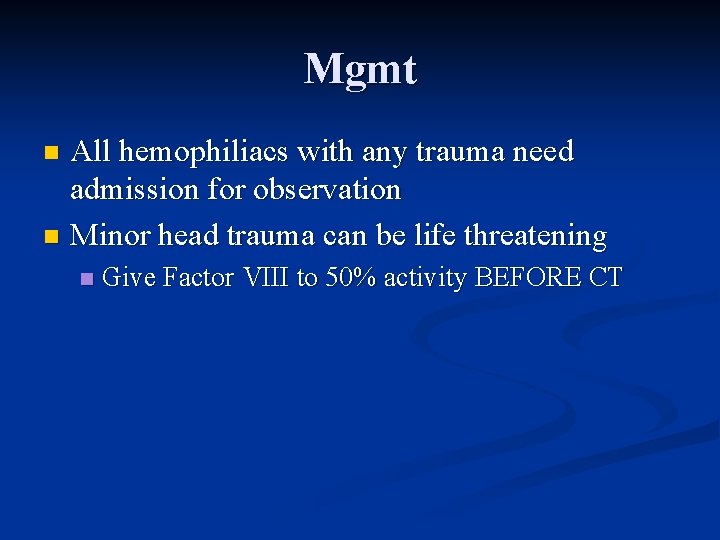
Mgmt All hemophiliacs with any trauma need admission for observation n Minor head trauma can be life threatening n n Give Factor VIII to 50% activity BEFORE CT
Take Home Points n Approach to bleeding disorders n High index of suspicion n Difference in presentation of platelet dysfunction vs. coagulation factor d/o n When to give blood products?

Take Home Points n DIC – treat underlying cause n v. WF – important to know type n Hemophilia – aggressive therapy with factors
Quiz n Which of the following is least likely due to a platelet disorder? A) Epistaxis n B) Retroperitoneal Bleeding n C) Ecchymoses n D) Petechiae n

Quiz n Which is least likely associated with coagulation factor deficiency? A) Intra-articular bleeding n B) Delayed bleeding n C) Retroperitoneal Bleeding n D) Petechiae n
Quiz n Which clinical finding is MOST COMMONLY associated with the onset of ITP? A) Ecchymoses n B) Purpura n C) Petechiae n D) Gingival bleeding n
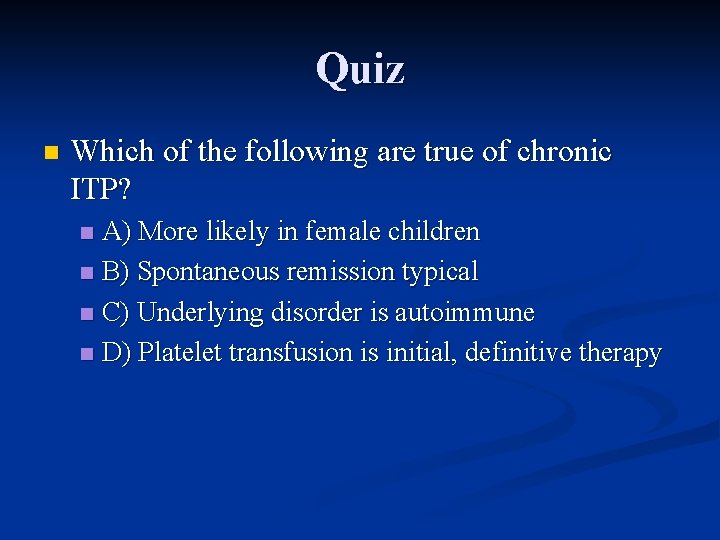
Quiz n Which of the following are true of chronic ITP? A) More likely in female children n B) Spontaneous remission typical n C) Underlying disorder is autoimmune n D) Platelet transfusion is initial, definitive therapy n
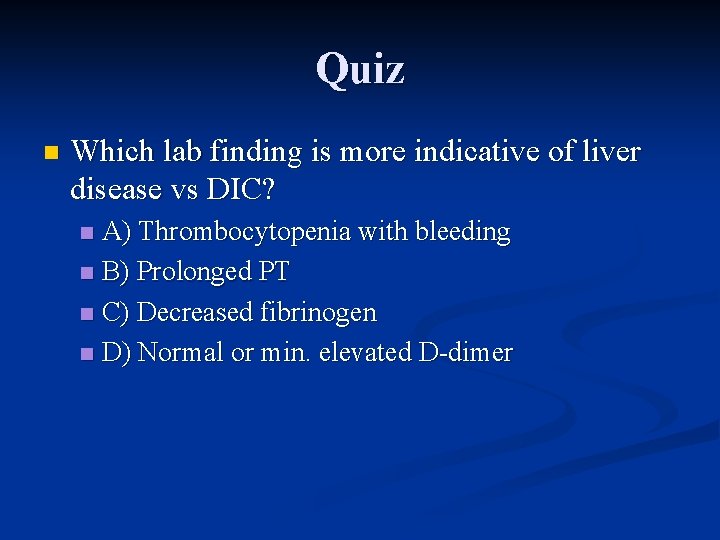
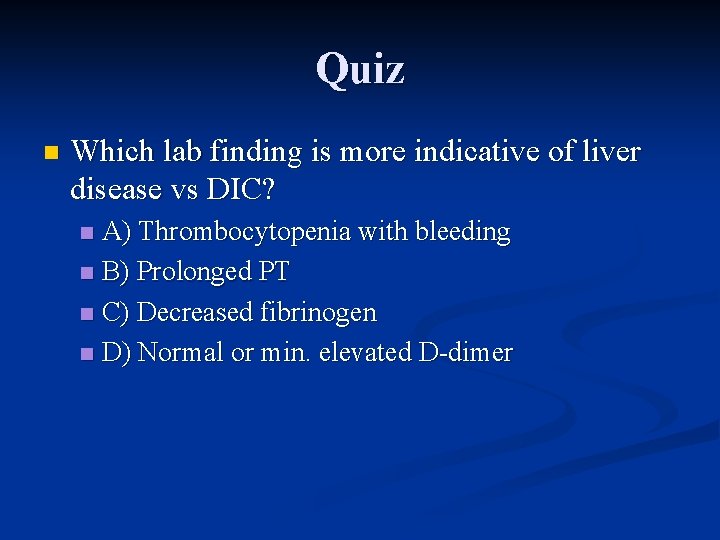
Quiz n Which lab finding is more indicative of liver disease vs DIC? A) Thrombocytopenia with bleeding n B) Prolonged PT n C) Decreased fibrinogen n D) Normal or min. elevated D-dimer n
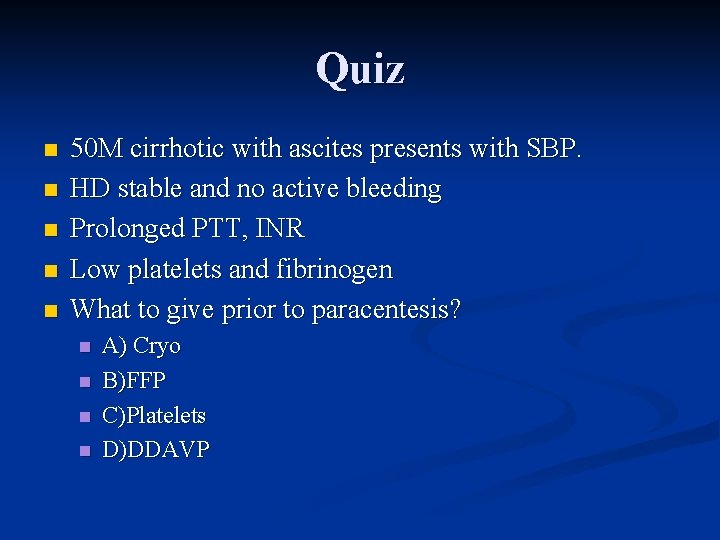
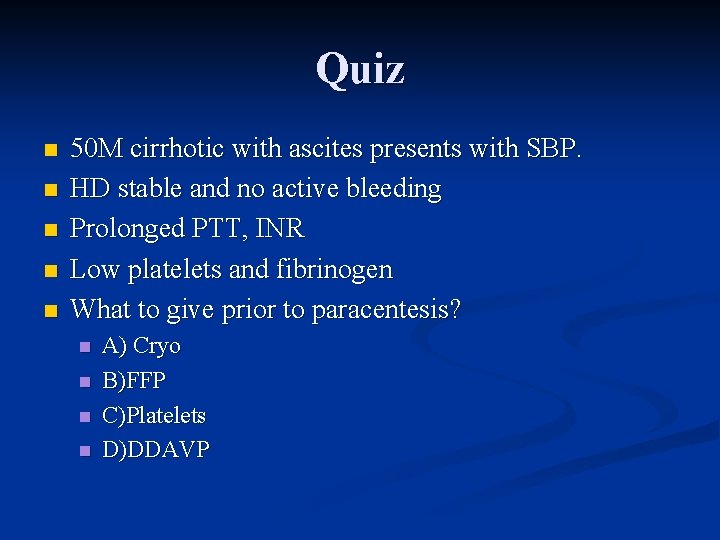
Quiz n n n 50 M cirrhotic with ascites presents with SBP. HD stable and no active bleeding Prolonged PTT, INR Low platelets and fibrinogen What to give prior to paracentesis? n n A) Cryo B)FFP C)Platelets D)DDAVP
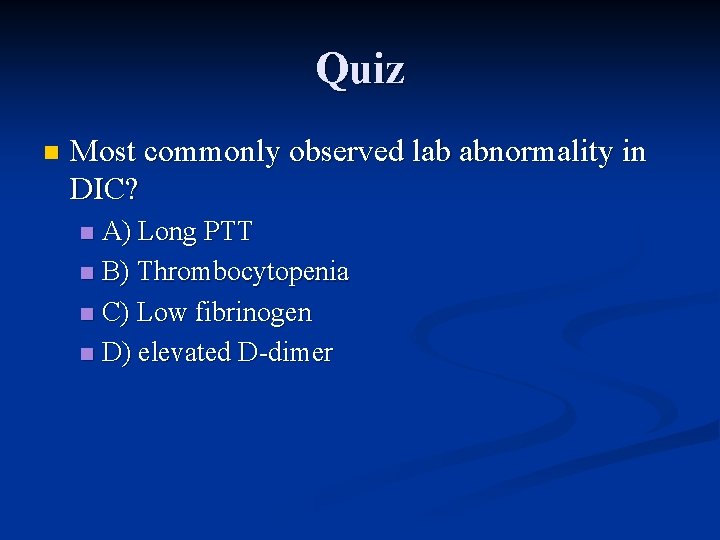
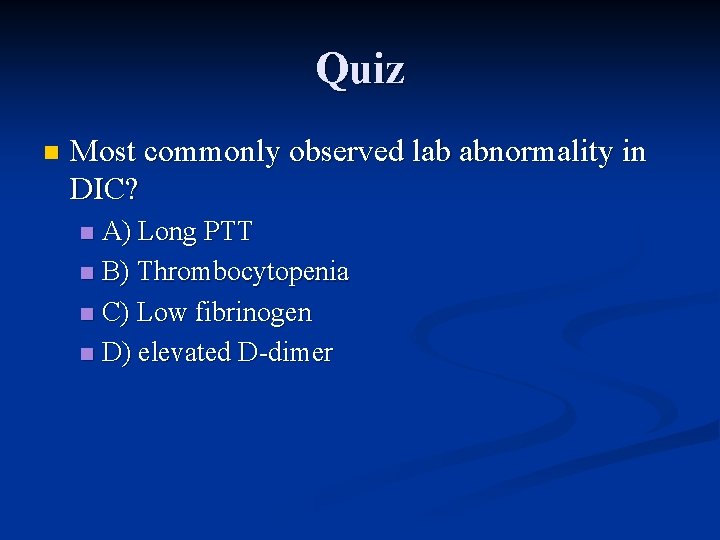
Quiz n Most commonly observed lab abnormality in DIC? A) Long PTT n B) Thrombocytopenia n C) Low fibrinogen n D) elevated D-dimer n
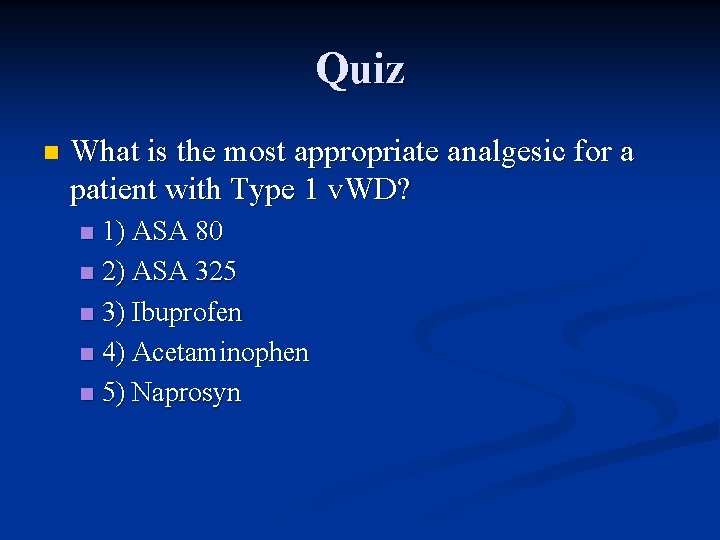
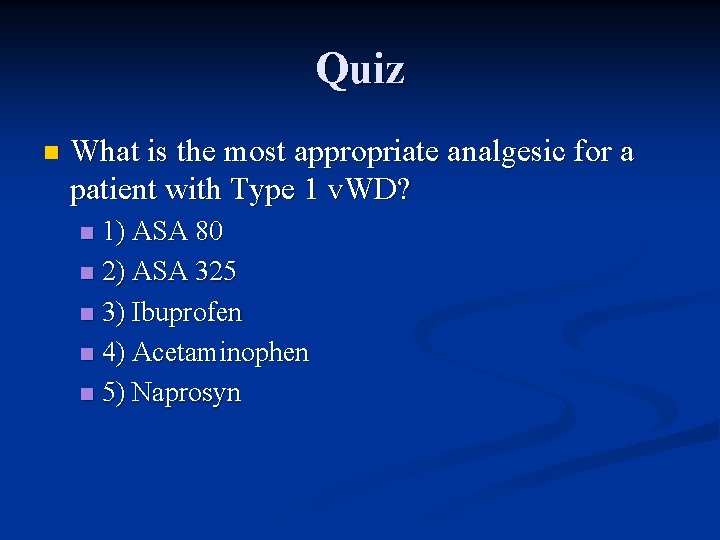
Quiz n What is the most appropriate analgesic for a patient with Type 1 v. WD? 1) ASA 80 n 2) ASA 325 n 3) Ibuprofen n 4) Acetaminophen n 5) Naprosyn n

Quiz 9 M with Type 1 v. WD presents with mild gingival bleeding after flossing. n Stable, however slow bleeding has continued for hours despite local pressure n Most appropriate treatment? n
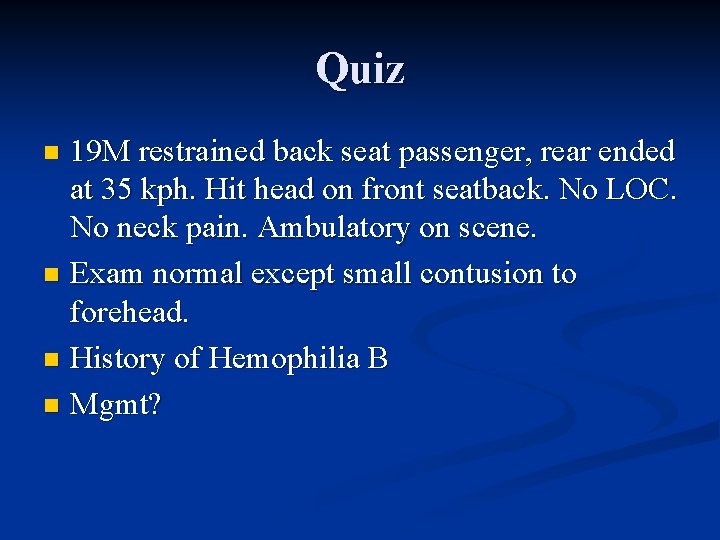
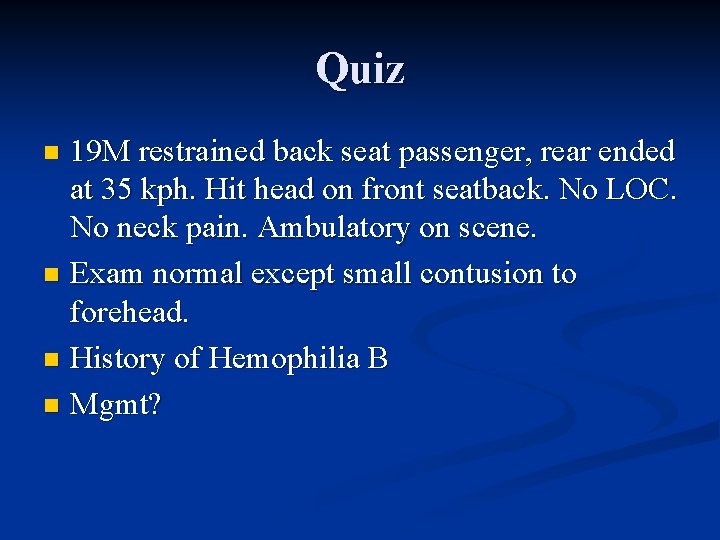
Quiz 19 M restrained back seat passenger, rear ended at 35 kph. Hit head on front seatback. No LOC. No neck pain. Ambulatory on scene. n Exam normal except small contusion to forehead. n History of Hemophilia B n Mgmt? n
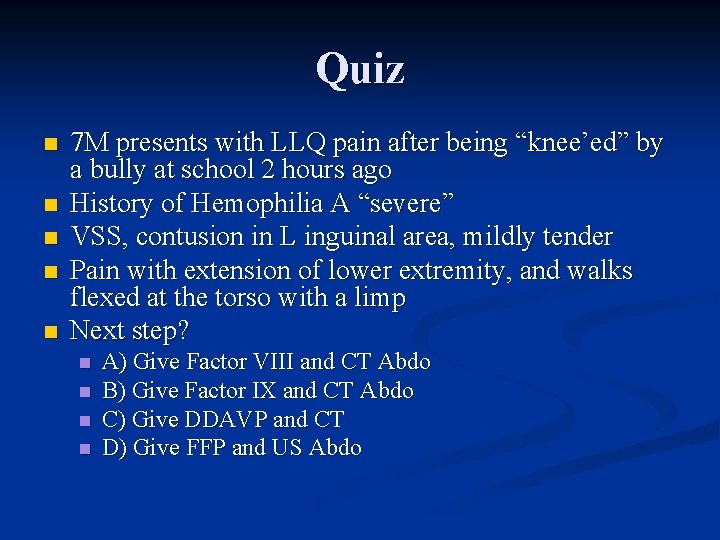
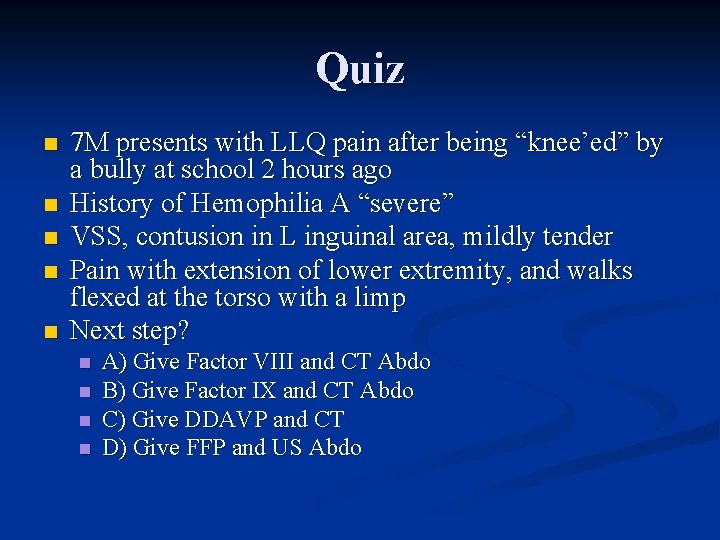
Quiz n n n 7 M presents with LLQ pain after being “knee’ed” by a bully at school 2 hours ago History of Hemophilia A “severe” VSS, contusion in L inguinal area, mildly tender Pain with extension of lower extremity, and walks flexed at the torso with a limp Next step? n n A) Give Factor VIII and CT Abdo B) Give Factor IX and CT Abdo C) Give DDAVP and CT D) Give FFP and US Abdo
 Subendotel
Subendotel Sơ đồ truyền máu
Sơ đồ truyền máu Hemophilia types
Hemophilia types Embolus
Embolus Thrombopoisis
Thrombopoisis 13 blood coagulation factors names
13 blood coagulation factors names Skema hemostasis
Skema hemostasis Alpha granules of platelets
Alpha granules of platelets Hemostasis
Hemostasis Primary hemostasis
Primary hemostasis Ecchumosis
Ecchumosis Surgicutt method
Surgicutt method 1ry hemostasis prescribed by
1ry hemostasis prescribed by Sultana daughter of boota singh
Sultana daughter of boota singh Richard sultana
Richard sultana Ryan sultana
Ryan sultana Dr nuzhat sultana
Dr nuzhat sultana Purpose of food preservation
Purpose of food preservation Balanced diet defination
Balanced diet defination Myapcl
Myapcl Sultana d oman
Sultana d oman Kazi zakia sultana
Kazi zakia sultana Dr riaz qureshi
Dr riaz qureshi Weerstand
Weerstand Moin qureshi gatech
Moin qureshi gatech 10 principles of family medicine
10 principles of family medicine Dr riaz qureshi
Dr riaz qureshi Samina qureshi md
Samina qureshi md Saiqa anne qureshi
Saiqa anne qureshi Red white and blue tortilla chips
Red white and blue tortilla chips Utmb grand rounds
Utmb grand rounds Rounds and fillets are usually dimensioned using
Rounds and fillets are usually dimensioned using Duke family medicine and community health
Duke family medicine and community health Schwartz rounds facilitator training
Schwartz rounds facilitator training Readiness rounds
Readiness rounds Five layers of neurosis
Five layers of neurosis Nursing grand rounds presentation example
Nursing grand rounds presentation example Sam rounds
Sam rounds Round off of 75
Round off of 75 Firing pin marks
Firing pin marks A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Quality teaching rounds coding sheet
Quality teaching rounds coding sheet Christmas table quiz seomra ranga
Christmas table quiz seomra ranga Richard elmore harvard
Richard elmore harvard Maintenance rounds
Maintenance rounds Resident and family engagement
Resident and family engagement Partially resident textures
Partially resident textures Biostats step 3
Biostats step 3 Pab ankle fracture
Pab ankle fracture Resident assessment instrument definition
Resident assessment instrument definition Examples of misappropriation of resident property
Examples of misappropriation of resident property Resident retention
Resident retention Resident and family engagement
Resident and family engagement Acgme resident survey
Acgme resident survey What is conflict resolution in customer service
What is conflict resolution in customer service Resident lifecycle
Resident lifecycle Tarrytown chief resident conference
Tarrytown chief resident conference Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease