Disorder of eccrine sweat glands Present all over



- Slides: 36
Disorder of eccrine sweat glands • Present all over the body especially on the palms, soles and in axillae. • Multiple factors are controlling rate of sweating-temp. , hormones, emotions, gustatory. • Disorders: • Generalized hyperhidrosis • Hypo and anhidrosis • miliaria
Miliaria • Spillage of sweat into dermis due to obstruction and rupture of eccrine sweat ducts. • Occurs – hot humid climate • Variation according to level of rupture: • Miliaria crystallina (rupture below stratum corneum) – Tiny clear noninflammed vesicles. • Miliaria rubra(rupture in epidermis) – Pricking or burning sensation with small erythematous papules surmounted by vesicles. • Miliaria profunda(rupture in dermoepidermal juncn. ) – Larger erythemaouts papules
treatment • • Avoid humid and humid places Avoid synthetic garments Calamine lotion Severe cases: short course of mild topical steroid
Disorder of apocrine gland • Present in axillae, nipples, periumbilical area, perineum and genitalia. • Duct of the gland connects into mid portion of the hair follicle. • Becomes functional just before puberty.
Disorder • Hidradenitis suppurtiva (apocrine acne) • Cause unknown • Microbs like staph. Aureus, anaerobic strpt. And bacteroides are often found in the lesions but their role in the pathogenesis is doubtful • Lesions seen are ndules, pustules, cysts and sinuses with interconnecting bridges. Comedones frequently seen. • Site-axilla, groins and perianal region.
• Treatment: • Severe cases large area of vault of axilla is excised to remove apocrine glands to prevent recurrences. • Medical : – Systemic antibiotics like tetracyclines and erythromycin) – Systemic antiandrogen and retinoids – Isotretinoin – Incision and drainage – Intralesional inj. Of triamcinolone
ABNORMAL VASCULAR RESPONSE • Both exogenous and endogenous stimuli can trigger vascular responses in skin. • At the beginning the epidermis is normal and later it may show changes in the form of necrosis mainly due to vascular compromise. • Different forms: – Vascular dilatation –erythema – Dermal and subcut. Oedema –urticaria and angioedema – Extravasation of blood due to vessel wall inflammation -vasculitis
ERYTHEMA MULTIFORME • As its name implies, this is a reaction pattern of multiform erythematous lesions. • PROVOKING FACTORS IN ERYTHEMA MULTIFORME • Herpes simplex infections • Other infections, e. g. mycoplasma , hepatitis A, histoplasmosis • Bacterial infections • Drugs, especially sulphonamides, penicillins , carbamazepine, phenitoin and barbiturates (most frequent in SJS-TEN COMPLEX) • Internal malignancy or its treatment with radiotherapy • SLE, graft vs host rxn. , lymphoreticular malignancies • Idiopathic (5%)
• The multiform erythematous lesions may be urticaria-like and some have obvious 'bull's-eye' or 'target' lesions. • Blisters may be seen in the centre or around the edges of the lesions • In some cases blisters dominate the picture; the Stevens. Johnson syndrome-toxic epidermal necrolysis comples(SJSTEN complex) is severe bullous erythema multiforme with emphasis on mucosal involvement including the mouth, eyes and genitals, with constitutional disturbance.
• Oral mucosa: hemorrhagic crusting of lips. Bullae which rapidly rupture to form erosions covered with grayish white slough • Eyes: purulent conjunctivitis, corneal erosions • Genital mucosa: erosion s and complicated by urinary retention • Nasal mucosa: erosions • SJS-TEN complex is clinically graded into • SJS- when the body surface area involves<10% • SJS-TEN- when BSA 10 -30% • TEN- >30%
• Management • Usually no treatment is required although symptomatic relief can be obtained with simple dressings. • Stevens-Johnson syndrome can be treated with a short course of intravenous immunoglobulin. Corticosteroids are best avoided.
ERYTHEMA NODOSUM • This characteristic reaction pattern is due to a vasculitis in the deep dermis and subcutaneous fat. • Clinical features • Painful, palpable, dusky blue-red nodules • most commonly seen on the lower legs. • Malaise, fever and joint pains are common. • The lesions resolve slowly over a month, leaving bruise-like marks.
• PROVOKING FACTORS IN ERYTHEMA NODOSUM • Infections • Bacteria (streptococci, tuberculosis, brucellosis and leprosy), viruses, mycoplasma, rickettsia, chlamydia and fungi • Drugs • e. g. Sulphonamides and oral contraceptives • Systemic disease • e. g. Sarcoidosis, ulcerative colitis and Crohn's disease • Management • The underlying cause should be determined and treated. Bed rest and oral NSAIDs may hasten resolution. Tapering systemic corticosteroid courses may be required in stubborn cases.

urticaria
• Also known as hives. • Eruption characterized by transient usually pruritic wheals due to acute dermal oedema from the extravascular leakage of plasma. • Angioedema signifies larger areas of oedema involving the dermis and subcutis.
Aetiopathogenesis • Immune • Non immune
• Lesion occurs due to release of biologically active substances from mast cells particularly histamine. • Histamine causes vasodilatation and increased vascular permeability.
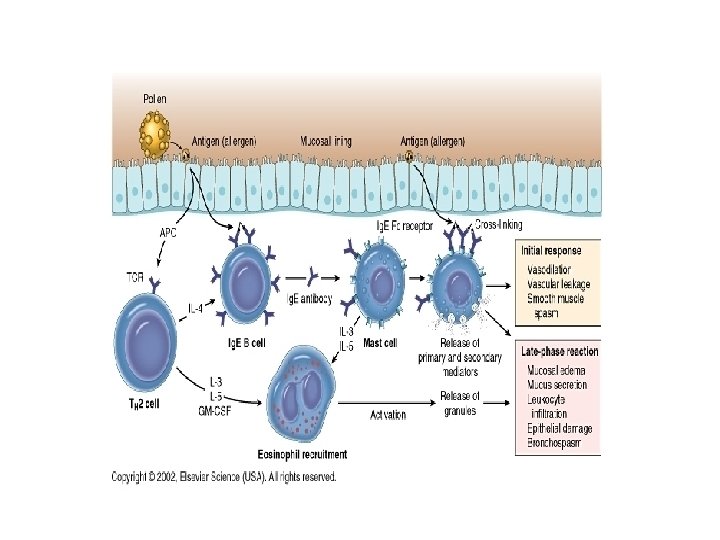
Different pathways involved • Antigen induced , Ig. E mediate histamine release from tissue mast cells causing immediate hypersensitivity. • Mast cell degranulation through the classical complement pathways. • Direct mast cell degranulation by certain drugs and chemicals
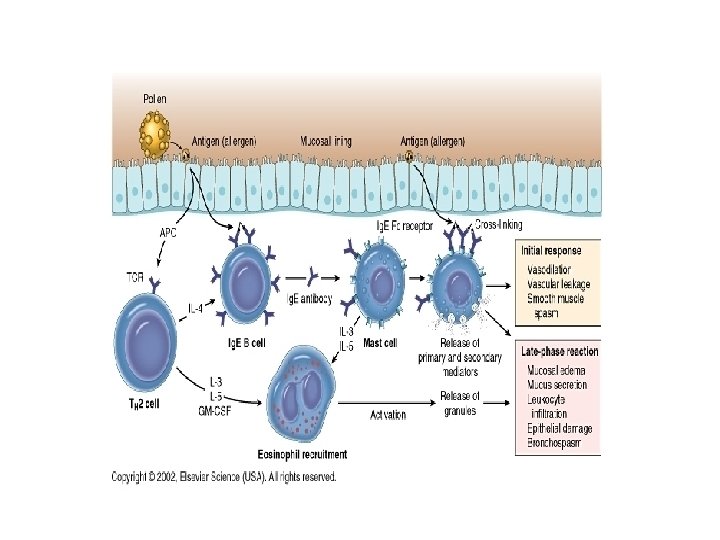
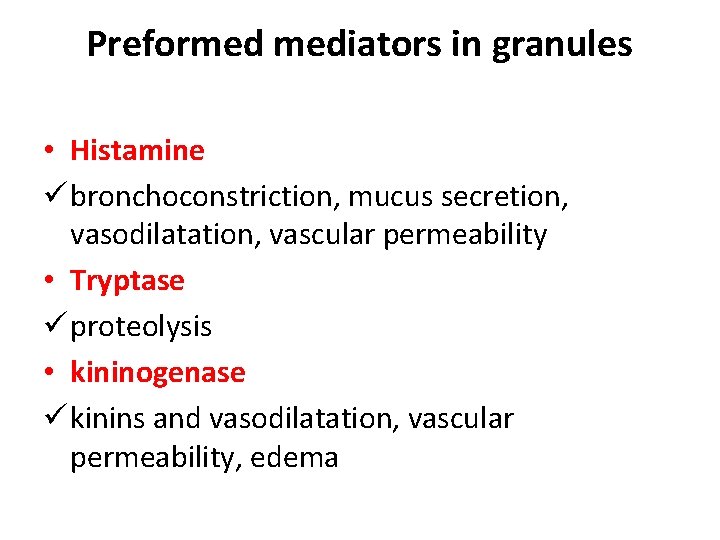
Preformed mediators in granules • Histamine ü bronchoconstriction, mucus secretion, vasodilatation, vascular permeability • Tryptase ü proteolysis • kininogenase ü kinins and vasodilatation, vascular permeability, edema
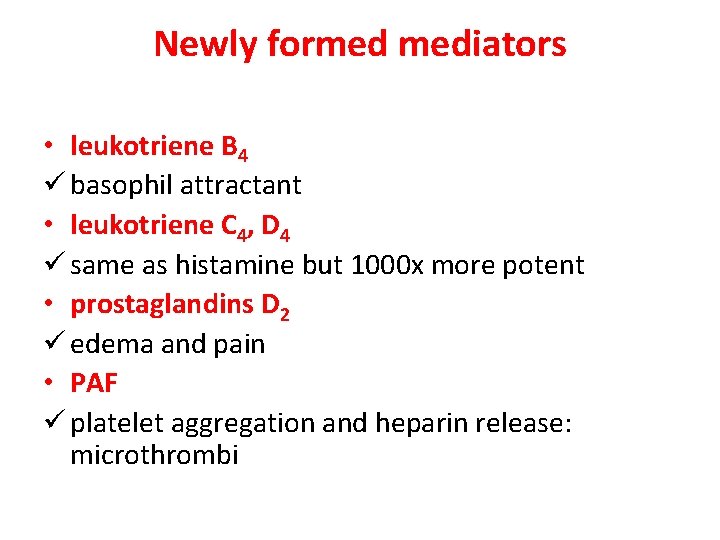
Newly formed mediators • leukotriene B 4 ü basophil attractant • leukotriene C 4, D 4 ü same as histamine but 1000 x more potent • prostaglandins D 2 ü edema and pain • PAF ü platelet aggregation and heparin release: microthrombi
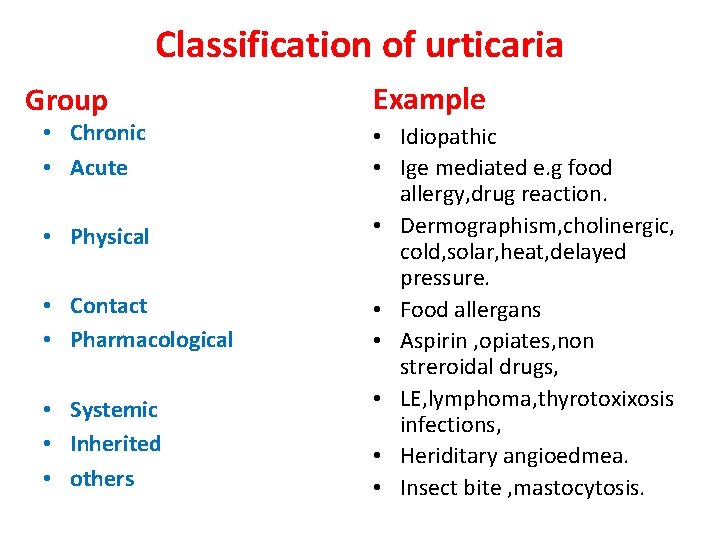
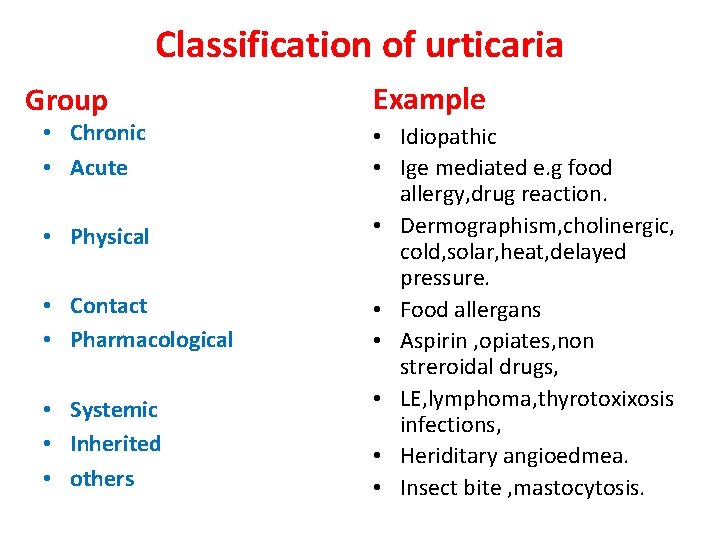
Classification of urticaria Group • Chronic • Acute • Physical • Contact • Pharmacological • Systemic • Inherited • others Example • Idiopathic • Ige mediated e. g food allergy, drug reaction. • Dermographism, cholinergic, cold, solar, heat, delayed pressure. • Food allergans • Aspirin , opiates, non streroidal drugs, • LE, lymphoma, thyrotoxixosis infections, • Heriditary angioedmea. • Insect bite , mastocytosis.
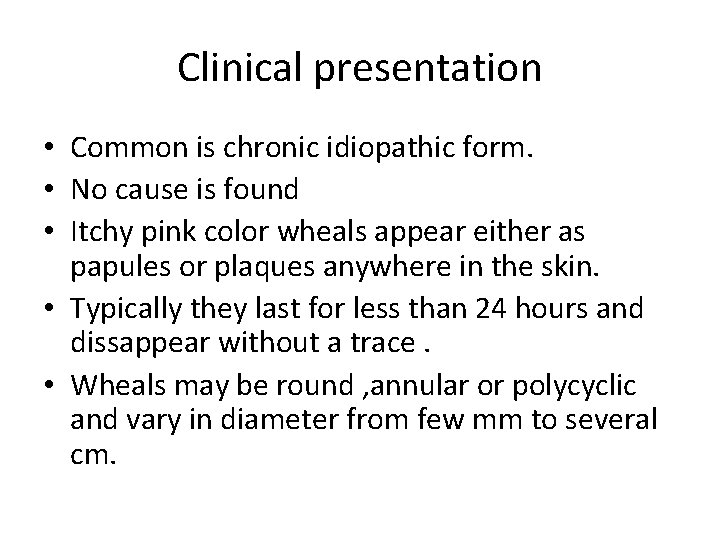
Clinical presentation • Common is chronic idiopathic form. • No cause is found • Itchy pink color wheals appear either as papules or plaques anywhere in the skin. • Typically they last for less than 24 hours and dissappear without a trace. • Wheals may be round , annular or polycyclic and vary in diameter from few mm to several cm.
• Their number can vary from few to many. • Angioedema usually with oedema of the tongue and lips may occur. • Resolves spontaneously within few months.
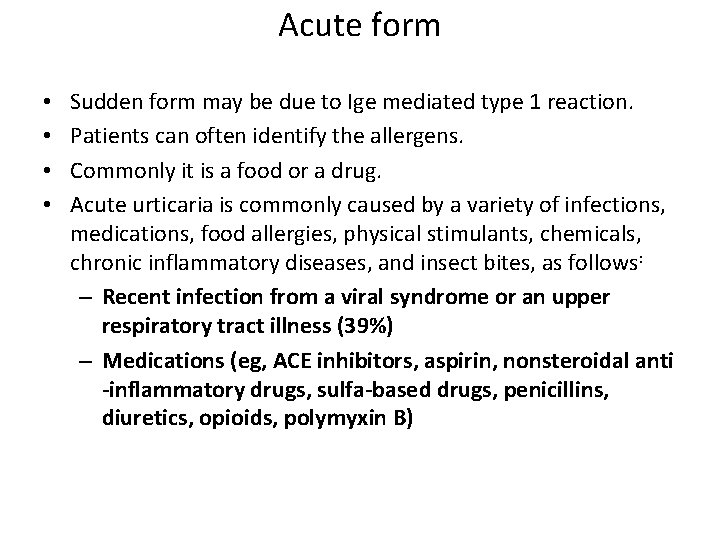
Acute form • • Sudden form may be due to Ige mediated type 1 reaction. Patients can often identify the allergens. Commonly it is a food or a drug. Acute urticaria is commonly caused by a variety of infections, medications, food allergies, physical stimulants, chemicals, chronic inflammatory diseases, and insect bites, as follows: – Recent infection from a viral syndrome or an upper respiratory tract illness (39%) – Medications (eg, ACE inhibitors, aspirin, nonsteroidal anti -inflammatory drugs, sulfa-based drugs, penicillins, diuretics, opioids, polymyxin B)
– Food and food additives (eg, nuts, fish, shellfish, eggs, chocolate, strawberries, salicylate, benzoates) – Parasitic infections (eg, Ascaris, Ancylostoma, Strongyloides, Echinococcus, Trichinella, Filaria) – Physical stimulants (eg, cold, pressure, aquagenic) – Chemicals (eg, latex, ammonium persulfate in hair chemicals) – Intravenous radiocontrast media – Arthropod bites

wheal
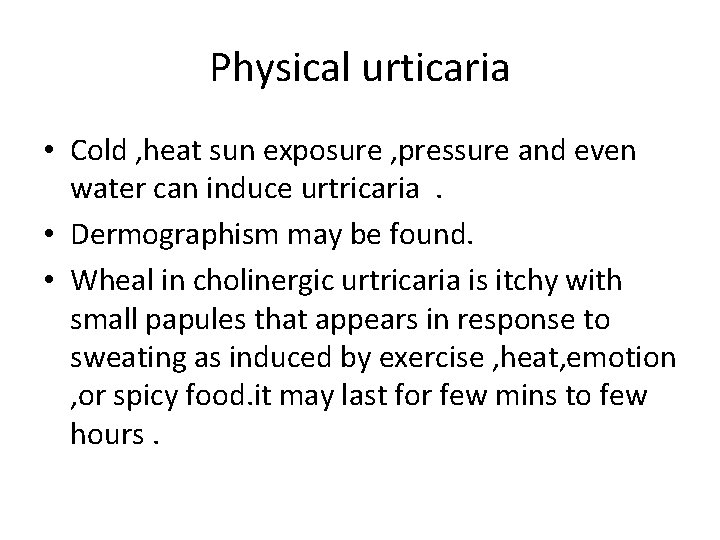
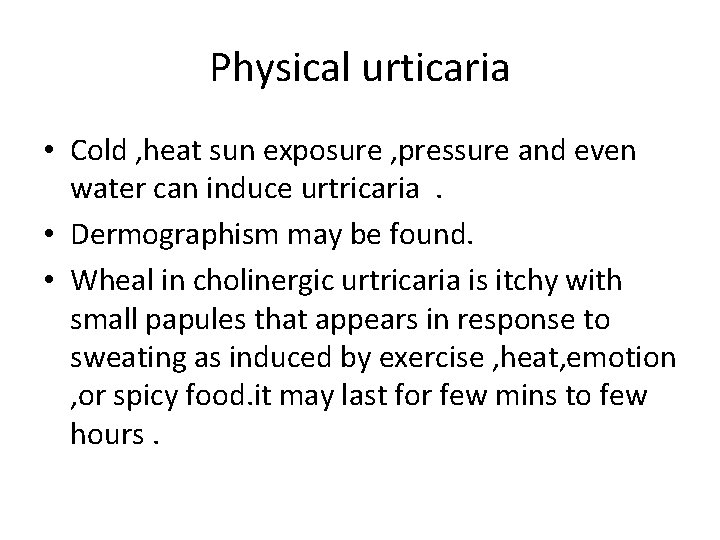
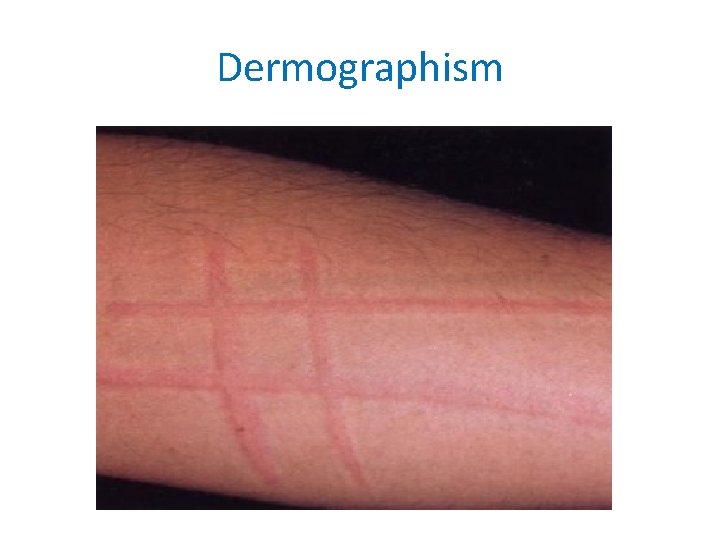
Physical urticaria • Cold , heat sun exposure , pressure and even water can induce urtricaria. • Dermographism may be found. • Wheal in cholinergic urtricaria is itchy with small papules that appears in response to sweating as induced by exercise , heat, emotion , or spicy food. it may last for few mins to few hours.
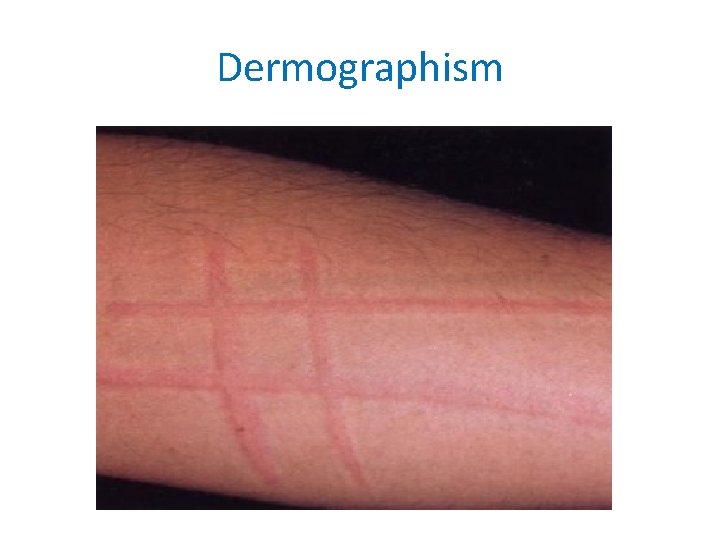
Dermographism
Hereditary angioedema • Autosomal dominant. • Usually fatal • Episode of angioedema involving larynx and gi tract. • Due to defficiency of c 1 esterase inhibitor that causes the activation of complement pathway and accumulation of vasoactive mediators. • In acute condition fresh frozen plasma are given. • In long term danazol is given.
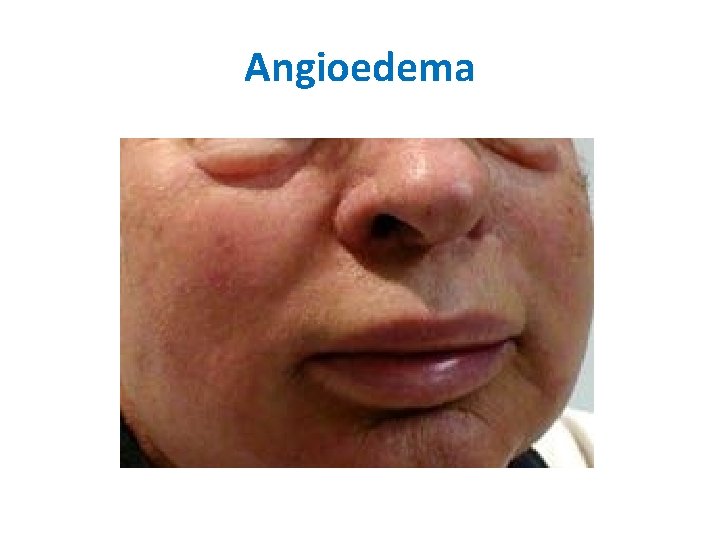
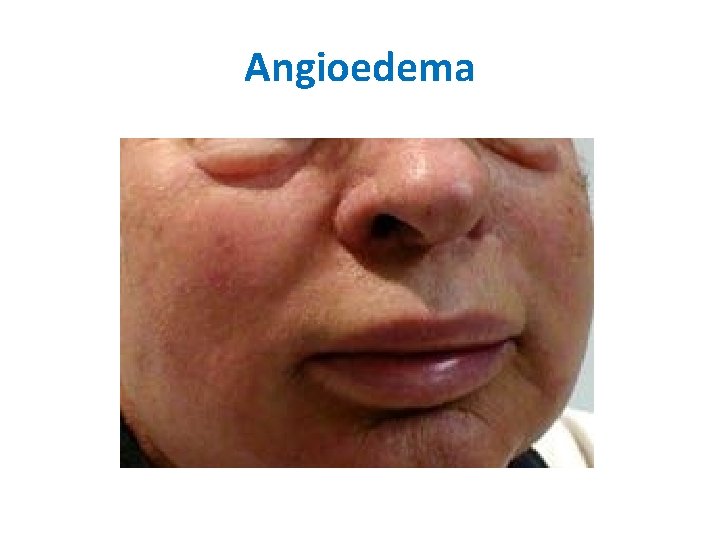
Angioedema
Management • Underlying cause should be eliminated. • Desensitization • Main stay of treatment is with antihistaminics.

• Cetirizine (Zyrtec) • Second-generation antihistamine with markedly reduced sedative effects and reduced anticholinergic effects. Forms complex with histamine for H 1 receptor sites in blood vessels, GI tract, and respiratory tract. • Adult • 5 -10 mg PO • Fexofenadine (Allegra) • Competes with histamine for H 1 receptors on GI tract, blood vessels, and respiratory tract, reducing hypersensitivity reactions. Does not sedate. • SR: 180 mg PO
Histamine H 2 antagonists • Cimetidine (Tagamet) • H 2 antagonist that when combined with an H 1 antagonist may be useful in treating itching and flushing in urticaria and contact dermatitis that do not respond to H 1 antagonists alone. Use in addition to H 1 antihistamines. • 300 mg PO qid
• Corticosteroid: used occassionaly in severe cases and in angioedema and urticarial vasculitis. Prednisone • Immunosuppressant for treatment of autoimmune disorders; may decrease inflammation by reversing increased capillary permeability. Stabilizes lysosomal membranes and suppresses lymphocytes and antibody production. • 0. 5 -2 mg/kg/d PO; taper as condition improves; single morning dose is safer for long-term use, but divided doses have more anti-inflammatory effect
Adrenaline • Acute airway obstruction or anaphylactic shock • Adrenaline together with an antihistaminics chlorpheniramine should be given i. v slowly. • Adrenaline dose 0. 5 -1 mg 0. 5 -1 ml of 1/1000.