DISORDER OF ADRENAL GLAND Lecture for 5 vintage




























- Slides: 109
DISORDER OF ADRENAL GLAND Lecture for 5. vintage 2. LF UK Prague

Adrenal Gland • • Cortex Medulla

Adrenal gland • Geminate organ - 10 - 15 g in adulthood • Influence over metabolism saccharides, oils, albumins, ions and water • Adaptation gadgetry
Adrenal cortex • Zona glomerulosa - small influence ACTH, secretion aldosterone • Zona fasciculata - cholesterol, below stimulation ACTH, cortisol • Zona reticularis - poor on lipids, secretion adrenal androgens, oestrogens, lower intensity production and readiness issue glucocorticoids and C 19 steroids
Development cortices • Zona juvenilis (DHEA) • Maturing fruit
Secretion of corticoids • ACTH • Changes in ionic economy (on K) • High flow neck

Products of cortices • Glukocorticoids • Mineralocorticoids • Adrenal gonadal hormones androgens and estrogens
Biosynthesis of steroids • Acetylcoenzym A • Esters cholesterol • Cholesterol
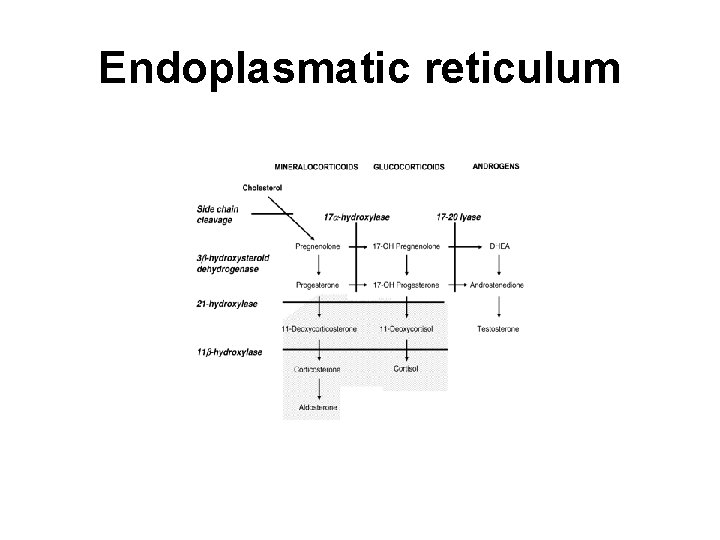
Cellulate biosynthesis • Mitochondrie cholesterol pregnenolon • Endoplasmatic reticulum
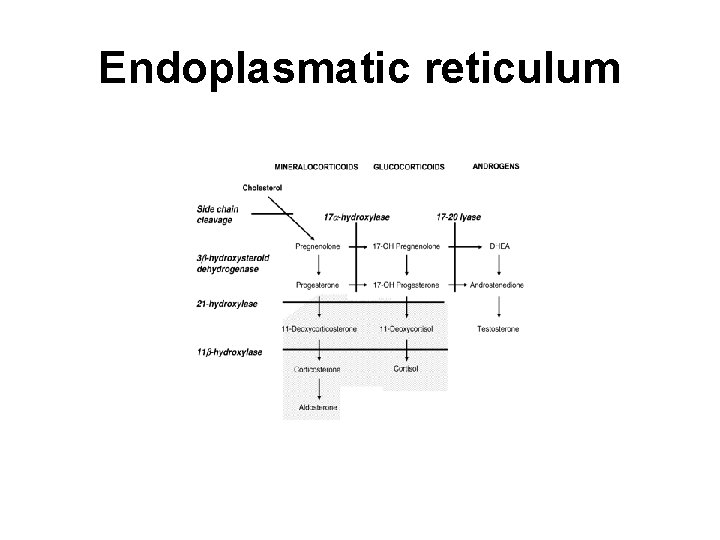
Endoplasmatic reticulum
Chief products • Glucocorticoid cortisol (10 - 30 mg/day) • DHEA ( 10 - 40 mg/day) • Mineralocorticoid aldosterone ( 0, 05 - 0, 25 mg/day)
Cortisol metabolism • Secretion in diurnal rhythm, maximum morning o'clock • Structure on CBG ( cortisol binding glob. ) ) (oestrogen. and tyroid. ) • alpha 1 fibralbumin- transcortin - 90 - 95 % cortisol • Biologist. half - time - 80 - 150 mine.

Cortisol metabolism II • Cortisol cortisone (11 beta dehyrogenasis) • Mineralocorticoid receptors
Drive secretion • Hypotalamus CRH • Hypophysis - ACTH • Adrenal gland - cortisol • Cortisol - CRH
Drive secretion II • Closed circuit backward structure • Variable setting • Daily rhythm • Stress • Displacement - supresion
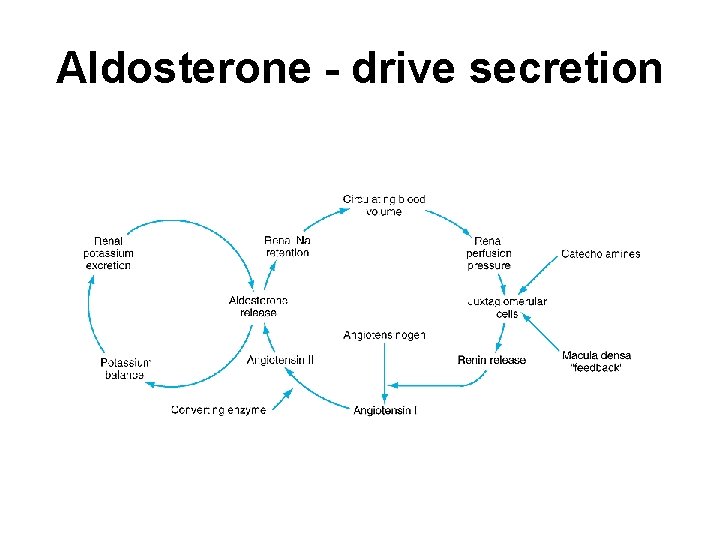
Aldosterone • Renin angiotenzin system • On and pressure in afferent arteriols • Rentention Na and vazocontriction rise blood pressure
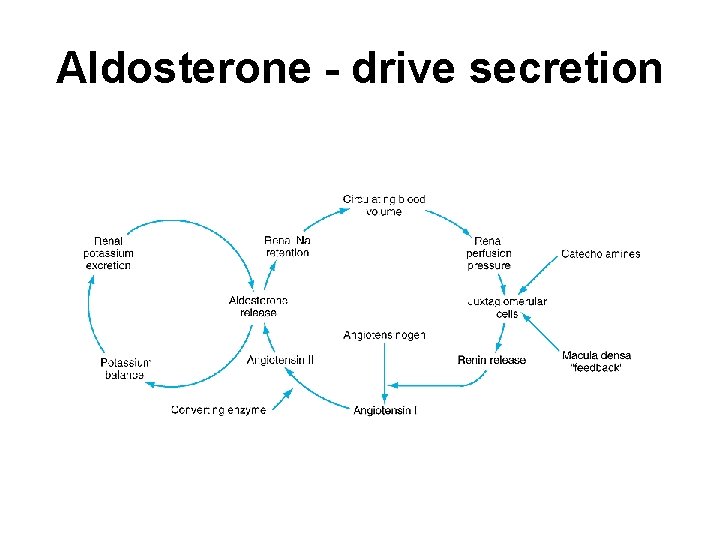
Aldosterone - drive secretion
Aldosterone • Primary hyperaldosteronism - low renin • Secondary hyperaldosteronism - high renin • ACTH - works less than cortisol
Effects of glucocorticoids • • • Influence over intermediary metabolism Stimulation of glukoneogenesis Increased saving glycogen in liver Decrease utilization glucose on the fringe Increased mobilization lipide
Effects of glukocorticoids II • • • Lowered extrahepatal proteosynthesis Increased evolution amino - acids Increased hepatic proteosynthesis Anti - inflammatory effect Immunosuppressive therapy effect Resorbence waters
Effects of mineralocorticoids • • Retention soda lye ions Excretion potassium ions Retention waters Regulation volume extracellular ( largely intravascular) liquid • Increasing extracellular space
Effects of androgens testosterone • • • Anabolic effect Muscle, vocal cords, bone External genital Growth, hematopoesis, spermatogenesis Sexual behaviour Back regulation
Effects of androgens DHT • • • Facial and bodily feathering Acne Sebum Prostate Back regulation
Hypocortisolism Addison dissease • 1. Primary - increased secretion ACTH acute chronic • 2. Secondary - lowered secretion ACTH

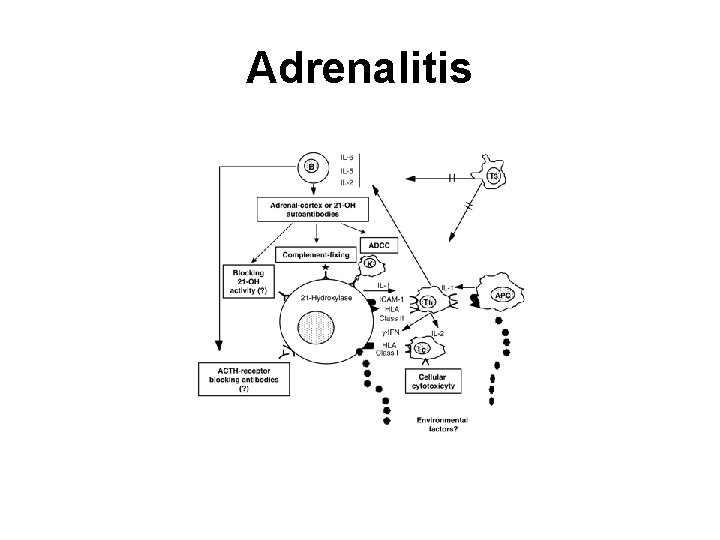
Chronic generalize • Prime atrophy adrenal- illnes of immunity adrenalitis • TBC of adrenal gland • Mycoses and histoplasma, syphilis • Inborn hypoplasis or aplaus od adrenal gland • State after adrenalectomy
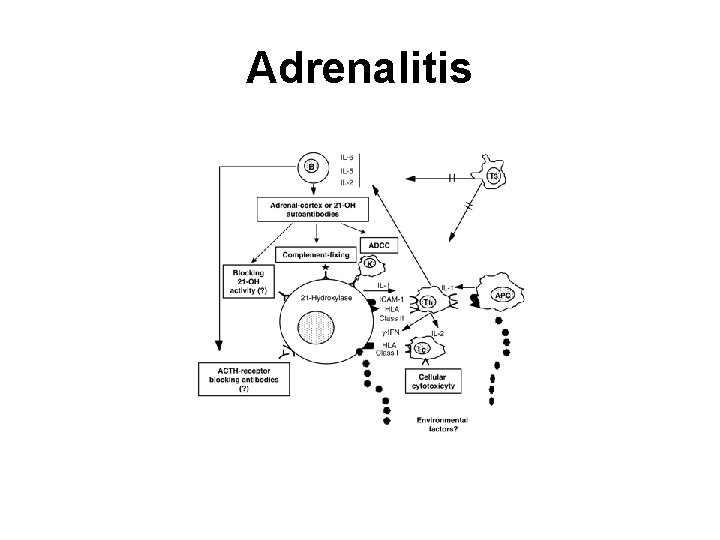
Adrenalitis
Chronic generalize II • Recessive hereditary falling - short with cerebral disorder (blocked on X chromosomal) • Destruction tissues - polypuses, base, oil, amyloid • Hemochormatosis

Chronic dissociation function • Block some from enzymes steroidogenesis with hyperplasia of adrenal gland • Wherewith height is block (more closely to cholesterol), by is major
Secondary hypocorticolism • Starvation wages ACTH • Hypotalamo -hypofysis : lesion of hypotalamus or hypophysis • State after therapy with corticoids inhibition of secretion
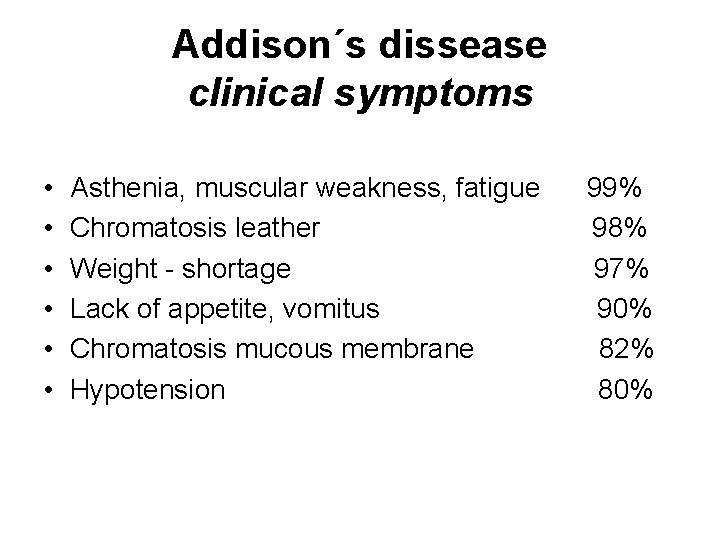
Addison´s dissease clinical symptoms • • • Asthenia, muscular weakness, fatigue Chromatosis leather Weight - shortage Lack of appetite, vomitus Chromatosis mucous membrane Hypotension 99% 98% 97% 90% 82% 80%
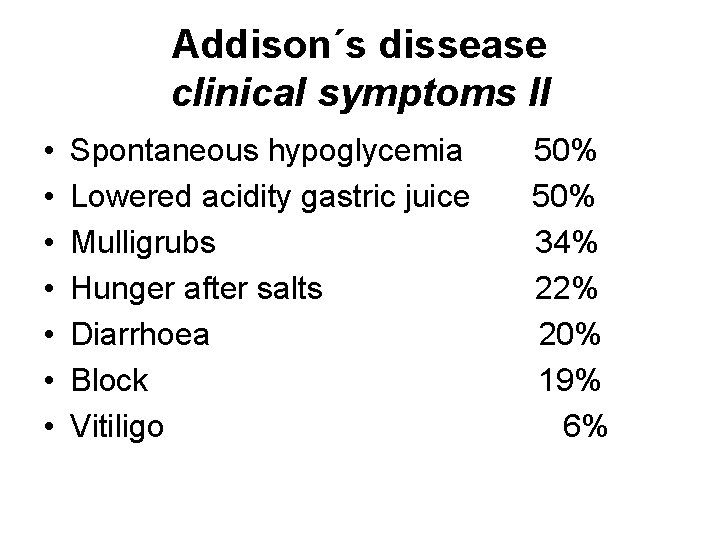
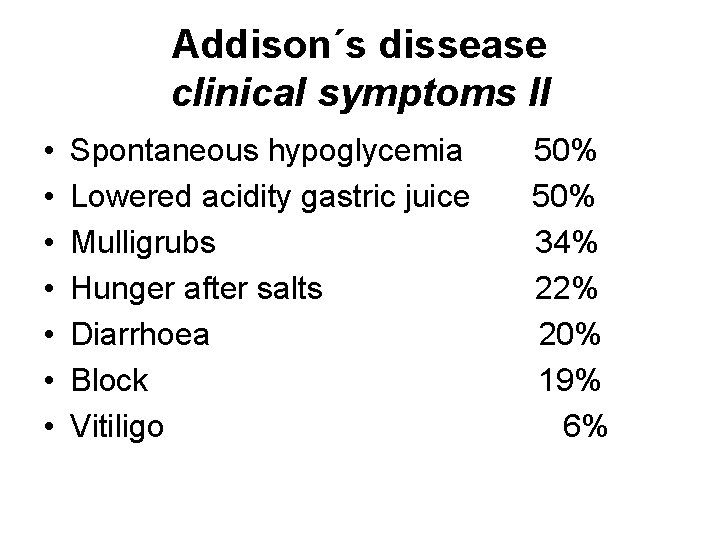
Addison´s dissease clinical symptoms II • • Spontaneous hypoglycemia Lowered acidity gastric juice Mulligrubs Hunger after salts Diarrhoea Block Vitiligo 50% 34% 22% 20% 19% 6%

Clinical symptoms Patofysiology of glucocorticoids • Sugars hypoglycemia, hunger, cereberal disfunction, changes EEG, nausea, sweat • Proteins and oils weight - shortage, astenia, hypochlesterolemia, keto - acidosis • Haemopoiesis normocyt. pancytopenia, hypoleucocytosis • CNS endocrinous psycho - complex • Increased issue MSH (ACTH) - chromatosis
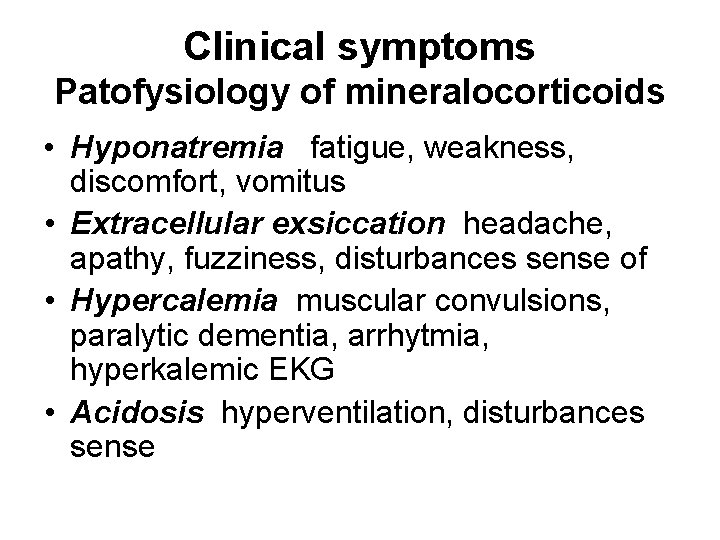
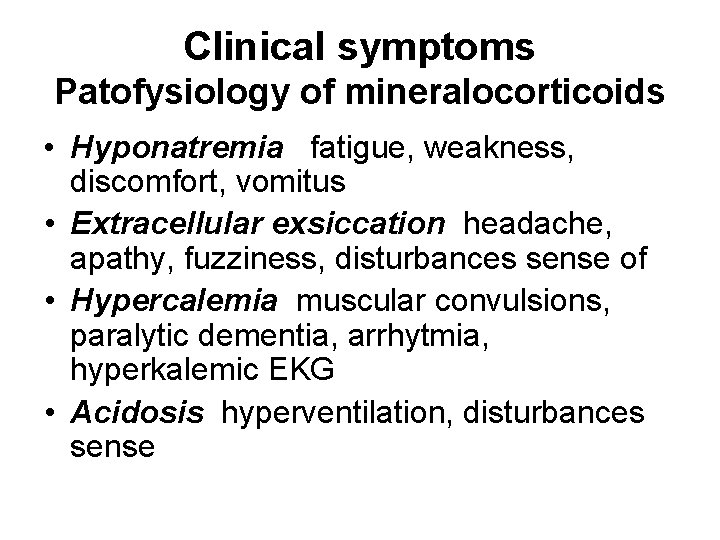
Clinical symptoms Patofysiology of mineralocorticoids • Hyponatremia fatigue, weakness, discomfort, vomitus • Extracellular exsiccation headache, apathy, fuzziness, disturbances sense of • Hypercalemia muscular convulsions, paralytic dementia, arrhytmia, hyperkalemic EKG • Acidosis hyperventilation, disturbances sense
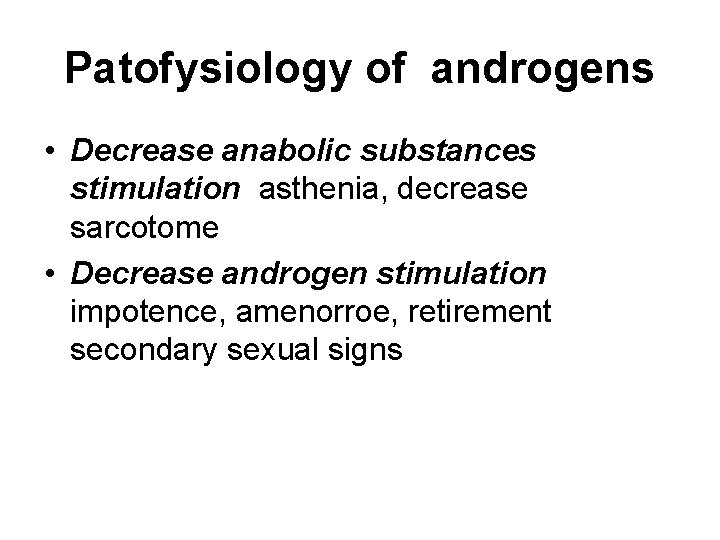
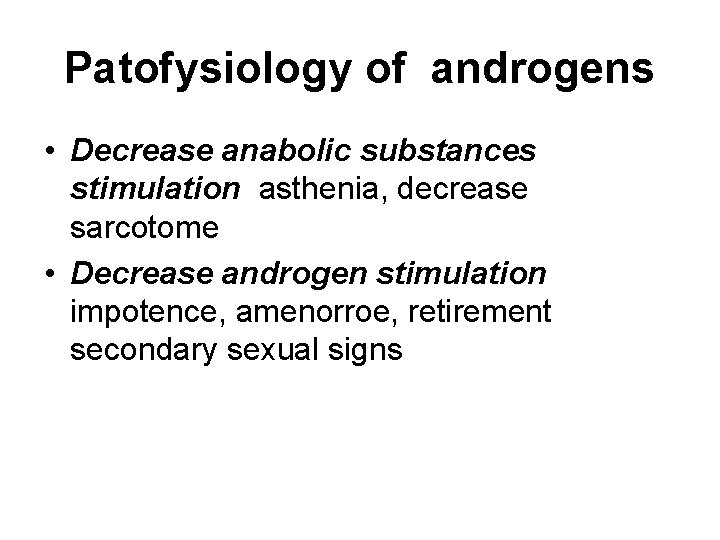
Patofysiology of androgens • Decrease anabolic substances stimulation asthenia, decrease sarcotome • Decrease androgen stimulation impotence, amenorroe, retirement secondary sexual signs
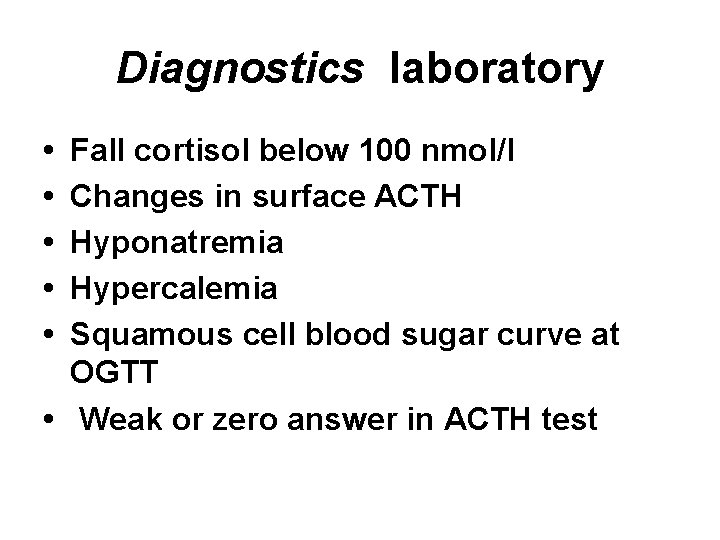
Diagnostics laboratory • • • Fall cortisol below 100 nmol/l Changes in surface ACTH Hyponatremia Hypercalemia Squamous cell blood sugar curve at OGTT • Weak or zero answer in ACTH test
Diagnostics of Addisonism Differential diagnosis • 1. construction sequence cases weakness, decrease yoke, anorexia, hypotension, diarrhoeas (gasteroenteritis, appendicitis, NPBacute abdominal cases, DM, Tx) • 2. construction sequence cases muscular adynamia ( we myasthenia syndromes)

Differential diagnosis II • 3. construction sequence cases with hyperpigmentation (porfyria, chronic liver dissease, hemochromatosis) • 4. construction sequence cases after bunk - up korticoicoids- relative hypocorticolism
Chronic adrenal insuficience Substitute therapy • 10 as far as 35 mg cortisol every day according to materiality p. about. • Hydrocortison digitizer. a 10 mg preservation rhythm • Synthetic korticoids always (Prednison) - mineralocorticoid! 1/4 digitizer. 9 - alpha- fluorokortizol (Florinef)
Reservation surgical achievements • Preoperative dosage 50 mg Hydrocortison and. m. or 100 mg and. v. (in infusion) • During operation 100 mg and. v. a 4 throw • After operation 50 as far as 25 mg and. m. /day until at application p. o.
Secondary adrenal insuficience Therapy • 1. Begin displacement • 2. Ablation causes -e. g. hypotyreosis
Addisons crisis Etiology • Crossing unrecognized or untreated insuficience to the crisis • Low treatment insuficience- stress, stress • Sudden bunk - up glucoortidoid therapy • Sudden destruction adrenal - bleeding,
Addisons crisis Symptoms • Muscular weakness, heavy adynamy as far as paralytic dementia limbs • Vomit, diarrhoea, coeliac colic • Hypotention, hypovolemia, hyponatremia • Circulatory malfunctioning, disturbances of kardiology- arythmia • Irritation and later apathy as far as somnolence
Addisons crisis Therapy • Bolus 100 mg Hydrocortisonu and. v. • Infusion 100 mg Hydrocortisonu and. v. a 1 throw. after 6 throw. • Supply liquid 2 - 4 l/day in infusion ev. inclusive glucose

Addisons crisis Therapy • After stabilization ( circulation, minerals etc. . ) - 50 mg and. m. a 12 h. • Displacement preparation p. about. antibiotics, treatment evocatory causes
Suprarenal overaction • Hypercorticolisms • Hyperaldosteronisms • Overproduction androgens or estrogens
Hypercortisolism Prime (Cushing´s sy. ) • Overproduction glucocorticoids mineralocorticoids, adrenal androgens • adenoma of adrenal gland • carcinoma of adrenal gland • ectopia or deposit of remnants andrenal tissues
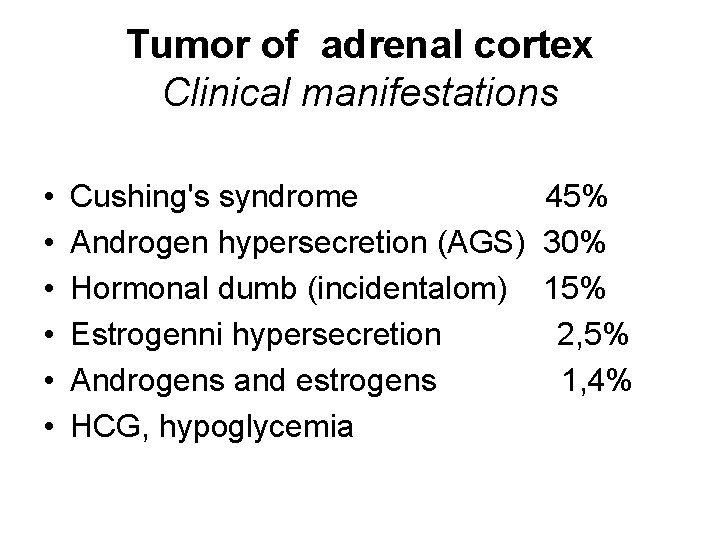
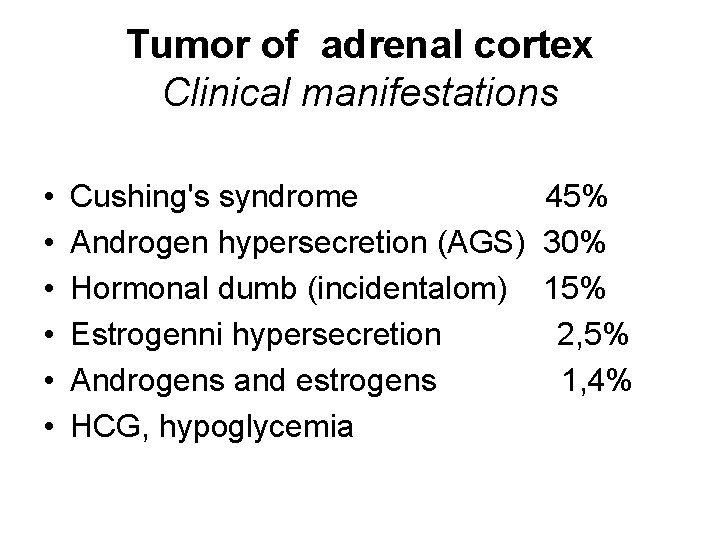
Tumor of adrenal cortex Clinical manifestations • • • Cushing's syndrome Androgen hypersecretion (AGS) Hormonal dumb (incidentalom) Estrogenni hypersecretion Androgens and estrogens HCG, hypoglycemia 45% 30% 15% 2, 5% 1, 4%

Hypercortisolism Clinical symptoms • • Marigold face Central obesity Hypertension Pletora Amenorroe Hirsutismus (women) Adynamia, weakness 88% 86% 85% 77% 72% 67%

Hypercortisolism Clinical symptoms II • • Reds stria, ecchymosis Fragility capillary Osteoporosis Dropsy subcutis Fat deposition piggyback Acne Mental changes 60% 59% 58% 57% 54% 46%
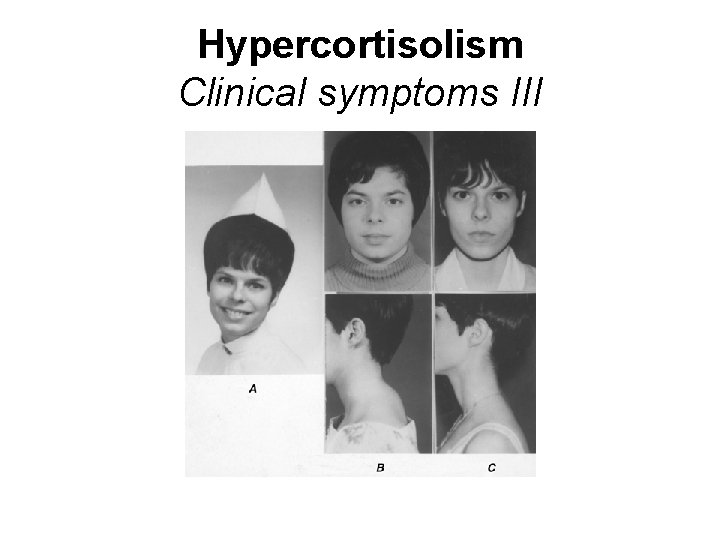
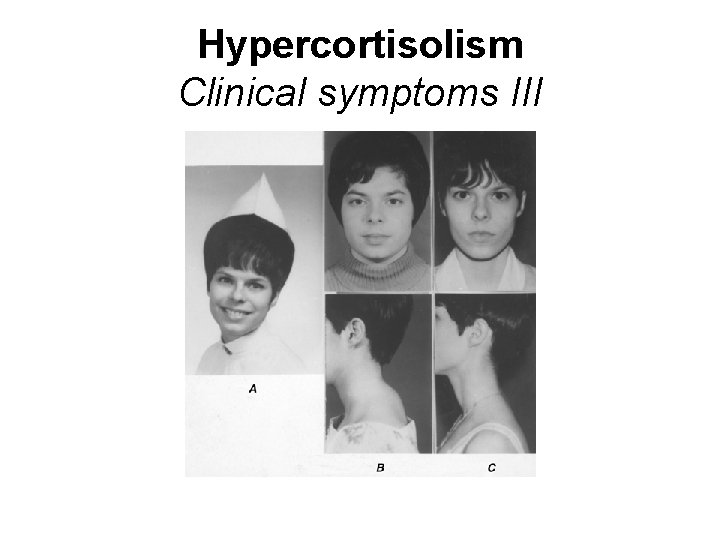
Hypercortisolism Clinical symptoms III
Hypercortisolisms Patofysiology of glucocorticoids • Sugars - diabetic resp. prediabet. metabolism, hyperglykemia, steroid diabetes, polyuria, polydypsia, nycturia • Proteins - adynamia, decrease sarcotome, osteoporosis • Lipids - lunar face, buffalo hump, centripetal distribution oil, arteriosclerosis, xantelasma
Clinical symptoms Patofysiology of glucocorticoids II • Haemopoiesis - polyglobulia, leucocytosis, eosinopenia, lymfopenia, trombocytosis, fall antithrombin • Mesenchyme. tissues stria, ecchymosis, purples, took immunity response • Mineralocorticoid. receptors- hypertension • CNS endocrinous psycho - complex
Clinical symptoms Patofysiology III • Surplus aldosterone propensity to hypokalemia, alkalosis and hypernatremia • Surplus androgens partial compensation proteinocatabolic effect of glucorticoids, virilization, acne, hirsutismu, amenorroe
Hypercorticolism • Primary Lowered performance ACTH • Secondary 1. increased performance ACTH 2. lowered performance ACTH
Hypercortisolism Primary • Cushing´s sy. contingent adrenal- tumors of adrenal cortex • Cushing´s sy. contingent ectopia adrenal tissue weaving tumours from adrenal the rest in ovarium or testicle, tumours from adrenal the rest
Hypercortisolism Secondary higher ACTH • Cushing´s sy. hypotalamus - hypophysis (Cushing´s dissease) basophilic or chromofobic adenoma hypophysis, malignant tumours or other lesion, disorder issue CRH • Cushing´s sy. parenoplastic influence peptide with effects ACTH from extrahypofysary tumours (pulmonary etc. )
Hypercortisolism Secondary starvation wages ACTH • Iatrogenic Cushing´s sy. after therapy corticoids or ACTH • Cushing´s sy. with relative hypercotisolism - lowered concetration of transcortin or incompatibility between cortisol-transcortin
Hypercortisolism Prime - diagnostics • High cortisol • Starvation wages ACTH • Adrenal steoidogenesis- inadequate responsive to ACTH • Dexametazon test
Hypercortisolism Secondary - diagnostics • High cortisol • High ACTH ( except bunk - up corticoids and sy. of lowered transkortin!) • Sonografy, CT, bllod tests of steroids after katetrisation of adrenal venous orifice, RTG pulmonary and mediastinum (paraneoplast. )

Hypercortisolism CT - diagnostics

Hypercortisolism Diagnostics fluxional • Obesity (often with DM and hypertensive) cortisol in urine higher cortisol/creatinine - normal purview supresion cortisol – Dexametazon • Sy. Stein Levethal (PCO) sonografy of ovary
Hypercortisolism Therapy • First fiddle. Cushing. sy. adrenalectomia + displacement • Cut. Cushing. sy. adrenalectomia thumped. + displacement • Inoperable construction sequence cases - blockers adrenal steroidogenesis
Hypercorticolism Therapy complication St. p. bilateral adrenalectomy near 7% cases happens to growth reactive hypofyseal adenomas (Nelsonuv sy. ) 50% radical neurosurgery solving
Hyperaldosteronism • Prime - Conn´s sy. adenoma more often sinistral less commonly malignant • Secondary metabolic response with adaptation character from extraadrenal dissease, stimulate system renin- angiotenzin

Hyperaldosteronism

Hyperaldosteronism Prime symptoms • HYPOCALEMIA muscular weakness, fatigue, hypocalemic changes on EKG • HYPERNATREMIA benign hypertension, cefalgia, retinopatia, aggramdizement heart, less frequent dropsies
Hyperaldosteronism Prime symptoms II • KIDNEY hypostenuria, isostenuria, proteinuria, nycturia, polydipsia, lower titrating acidity urine, higher content ammonium ions in urine • ALKALOSIS parestezia

Hyperaldosteronism Prime diagnostics • High surface aldosterone and his metabolites in urine • High surface aldosterone an blood test and after katetrisation of adrenal lived • Low plasmatical surface of renin • Normal surface of 17 - cetosteroids and 17 - hydroxycorticoids
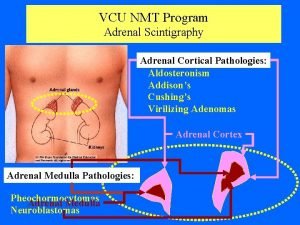
Hyperaldosteronisms Prime diagnostics II • Imaging method sonografy CT scintigrafy 19 -125 I cholesterol
Hyperaldosteronism Prime therapy • Adrenalektomia 2/3 standardization hypertensive (months) 1/5 improvement hypertensive always - ren. insuf. cut - and dry • Conservatively (inoperable construction sequence cases) Spirolakton in high taxs (300 - 400 mg) every day
Hyperaldosteronism Secondary - aetiology • Stimulation system renin- angiotenzin Reno - vascular hypertensive, malignant hypertensive overproduction of renin (haemangiopericytoma renis, Robertsons sy. ) hyperplasy ev. Hypertrophy of juxtaglomerular apparatus

Hyperaldosteronisms Secondary - aetiology II • Tubulopaty of kidney – Bartter´s sy. (isn't backward resorpse on) • Overproduction ACTH
Hyperaldosteronism Secondary • Increased surface of aldosterone • Increased surface of renin • Therapy evocatory causes • Spirolakton
Adrenal hyperandrogenism • Clinical manifestations - Adrenogenital sy. • Tumour or hyperplasia cortices adrenal selective disorder steroidogenesis • Overproduction C 19 steroids adenoma or carcinoma
Adrenal hyperandrogenism • Clinical symptoms of virilization near women with hirsutism, hypertrichosis, hair loss • Imaging method • Single out gonadoblastoma overproduction - tumours • Surgical solving

Adrenal hyperestrogenism • Insulated hypersecretion rare, more often with others steroids • Men - waste virilization signs, gynecomastia, atrophy testicles • Women - disturbances cycle and hypermenorroe

Steroid enzymopaty • Metabolism disturbances steroidogenesis • Dissociation adrenal function • Infliction near initial steps of streoidogenesis – high morbidity and morality

Inborn adrenal hyperplasia with virilization • Inborn Adrenogenital sy. • Block 21 - hydroxylase - light forms 70 % of all hyperplazia, heavy form ( salt disorder) 25% • Block 11 a -hydroxylase 3 % • Next blocks forms c. 1%

Defect 21 - hydroxylase • 17 a- hydroxyprogesteron
Defect 21 - hydroxylase • Light form ACTH, hyperplasia with hypersecretion of mineralocorticoids and cortisol with androgen hyperproduction – virilization of habitus (hypertrophy clitoris) • Heavy form trenchs all corticosteroid drugs - virilization waste salts, manifestations at once post natal - exsiccation, vomit, shock, hypo -Na, hyper- K
Steroid enzymopaty Therapy complex • Glucokorticoids - supresesion adrenal stimulation ACTH and overproduction C 19 steroids, at disorder synthesis mineralocorticoid - Florinef • Poverty of androgens – displacement • Virilization near girls - anti - androgens
ADRENAL MEDULLA
Secretion of catecholamines • 90% adrenal pith • 10% chromium - affine tissue except adrenal medula – paragangliomyschemodektoms • paraganglioms- chromium - affine tissue near likable nerve knot on hand • mediastinum, abdomen and saucepan • Zuckerkandl´s organ – chromium - affine tissue near lower mesenteric artery
Pheochromocytoma • Secretion – epinephrine, noradrenaline and dopamin • gastrin, kacitonin, somatostatin, vaso active intestinal peptide (VAS), adrenokortikotropin and adrenomedulin
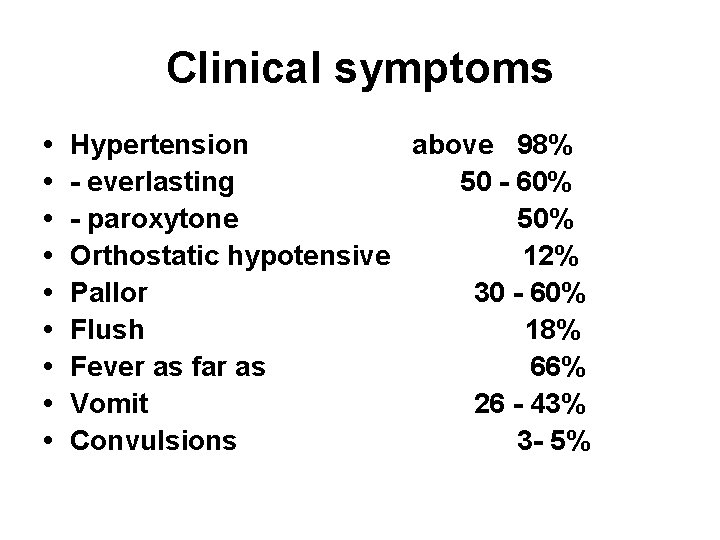
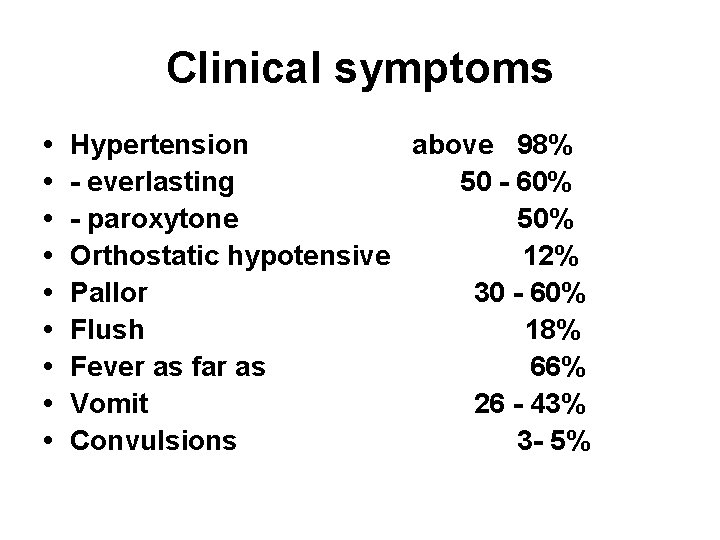
Clinical symptoms • • • Hypertension above 98% - everlasting 50 - 60% - paroxytone 50% Orthostatic hypotensive 12% Pallor 30 - 60% Flush 18% Fever as far as 66% Vomit 26 - 43% Convulsions 3 - 5%

Glucosic metabolism • Hyperglykemia 42% • PGT 60 - 80% • Diabetes mellitus 25%
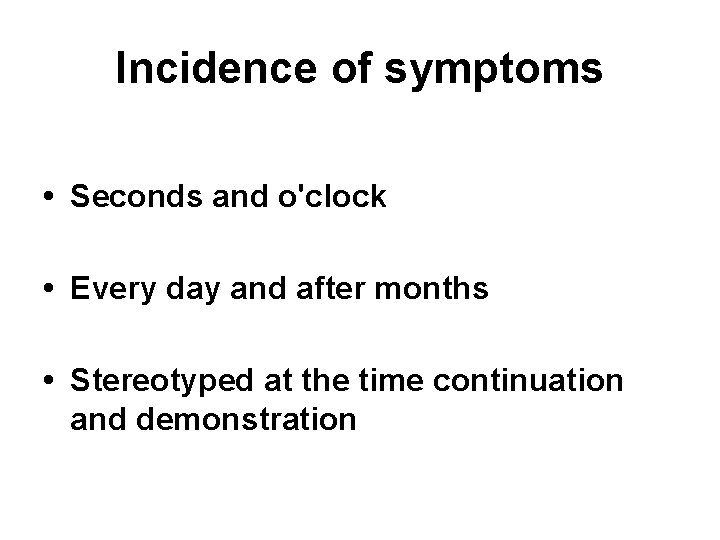
Incidence of symptoms • Seconds and o'clock • Every day and after months • Stereotyped at the time continuation and demonstration

Causes episodic secretion catecholamines • Physical activity, shock • Direct stimulation tumour /tumour urine. bladder/ • Pharmaceuticals – histamine, tyramine, guanethidin, metoklopramid, methyldopa, ethanol, fenothiazin, tricyclic antidepressant drug • Estrogens and STH
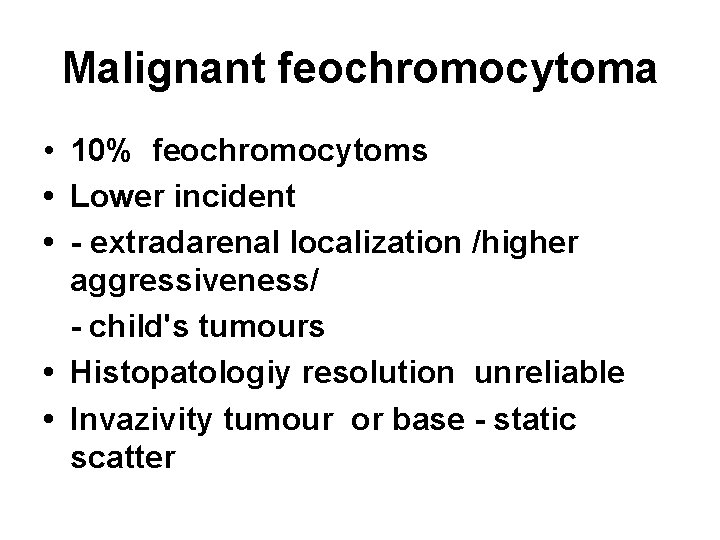
Malignant feochromocytoma • 10% feochromocytoms • Lower incident • - extradarenal localization /higher aggressiveness/ - child's tumours • Histopatologiy resolution unreliable • Invazivity tumour or base - static scatter
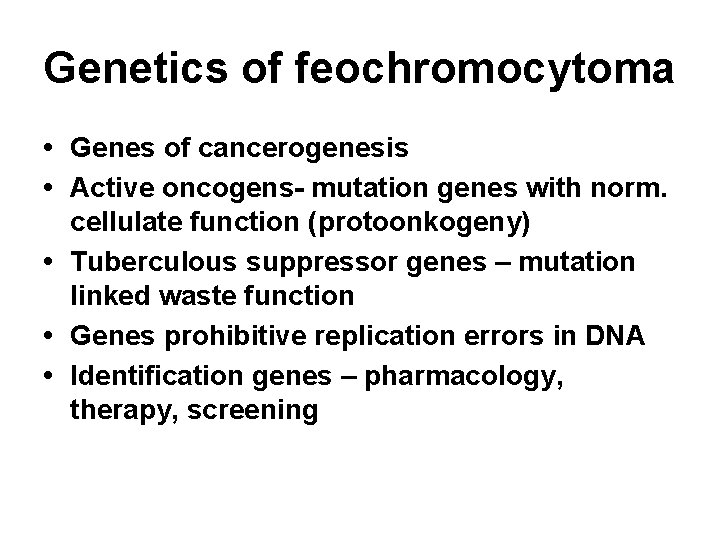
Genetics of feochromocytoma • Genes of cancerogenesis • Active oncogens- mutation genes with norm. cellulate function (protoonkogeny) • Tuberculous suppressor genes – mutation linked waste function • Genes prohibitive replication errors in DNA • Identification genes – pharmacology, therapy, screening
Familiarity of feochromocytoma • MEN 2 • von Hippel- Lindu illness (VHL) • Neurofibromatosis type I
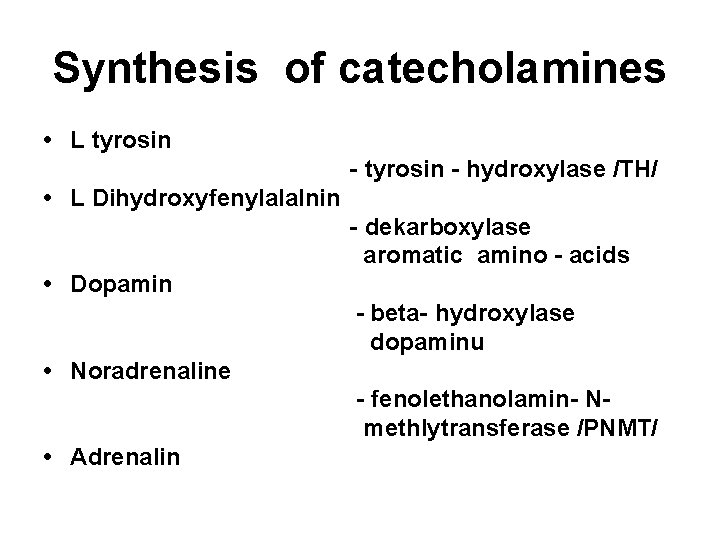
Synthesis of catecholamines • L tyrosin - hydroxylase /TH/ • L Dihydroxyfenylalalnin - dekarboxylase aromatic amino - acids • Dopamin - beta- hydroxylase dopaminu • Noradrenaline - fenolethanolamin- Nmethlytransferase /PNMT/ • Adrenalin
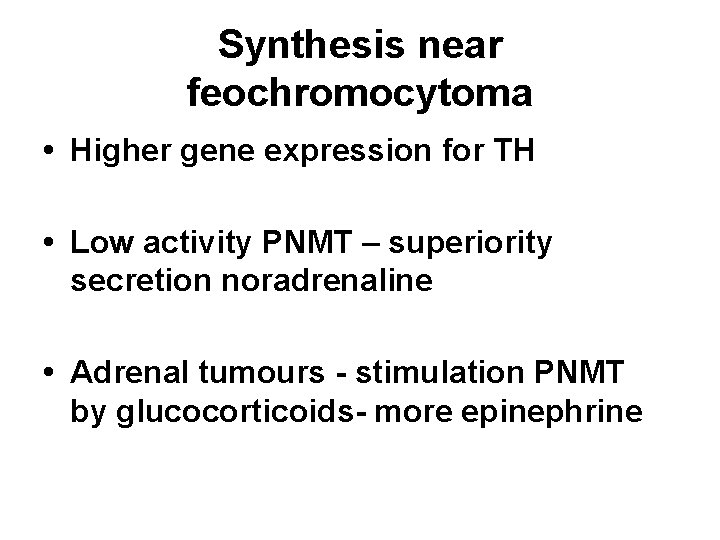
Synthesis near feochromocytoma • Higher gene expression for TH • Low activity PNMT – superiority secretion noradrenaline • Adrenal tumours - stimulation PNMT by glucocorticoids- more epinephrine
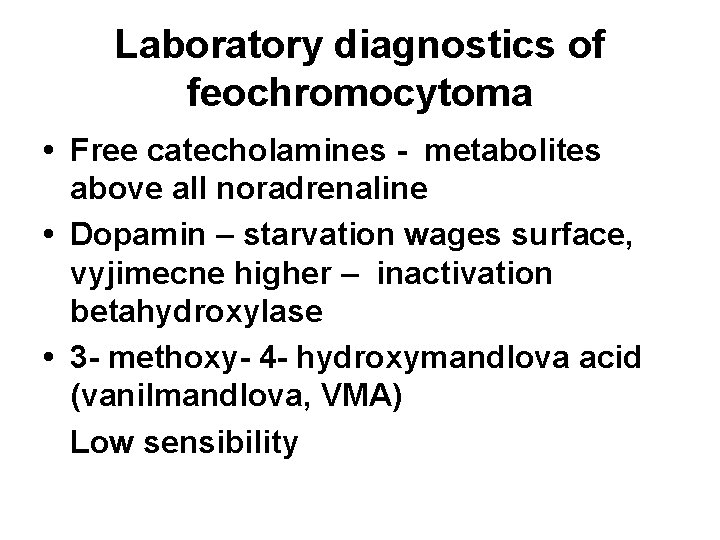
Laboratory diagnostics of feochromocytoma • Free catecholamines - metabolites above all noradrenaline • Dopamin – starvation wages surface, vyjimecne higher – inactivation betahydroxylase • 3 - methoxy- 4 - hydroxymandlova acid (vanilmandlova, VMA) Low sensibility
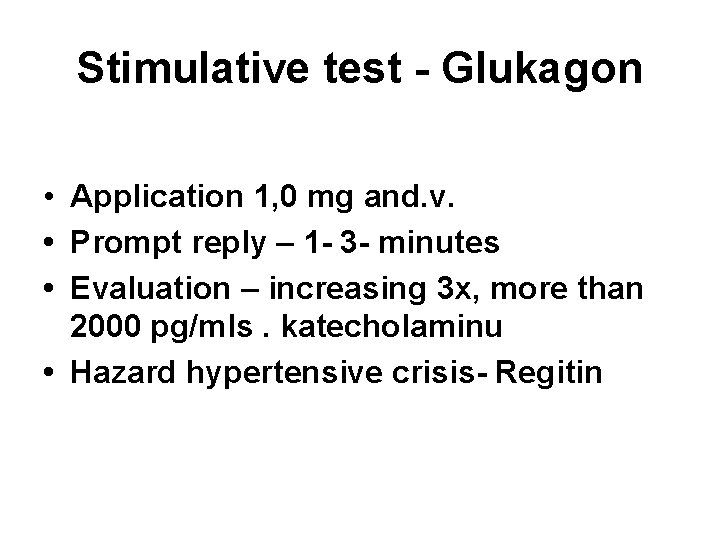
Stimulative test - Glukagon • Application 1, 0 mg and. v. • Prompt reply – 1 - 3 - minutes • Evaluation – increasing 3 x, more than 2000 pg/mls. katecholaminu • Hazard hypertensive crisis- Regitin
Supresion test - Klonidin • Alfa 2 adrenoreceptor´s agonist inhibits vacation noradrenaline • Feochromocytoma - without response • Application 0, 3 mg p. o. Absence fall noradrenaline below 500 pg/ml, behind 2 - 3 o'clock, different kriteria • Hazard bradycardia and hypotension

Evaluation tests • Glukagony specificity 100% sensibility 81% • Klonidin specificity 67% sensibility 97% • Combination 80% handhold disorder • Farmakolog. interference – tricyclic antidepressant drug
Imagine of tumor • CT 85 - 95% • MRI – better record, largely extra - adrenal localization • MIBG – 123 I and 131 I /metajodbenzylguanidin/ • 111 I octreotid – malignant feochromocytom • Positron emissive tomography /PET/ - (18 F) -fluorodeoxyglukoza - (11 C) -hydroxyefedrin
Incidentalom • Dispenzarisation – repeated taking • Above 3 cm – surgical solving

Therapy of Feochromocytoma Pre - operative • Stationary bllood pressure 2 - 4 for weeks before operation • Alpha adrenergic blockers
Alpha adrenergic blockers • • Fenoxybeznamin /Dibenylin cps. / • Prazosin /Deprazolin 1 mg, 2 mg digitizer. , , Adversuten 1 mg, 5 mg digitizer. stainless steel. /
Pre - operative options • TK no transcendent 160/90 mm Hg • Orthostatic hypotensixe below 80/45 mm. Hg • Max. 1 cellular extra - systole behind 5 mine. , , EKG without elevace or depression ST and inversion Tvlny
Surgical therapy • Preference laparoscopy achievements • Prevention hypovolemie and hypoglykemie • Selection anaesthetic – halotan increases sensibility myocardium on catecholamines
Postoperative care • Surgical verification laboratory max. behind 2 for weeks • Dispensarisation – lab. verification 1 x yearly after 5 years

Inoperable construction sequence cases • Fenoxybenzamin – Dibenylin • Metyrosin Demser
Cytostatic treatment malignity • Cyklofosfamid, Vinkristin, Dacarbazin • adjustment clinic near 57% • laboratory answer 79%

Other options therapy • Octerotid or alpha interferon • • 50% without progression tumour 2/3 improvement pac. with diarrhoeas, gob and brochoconstriction
Next therapy • Bone implantation – external radiating • MIBG – high doses

Forecast after operation Benign – quinquennial survival 95% Malignant – quinquennial survival 35 60%
 Adrenal gland regions
Adrenal gland regions Relation of suprarenal gland
Relation of suprarenal gland Ultimobranchial body
Ultimobranchial body Adrenal gland regions
Adrenal gland regions Adrenal gland hormones
Adrenal gland hormones Summary of adrenal gland
Summary of adrenal gland Cat digestive
Cat digestive Adrenal gland
Adrenal gland Ectocrine
Ectocrine Cells of adrenal gland
Cells of adrenal gland Parasympathetic and sympathetic
Parasympathetic and sympathetic Adrenal gland epithelium
Adrenal gland epithelium Acth
Acth My little vintage
My little vintage Luisa espinosa593
Luisa espinosa593 Xxxx vintage
Xxxx vintage Vintage
Vintage Endomort
Endomort Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Pineal gland pituitary gland
Pineal gland pituitary gland Malingering
Malingering 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad Raa pathway
Raa pathway Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Adrenal drugs pharmacology
Adrenal drugs pharmacology Capta rh
Capta rh Adenoma
Adenoma Site:slidetodoc.com
Site:slidetodoc.com Congenital adrenal hyperplasia electrolytes
Congenital adrenal hyperplasia electrolytes Slide
Slide The suprarenal (adrenal) medullae secrete
The suprarenal (adrenal) medullae secrete Adrenal cushing
Adrenal cushing Menopause and mania
Menopause and mania Adrenal insufficency
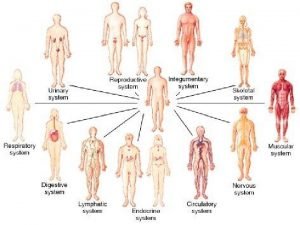
Adrenal insufficency Human body organ systems
Human body organ systems Mineralocorticoid function
Mineralocorticoid function Adrenal glands
Adrenal glands Adrenal cortex develops from
Adrenal cortex develops from Caso clínico sop
Caso clínico sop Adrenal bezin hipofonksiyonu sonucu gelişen tablo
Adrenal bezin hipofonksiyonu sonucu gelişen tablo Adrenal hormone pathway
Adrenal hormone pathway Schlussel urology
Schlussel urology Thyroid
Thyroid Adrenal yetmezlik acilci
Adrenal yetmezlik acilci Adrenal bez histolojisi
Adrenal bez histolojisi Kolekalsiferol
Kolekalsiferol Cortex
Cortex Adrenal cushing
Adrenal cushing Adrenal medulla cortex
Adrenal medulla cortex Non klasik kah
Non klasik kah Addison's disease vs cushing's syndrome
Addison's disease vs cushing's syndrome Adrenal fatigue symptoms
Adrenal fatigue symptoms Adrenal sympathetic pathway
Adrenal sympathetic pathway 21 hydroxylase deficiency
21 hydroxylase deficiency Hipotálamo-hipófise-adrenal
Hipotálamo-hipófise-adrenal Arka hipofiz hormonları
Arka hipofiz hormonları Costan mefenamic acid
Costan mefenamic acid Adrenal sympathetic pathway
Adrenal sympathetic pathway Psödocushing
Psödocushing Vad är densitet
Vad är densitet Kung som dog 1611
Kung som dog 1611 Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Vad är referatmarkeringar
Vad är referatmarkeringar Texter för hinduer tantra
Texter för hinduer tantra Fimbrietratt
Fimbrietratt Arkimedes princip formel
Arkimedes princip formel Större än
Större än Magnetsjukhus
Magnetsjukhus Elektronik för barn
Elektronik för barn Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Toppslätskivling effekt
Toppslätskivling effekt Borra hål för knoppar
Borra hål för knoppar Bra mat för unga idrottare
Bra mat för unga idrottare Läkarutlåtande för livränta
Läkarutlåtande för livränta Jiddisch
Jiddisch Ledarskapsteorier
Ledarskapsteorier Datorkunskap för nybörjare
Datorkunskap för nybörjare Ellika andolf
Ellika andolf Returpilarna
Returpilarna Rita perspektiv
Rita perspektiv Fspos
Fspos Redogör för vad psykologi är
Redogör för vad psykologi är Mitos steg
Mitos steg Bästa kameran för astrofoto
Bästa kameran för astrofoto Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Klassens mamma rim
Klassens mamma rim Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Gibbs reflekterande cykel
Gibbs reflekterande cykel Fredsgudinna pax
Fredsgudinna pax Tidbok
Tidbok Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Expektans eller exspektans
Expektans eller exspektans Sten karttecken
Sten karttecken Kanaans land
Kanaans land Ro i rom pax
Ro i rom pax Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Shingelfrisyren
Shingelfrisyren Ledningssystem för verksamhetsinformation
Ledningssystem för verksamhetsinformation Matematisk modellering eksempel
Matematisk modellering eksempel Bris för vuxna
Bris för vuxna Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Trög för kemist
Trög för kemist Urban torhamn
Urban torhamn Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Påbyggnader för flakfordon
Påbyggnader för flakfordon Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning