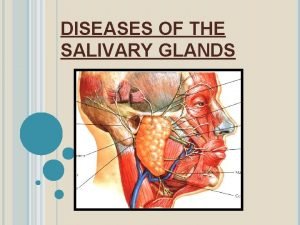
DISEASES OF THE SALIVARY GLANDS 1 Sialolithiasis Nonspecific
- Slides: 47
DISEASES OF THE SALIVARY GLANDS 1
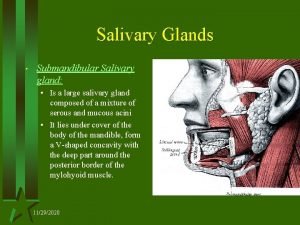
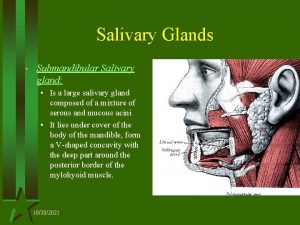
Sialolithiasis & Nonspecific sialadenitis • Submandibular • Stones nidus - impacted food debris - dehydration with decreased secretion • Stone → duct obstruction • Nonspecific interstitial inflammation • Or suppuration (abscess) – Staph. Strep 2
Sialolithiasis & Nonspecific sialadenitis • • Unilateral Painful – during meals Purulent ductal discharge + Recurrent 3
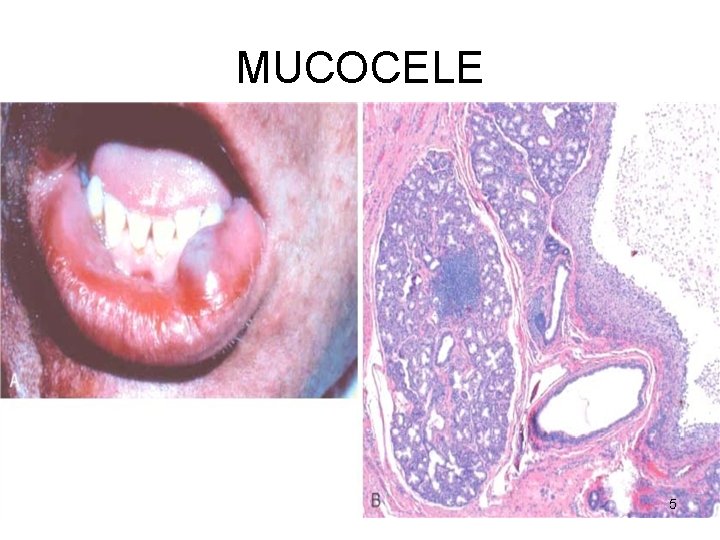
MUCOCELE • • Trauma Lower lip Fluctuant swelling Blockage / rupture of salivary duct → leakage of saliva into the surrounding stroma • RANULA – mucocele of the sublingual 4
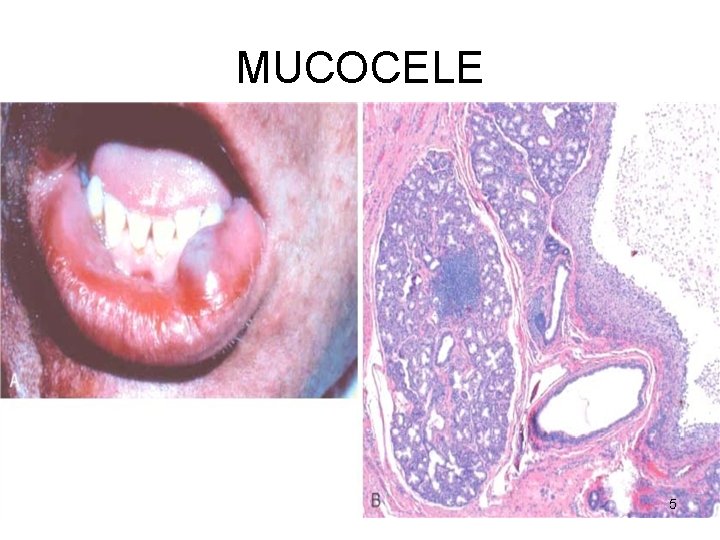
MUCOCELE 5
Sjogren’s syndrome • Immune destruction • Salivary – xerostomia (dry mouth) • Lacrimal – keratoconjunctivitis sicca (dry eyes) 6
TUMOURS • • Approx. 30 in number 2% of all tumours Benign – 5 th – 7 th decade Malignant – later than above 7
BENIGN TUMOURS • • • PLEOMORPHIC ADENOMA – 50% Warthin’s tumour Oncocytoma Basal cell adenoma Canalicular adenoma Ductal papilloma 8
PLEOMORPHIC ADENOMA • Benign tumour of glands – ADENOMA • Remarkable histologic diversity PLEOMORPHIC • Commonest • Also called Mixed tumour – epithelial and connective tissue components 9
PLEOMORPHIC ADENOMA • Cell of origin → EPITHELIAL epithelial-myoepithelial / ductal reserve cells 10
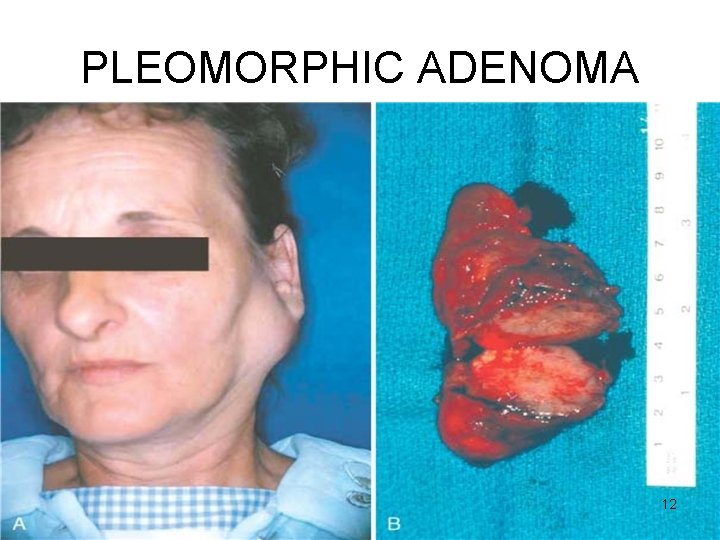
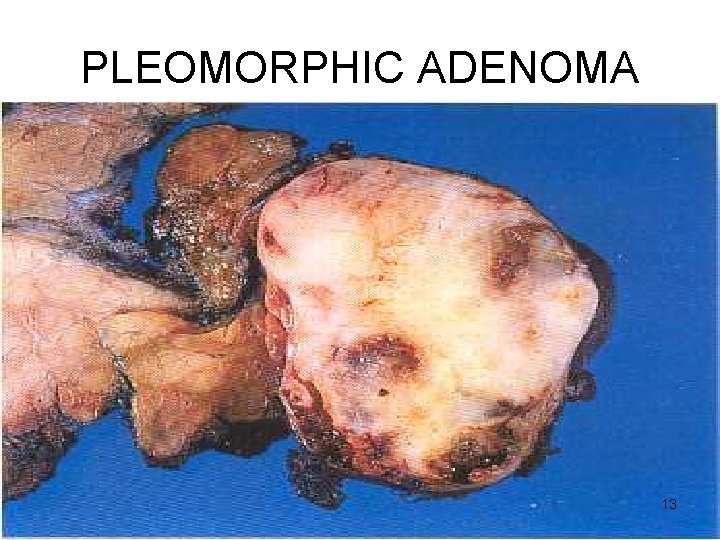
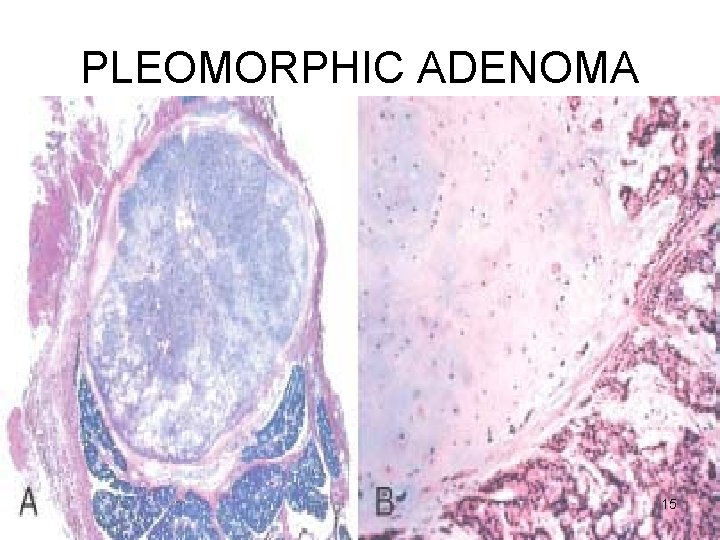
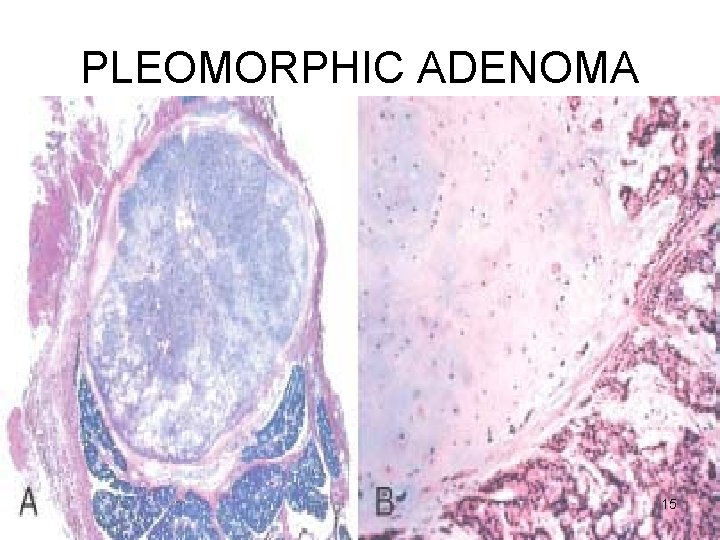
PLEOMORPHIC ADENOMA Gross • < 6 cms • Bosselated • Well-demarcated / encapsulated / tongue-like protrusions • Cut surface: gray-white / variegated / myxoid / bluish translucent (chondroid) 11
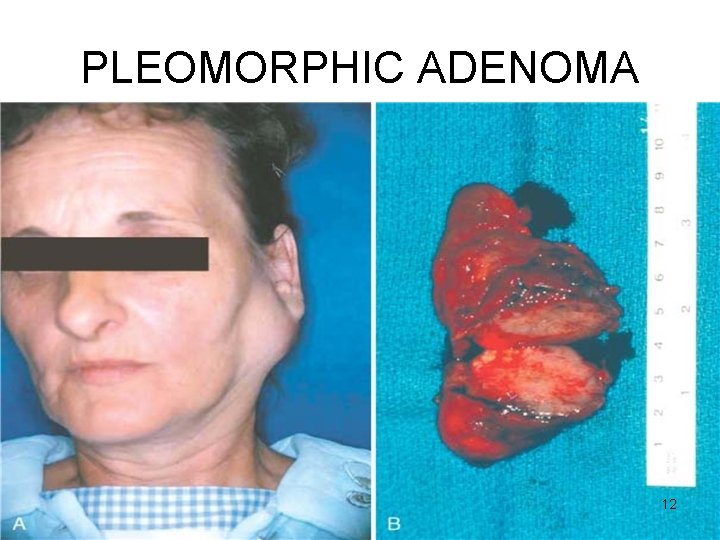
PLEOMORPHIC ADENOMA 12
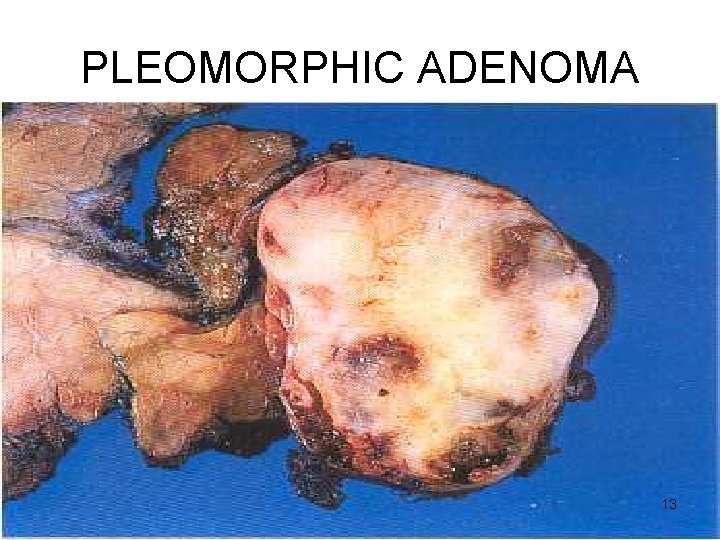
PLEOMORPHIC ADENOMA 13
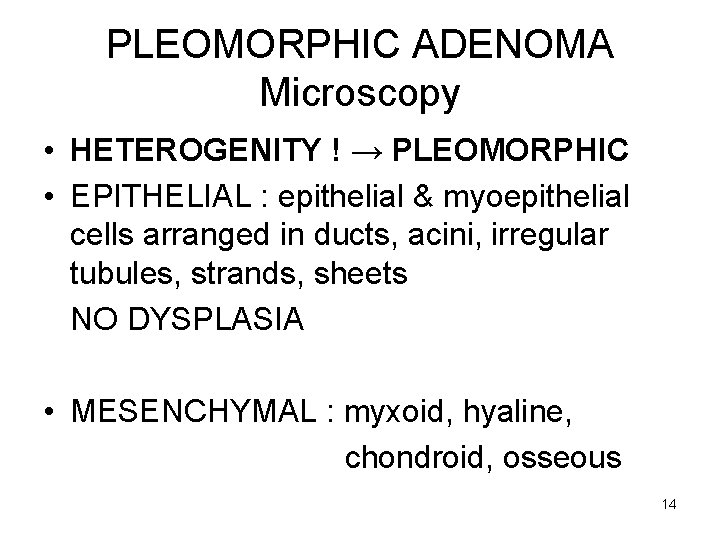
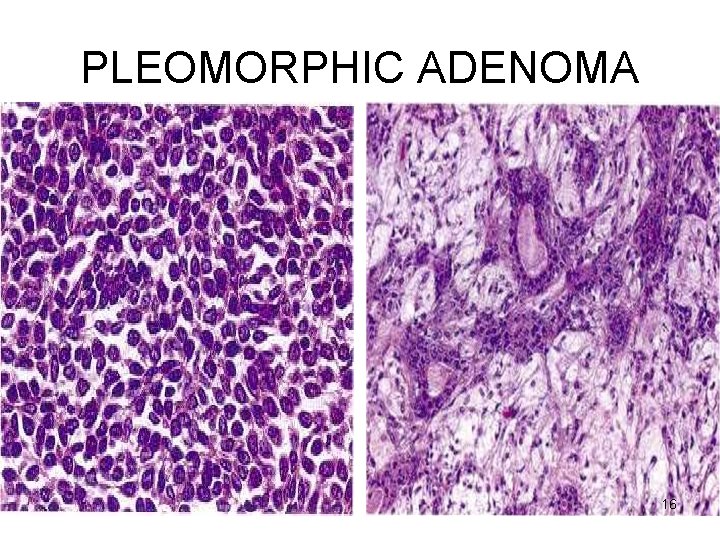
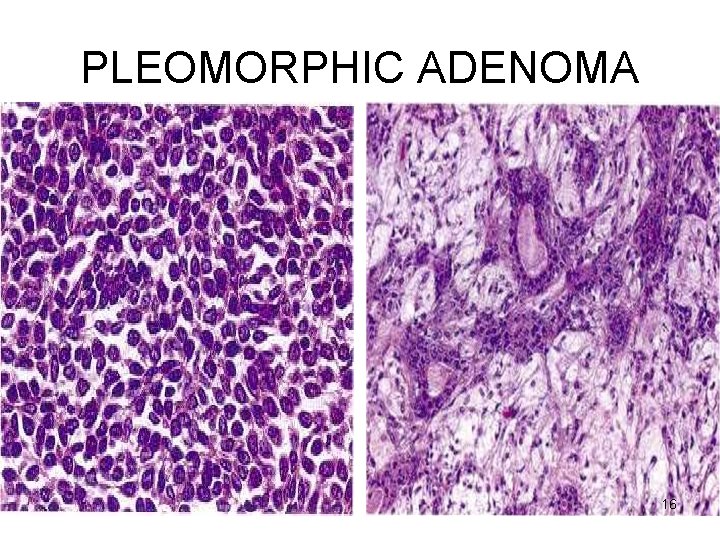
PLEOMORPHIC ADENOMA Microscopy • HETEROGENITY ! → PLEOMORPHIC • EPITHELIAL : epithelial & myoepithelial cells arranged in ducts, acini, irregular tubules, strands, sheets NO DYSPLASIA • MESENCHYMAL : myxoid, hyaline, chondroid, osseous 14
PLEOMORPHIC ADENOMA 15
PLEOMORPHIC ADENOMA 16
PLEOMORPHIC ADENOMA CLINICAL ASPECTS • Slow growing • Painless • Parotid – swelling below & in front of the year • RECURRENT – tongue-like protrusions Enucleation – 25% with Parotidectomy – 4% 17
CARCINOMA ex PLEOMORHIC ADENOMA OR MALIGNANT MIXED TUMOUR Adenocarcinoma 18
WARTHIN’S TUMOUR Papillary cystadenoma lymphomatosum Adenolymphoma 19
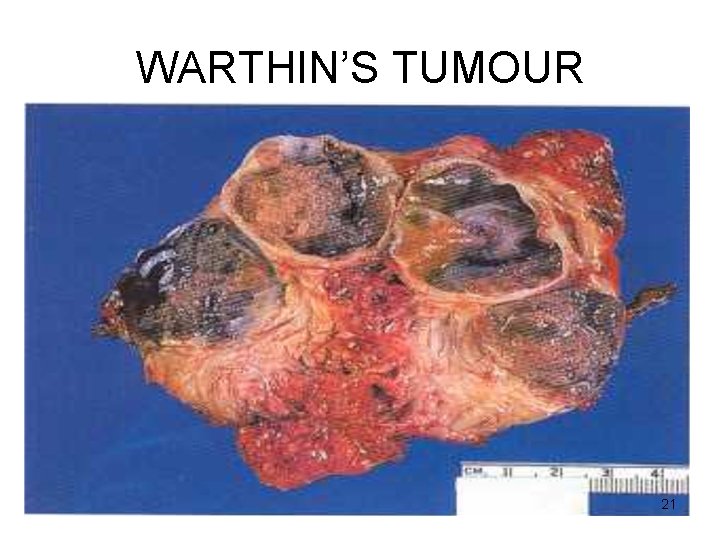
WARTHIN’S TUMOUR Gross • Encapsulated • Cut surface : pale-grey narrow cystic / cleft-like / convoluted spaces contain serous / mucinous fluid 20
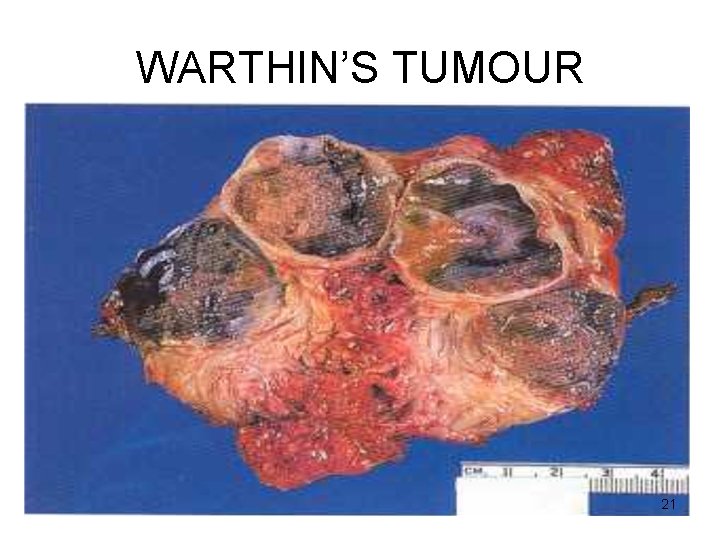
WARTHIN’S TUMOUR 21
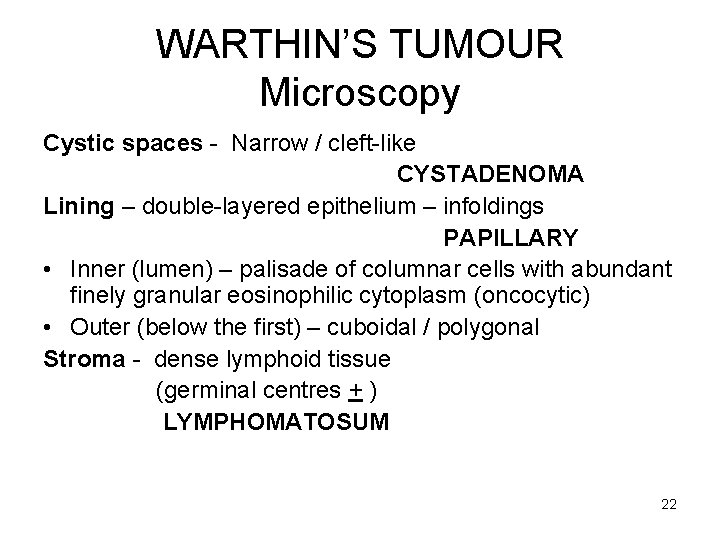
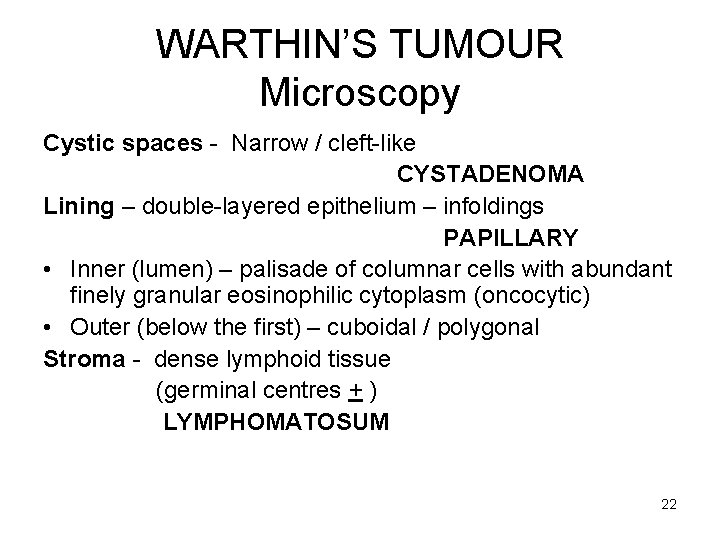
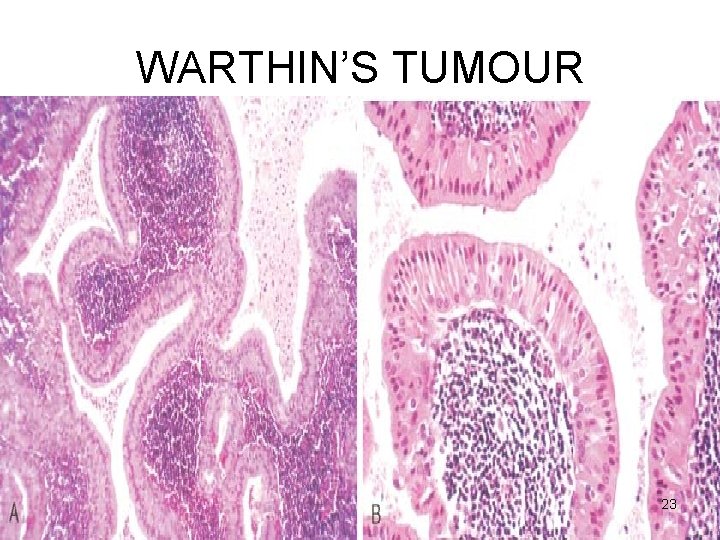
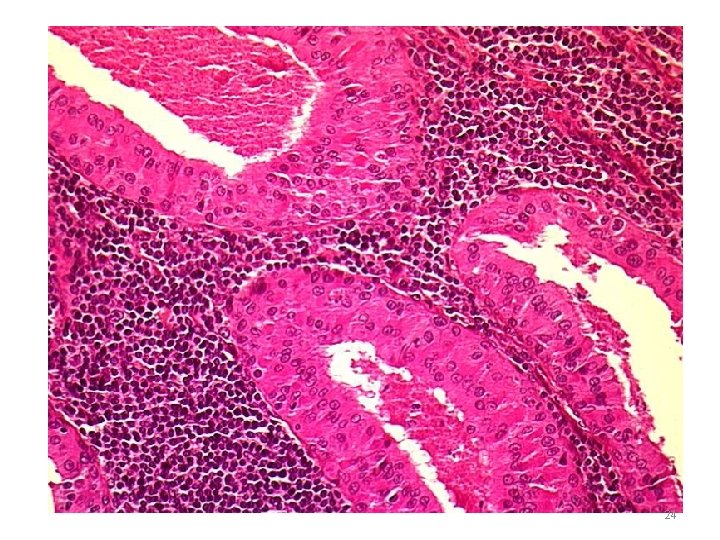
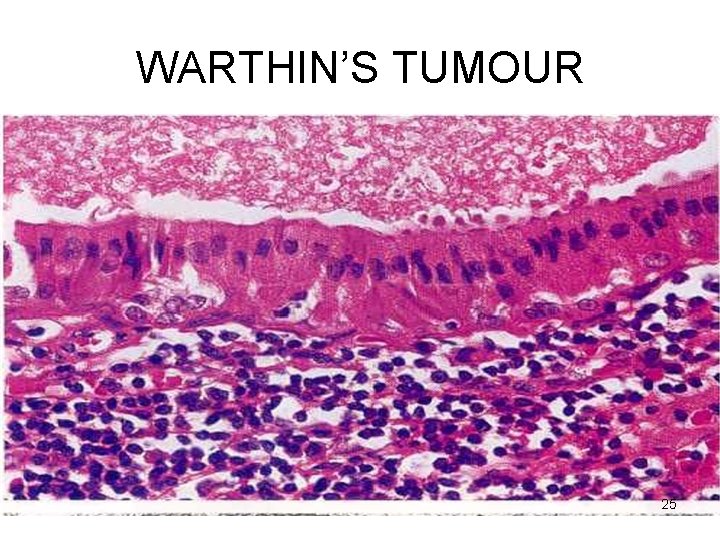
WARTHIN’S TUMOUR Microscopy Cystic spaces - Narrow / cleft-like CYSTADENOMA Lining – double-layered epithelium – infoldings PAPILLARY • Inner (lumen) – palisade of columnar cells with abundant finely granular eosinophilic cytoplasm (oncocytic) • Outer (below the first) – cuboidal / polygonal Stroma - dense lymphoid tissue (germinal centres + ) LYMPHOMATOSUM 22
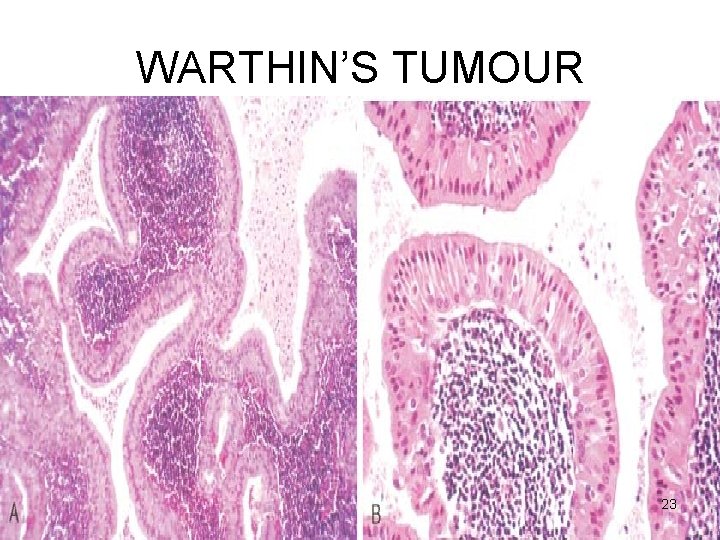
WARTHIN’S TUMOUR 23
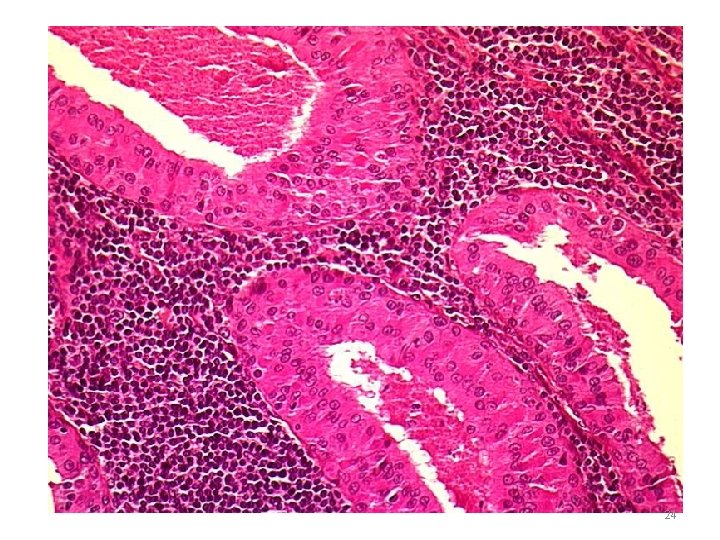
24
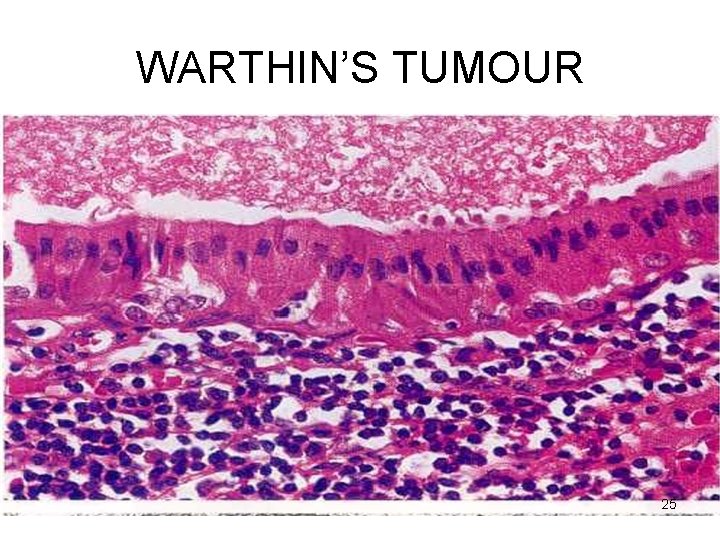
WARTHIN’S TUMOUR 25
WARTHIN’S TUMOUR • HISTOGENESIS ? Aberrant inclusions of lymphoid tissue in salivary glands 26
WARTHIN’S TUMOUR CLINICAL ASPECTS • Benign • Very rarely recurs 27
MALIGNANT TUMOURS • • Mucoepidermoid ca Acinic cell ca Adenoid cystic ca Malignant mixed tumour 28
Malignant tumours • Old age • Max (70 -90%) – sublingual • Malignant tumours more in smaller glands 29
MUCO-EPIDERMOID CARCINOMA • 15% • 60 -70% in the parotid, also in others • MOST COMMON MALIGNANT • Most common radiation-induced 30
MUCO-EPIDERMOID CARCINOMA Gross • < 8 cms. • Apparently circumscribed / infiltrative • Cut surface : pale grey-white small mucin-filled cysts 31
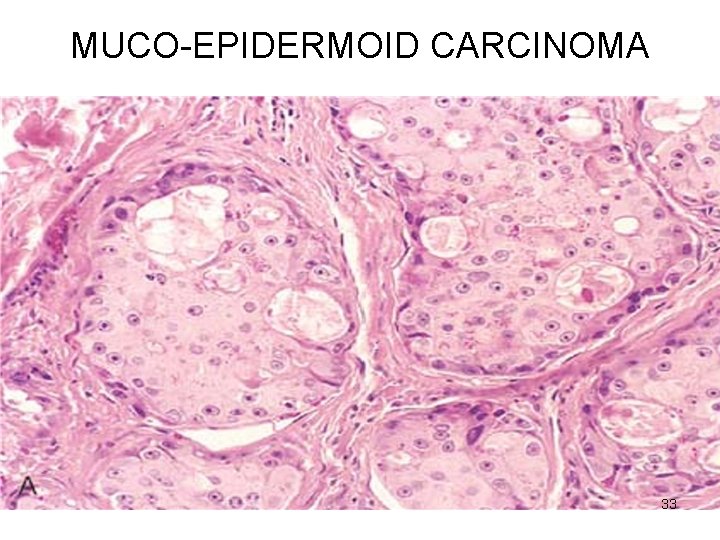
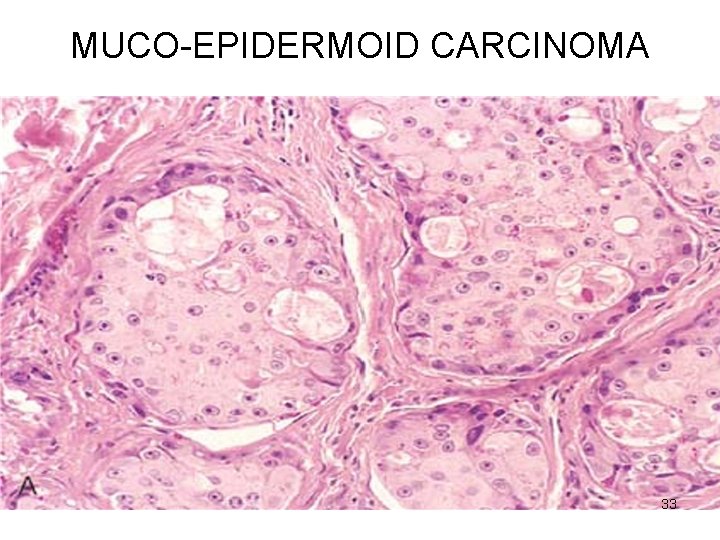
MUCO-EPIDERMOID CARCINOMA Microscopy • Mixtures of three cell types arranged in cords, sheets, cystic 1. mucus-secreting cells 2. intermediate cells (hybrid) squamoid features with small to large mucusfilled vacuoles 3. squamous cells 32
MUCO-EPIDERMOID CARCINOMA 33
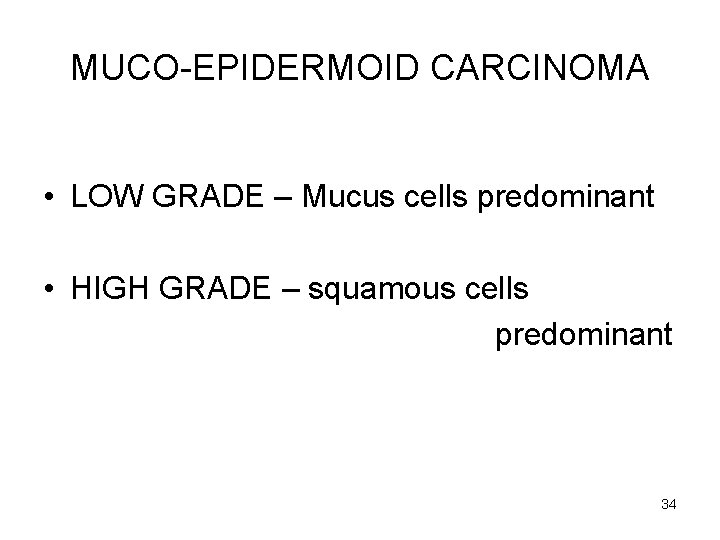
MUCO-EPIDERMOID CARCINOMA • LOW GRADE – Mucus cells predominant • HIGH GRADE – squamous cells predominant 34
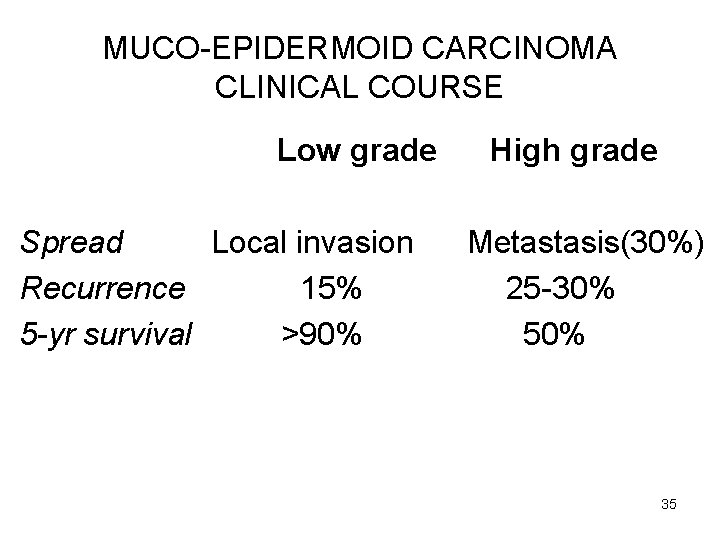
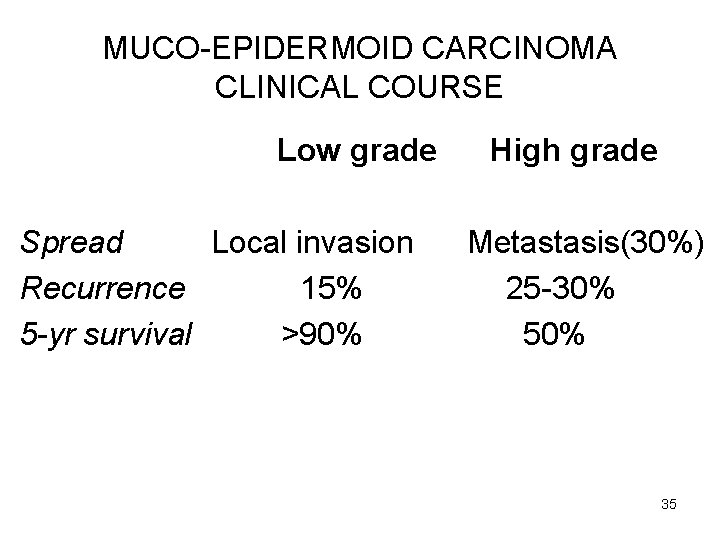
MUCO-EPIDERMOID CARCINOMA CLINICAL COURSE Low grade Spread Local invasion Recurrence 15% 5 -yr survival >90% High grade Metastasis(30%) 25 -30% 50% 35
ADENOID CYSTIC CARCINOMA • Mouth – minor, rare in parotid • Nose, paranasal sinuses • Upper airways 36
ADENOID CYSTIC CARCINOMA Gross • Small • Poorly encapsulated, infiltrative • Gray-pink 37
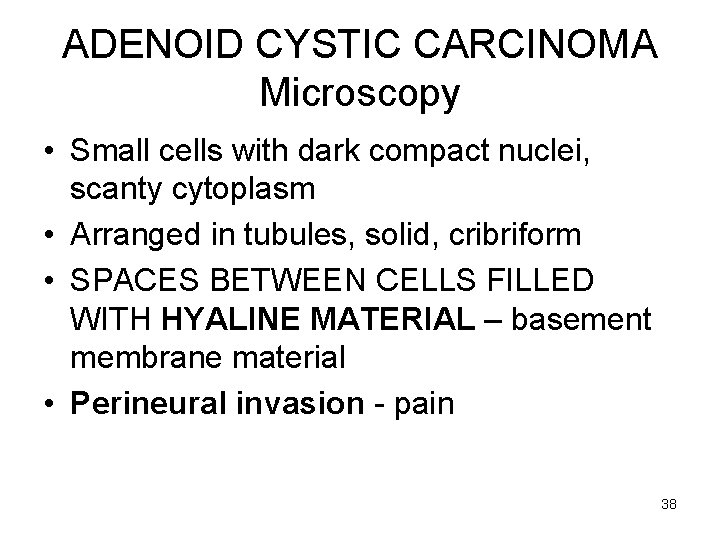
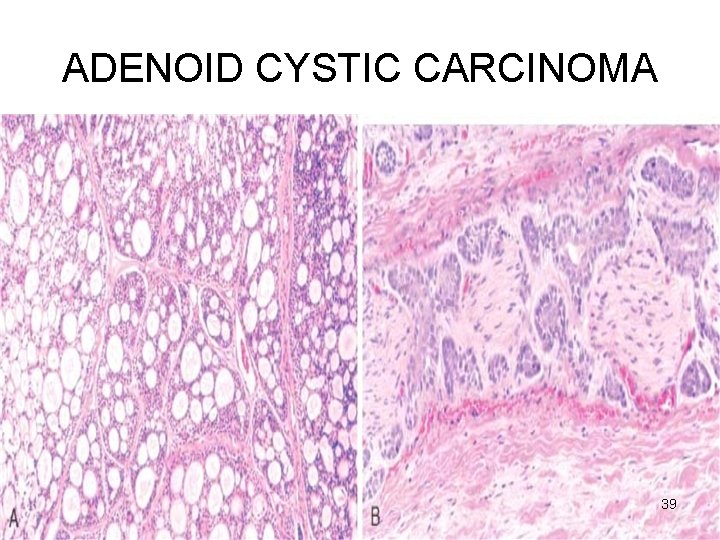
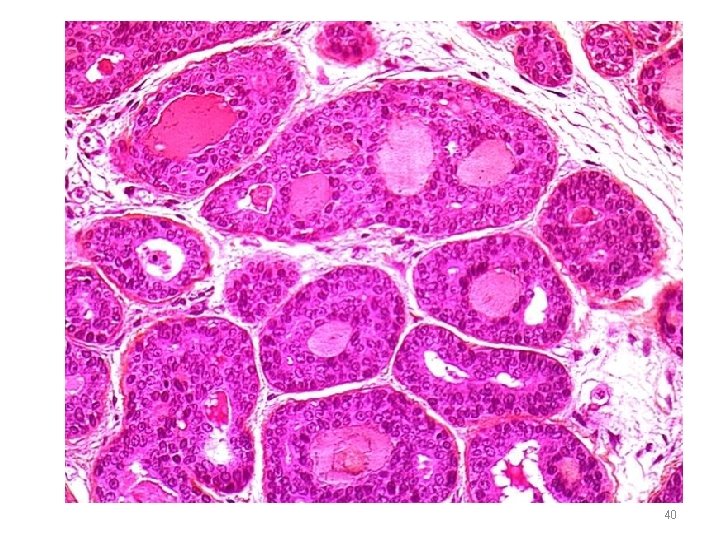
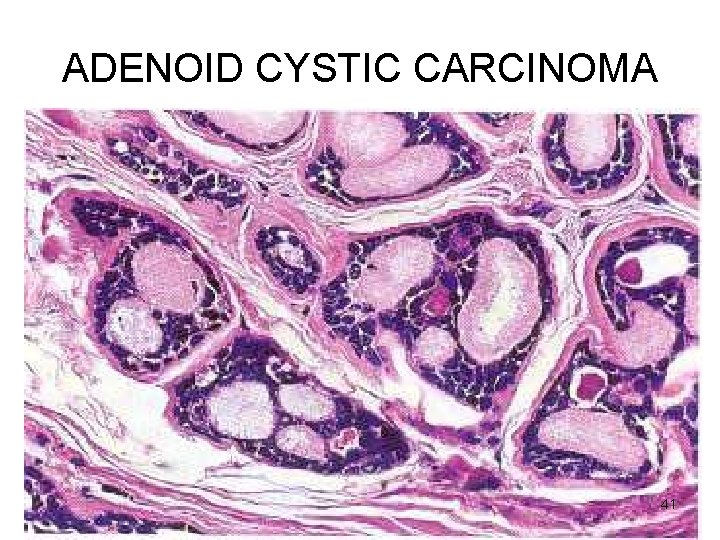
ADENOID CYSTIC CARCINOMA Microscopy • Small cells with dark compact nuclei, scanty cytoplasm • Arranged in tubules, solid, cribriform • SPACES BETWEEN CELLS FILLED WITH HYALINE MATERIAL – basement membrane material • Perineural invasion - pain 38
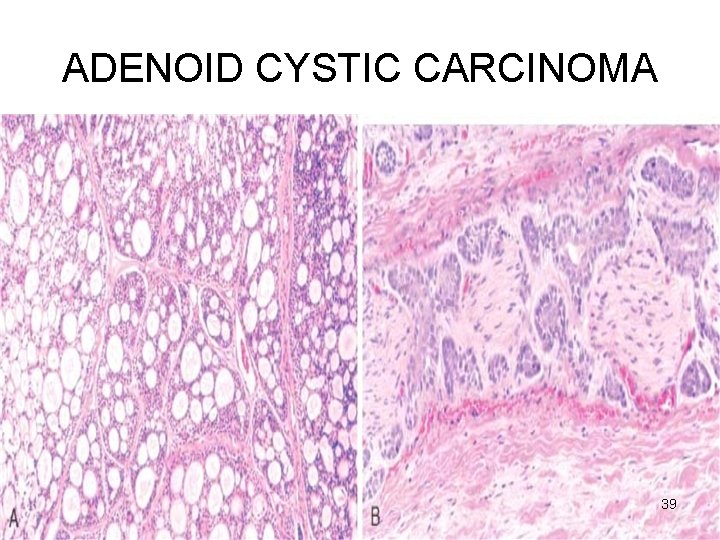
ADENOID CYSTIC CARCINOMA 39
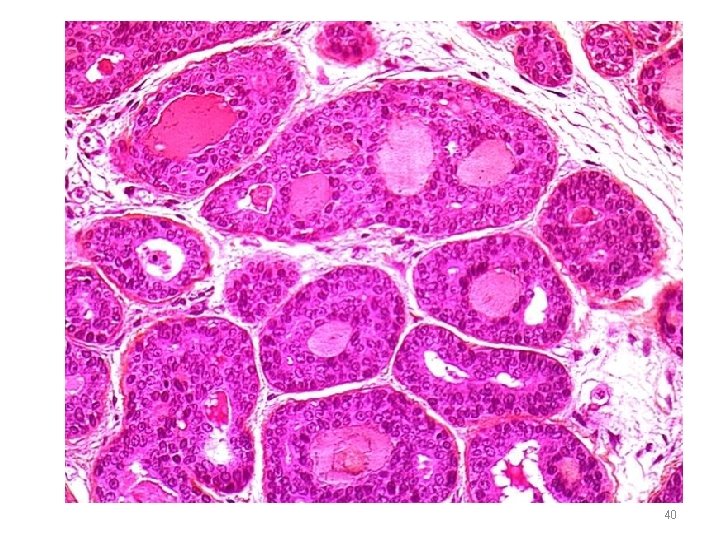
40
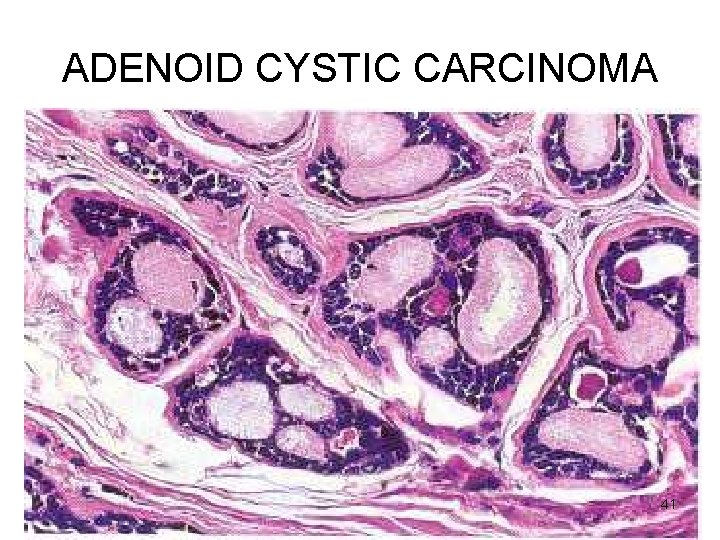
ADENOID CYSTIC CARCINOMA 41
ADENOID CYSTIC CARCINOMA CLINICAL ASPECTS • • Malignant Slow growing Stubbornly recurrent Painful – perineural invasion 42
Acinic cell carcinoma (tumour) • Most PAROTID – composed of serous cells 43
Acinic cell carcinoma Gross • Small • Encapsulated 44
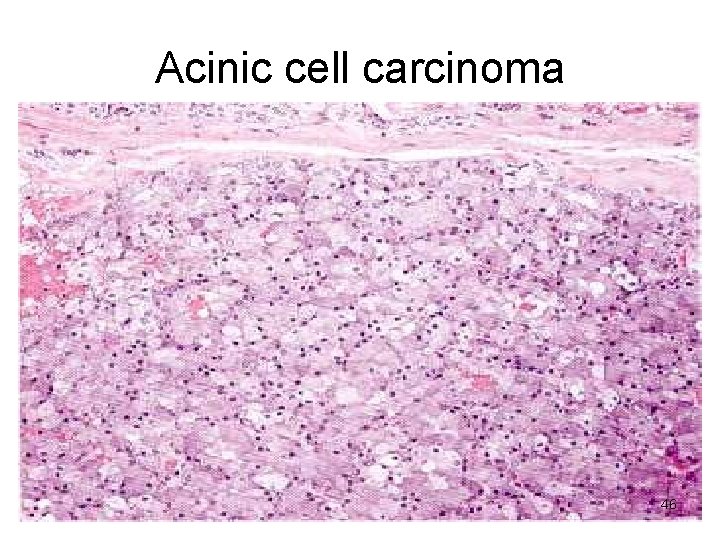
Acinic cell carcinoma Microscopy • Look like serous cells • Clear cytoplasm • Solid sheets, microcystic, glandular, follicular, papillary • Little anaplasia 45
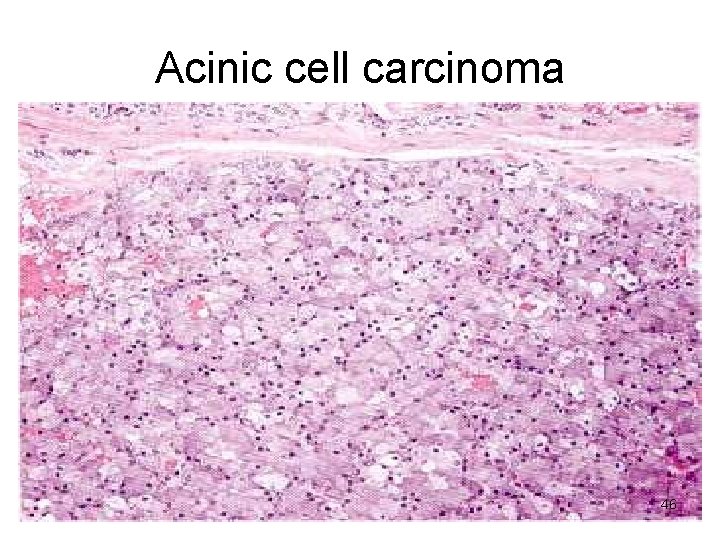
Acinic cell carcinoma 46
Acinic cell carcinoma CLINICAL ASPECTS • Good prognosis • Recurrence rare 47
 Ts of liver
Ts of liver Intercalated duct histology
Intercalated duct histology Youtube
Youtube Submandibular gland excision
Submandibular gland excision Dysphagia terminology
Dysphagia terminology Salivary gland swelling
Salivary gland swelling Function of salivary glands
Function of salivary glands Sialography
Sialography Sialography
Sialography Phadebas paper
Phadebas paper Weber salivary gland
Weber salivary gland Colon
Colon Minor salivary glands
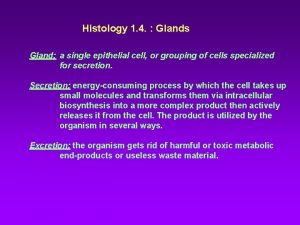
Minor salivary glands Modes of glandular secretion
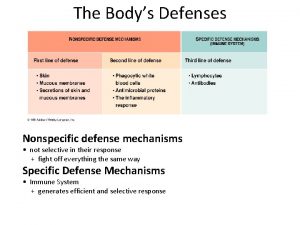
Modes of glandular secretion Specific vs nonspecific defense
Specific vs nonspecific defense романенко
романенко Th and tc cells
Th and tc cells V/q scan pulmonary embolism
V/q scan pulmonary embolism J point
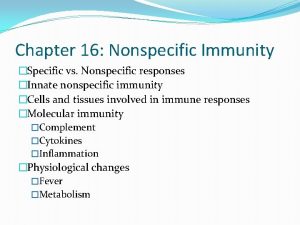
J point Nonspecific vs specific immunity
Nonspecific vs specific immunity Nonspecific host defense mechanism
Nonspecific host defense mechanism Salivary amylase digestion of starch
Salivary amylase digestion of starch Mucous acini
Mucous acini Pleomorphic adenoma
Pleomorphic adenoma Warthin's tumor
Warthin's tumor Function of bile
Function of bile Fosdick calcium dissolution test
Fosdick calcium dissolution test Oncocytoma salivary gland
Oncocytoma salivary gland Cylindroma slideshare
Cylindroma slideshare Salivary gland
Salivary gland Salivary gland tumor
Salivary gland tumor Lactobacillus count test
Lactobacillus count test Oncocytoma salivary gland
Oncocytoma salivary gland Oncocytoma salivary gland
Oncocytoma salivary gland Salivary gland pathology
Salivary gland pathology Simple branched alveolar gland
Simple branched alveolar gland Salivary gland disorders classification
Salivary gland disorders classification Oxyntic glands
Oxyntic glands Major endocrine glands male and female
Major endocrine glands male and female What glands are flask shaped with short ducts
What glands are flask shaped with short ducts Layer of dermis
Layer of dermis Multicellular exocrine glands can be classified
Multicellular exocrine glands can be classified The only example of unicellular exocrine glands are
The only example of unicellular exocrine glands are Pineal and pancreas glands
Pineal and pancreas glands Gonads glands
Gonads glands Serous vs mucous
Serous vs mucous Coiled gland
Coiled gland Adrenal glands
Adrenal glands