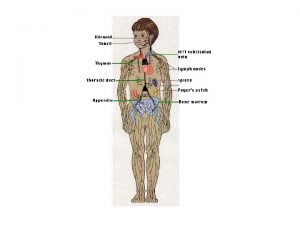
DISEASES OF SMALL AND LARGE INTESTINE Diseases of






- Slides: 39

DISEASES OF SMALL AND LARGE INTESTINE
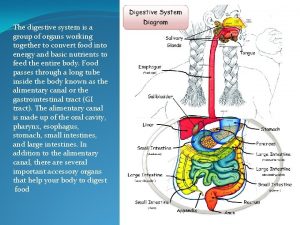
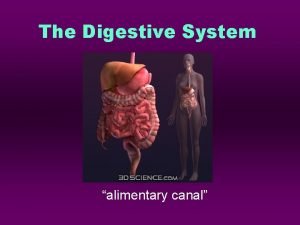
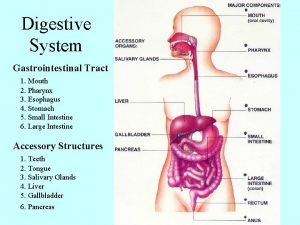
Diseases of small and large intestine � Disease of bowel caused by: � � � Developmental anomalies (Hirschsprung Disease) Vascular Disorders Diarrheal diseases Idiopathic inflammatory bowel disease Tumors Others.
Developmental anomalies Meckel diverticulum � � � is the most common and innocuous of the anomalies. It results from failure of involution of the omphalomesenteric duct, leaving a persistent blindended tubular protrusion as long as 5 to 6 cm in the ileum, about 80 cm proximal to the ileocecal valve Peptic ulceration in the adjacent intestinal mucosa

Developmental anomalies (Hirschsprung Disease) � � during development, the migration of neural crestderived cells along the alimentary tract arrests at some point before reaching the anus. an aganglionic segment is formed that lacks both the Meissner submucosal and Auerbach myenteric plexuses. This causes functional obstruction and progressive distention of the colon proximal to the affected segment. Ganglia are absent from the muscle wall and submucosa of the constricted segment but may be present in the dilated portion.
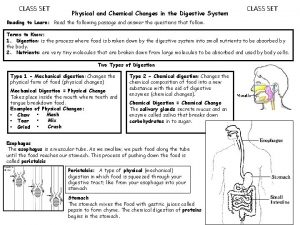
Diarrheal diseases including l. Acute inflammation caused by infectious organism l. Malabsorption l. Idiopathic disorder. inflammatory bowel disease. Symptoms: diarrhea, dysentery and pain.
Diarrheal diseases � � � Diarrhea consists of daily stool production in excess of 250 g, containing 70% to 90% water. Often accompanied by pain, discomfort, urgency and incontinence. Dysentery is low volume painful, bloody diarrhea
Principal mechanisms of diarrhea Secretory: • • Osmotic: • • excessive osmotic forces as Lactulose therapy and antiacids Exudative: • • output of purulent, bloody stool, occur in infectious conditions and Idiopathic inflammatory bowel disease Malabsorption: • • • isotonic to plasma, occur in infectious conditions, neoplastic conditions and in excessive laxatives used voluminous stool, occur in defective absorption and intraluminal digestion or lymphatic obstruction Deranged motility
Infectious Enterocolitis � � A global problem, 2. 9 million death per year Account for 1/2 of death in children younger than 5 years in some countries In USA, about 500 infants and young children die each year because of diarrheal disease Most common problem in traveler
Infectious Enterocolitis � � Direct invasion of microbe with ulceration. Production of enterotoxin. Ability to adhere to mucosal lining. Major causative agents: bacteria (E. coli), virus (calcivirus, rotavirus and Norwalk virus), fungus and protozoa.
Infectious Enterocolitis Viral gastroenterocolitis � � � Viral infection destroy superficial epithelium in small intestine & their absorptive function Repair by immature enterocytes with secretory function Rotavirus: 130 million cases per year and 0. 9 million deaths worldwide per year, mainly children (6 -24 month)
Viral gastroenterocolitis � � � Rotavirus is the most common agent (140 million cases and 1 million death 1 year). Affect children 6 -24 months. Incubation period is 2 days followed by vomiting and watery diarrhea. Affect epithelium of the small intestine leading to secretion of water and electrolytes May produce a flat mucosa in small intestine. Rotavirus have intrinsic viral factor, nonstuctural protein 4 (NSP 4) that induce direct diarrhea

Viral gastroenterocolitis � � Caliciviruses most common virus of nonbacterial foodborne epidemic in older children and adult. Adenovirus and astrovirus
Infectious Enterocolitis Bacterial enterocolitis � � Caused by a variety of bacterial species e. g. E. coli, salmonella, shigella, campylobacter, vibrio cholerae and others. Pathogenic mechanism: 1. Ingestion of preformed toxin e. g. C. botulism and S. aureus. 2. Infection by toxigenic organisms, e. g. E. coli, V. cholerae. 3. Infection by enteroinvasive organism e. g. salmonella, shigella or E. coli.
Infectious Enterocolitis Bacterial enterocolitis � In enteroinvasive organism and toxigenic organisms bacterial replication occur � This depend on: The ability to adhere to mucosa ( adhesins ) � The ability to elaborate toxins � The capacity to invade �
Bacterial Enterocolitis Morphology � Pathologic manifestations are variable – normal (v. cholerae) to non specific inflammation and severe ulceration � E. coli - different subtypes Entertoxigenic The Shiga toxin - producing strain Enteropathogenic strains Enteroinvasive strains Enteroaggregating strains Shigella – distal colon, acute mucosal inflammation and erosion. � C. Jejuni – small and large intestine; villus blunting, ulceration. �
Bacterial Enterocolitis � Y enterocolitis – ileum, appendix and colon; hemorrhage. and necrosis, invade Peyer patches and lymph node leading to necrotizing granulomas � Salmonella – ileum and colon; invade Peyer patches and produce linear ulceration, serosa may be normal or covered by serous, fibrinous or hemorrhagic exudate, regional lymph node may be enlarged, systemic infection (Typhoid fever) � Mycobacterium tuberculosis

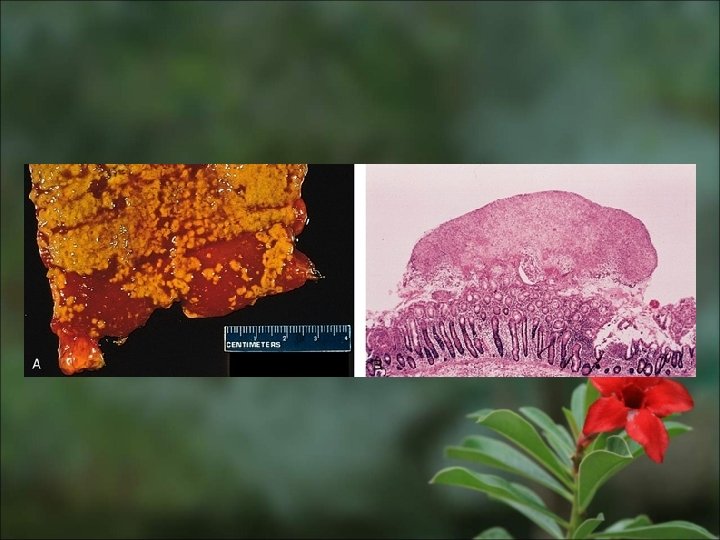
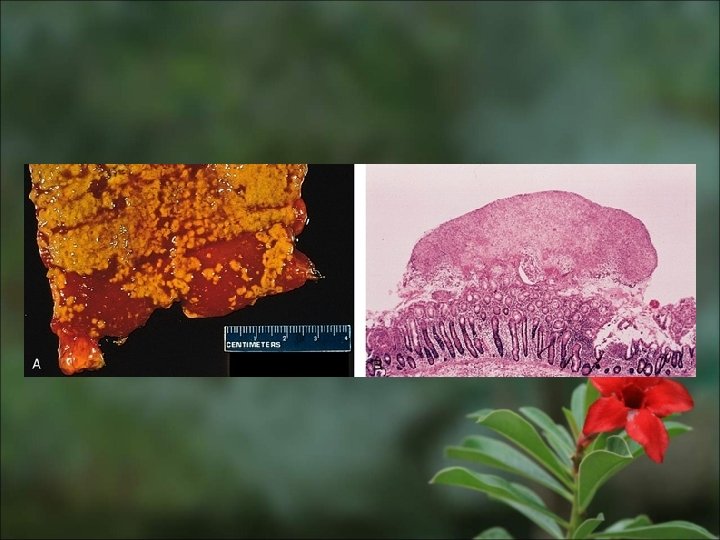
Antibiotic Associated Colitis (Pseudomembranous colitis) � � Acute colitis with formation of adherent inflammtory exudate. Caused by C. difficile (produce two protein exotoxins A & B). Occur after a coarse of broad spectrum antibiotic. Can occur after severe necrotizing enterocolitis or in ischemic colitis.
Bacterial Enterocolitis Clinical manifestation � � � Ingestion of preformed toxin: diarrhea, acute abdominal pain. Infection with enteric pathogens: - Secretory enterotoxin: diarrhea - Cytotoxin or enteroinvasive process: dysentery. Insidious infection: Yersenia and TB – subacute diarrheal illness.
Protozoal Infection Amebiasis � � � Entamoeba histiolytica is a common pathogen of colon. Ingestion of cysts in the contaminated food and water. Cysts release active amebas (trophozoites), invade large bowel mucosa and enter the submucosa (site of maximum involvement), enzymatic necrosis (flask-shaped ulcer).
Amebiasis n. Gross: multiple ulcers separated by healthyappearing mucosa, undermined by submucosal abscesses. n. Micro: mucosal ulcers covered by a necrotic base. Amebas are found in the wall of the ulcer. n. Complication: perforation, haemorrhage, toxic megacolon, amebic abscess.
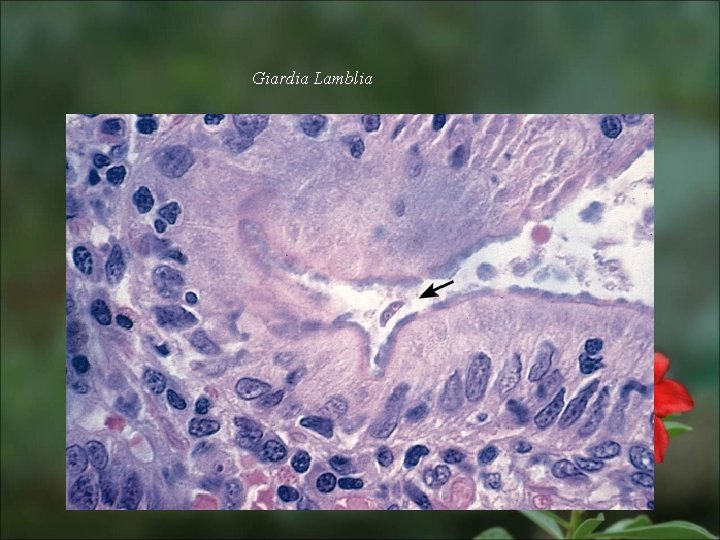
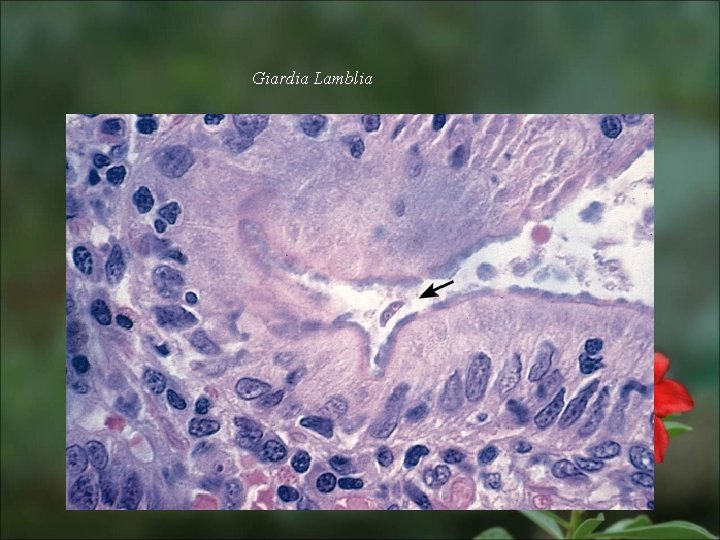
Giardia Lamblia

Malabsorption Syndrome
Malabsorption Syndrome � � There is increased fecal excretion of fat (steatorrhea) and the systemic effects of deficiency of vitamins, minerals, protein and carbohydrates. Steatorrhea is passage of soft, yellowish, greasy stools containing an increased amount of fat. Fat excretion exceeding 6 g/d is demonstrated in a 72 -hour stool sample. Disturbance of normal digestive function.
Mechanism of Malabsorption � It result from disturbance of one of these normal digestive functions � Intraluminal digestion � Terminal digestion � Transepithelial transport
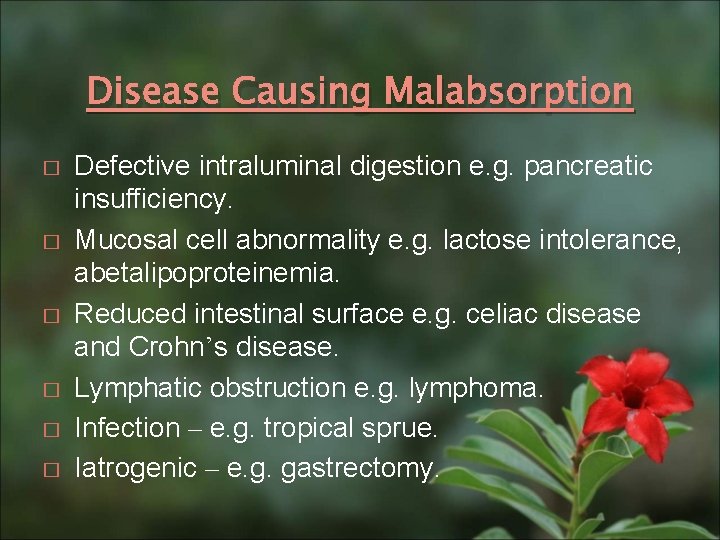
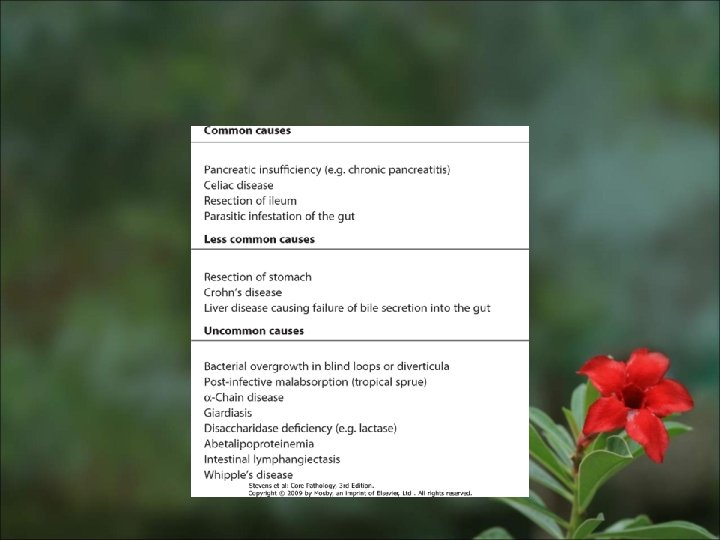
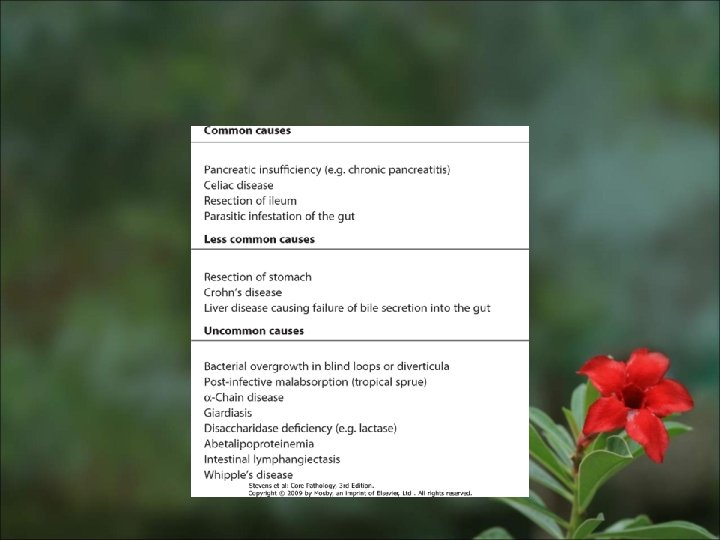
Disease Causing Malabsorption � � � Defective intraluminal digestion e. g. pancreatic insufficiency. Mucosal cell abnormality e. g. lactose intolerance, abetalipoproteinemia. Reduced intestinal surface e. g. celiac disease and Crohn’s disease. Lymphatic obstruction e. g. lymphoma. Infection – e. g. tropical sprue. Iatrogenic – e. g. gastrectomy.
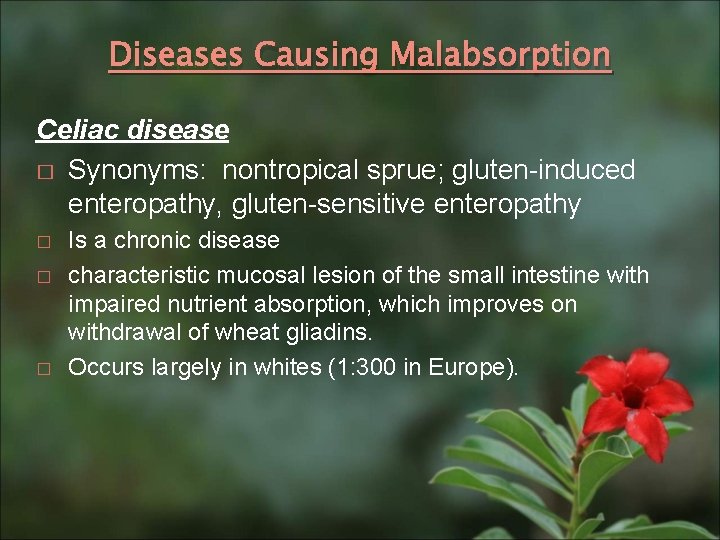
Diseases Causing Malabsorption Celiac disease � Synonyms: nontropical sprue; gluten-induced enteropathy, gluten-sensitive enteropathy � � � Is a chronic disease characteristic mucosal lesion of the small intestine with impaired nutrient absorption, which improves on withdrawal of wheat gliadins. Occurs largely in whites (1: 300 in Europe).
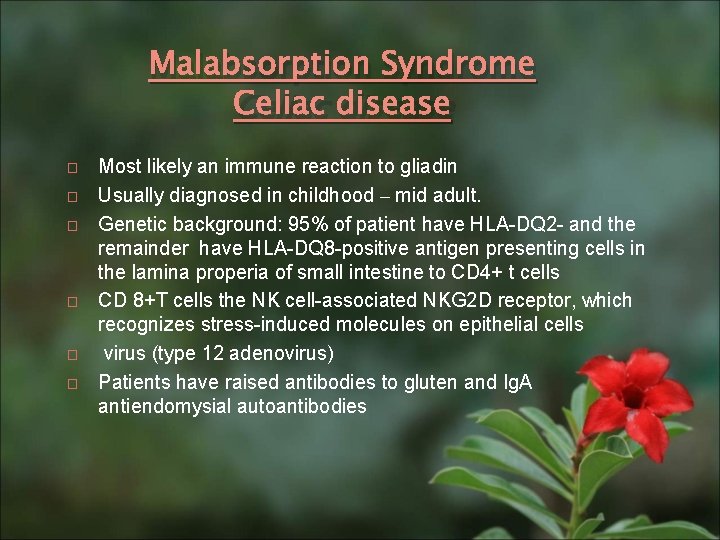
Malabsorption Syndrome Celiac disease � � � Most likely an immune reaction to gliadin Usually diagnosed in childhood – mid adult. Genetic background: 95% of patient have HLA-DQ 2 - and the remainder have HLA-DQ 8 -positive antigen presenting cells in the lamina properia of small intestine to CD 4+ t cells CD 8+T cells the NK cell-associated NKG 2 D receptor, which recognizes stress-induced molecules on epithelial cells virus (type 12 adenovirus) Patients have raised antibodies to gluten and Ig. A antiendomysial autoantibodies
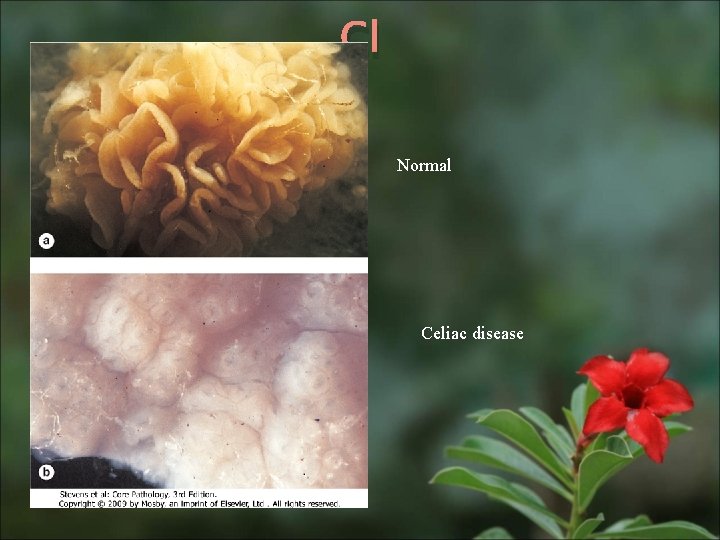
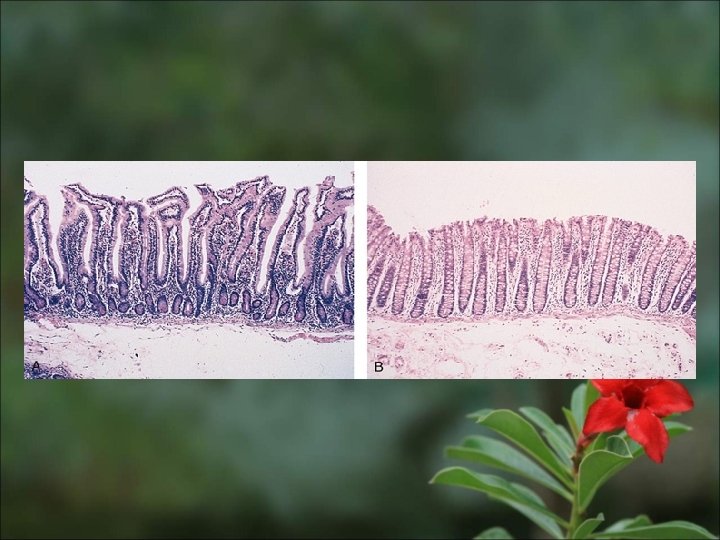
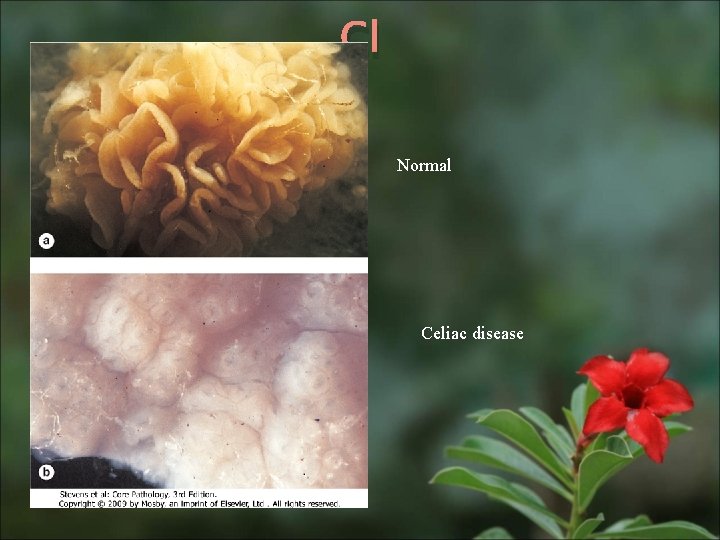
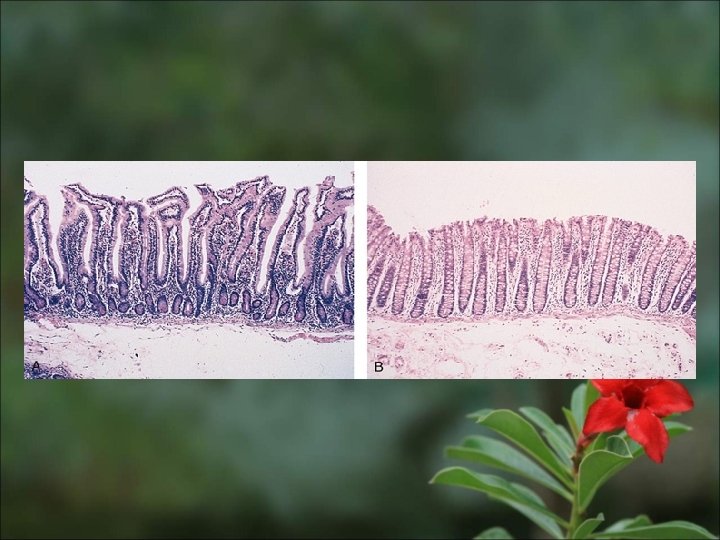
Cl Normal Celiac disease
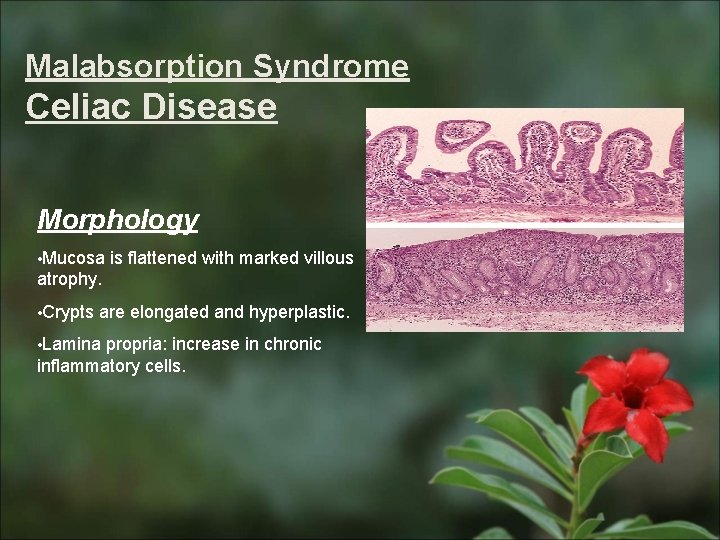
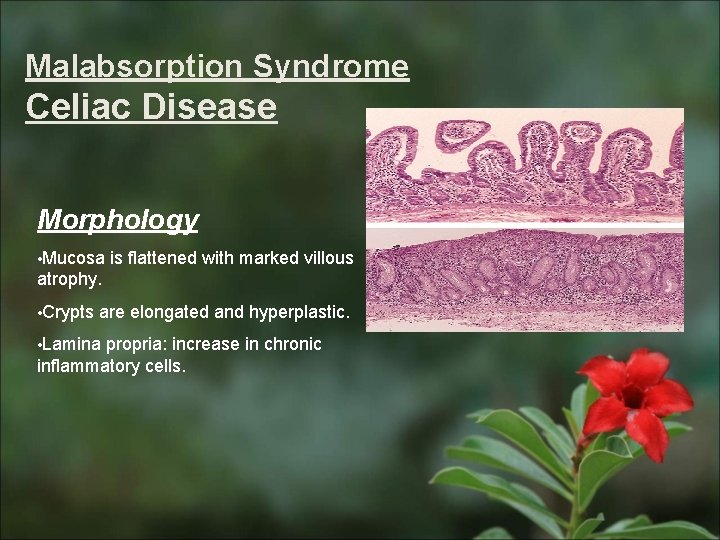
Malabsorption Syndrome Celiac Disease Morphology • Mucosa is flattened with marked villous atrophy. • Crypts are elongated and hyperplastic. • Lamina propria: increase in chronic inflammatory cells.
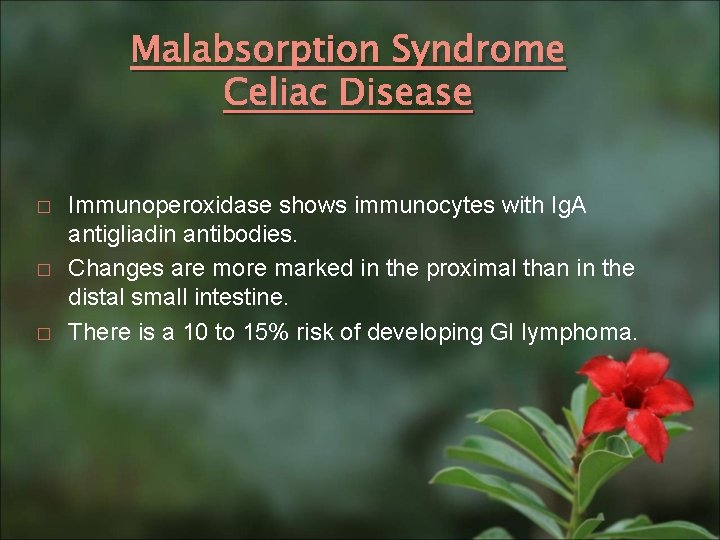
Malabsorption Syndrome Celiac Disease � � � Immunoperoxidase shows immunocytes with Ig. A antigliadin antibodies. Changes are more marked in the proximal than in the distal small intestine. There is a 10 to 15% risk of developing GI lymphoma.
Malabsorption Syndrome Celiac Disease Clinical features Infants : Adults : Failure to thrive, diarrhea. Diarrhea, flatulence, weight loss and fatigue.
Malabsorption Syndrome Celiac Disease Diagnosis 1. Clinical documentations of malabsorption. 2. Small intestine biopsy demonstrate intestinal lesion. 3. Improvement of symptom and mucosal histology on gluten withdrawal from diet. 4. Challenge test.
Malabsorption Syndrome Tropical Sprue (post-infectious sprue) � Occurs in people living in or visiting tropical or semitropical locales. � Of unknown etiology, perhaps enterotoxigenic E. coli or haemophilus. � Most patients improve or are cured with long-term broad spectrum antibiotic therapy.
Malabsorption Syndrome Tropical Sprue (post-infectious sprue) Morphology � Variable ranging from normal to those of celiac disease. � Unlike celiac disease, injury of small intestine occur at all levels. � Deficiency of folic acid and vit. B 12 – megaloblastic changes.

Malabsorption Syndrome Clinical features Malabosortion affect many organs � Hematopiotic system, anemia and bleeding � Musculoskeletal system, osteopenia and tetany � Endocrine system, amenorrhea, infertility, hyperparathyridism � Skin, purpura dermatitis hyperkeratosis � Nervous system, neuropathy
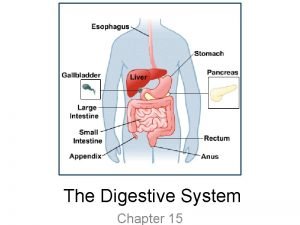
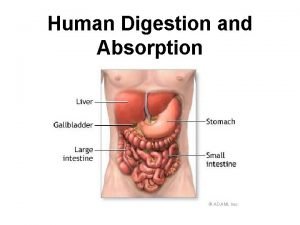
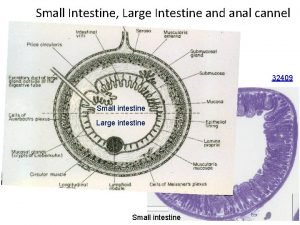
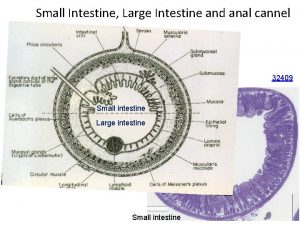
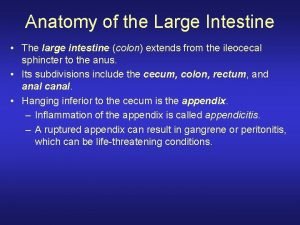
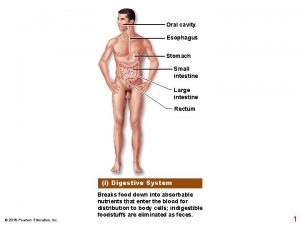
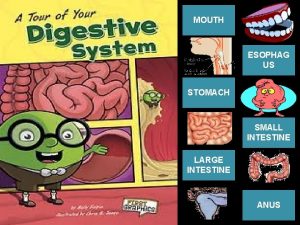
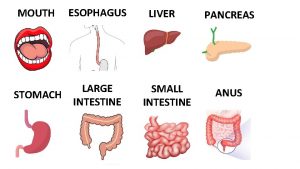
 Esophagus stomach small intestine large intestine
Esophagus stomach small intestine large intestine Main functions of small intestine
Main functions of small intestine Large intestine labeled
Large intestine labeled Function of digestive tract
Function of digestive tract Diareherra
Diareherra Lymphoid tissue in large intestine
Lymphoid tissue in large intestine Regions of large intestine
Regions of large intestine Large intestine relations
Large intestine relations Labelled diagram of a tooth
Labelled diagram of a tooth Functions of the large intestine
Functions of the large intestine Plica ileocolica
Plica ileocolica Colon gross anatomy
Colon gross anatomy Copyright
Copyright Colon histology
Colon histology Strongylus vulgaris
Strongylus vulgaris Large intestine function in digestive system
Large intestine function in digestive system The main jobs of the large intestine are _____.
The main jobs of the large intestine are _____. Part of large intestine
Part of large intestine Large intestine function in digestive system
Large intestine function in digestive system Dr malak
Dr malak Mash, grind, mix and tear food.
Mash, grind, mix and tear food. Sigmoid colon peritoneum
Sigmoid colon peritoneum Brush border enzyme
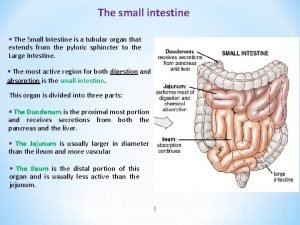
Brush border enzyme The small intestine extends from the
The small intestine extends from the Small intestine gangrene
Small intestine gangrene Left colic flexure
Left colic flexure Digestion begins in the when you chew and swallow
Digestion begins in the when you chew and swallow 13.2 structures of the digestive system
13.2 structures of the digestive system Is the small intestine a physical or chemical change
Is the small intestine a physical or chemical change Blood supply small bowel
Blood supply small bowel Small intestine relations
Small intestine relations Yellowish structures that serve as an energy reserve frog
Yellowish structures that serve as an energy reserve frog The combining form celi/o means:
The combining form celi/o means: What is the function of the small intestine?
What is the function of the small intestine? Small intestine
Small intestine Galt
Galt Parts of small intestine
Parts of small intestine Small intestine villi function
Small intestine villi function Small intestine peristalsis
Small intestine peristalsis Plica circularis
Plica circularis