Discharge Planning and Transition to Home Sarah Sexton




- Slides: 13
Discharge Planning and Transition to Home Sarah Sexton Walters, APRN and Frank Virgin, MD Pediatric Otolaryngology Monroe Carell Jr. Children’s Hospital at Vanderbilt.

Disclosures • I have no disclosures
Background • Length of Stay • Consistency and Assessment of Education • Early Readmissions
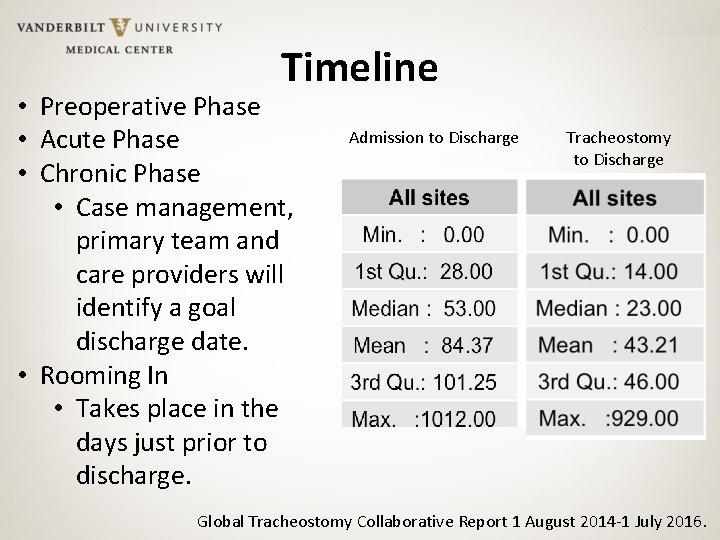
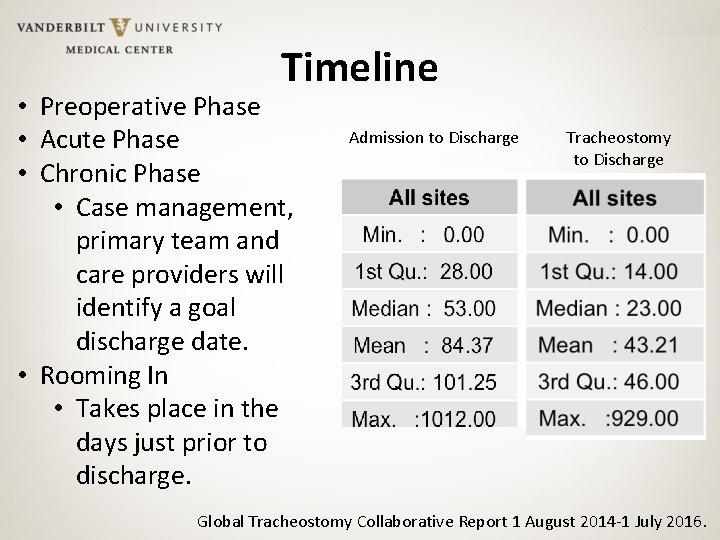
Timeline • Preoperative Phase • Acute Phase • Chronic Phase • Case management, primary team and care providers will identify a goal discharge date. • Rooming In • Takes place in the days just prior to discharge. Admission to Discharge Tracheostomy to Discharge Global Tracheostomy Collaborative Report 1 August 2014 -1 July 2016.
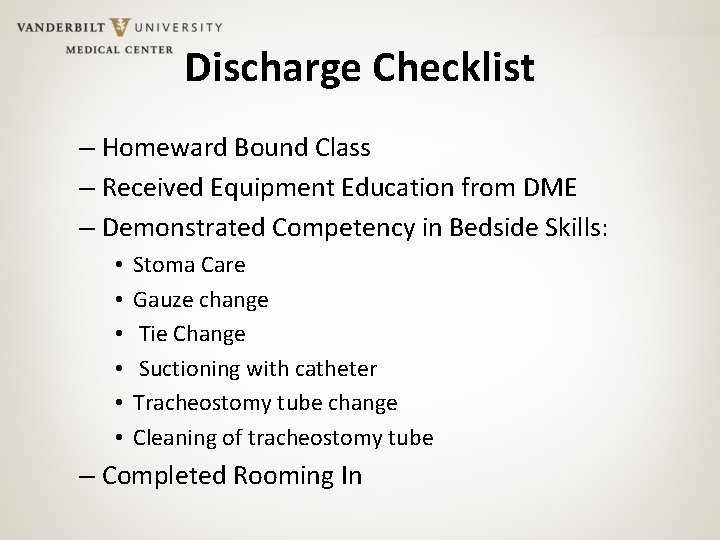
Discharge Checklist – Homeward Bound Class – Received Equipment Education from DME – Demonstrated Competency in Bedside Skills: • • • Stoma Care Gauze change Tie Change Suctioning with catheter Tracheostomy tube change Cleaning of tracheostomy tube – Completed Rooming In
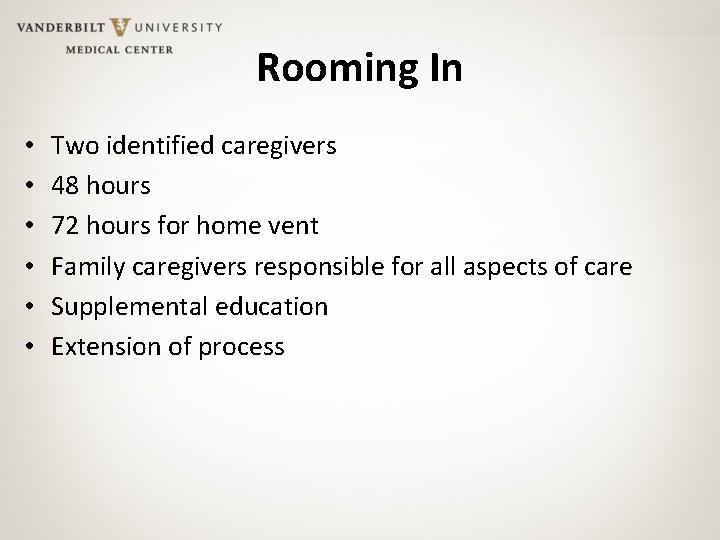
Rooming In • • • Two identified caregivers 48 hours 72 hours for home vent Family caregivers responsible for all aspects of care Supplemental education Extension of process

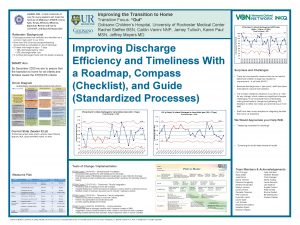
Readmissions • Trends of readmissions within 48 hours of discharge • Identified risk factors for readmission – DCS involvement – Home Ventilator – No Home Health • Preventable causes – Equipment malfunction – Intolerance to home equipment – Lack of family understanding on how to use home equipment – Home health staffing
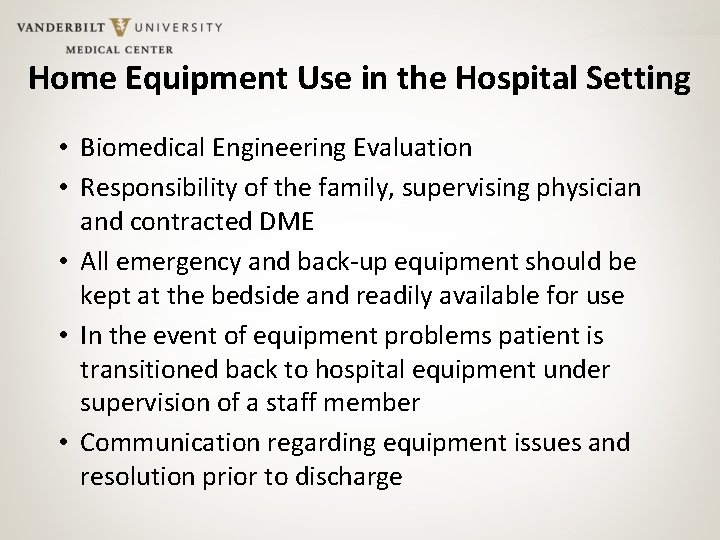
Home Equipment Use in the Hospital Setting • Biomedical Engineering Evaluation • Responsibility of the family, supervising physician and contracted DME • All emergency and back-up equipment should be kept at the bedside and readily available for use • In the event of equipment problems patient is transitioned back to hospital equipment under supervision of a staff member • Communication regarding equipment issues and resolution prior to discharge
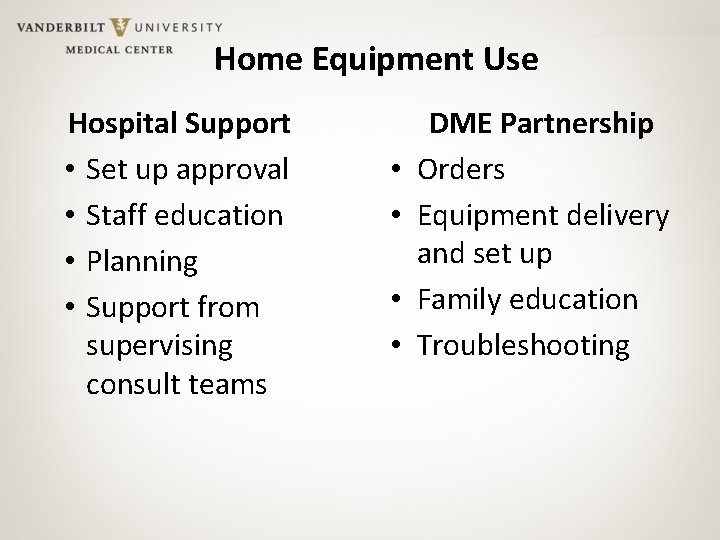
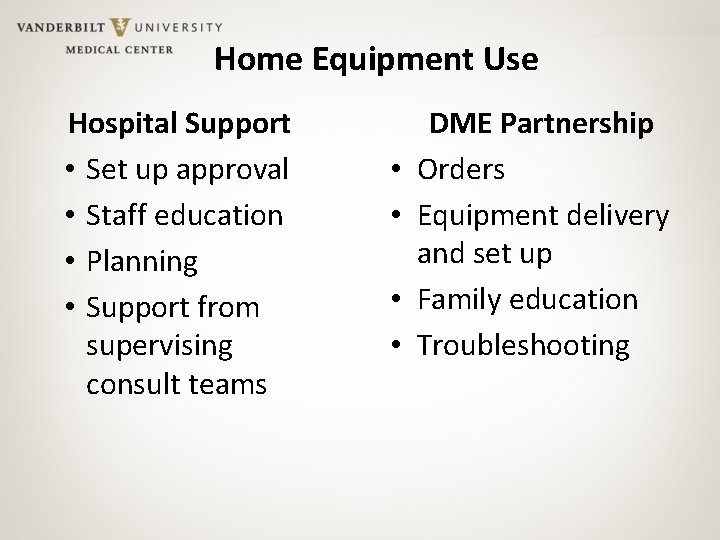
Home Equipment Use Hospital Support • Set up approval • Staff education • Planning • Support from supervising consult teams • • DME Partnership Orders Equipment delivery and set up Family education Troubleshooting
Home Health • Private Duty Nursing – Limited training – Scope of practice restrictions for LPNs – Staffing availability • Respiratory Care – Lack of pediatric-trained therapists

Special Considerations • Physical Rehabilitation – Identify timeline goals for follow up – DME Orders • DCS/ Foster Care – Caregiver training – Length of stay • Complex Care – Follow up
Follow Up • PCP follow up within 1 week • Clinic follow up scheduled within 1 month of discharge • Specialty care/ CADET

Contact Info sarah. l. sexton@vanderbilt. edu
 Paul sexton wholesale cars
Paul sexton wholesale cars Jill sexton
Jill sexton Briar sexton
Briar sexton Aerosol overcaps
Aerosol overcaps Whitney sexton
Whitney sexton Dan sexton civil service
Dan sexton civil service Rhonda sexton
Rhonda sexton Sexton engineering
Sexton engineering Mental health discharge planning checklist
Mental health discharge planning checklist Mental health discharge planning checklist
Mental health discharge planning checklist Arti dari home care
Arti dari home care Perbedaan home care dan home visit
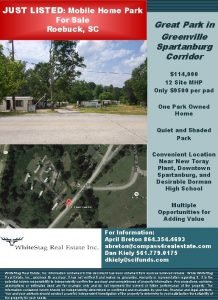
Perbedaan home care dan home visit South carolina mobile home parks for sale
South carolina mobile home parks for sale Plurals of flower
Plurals of flower