Digestive System Part 3 Honors Anatomy Physiology Chapter
- Slides: 33
Digestive System Part 3 Honors Anatomy & Physiology Chapter 23
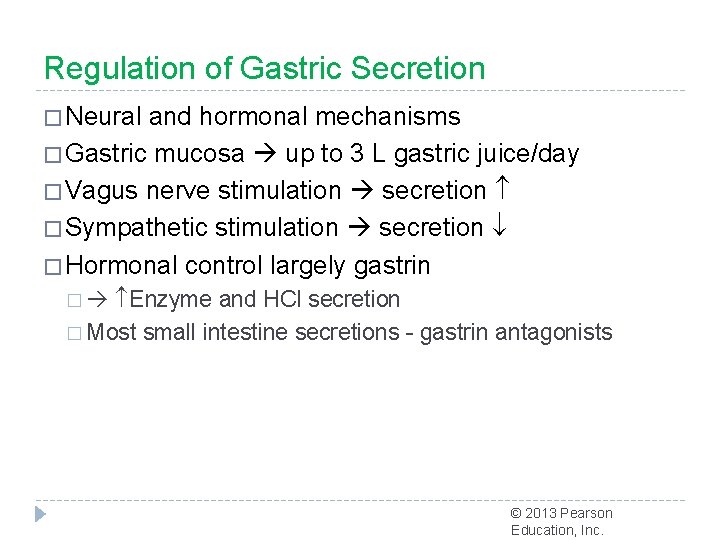
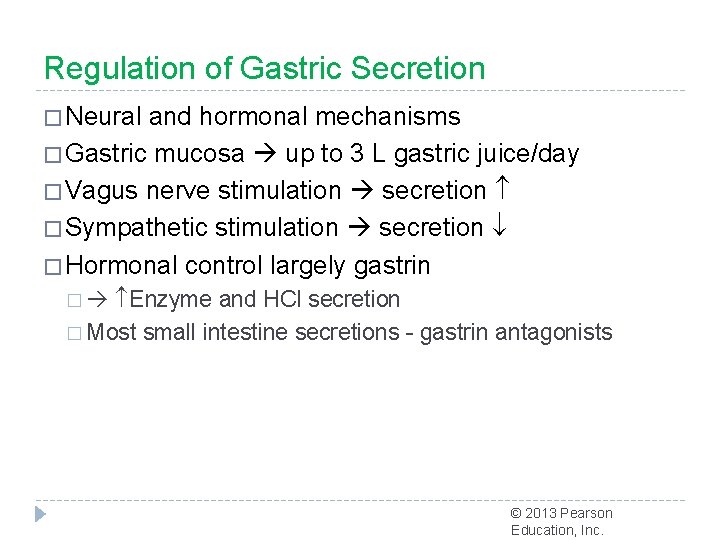
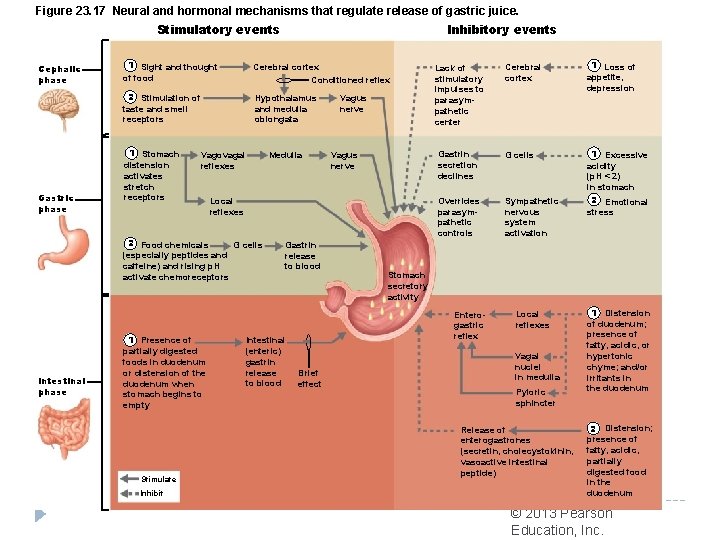
Regulation of Gastric Secretion � Neural and hormonal mechanisms � Gastric mucosa up to 3 L gastric juice/day � Vagus nerve stimulation secretion � Sympathetic stimulation secretion � Hormonal control largely gastrin � Enzyme and HCl secretion � Most small intestine secretions - gastrin antagonists © 2013 Pearson Education, Inc.
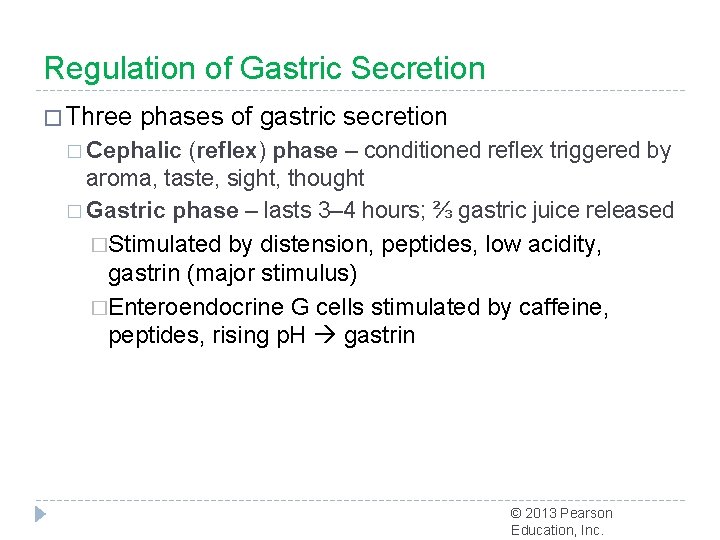
Regulation of Gastric Secretion � Three phases of gastric secretion � Cephalic (reflex) phase – conditioned reflex triggered by aroma, taste, sight, thought � Gastric phase – lasts 3– 4 hours; ⅔ gastric juice released �Stimulated by distension, peptides, low acidity, gastrin (major stimulus) �Enteroendocrine G cells stimulated by caffeine, peptides, rising p. H gastrin © 2013 Pearson Education, Inc.
Stimuli of Gastric Phase �Gastrin enzyme and HCl release � Low p. H inhibits gastrin secretion (as between meals) �Buffering action of ingested proteins rising p. H gastrin secretion �Three chemicals - ACh, histamine, and gastrin - stimulate parietal cells through secondmessenger systems � All three are necessary for maximum HCl secretion © 2013 Pearson Education, Inc.
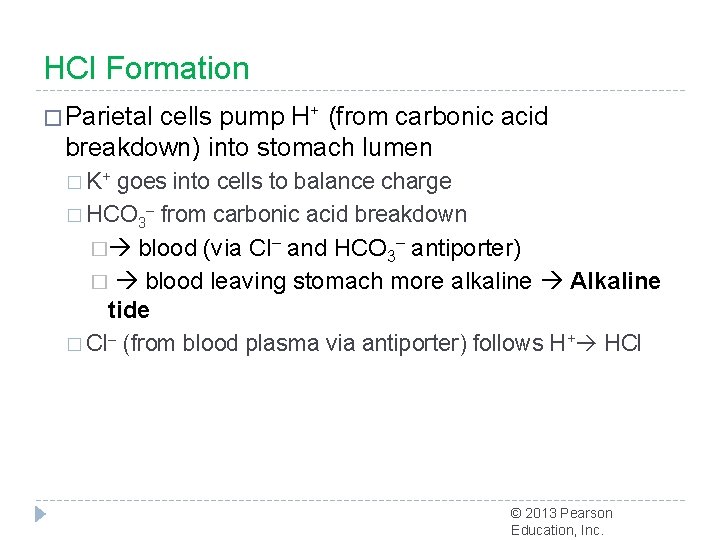
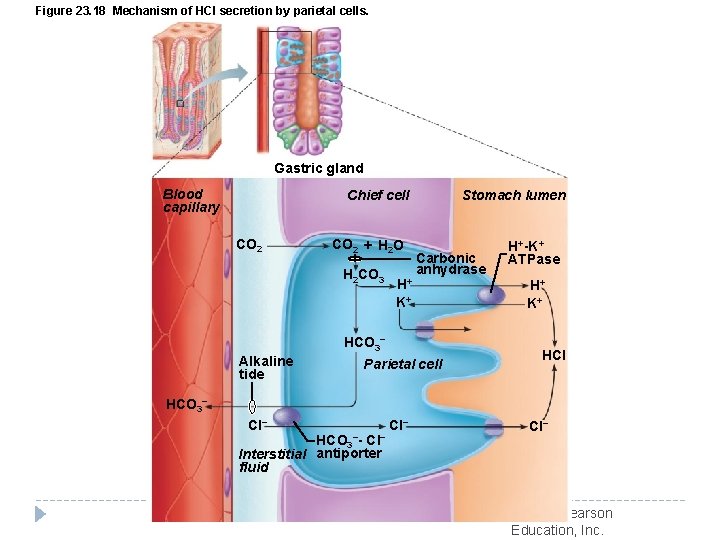
HCl Formation � Parietal cells pump H+ (from carbonic acid breakdown) into stomach lumen � K+ goes into cells to balance charge � HCO 3– from carbonic acid breakdown � blood (via Cl– and HCO 3– antiporter) � blood leaving stomach more alkaline Alkaline tide � Cl– (from blood plasma via antiporter) follows H+ HCl © 2013 Pearson Education, Inc.
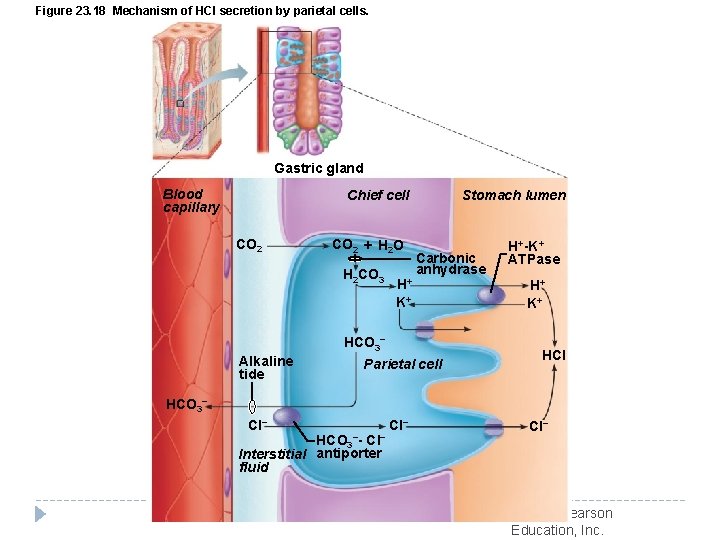
Figure 23. 18 Mechanism of HCl secretion by parietal cells. Gastric gland Blood capillary Chief cell CO 2 + H 2 O H 2 CO 3 H+ K+ Stomach lumen Carbonic anhydrase HCO 3− Alkaline tide Parietal cell H+-K+ ATPase H+ K+ HCI HCO 3− Cl− HCO 3−- Cl− Interstitial antiporter fluid Cl− © 2013 Pearson Education, Inc.
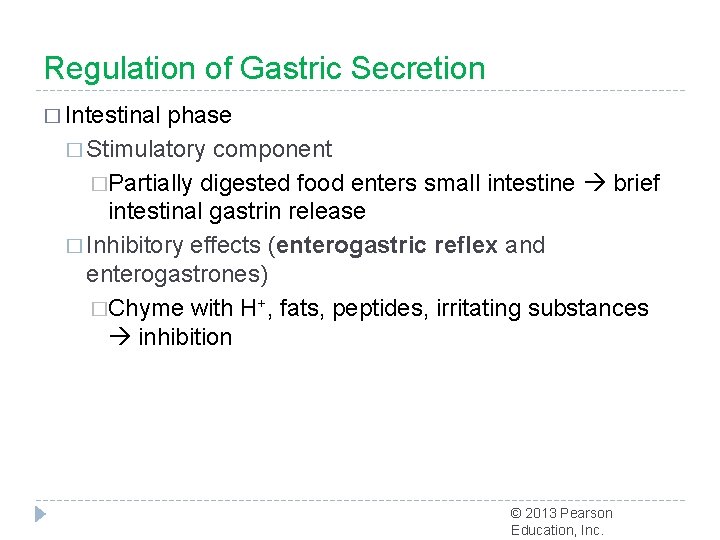
Regulation of Gastric Secretion � Intestinal phase � Stimulatory component �Partially digested food enters small intestine brief intestinal gastrin release � Inhibitory effects (enterogastric reflex and enterogastrones) �Chyme with H+, fats, peptides, irritating substances inhibition © 2013 Pearson Education, Inc.
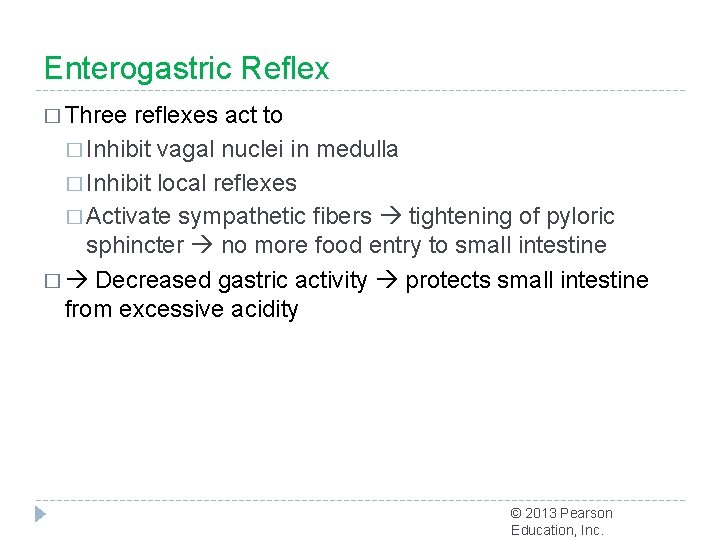
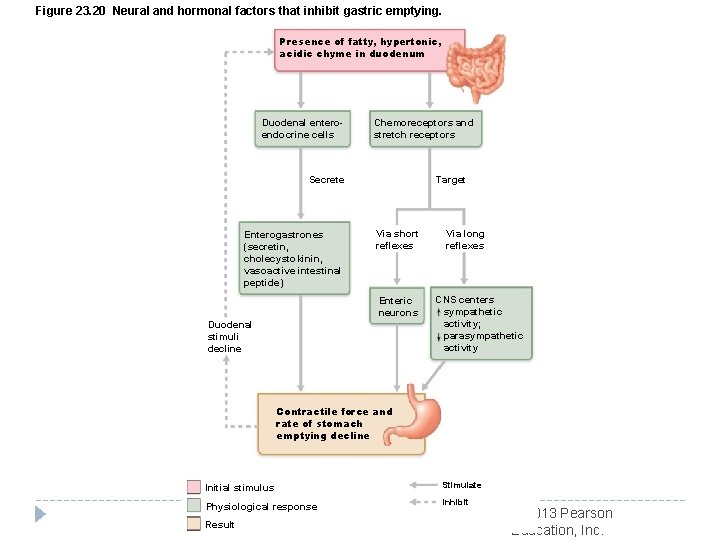
Enterogastric Reflex � Three reflexes act to � Inhibit vagal nuclei in medulla � Inhibit local reflexes � Activate sympathetic fibers tightening of pyloric sphincter no more food entry to small intestine � Decreased gastric activity protects small intestine from excessive acidity © 2013 Pearson Education, Inc.
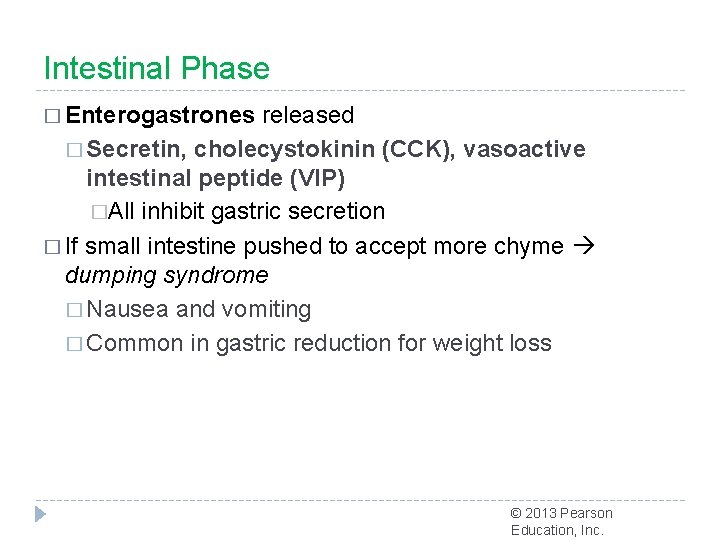
Intestinal Phase � Enterogastrones released � Secretin, cholecystokinin (CCK), vasoactive intestinal peptide (VIP) �All inhibit gastric secretion � If small intestine pushed to accept more chyme dumping syndrome � Nausea and vomiting � Common in gastric reduction for weight loss © 2013 Pearson Education, Inc.
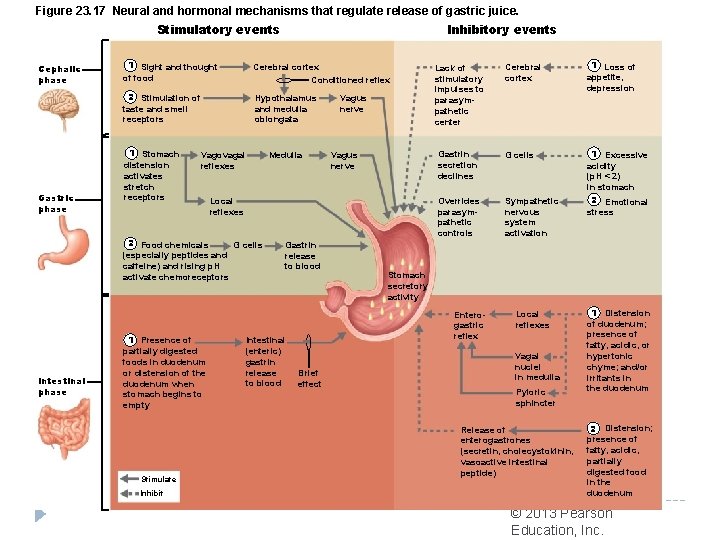
Figure 23. 17 Neural and hormonal mechanisms that regulate release of gastric juice. Inhibitory events Stimulatory events Cephalic phase Gastric phase 1 Sight and thought of food Cerebral cortex Conditioned reflex 2 Stimulation of taste and smell receptors Hypothalamus and medulla oblongata 1 Stomach distension activates stretch receptors Vagovagal reflexes Medulla Intestinal phase Stimulate Inhibit Vagus nerve Local reflexes 2 Food chemicals G cells (especially peptides and caffeine) and rising p. H activate chemoreceptors 1 Presence of partially digested foods in duodenum or distension of the duodenum when stomach begins to empty Vagus nerve Intestinal (enteric) gastrin release to blood Gastrin release to blood Cerebral cortex 1 Loss of appetite, depression Gastrin secretion declines G cells Overrides parasympathetic controls Sympathetic nervous system activation 1 Excessive acidity (p. H < 2) in stomach 2 Emotional stress Lack of stimulatory impulses to parasympathetic center Stomach secretory activity Enterogastric reflex Brief effect Local reflexes Vagal nuclei in medulla Pyloric sphincter Release of enterogastrones (secretin, cholecystokinin, vasoactive intestinal peptide) 1 Distension of duodenum; presence of fatty, acidic, or hypertonic chyme; and/or irritants in the duodenum 2 Distension; presence of fatty, acidic, partially digested food in the duodenum © 2013 Pearson Education, Inc.
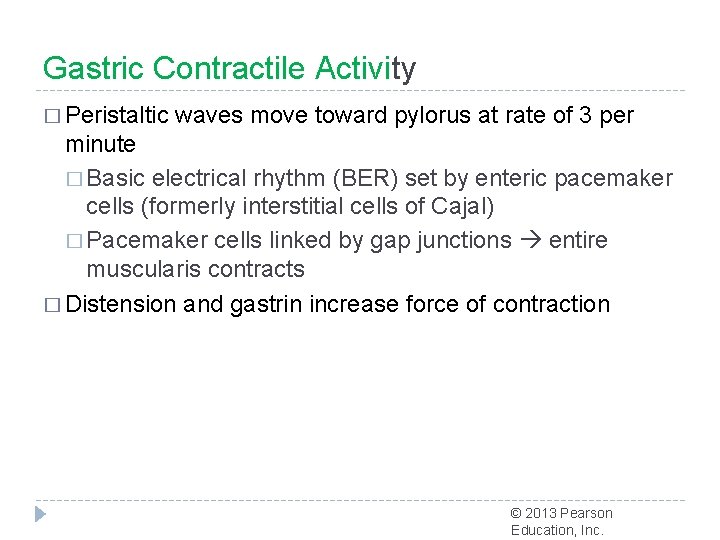
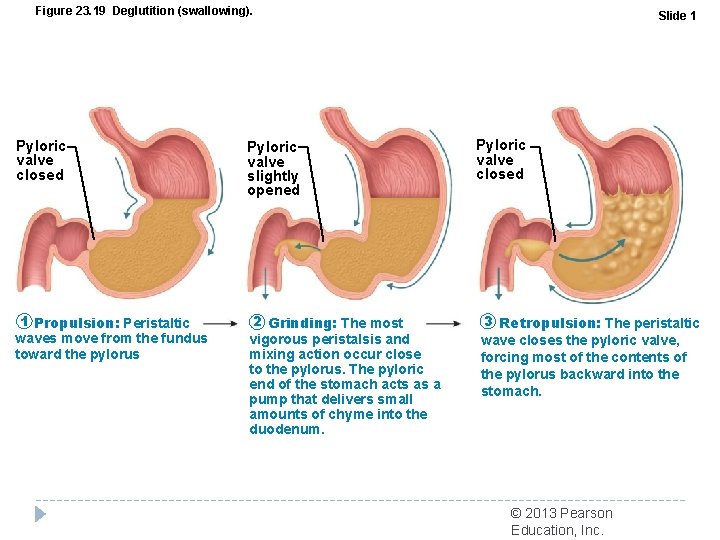
Gastric Contractile Activity � Peristaltic waves move toward pylorus at rate of 3 per minute � Basic electrical rhythm (BER) set by enteric pacemaker cells (formerly interstitial cells of Cajal) � Pacemaker cells linked by gap junctions entire muscularis contracts � Distension and gastrin increase force of contraction © 2013 Pearson Education, Inc.
Gastric Contractile Activity � Most vigorous near pylorus � Chyme is either � Delivered in ~3 ml spurts to duodenum, or � Forced backward into stomach © 2013 Pearson Education, Inc.
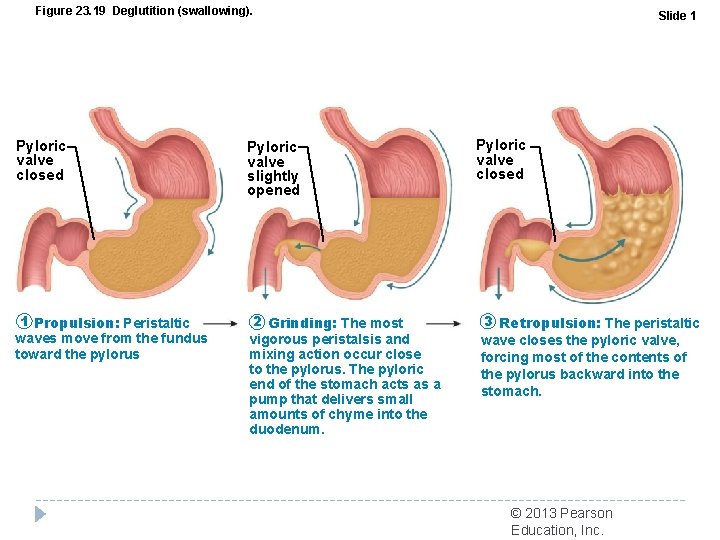
Figure 23. 19 Deglutition (swallowing). Pyloric valve closed 1 Propulsion: Peristaltic waves move from the fundus toward the pylorus Pyloric valve slightly opened 2 Grinding: The most vigorous peristalsis and mixing action occur close to the pylorus. The pyloric end of the stomach acts as a pump that delivers small amounts of chyme into the duodenum. Slide 1 Pyloric valve closed 3 Retropulsion: The peristaltic wave closes the pyloric valve, forcing most of the contents of the pylorus backward into the stomach. © 2013 Pearson Education, Inc.
Regulation of Gastric Emptying � As chyme enters duodenum � Receptors respond to stretch and chemical signals � Enterogastric reflex and enterogastrones inhibit gastric secretion and duodenal filling � Carbohydrate-rich chyme moves quickly through duodenum � Fatty chyme remains in duodenum 6 hours or more © 2013 Pearson Education, Inc.
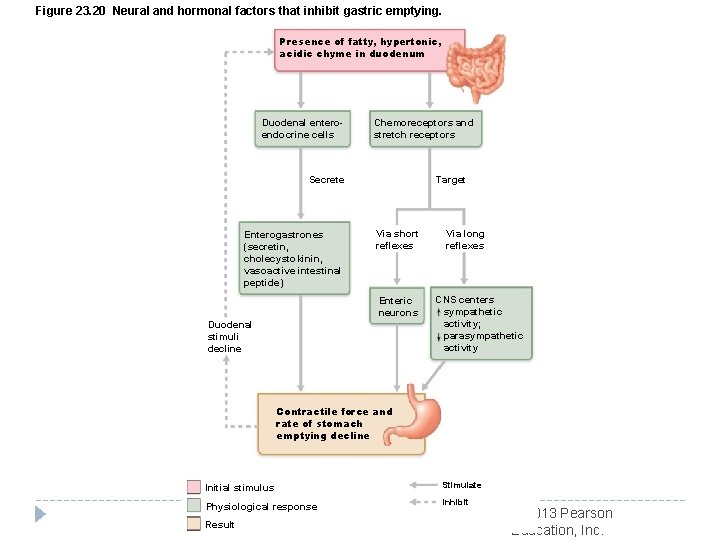
Figure 23. 20 Neural and hormonal factors that inhibit gastric emptying. Presence of fatty, hypertonic, acidic chyme in duodenum Duodenal enteroendocrine cells Chemoreceptors and stretch receptors Secrete Enterogastrones (secretin, cholecystokinin, vasoactive intestinal peptide) Target Via short reflexes Enteric neurons Duodenal stimuli decline Via long reflexes CNS centers sympathetic activity; parasympathetic activity Contractile force and rate of stomach emptying decline Initial stimulus Stimulate Physiological response Inhibit Result © 2013 Pearson Education, Inc.
Homeostatic Imbalance �Vomiting (emesis) caused by �Extreme stretching �Intestinal irritants, e. g. , bacterial toxins, excessive alcohol, spicy food, certain drugs � Chemicals/sensory impulses emetic center of medulla � Excessive vomiting dehydration, electrolyte and acidbase imbalances (alkalosis) © 2013 Pearson Education, Inc.
Intestinal Juice � 1 -2 L secreted daily in response to distension or irritation of mucosa � Slightly alkaline; isotonic with blood plasma � Largely water; enzyme-poor (enzymes of small intestine only in brush border); contains mucus � Facilitates transport and absorption of nutrients © 2013 Pearson Education, Inc.
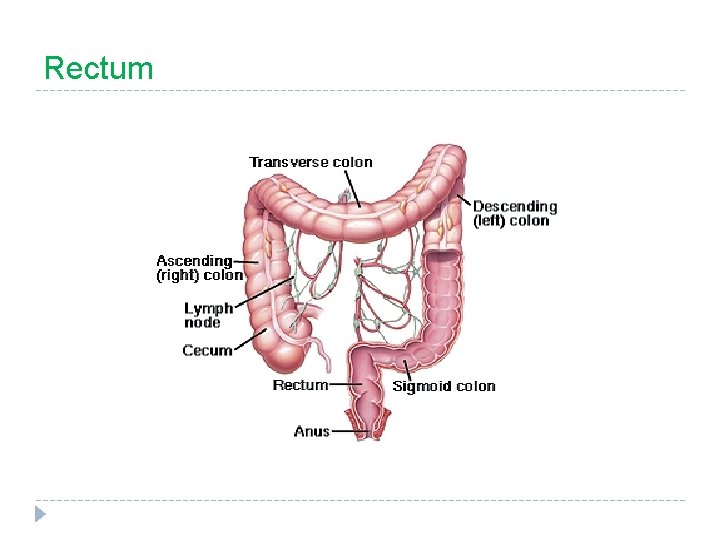
Large Intestine � “colon” � larger in diameter but shorter than small intestine (which it “frames”) � functions: 1. dry out indigestible food residue by absorbing water 2. elimination
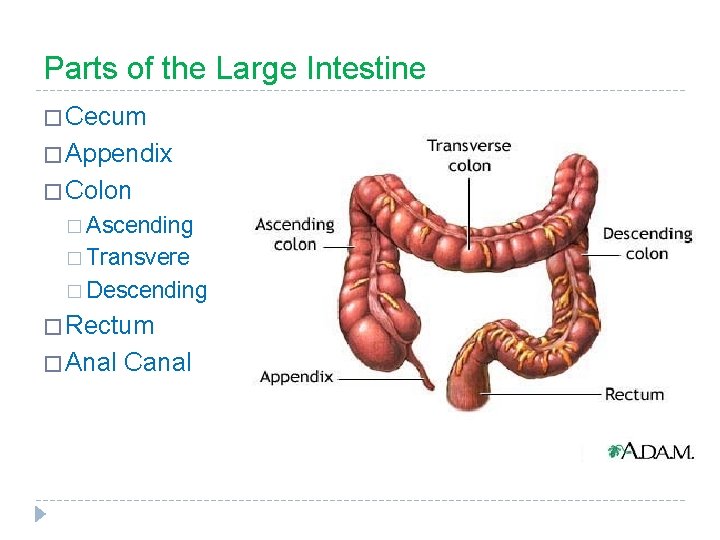
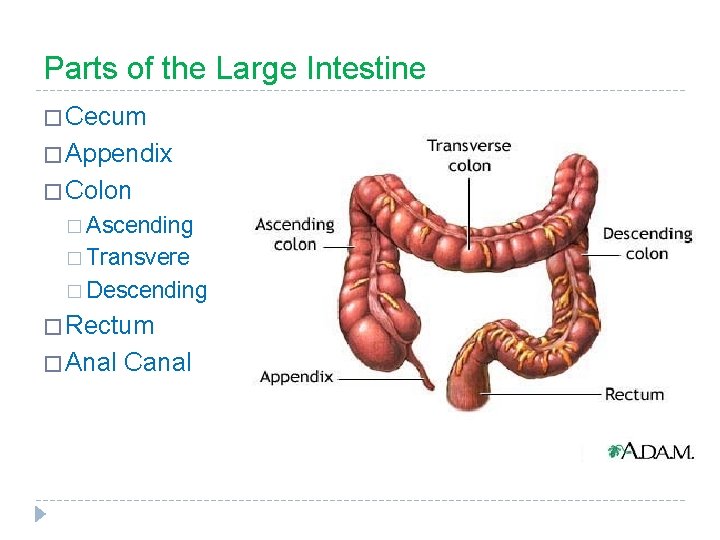
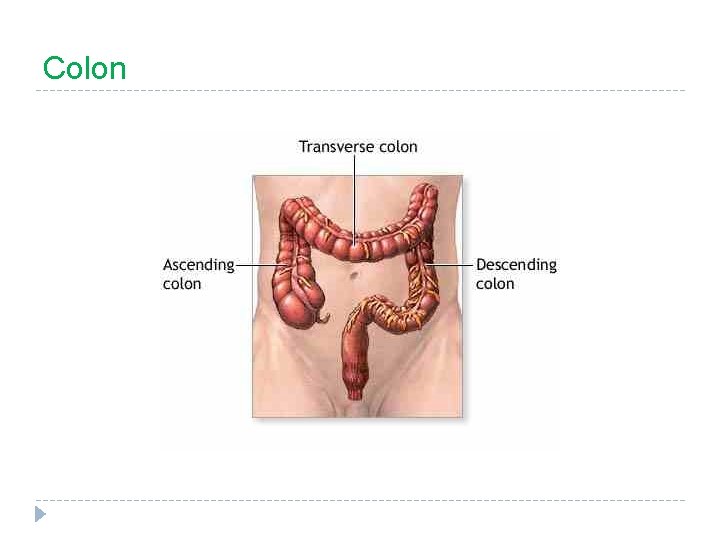
Parts of the Large Intestine � Cecum � Appendix � Colon � Ascending � Transvere � Descending � Rectum � Anal Canal
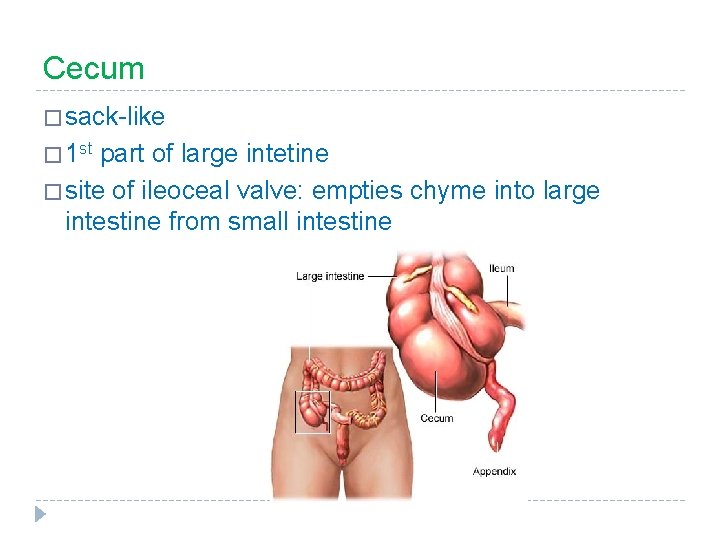
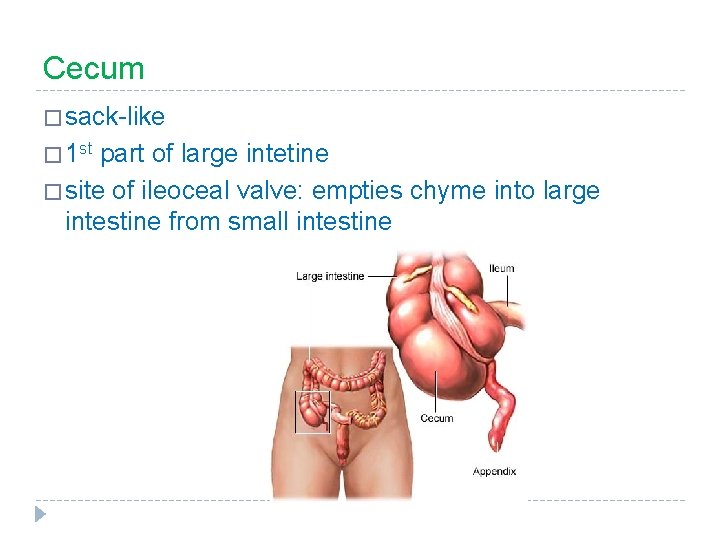
Cecum � sack-like � 1 st part of large intetine � site of ileoceal valve: empties chyme into large intestine from small intestine
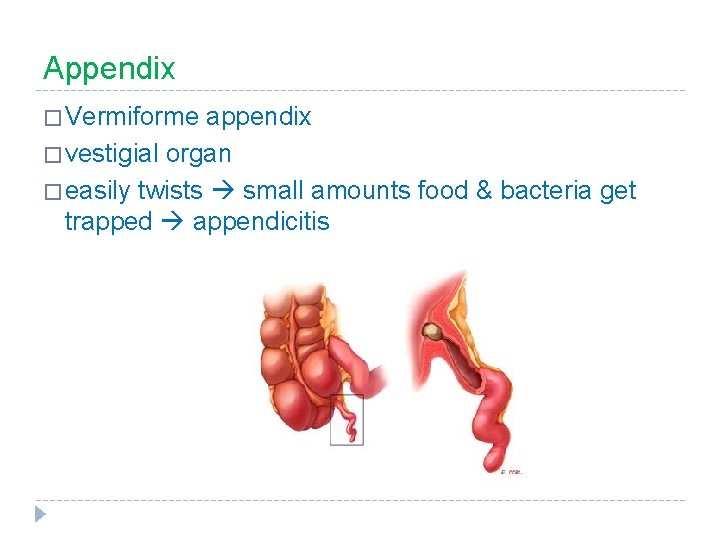
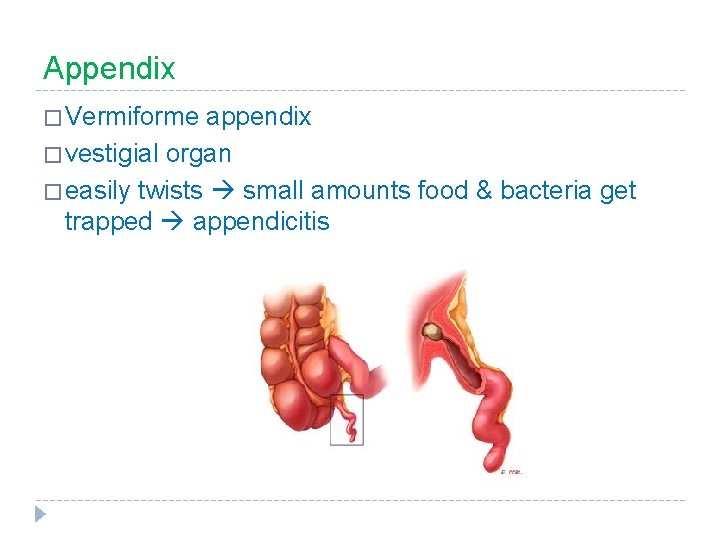
Appendix � Vermiforme appendix � vestigial organ � easily twists small amounts food & bacteria get trapped appendicitis
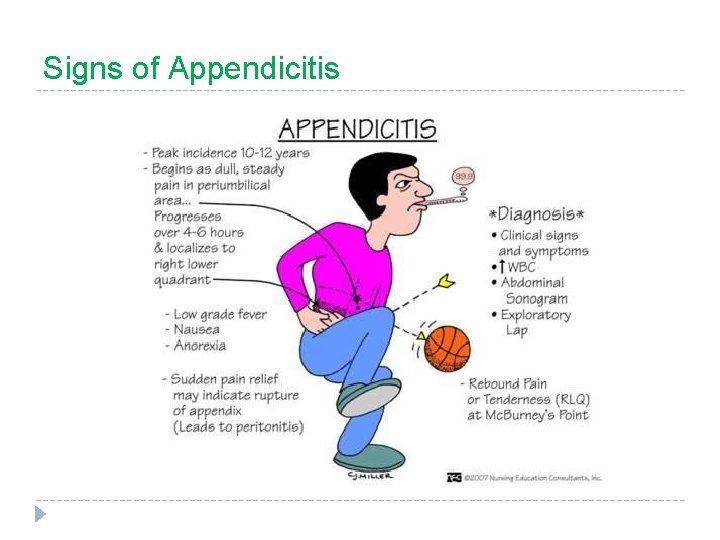
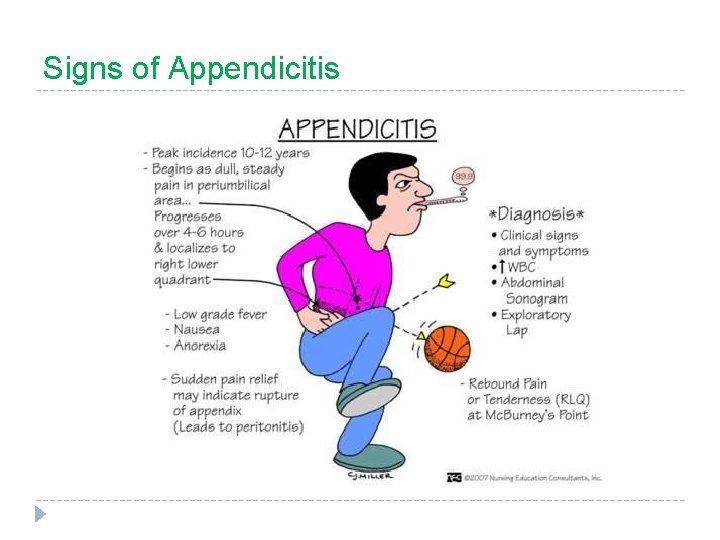
Signs of Appendicitis
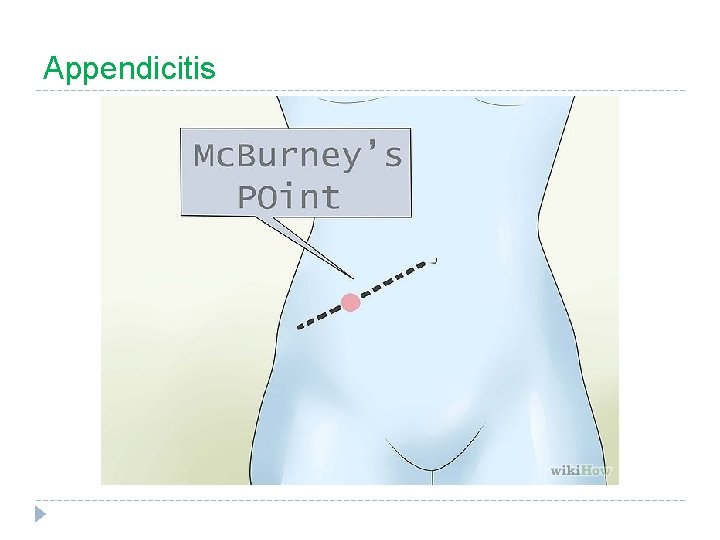
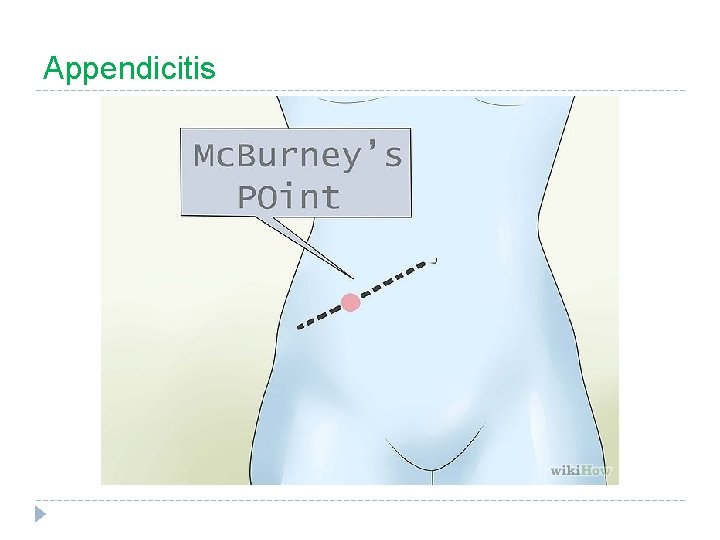
Appendicitis
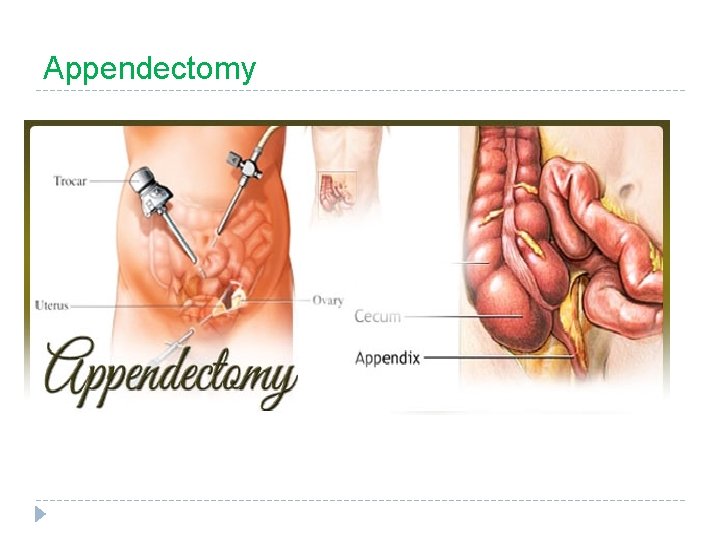
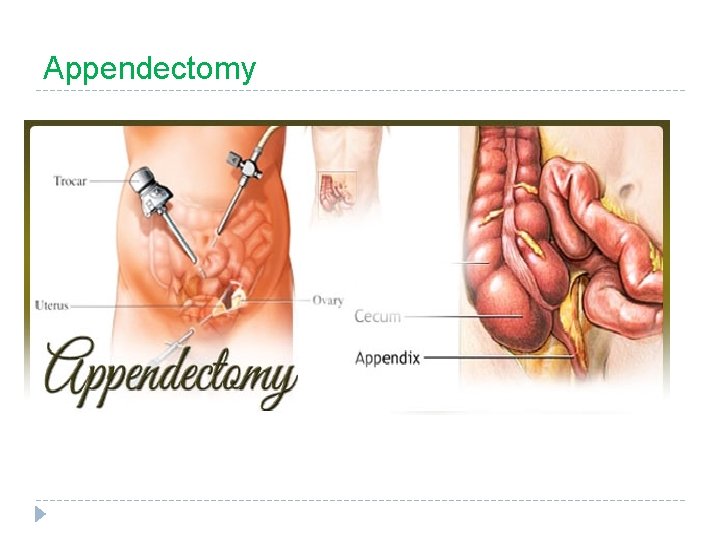
Appendectomy
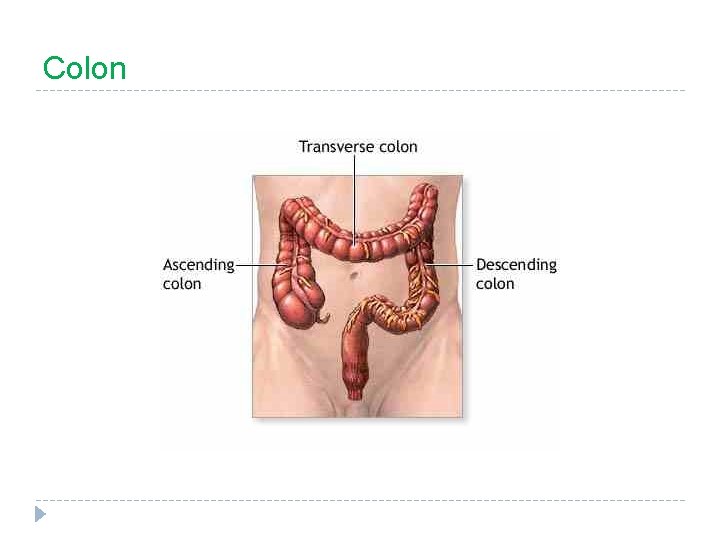
Colon
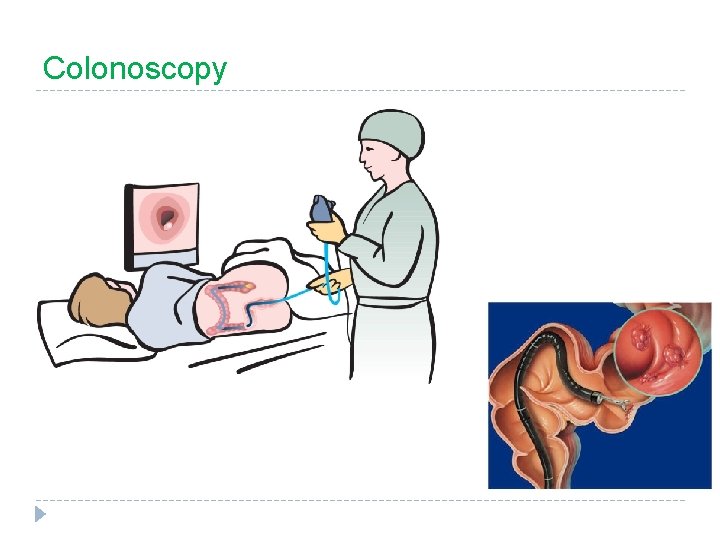
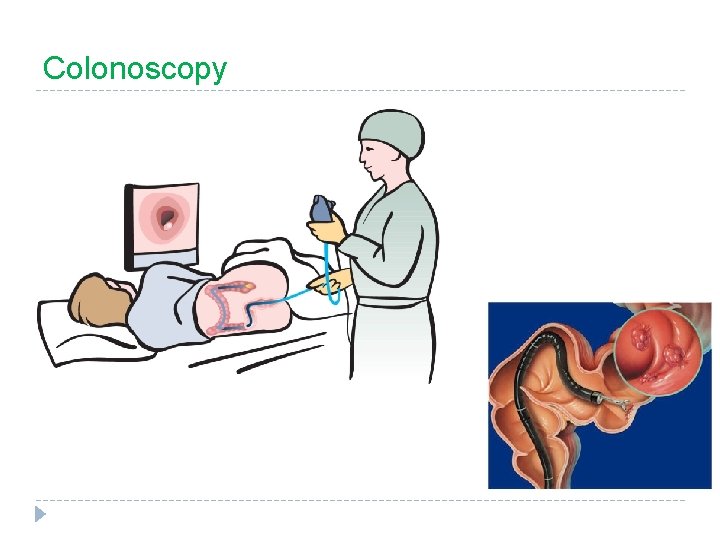
Colonoscopy
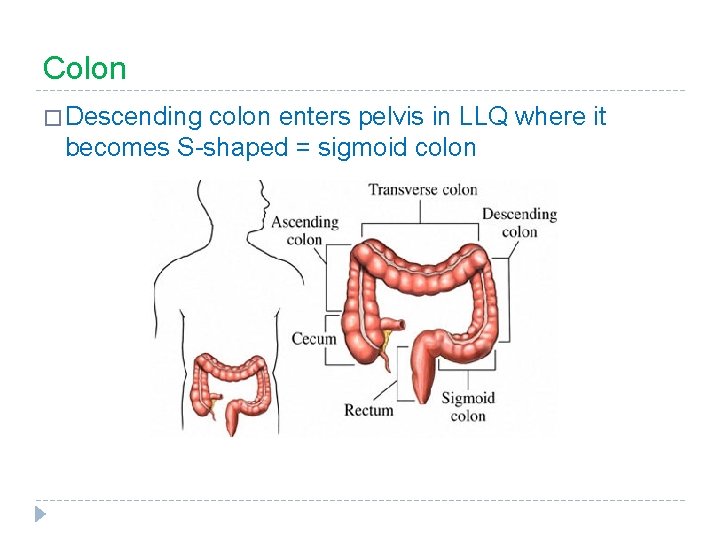
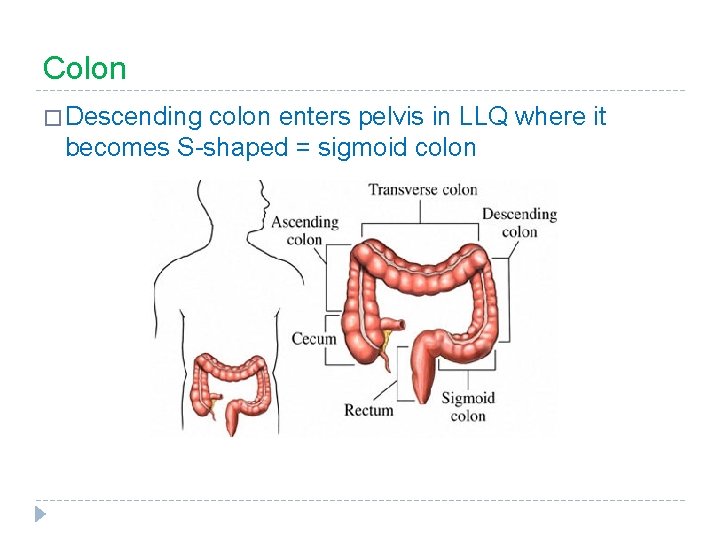
Colon � Descending colon enters pelvis in LLQ where it becomes S-shaped = sigmoid colon
Rectum
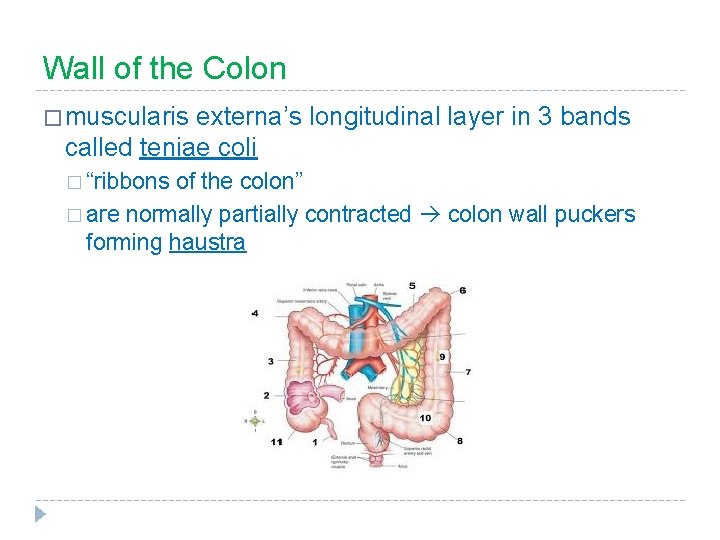
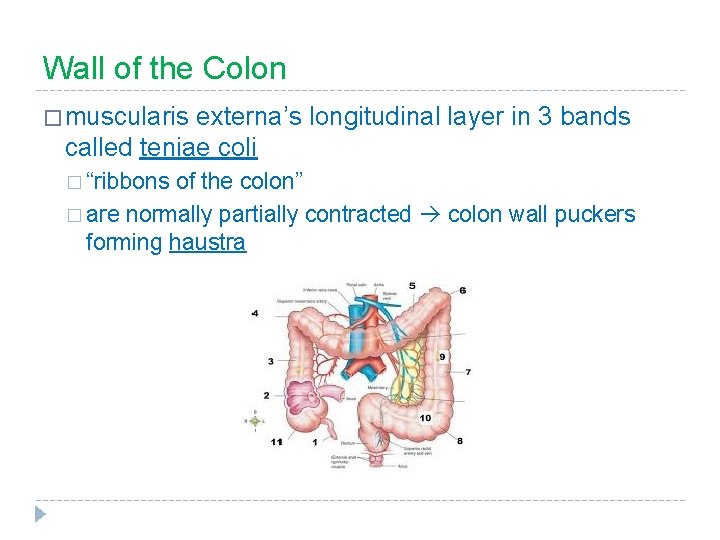
Wall of the Colon � muscularis externa’s longitudinal layer in 3 bands called teniae coli � “ribbons of the colon” � are normally partially contracted colon wall puckers forming haustra
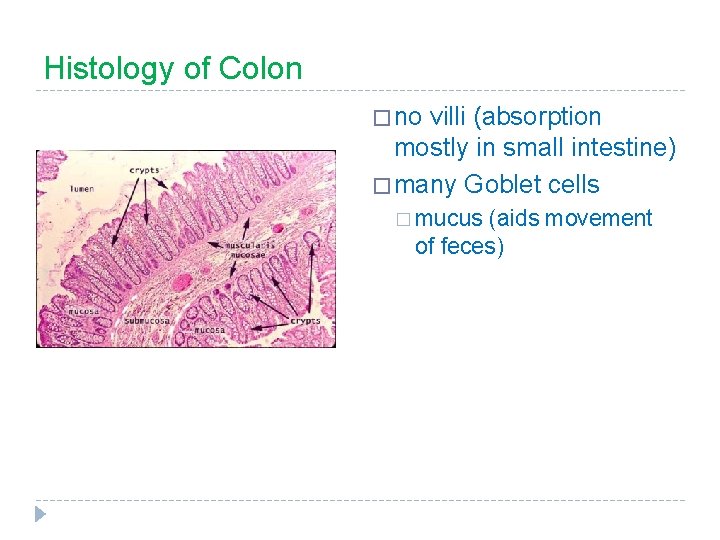
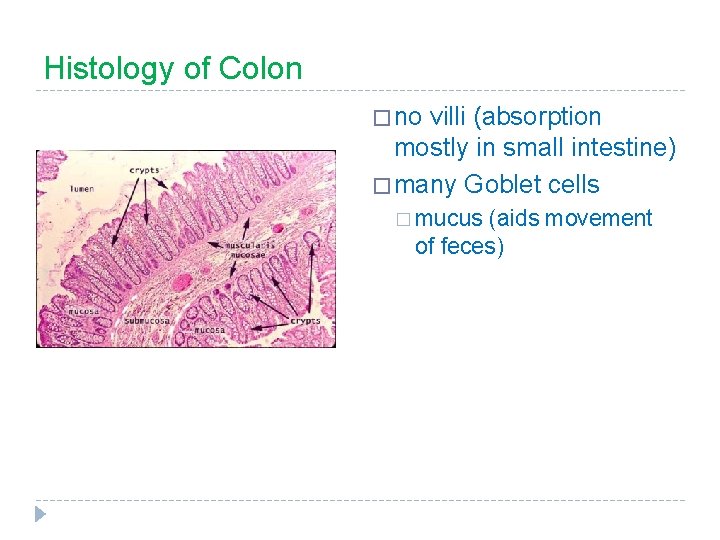
Histology of Colon � no villi (absorption mostly in small intestine) � many Goblet cells � mucus (aids movement of feces)
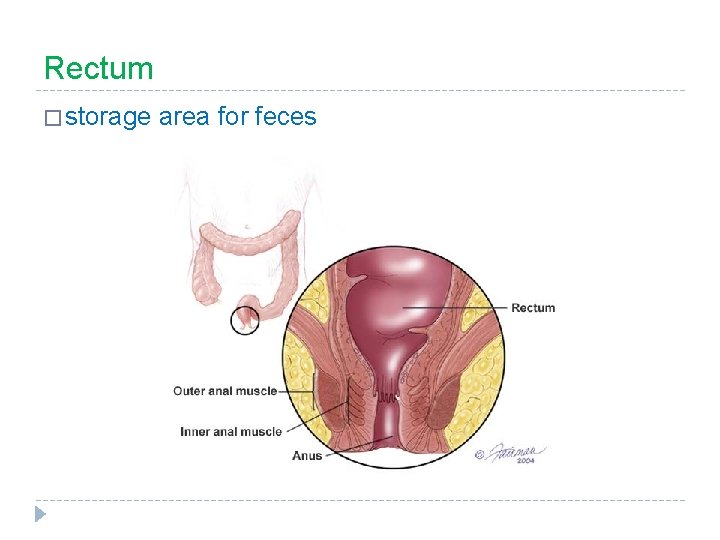
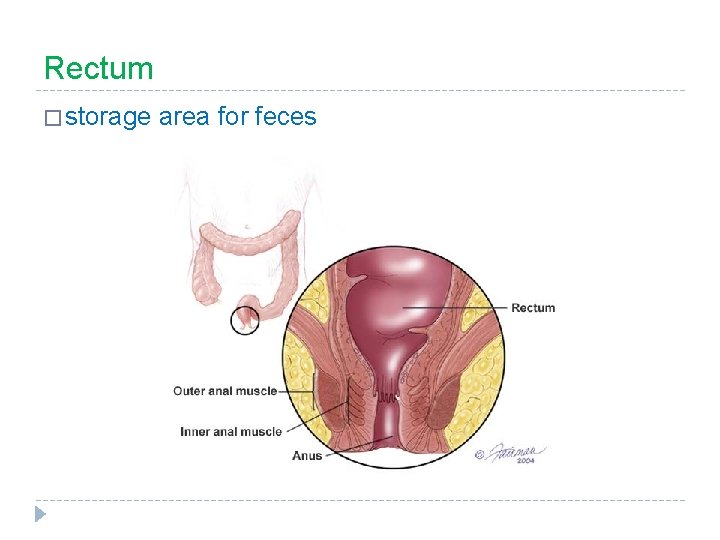
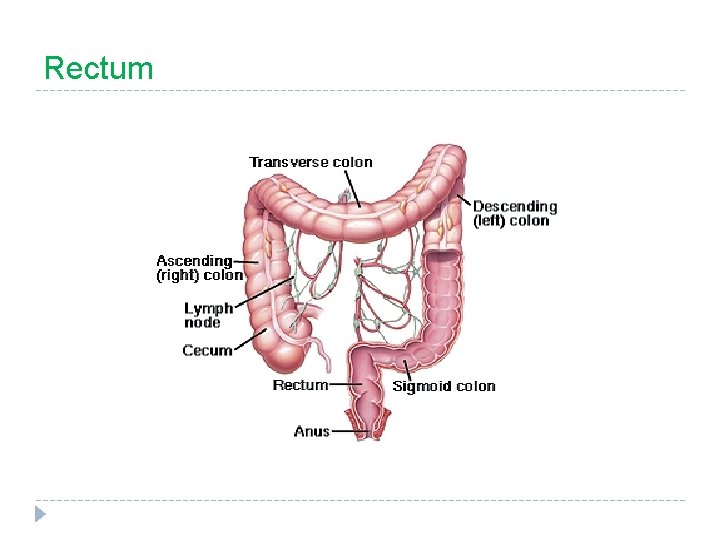
Rectum � storage area for feces
Anal Canal � 2 sphincters: external sphincter 1. � skeletal muscle (voluntary) internal sphincter 2. � smooth muscle (involuntary)