Digestive system I Alimentary tract Continuous provision Water
- Slides: 27
Digestive system I
Alimentary tract • Continuous provision – Water – Electrolytes – Nutrients • Achieved by – Movement of food – Digestion • Mechanical and chemical – Absorption – Transport
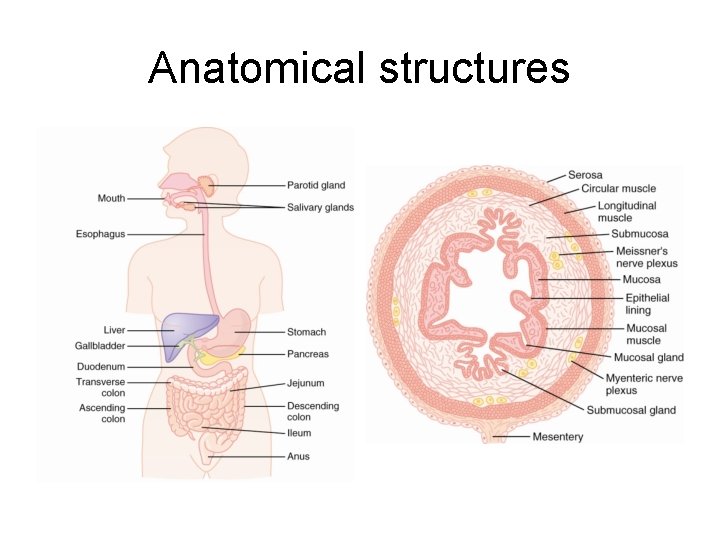
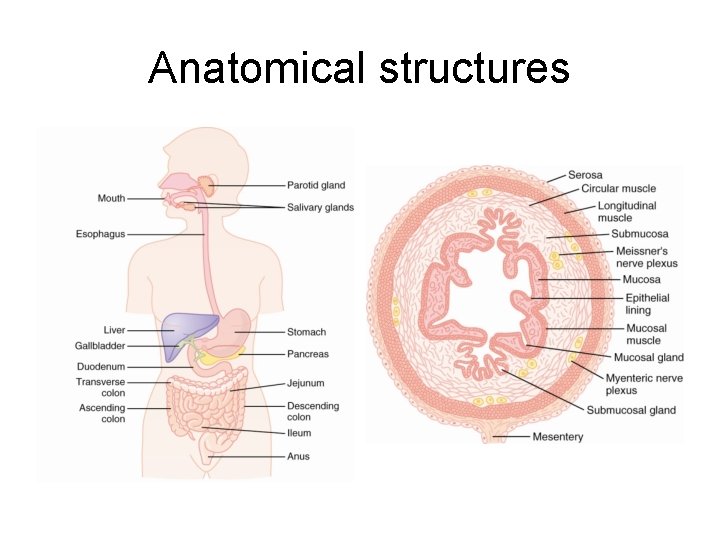
Anatomical structures
Smooth muscles within the GI tract • Layers – Longitudinal • Length-wise – Circular – Formation of syncitium • Each fiber within respective layer – Connected via gap junctions • Ion movement
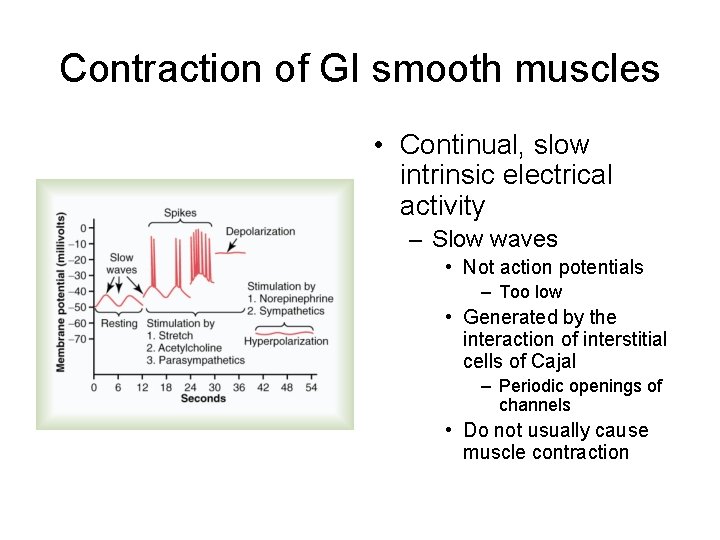
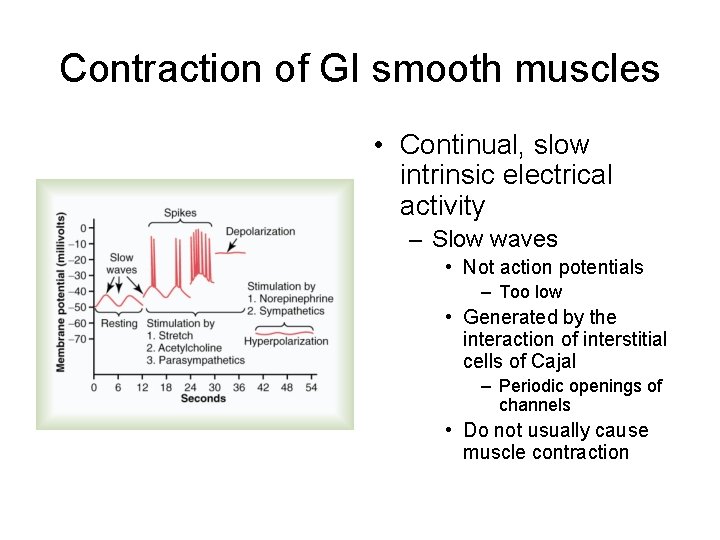
Contraction of GI smooth muscles • Continual, slow intrinsic electrical activity – Slow waves • Not action potentials – Too low • Generated by the interaction of interstitial cells of Cajal – Periodic openings of channels • Do not usually cause muscle contraction
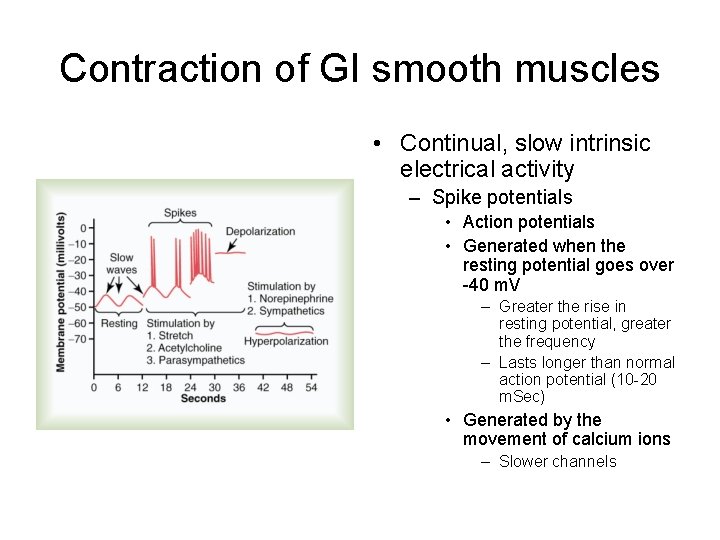
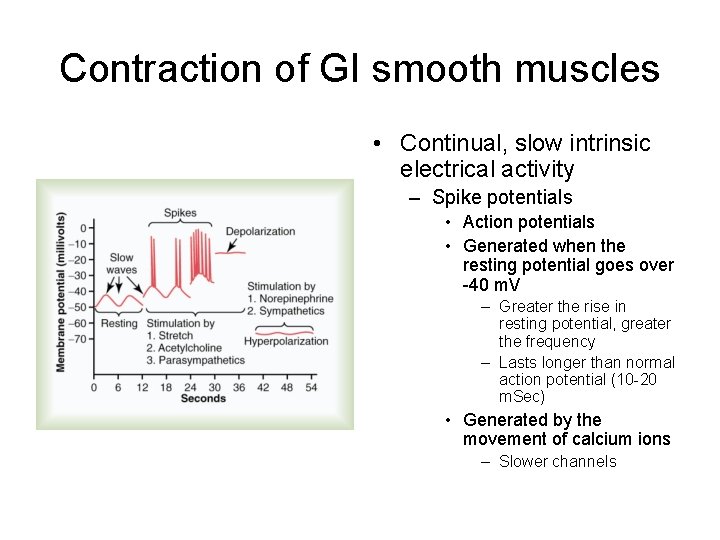
Contraction of GI smooth muscles • Continual, slow intrinsic electrical activity – Spike potentials • Action potentials • Generated when the resting potential goes over -40 m. V – Greater the rise in resting potential, greater the frequency – Lasts longer than normal action potential (10 -20 m. Sec) • Generated by the movement of calcium ions – Slower channels
• Changes in resting potentials – Depolarization • • Stretching of muscle Acetylcholine Stimulation of parasympathetic nerves GI hormones – Hyperpolarization • Epinephrine and norepinephrine • Stimulation of sympathetic nerves
• Role of calcium ions – Entrance to cells • Slow waves – No muscle contraction • Spike potentials • Tonic – Continuous but not associated with slow waves • Continuous repetitive spike potentials • Hormones and other factors • Continuous entry of calcium ions – Not associated with changes in membrane potential
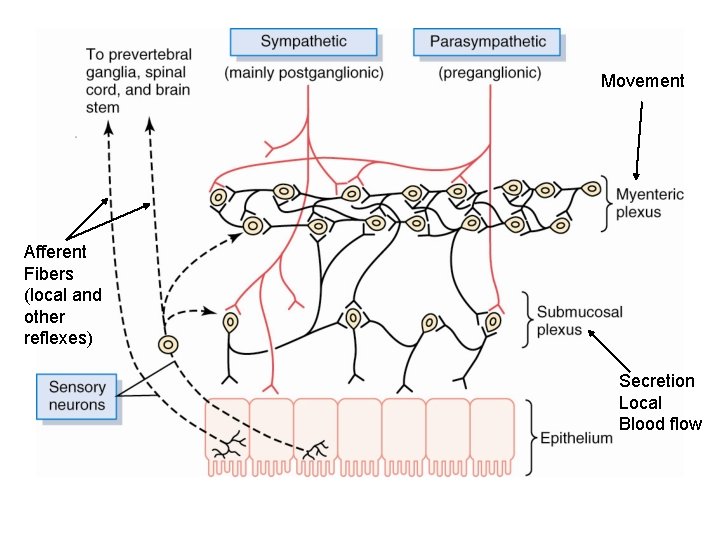
Enteric nervous system • Regulation – GI tract movement – GI tract secretion
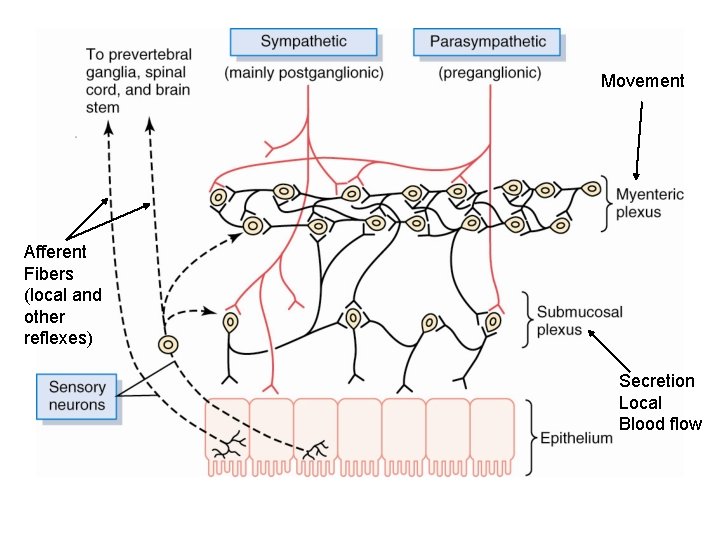
Movement Afferent Fibers (local and other reflexes) Secretion Local Blood flow
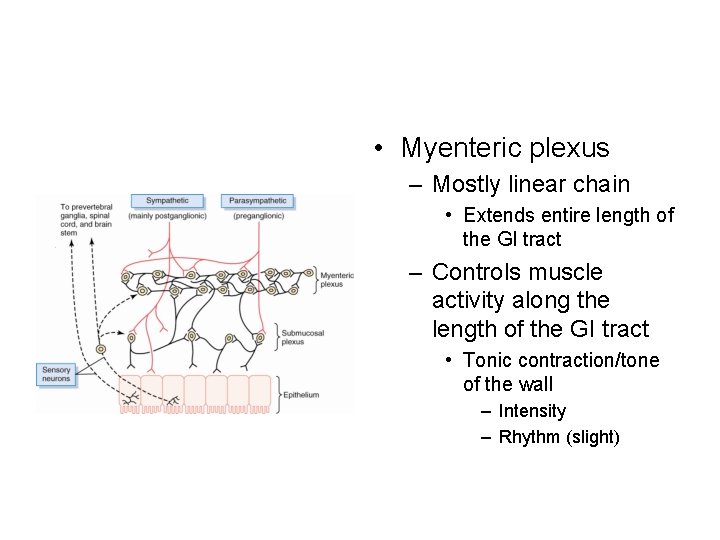
• Myenteric plexus – Mostly linear chain • Extends entire length of the GI tract – Controls muscle activity along the length of the GI tract • Tonic contraction/tone of the wall – Intensity – Rhythm (slight)
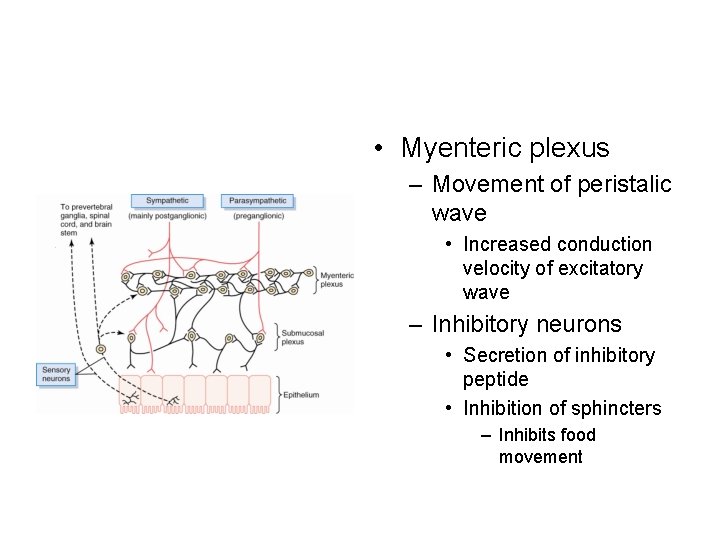
• Myenteric plexus – Movement of peristalic wave • Increased conduction velocity of excitatory wave – Inhibitory neurons • Secretion of inhibitory peptide • Inhibition of sphincters – Inhibits food movement
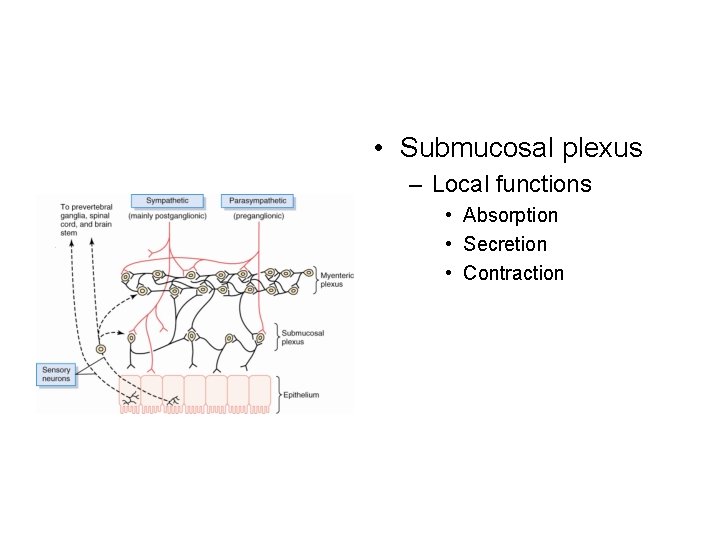
• Submucosal plexus – Local functions • Absorption • Secretion • Contraction
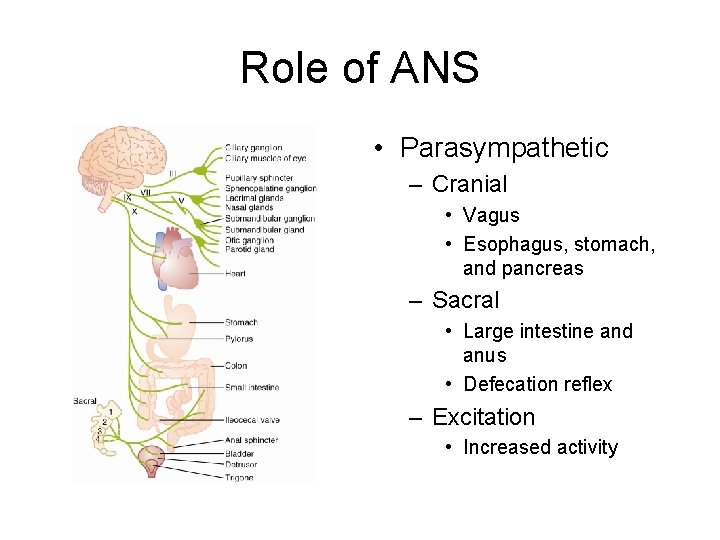
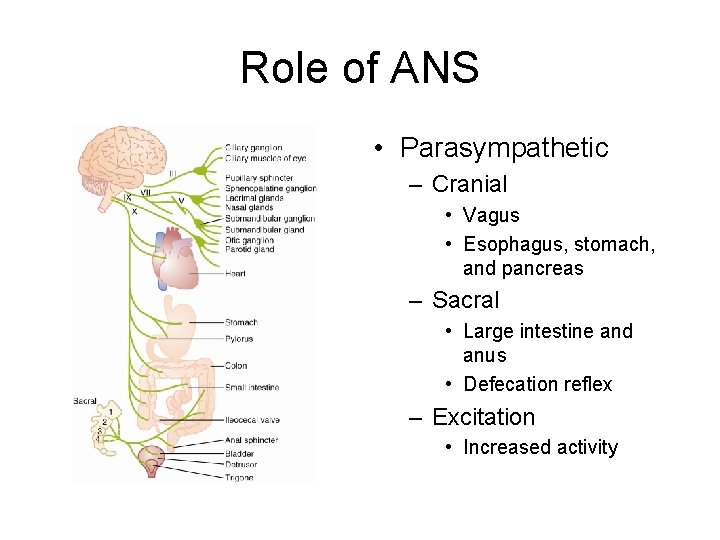
Role of ANS • Parasympathetic – Cranial • Vagus • Esophagus, stomach, and pancreas – Sacral • Large intestine and anus • Defecation reflex – Excitation • Increased activity
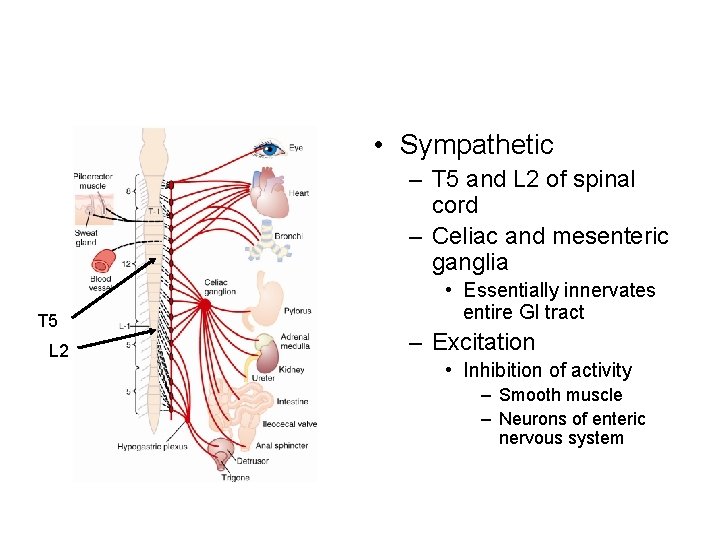
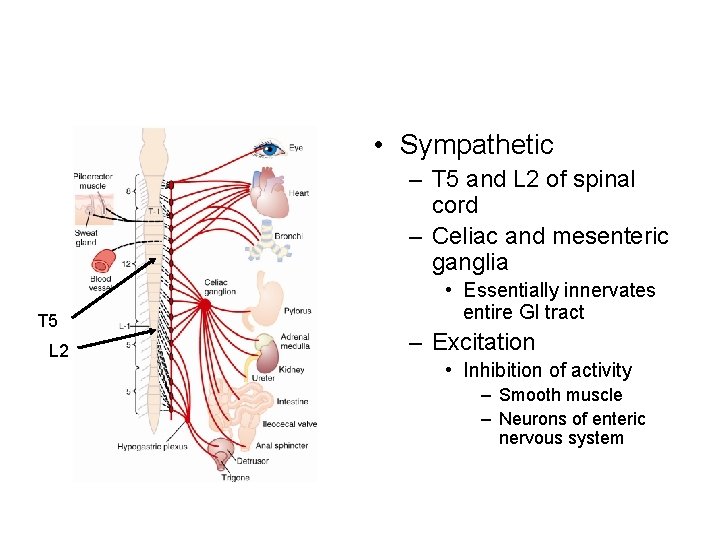
• Sympathetic – T 5 and L 2 of spinal cord – Celiac and mesenteric ganglia T 5 L 2 • Essentially innervates entire GI tract – Excitation • Inhibition of activity – Smooth muscle – Neurons of enteric nervous system
• Neurotransmitters – Aceylcholine • Excitation – Norepinephrine/epinephrine • Inhibition
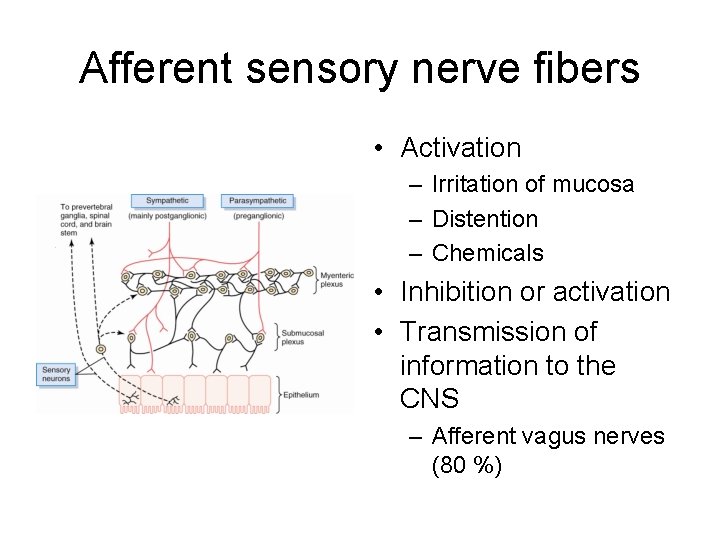
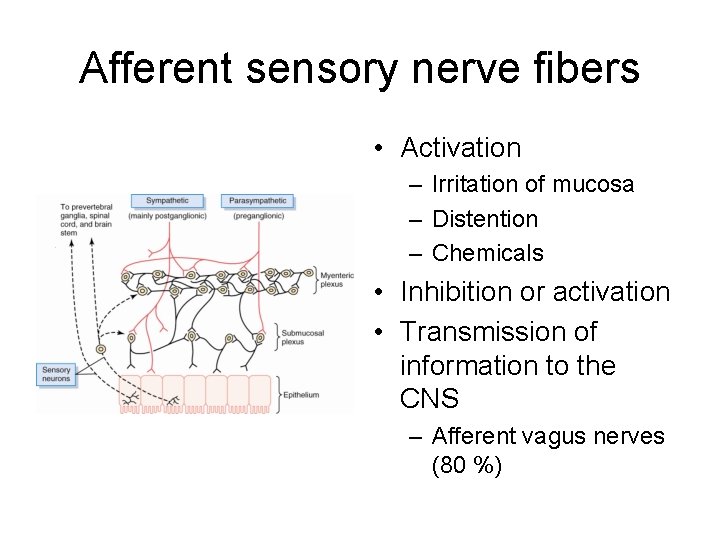
Afferent sensory nerve fibers • Activation – Irritation of mucosa – Distention – Chemicals • Inhibition or activation • Transmission of information to the CNS – Afferent vagus nerves (80 %)
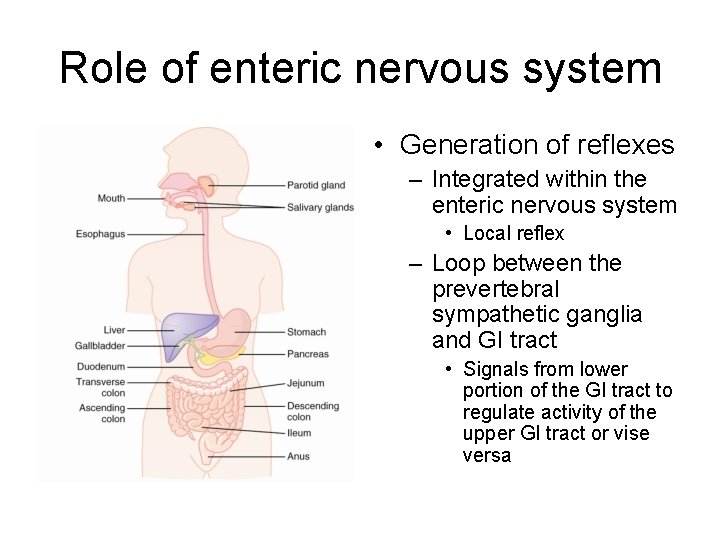
Role of enteric nervous system • Generation of reflexes – Integrated within the enteric nervous system • Local reflex – Loop between the prevertebral sympathetic ganglia and GI tract • Signals from lower portion of the GI tract to regulate activity of the upper GI tract or vise versa
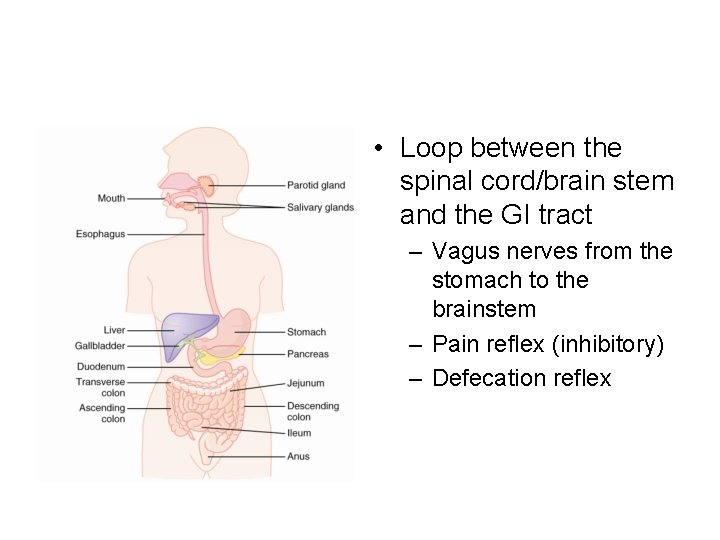
• Loop between the spinal cord/brain stem and the GI tract – Vagus nerves from the stomach to the brainstem – Pain reflex (inhibitory) – Defecation reflex
Movement within the GI tract • Propulsive movement – Peristalsis • Generated in response to GI tract distension • Requires active myenteric plexus – Formation of the contractile rings – Receptive relaxation • Polarized movement – Move in one direction
• Mixing movement – Inhibition of peristalisis forward movement • Sphincter • Churning of the content within the segment – Local intermittent constrictive contractions
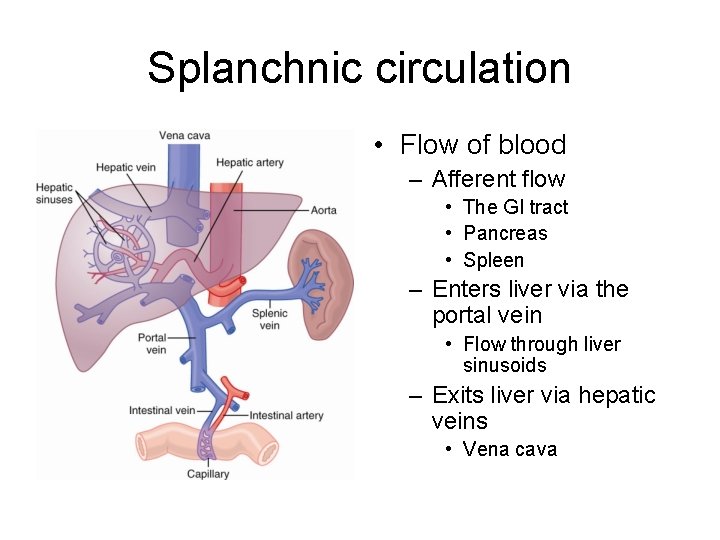
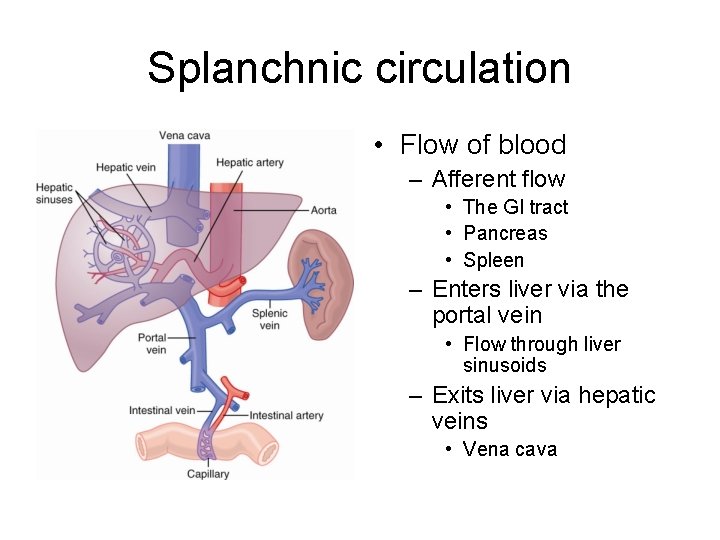
Splanchnic circulation • Flow of blood – Afferent flow • The GI tract • Pancreas • Spleen – Enters liver via the portal vein • Flow through liver sinusoids – Exits liver via hepatic veins • Vena cava
• Absorption of nutrients – Water soluble molecules • 75 % temporally stored in liver – Fats • Intestinal lymphatics • Enters circulation via thoracic duct
• Arterial supply to the GI tract – Mesenteric arteries (superior and inferior) • Intestines – Celiac artery • Stomach • Branches of arteries – Muscle bundles – Intestinal villi – Submucosal vessels
• Rate of flow – Proportional to activity levels • Active absorption increases flow by max. 8 X – Increased flow • Vasodilators • Decreased tissue oxygen concentrations
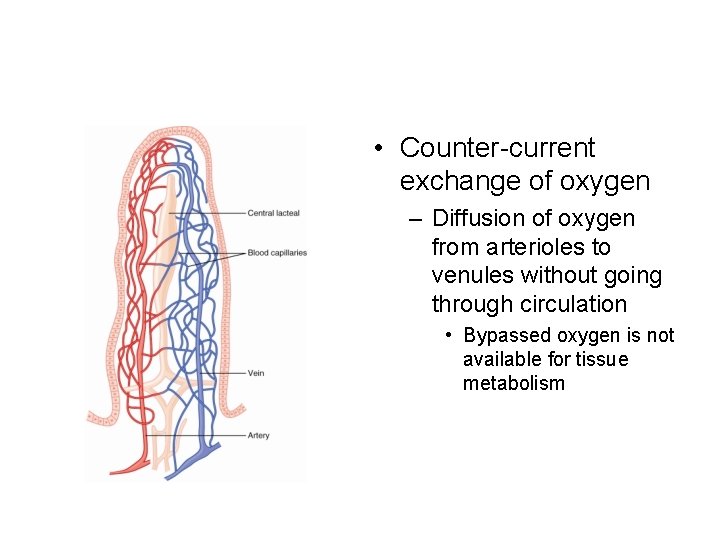
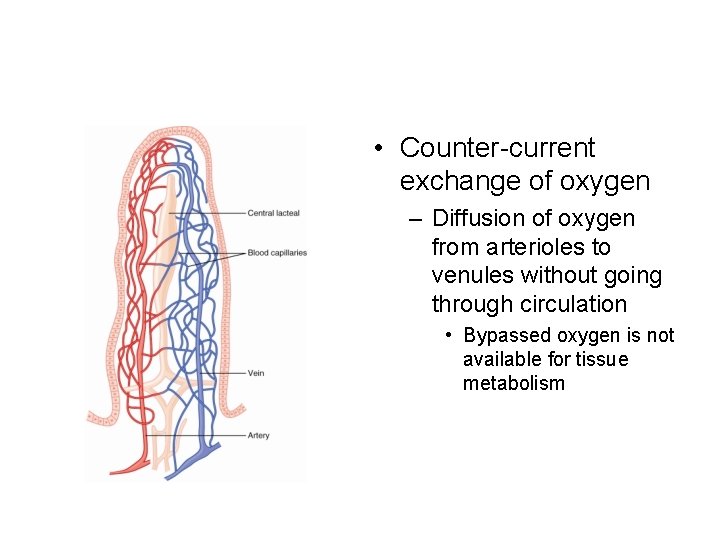
• Counter-current exchange of oxygen – Diffusion of oxygen from arterioles to venules without going through circulation • Bypassed oxygen is not available for tissue metabolism
• Neural regulation – Parasympathietic stimulation • Increased flow • Increased glandular secretions – Cause of increased flow – Sympathetic stimulation • Decreased flow – Vasoconstriction • Overcome by local vasodilators – Local ischemia – Allows re-direction of blood