Digestive System https kidshealth orgenkidsdigestivesystem html The digestive
- Slides: 28
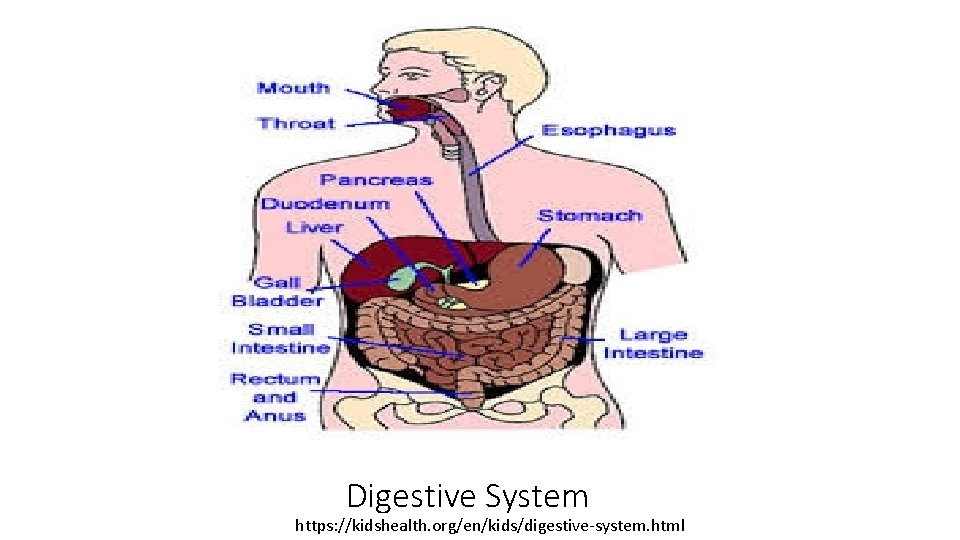
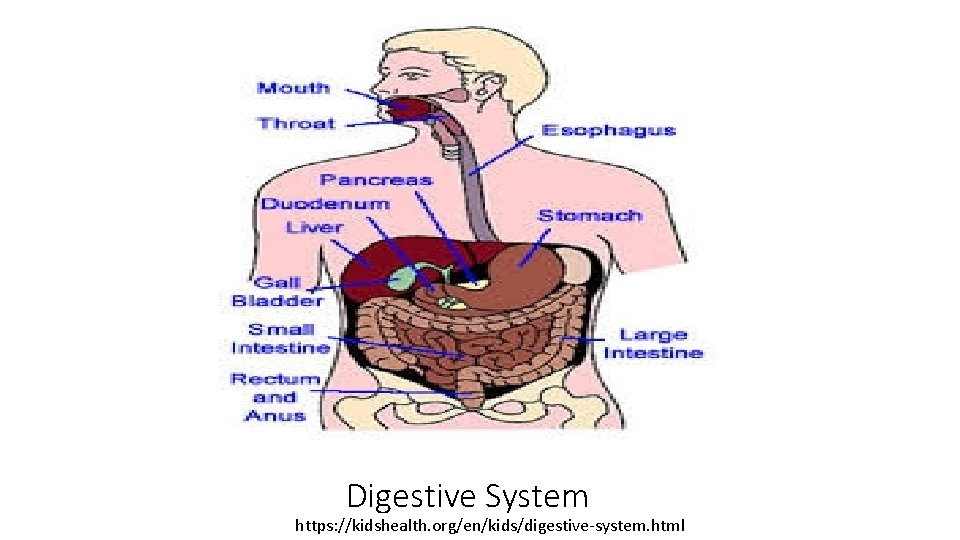
Digestive System https: //kidshealth. org/en/kids/digestive-system. html
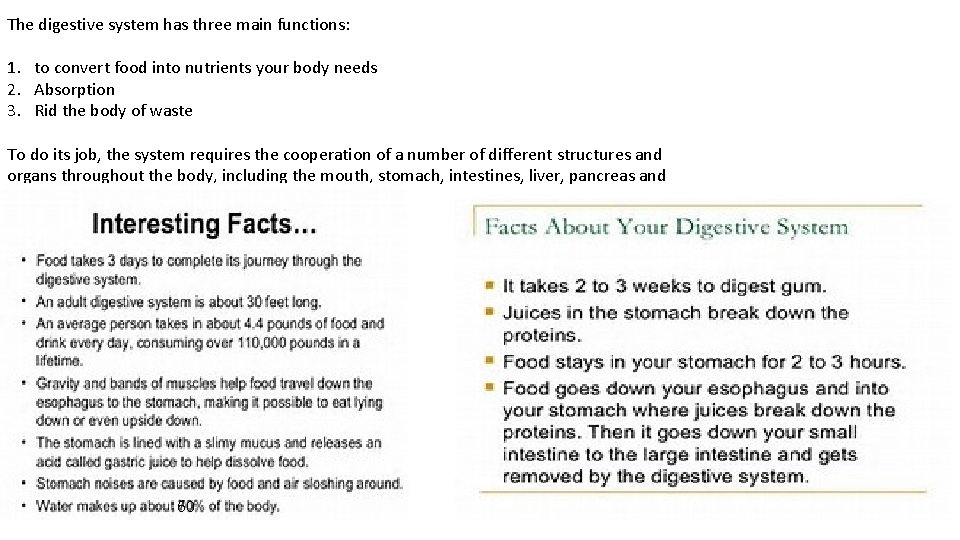
The digestive system has three main functions: 1. to convert food into nutrients your body needs 2. Absorption 3. Rid the body of waste To do its job, the system requires the cooperation of a number of different structures and organs throughout the body, including the mouth, stomach, intestines, liver, pancreas and gallbladder. 60
Hey there!! Here are 10 Fun Facts +1!! • 1. An adult esophagus ranges from 10 to 14 inches in length, and 1 inch in diameter. • 2. We make 1 to 3 pints of saliva a day. • 3. Muscles contract in waves to move the food down the esophagus. Peristalsis action This means that food would get to a person's stomach, even if they were standing on their head • 4. It takes your mouth, esophagus, stomach, small intestine, large intestine, gallbladder, pancreas and liver just to digest a glass of milk. • 5. An adults stomach can hold approximately 1. 5 liters of material. (1 to 1 ½ quarts) • 6. The average male will eat about 50 tons of food during his lifetime in order to sustain a weight of 150 pounds. • 7. Within the colon, a typical person harbors more than 400 distinct species of bacteria. Lactobacillus-used in probiotic foods. E-coli bacteria • PH 5. 5 -7 “Gut Flora” 100 trillion bacteria in the gut! 300 -1, 000 species of bacteria in the digestive tract. • 8. The liver is the largest organ in the body and performs many functions. Four functions I want you to know are: Breaks down toxins, produces bile, stores fat soluble vitamins A, D, K, E, and stores glycogen-sugar • 9. The small intestine (pronounced in-test-in) is a long tube about 1 and a half to 2 inches around, and about 22 feet long. • 10. A full grown horse? ? Their coiled up intestines are 89 feet long. • 11. Food stays in your stomach for 2 to 3 hours. https: //sites. google. com/site/digestivesystem 3051/fun-facts-2
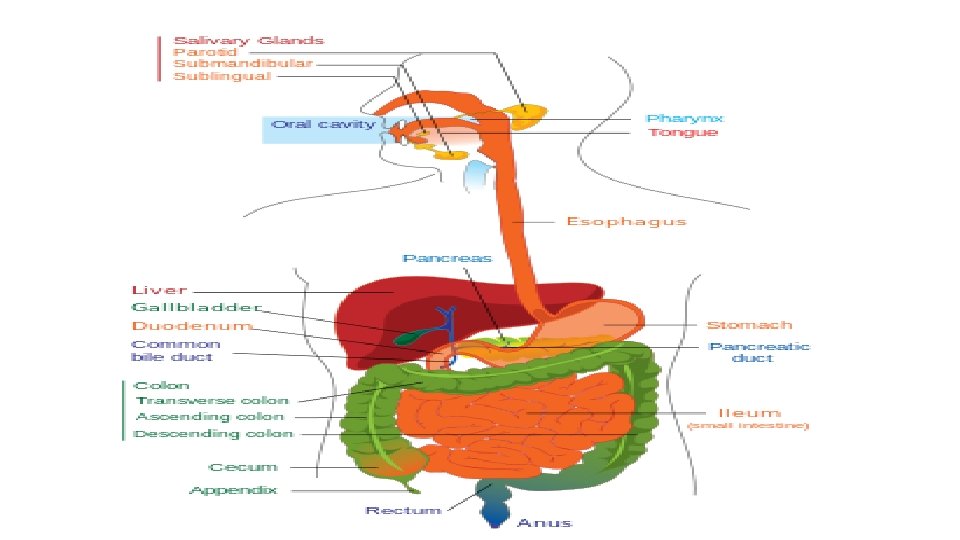
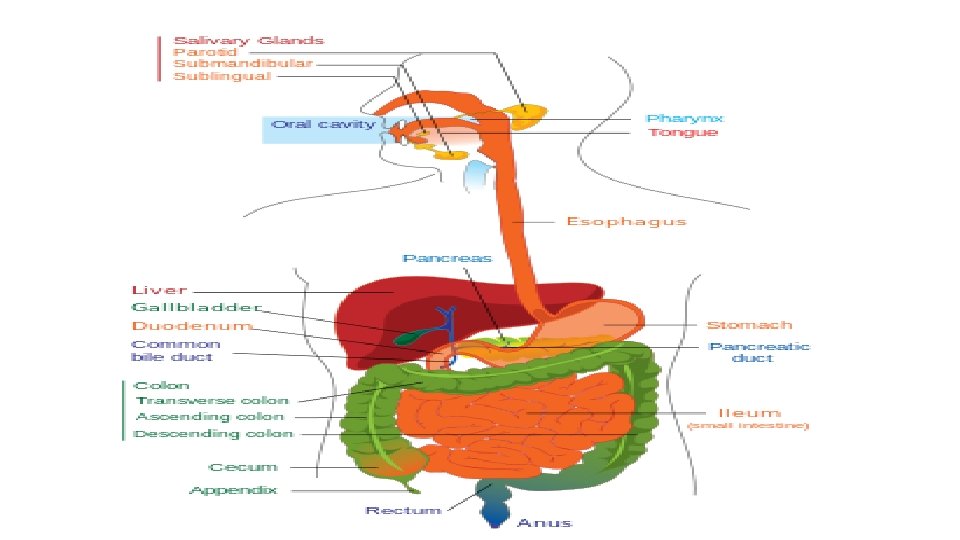
Digestive System Overview • The major parts of the Digestive System: • Salivary glands/Tongue-no hair on the tongue! Microvilli-papilla • Tongue- taste buds, 5 -sweet, salty, sour, bitter and umami(oomaamee) • Pharynx-another name for the throat • Epiglottis-”trap door” • Esophagus-peristalsis action • Stomach-J shaped Gastric juices, HCL • Liver & Gall Bladder • Pancreas • Small Intestine-Villi Most of simpler form of digestion occurs here • Large Intestine No digestion, water intake, High in Bacteria • Rectum • Anus • Accessory digestive organs: liver, gallbladder, pancreas
Esophagus • From pharynx to stomach • Pharynx-Another name for the throat • Salivary glands release mucus for lubrication, antimicrobial agents, and amylase to digest starch. • Epiglottis (Trap door)covers respiratory tract during swallowing • Esophagus-food tube: • At end of esophagus is the lower esophageal sphincter (LES) • Propulsion of food occurs through Peristalsis: • Contraction occurs behind the bolus of food and Relaxation occurs ahead of the bolus of food
Stomach Functions: • store food • initiate digestion of proteins-peptoids • kill bacteria with the strong acidity (low p. H of the gastric juice) HCL • make chyme • material passed from the stomach to the small intestine is called the chyme. • Food stays in this area for 2 -3 hours
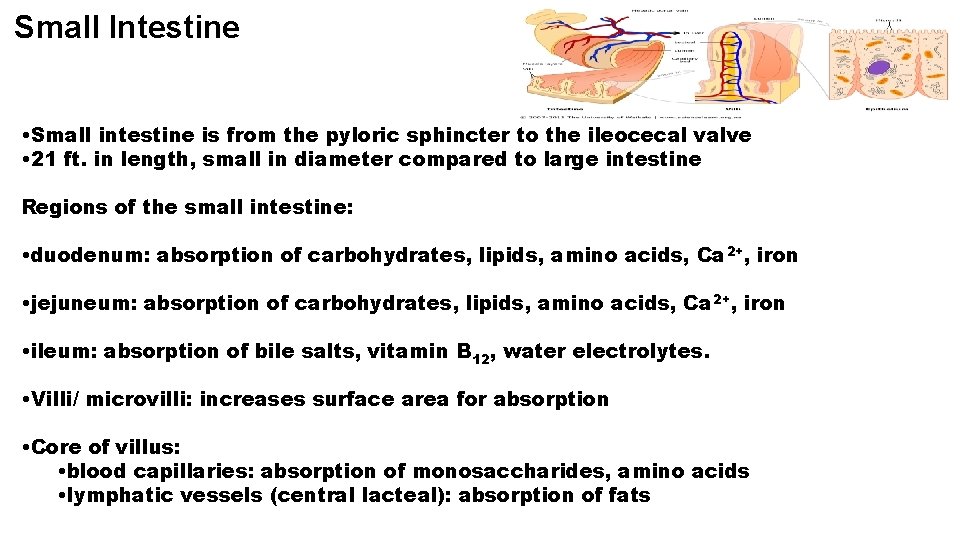
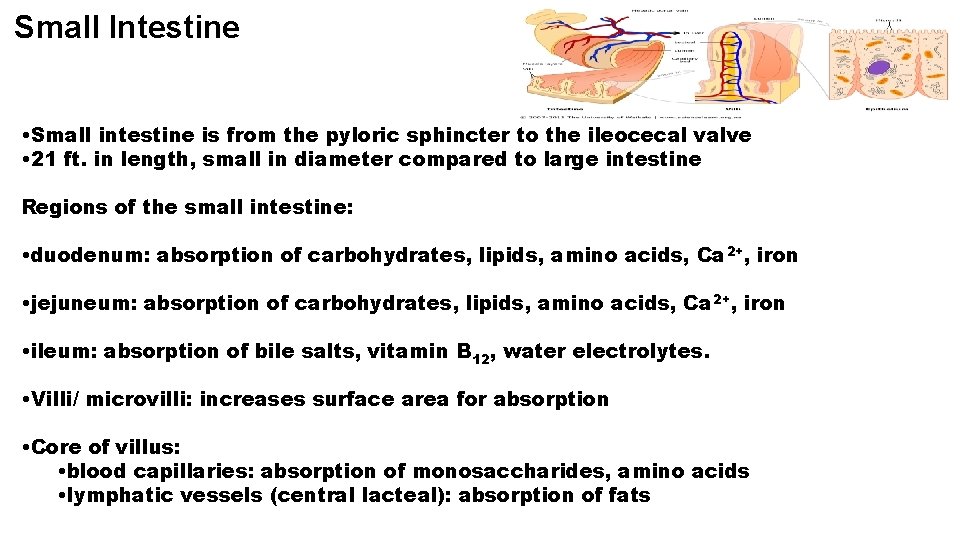
Small Intestine • Small intestine is from the pyloric sphincter to the ileocecal valve • 21 ft. in length, small in diameter compared to large intestine Regions of the small intestine: • duodenum: absorption of carbohydrates, lipids, amino acids, Ca 2+, iron • jejuneum: absorption of carbohydrates, lipids, amino acids, Ca 2+, iron • ileum: absorption of bile salts, vitamin B 12, water electrolytes. • Villi/ microvilli: increases surface area for absorption • Core of villus: • blood capillaries: absorption of monosaccharides, amino acids • lymphatic vessels (central lacteal): absorption of fats
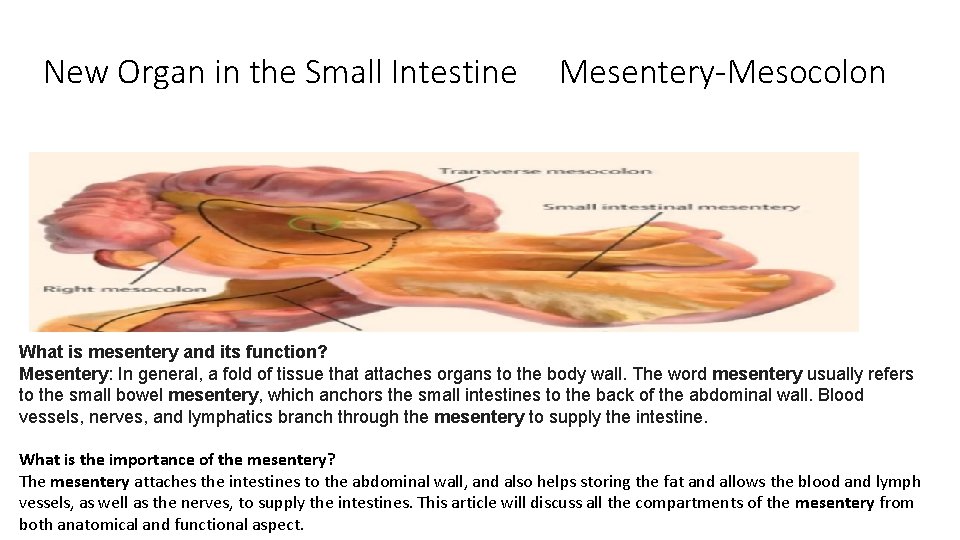
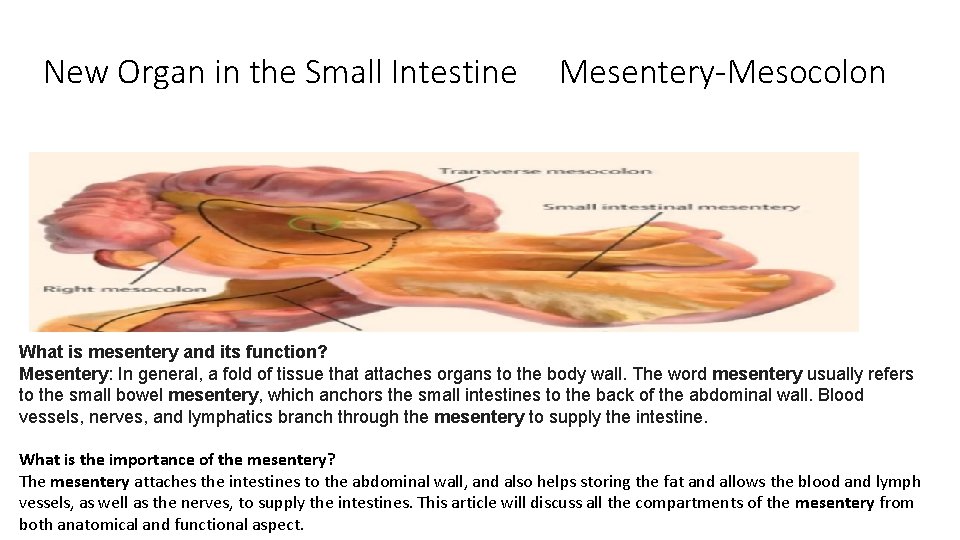
New Organ in the Small Intestine Mesentery-Mesocolon What is mesentery and its function? Mesentery: In general, a fold of tissue that attaches organs to the body wall. The word mesentery usually refers to the small bowel mesentery, which anchors the small intestines to the back of the abdominal wall. Blood vessels, nerves, and lymphatics branch through the mesentery to supply the intestine. What is the importance of the mesentery? The mesentery attaches the intestines to the abdominal wall, and also helps storing the fat and allows the blood and lymph vessels, as well as the nerves, to supply the intestines. This article will discuss all the compartments of the mesentery from both anatomical and functional aspect.
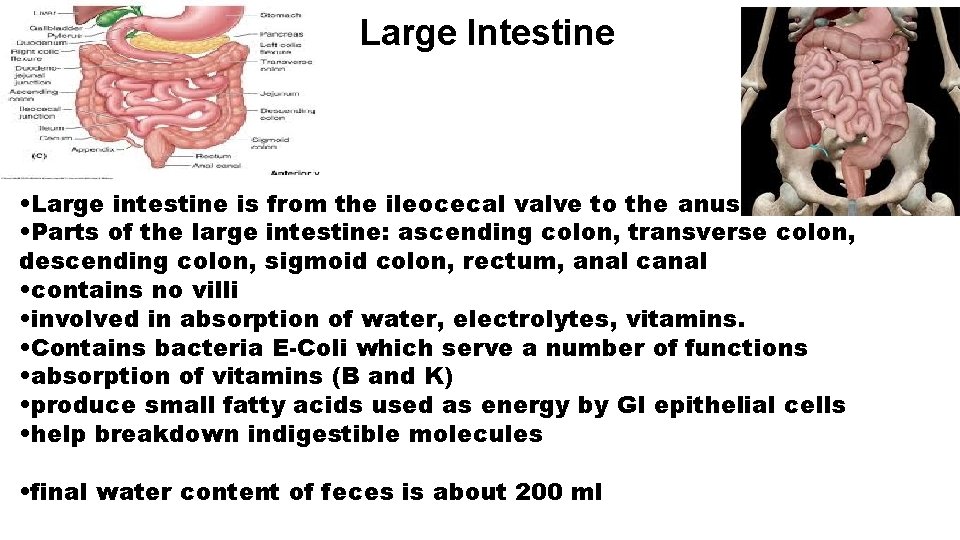
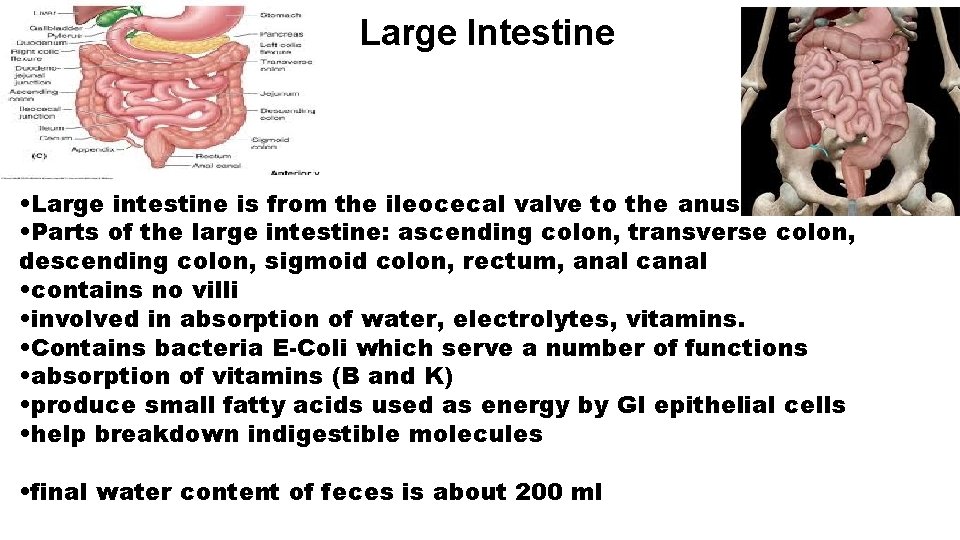
Large Intestine • Large intestine is from the ileocecal valve to the anus • Parts of the large intestine: ascending colon, transverse colon, descending colon, sigmoid colon, rectum, anal canal • contains no villi • involved in absorption of water, electrolytes, vitamins. • Contains bacteria E-Coli which serve a number of functions • absorption of vitamins (B and K) • produce small fatty acids used as energy by GI epithelial cells • help breakdown indigestible molecules • final water content of feces is about 200 ml
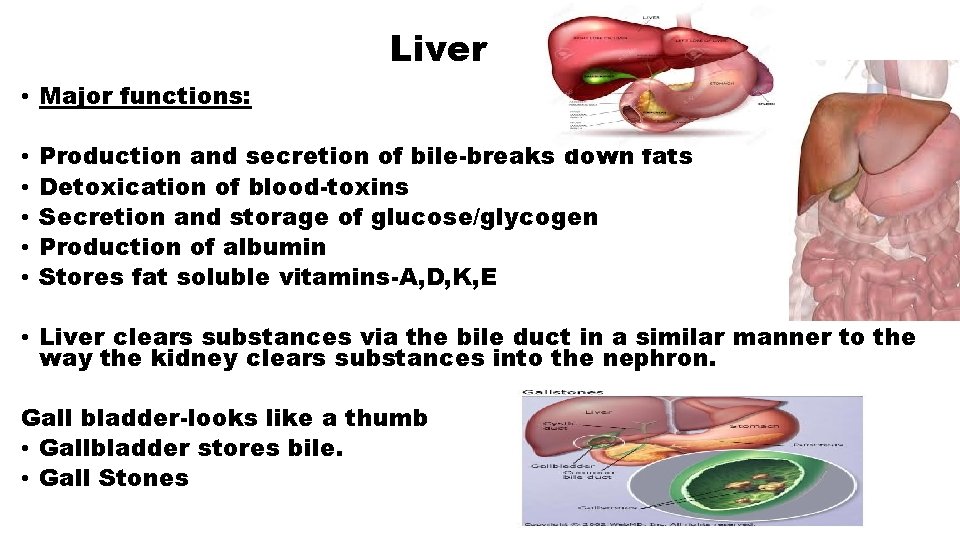
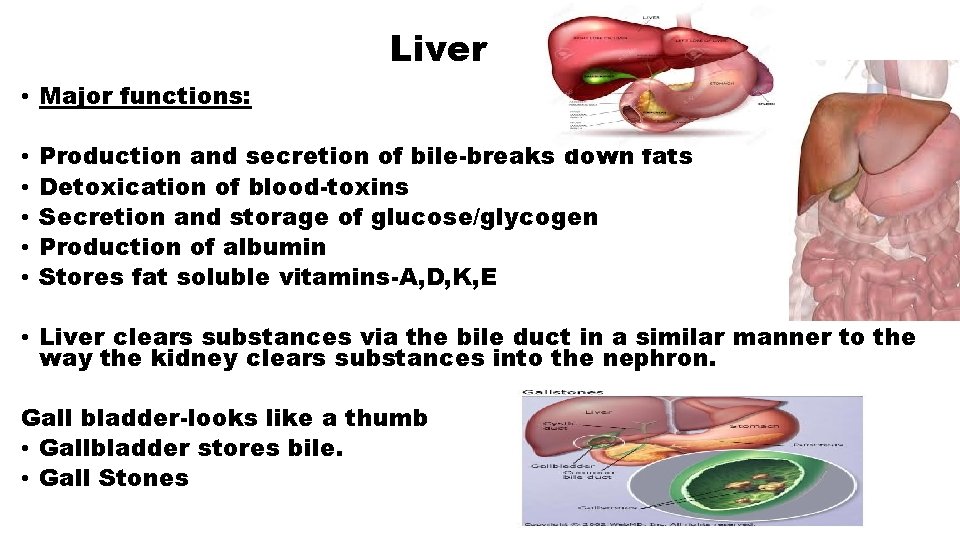
Liver • Major functions: • • • Production and secretion of bile-breaks down fats Detoxication of blood-toxins Secretion and storage of glucose/glycogen Production of albumin Stores fat soluble vitamins-A, D, K, E • Liver clears substances via the bile duct in a similar manner to the way the kidney clears substances into the nephron. Gall bladder-looks like a thumb • Gallbladder stores bile. • Gall Stones
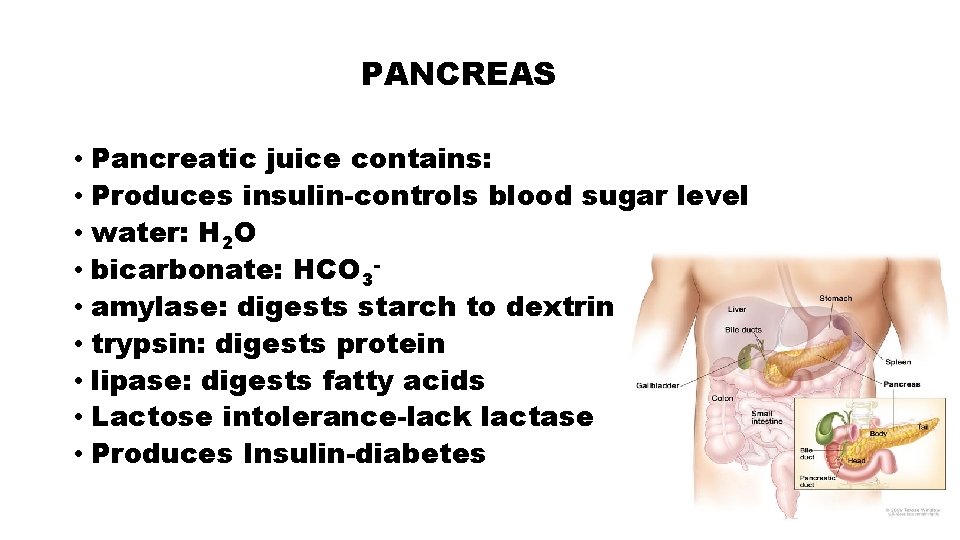
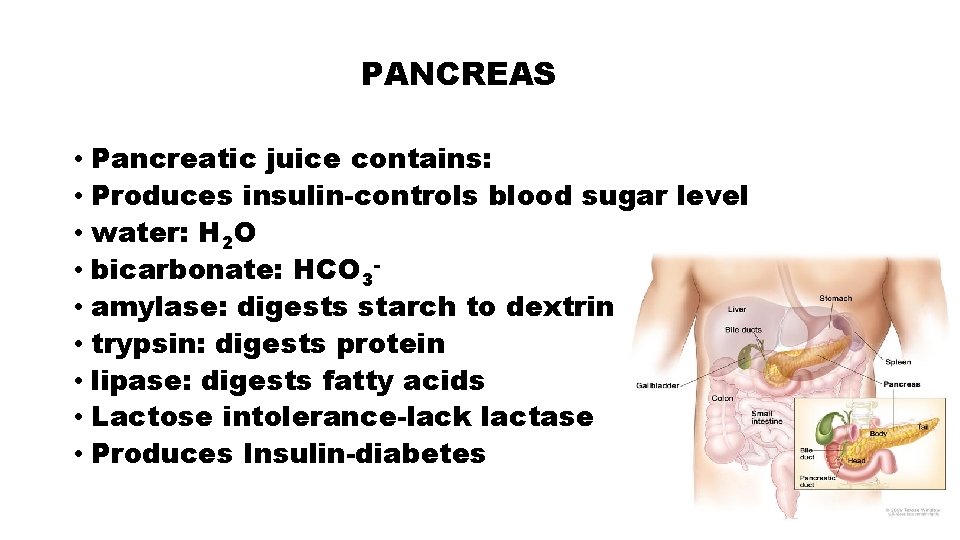
PANCREAS • Pancreatic juice contains: • Produces insulin-controls blood sugar level • water: H 2 O • bicarbonate: HCO 3 • amylase: digests starch to dextrin • trypsin: digests protein • lipase: digests fatty acids • Lactose intolerance-lack lactase • Produces Insulin-diabetes
Enzymes Chemicals that breakdown food into simpler form • Pepsin- Converts proteins to peptones and proteoses • Trypsin-Changes proteins to peptones and proteoses to peptids • Erepsin-Changes peptids to amino acids • Lipase-changes fats to fatty acids and glycerin • Amylase-changes starch and dextrin to maltose • Maltase-Changes maltose to glucose • Sucrase-changes sugar to glucose and fructose • Lactase-changes lactose to glucose and galactose
• Gastritis-inflammation of the stomach. drinking excessive amounts of alcohol, vomiting repetitively, prolonged stress, or taking certain types of medications that can damage the stomach, such as aspirin, narcotic pills. Gastritis can also be caused by a type of bacteria known as Helicobacter pylori-bacteria in the stomach. • Hemorrhoids-inflammation of the rectum and or anus area-blood vessels. The veins around your anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from increased pressure in the lower rectum. Hemorrhoids are more likely with aging because the tissues that support the veins in your rectum and anus can weaken and stretch. • Hernia-intestine protrudes through the abdominal wall Anything that causes an increase in pressure in the abdomen cause a hernia, including: Lifting heavy objects without stabilizing the abdominal muscles. Diarrhea or constipation. Persistent coughing or sneezing. • Ulcers-“bacteria” breaking down the mucin layer in the stomach exposing the inner layermucosa layer of the stomach. Mucus in the stomach functions as a buffer between the stomach acid and the tissue in the stomach. When this mucus stops working the acid comes directly into contact with the lining and causes the issue with the lining and the intestine. Ulcers generally are not caused by stress and diet, but these two factors can aggravate an existing ulcer. Additionally, stress can raise a person’s risk factors for an ulcer. Some ulcers occur as a result of bacterial infection.
Hepatitis-viral infections of the liver A & B & C (itis=Inflammation) Body fluids of infected person, “A”-raw sewage, infected person not washing hands whom is a carrier, “C”-needle use-addicts. Most contact travelling out the US. Diarrhea-liquid state of waste-feces. Food poisoning, food allergy, food intolerance, Irritable Bowel Syndrome-Crohn’s disease and ulcerative colitis, Celiac Disease, Medications others. Constipation-solid state of the waste-feces. Lack of water intake, diets are lacking in adequate fiber, if we don’t exercise, if we smoke, or if we drink to excess, painkillers and antidepressants Acid Reflux-value at the end of the esophagus-food, gastric juices, HCl, back washes into the esophagus. Colitis-Irritable bowel syndrome-IBS Irritable bowel syndrome-Spastic colon spontaneous contractions or loss of movement of the muscles in the small and large intestines Abdominal bloating, cramping abdominal, pain, constipation, diarrhea.
Disorders: • Crohn’s Disease • Causes: unknown Environmental, genetics, overactive immune system • Chronic inflammation bowel disease (IBD) • Effects especially the last part of the small intestine, but can affect from mouth to anus area. • Age 15 -35 700, 00 people in US • Symptoms: Flare up Diagnosis: • Abdominal pain blood test • Diarrhea stool test • Fever video capsule endoscopy • Weight loss barium x-ray • Vomiting • Dehydration Treatment: Diet/Medication Seler a/Humira
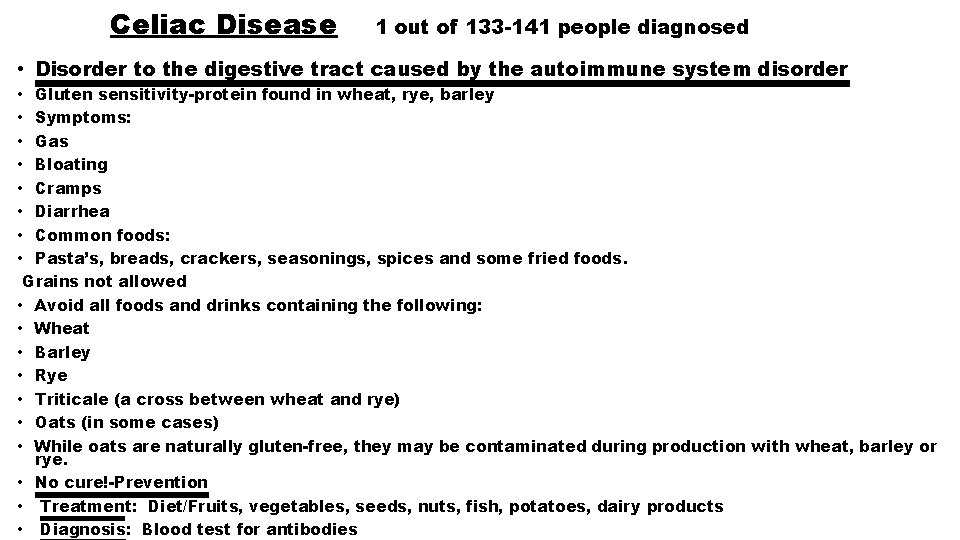
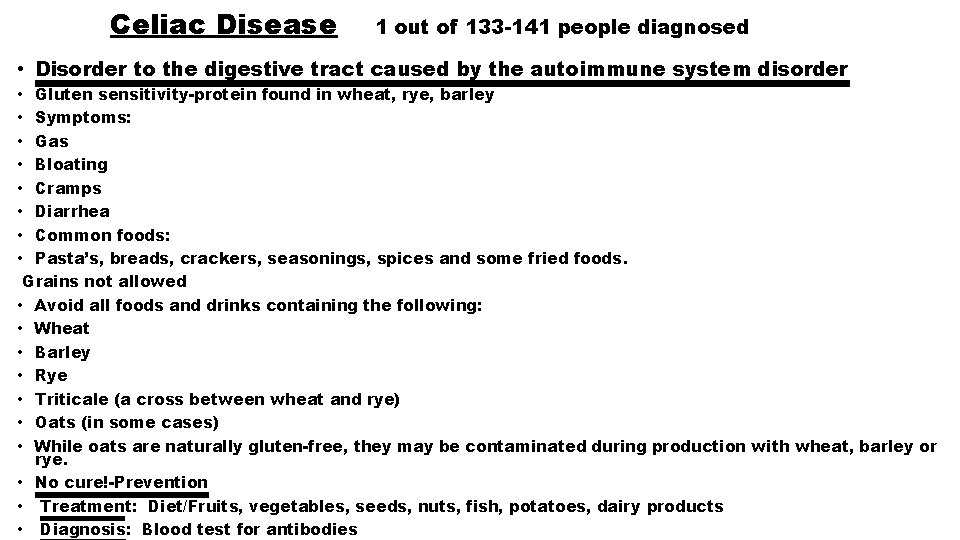
Celiac Disease 1 out of 133 -141 people diagnosed • Disorder to the digestive tract caused by the autoimmune system disorder • Gluten sensitivity-protein found in wheat, rye, barley • Symptoms: • Gas • Bloating • Cramps • Diarrhea • Common foods: • Pasta’s, breads, crackers, seasonings, spices and some fried foods. Grains not allowed • Avoid all foods and drinks containing the following: • Wheat • Barley • Rye • Triticale (a cross between wheat and rye) • Oats (in some cases) • While oats are naturally gluten-free, they may be contaminated during production with wheat, barley or rye. • No cure!-Prevention • Treatment: Diet/Fruits, vegetables, seeds, nuts, fish, potatoes, dairy products • Diagnosis: Blood test for antibodies
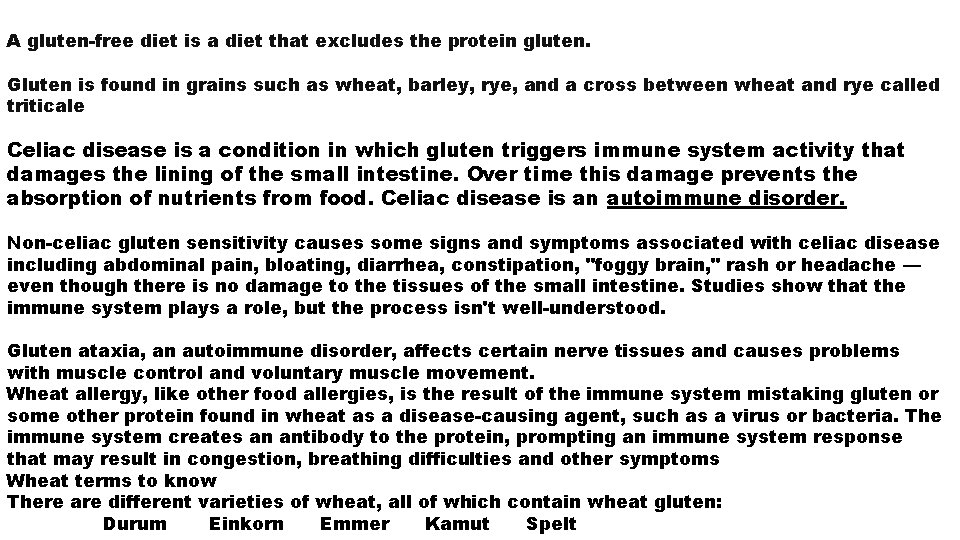
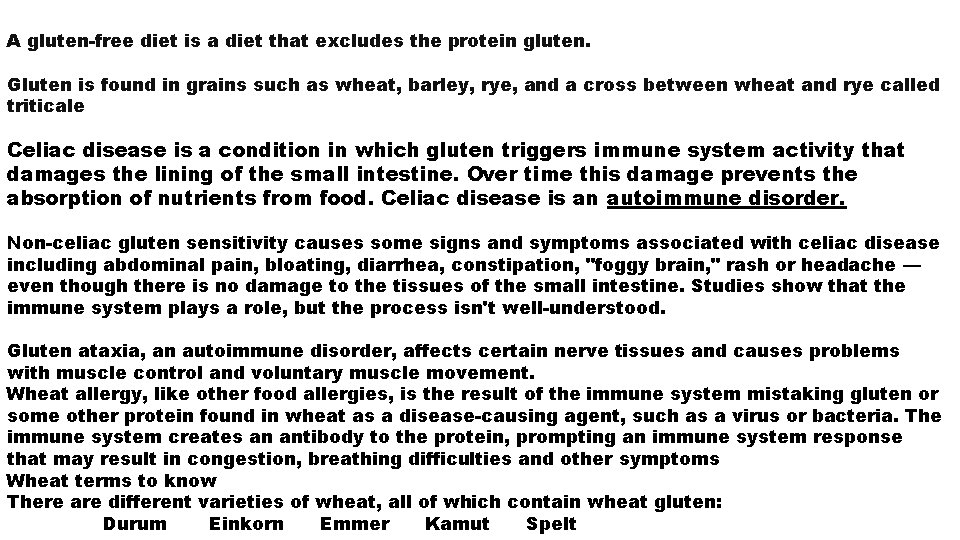
A gluten-free diet is a diet that excludes the protein gluten. Gluten is found in grains such as wheat, barley, rye, and a cross between wheat and rye called triticale Celiac disease is a condition in which gluten triggers immune system activity that damages the lining of the small intestine. Over time this damage prevents the absorption of nutrients from food. Celiac disease is an autoimmune disorder. Non-celiac gluten sensitivity causes some signs and symptoms associated with celiac disease including abdominal pain, bloating, diarrhea, constipation, "foggy brain, " rash or headache — even though there is no damage to the tissues of the small intestine. Studies show that the immune system plays a role, but the process isn't well-understood. Gluten ataxia, an autoimmune disorder, affects certain nerve tissues and causes problems with muscle control and voluntary muscle movement. Wheat allergy, like other food allergies, is the result of the immune system mistaking gluten or some other protein found in wheat as a disease-causing agent, such as a virus or bacteria. The immune system creates an antibody to the protein, prompting an immune system response that may result in congestion, breathing difficulties and other symptoms Wheat terms to know There are different varieties of wheat, all of which contain wheat gluten: Durum Einkorn Emmer Kamut Spelt
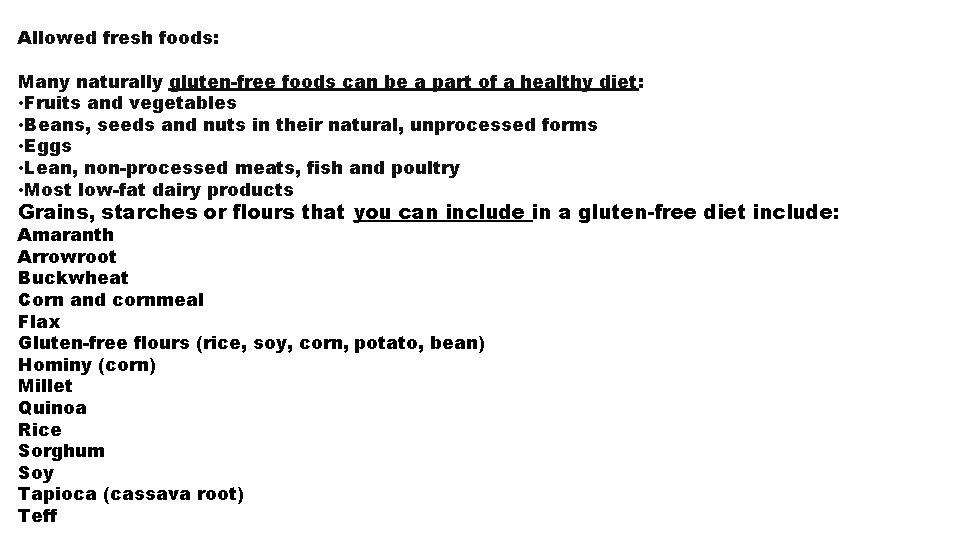
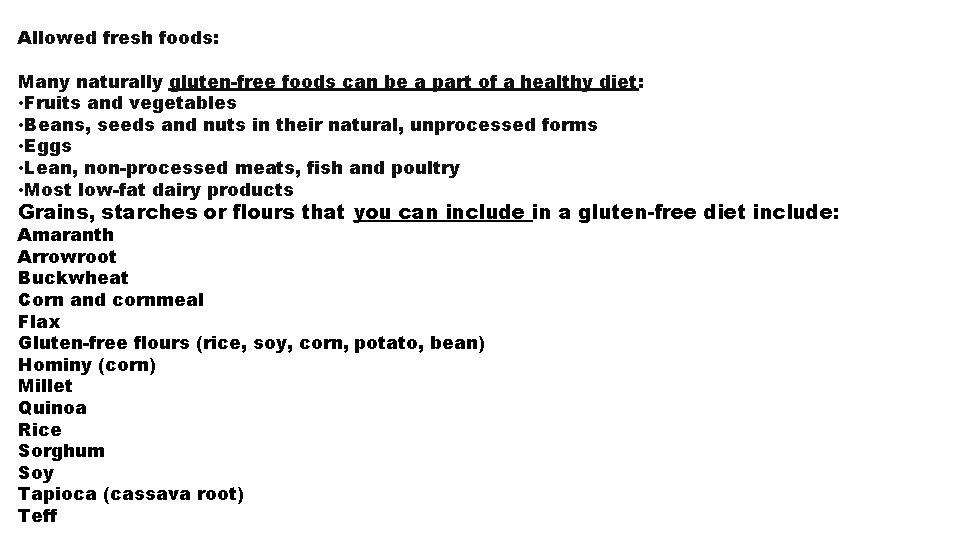
Allowed fresh foods: Many naturally gluten-free foods can be a part of a healthy diet: • Fruits and vegetables • Beans, seeds and nuts in their natural, unprocessed forms • Eggs • Lean, non-processed meats, fish and poultry • Most low-fat dairy products Grains, starches or flours that you can include in a gluten-free diet include: Amaranth Arrowroot Buckwheat Corn and cornmeal Flax Gluten-free flours (rice, soy, corn, potato, bean) Hominy (corn) Millet Quinoa Rice Sorghum Soy Tapioca (cassava root) Teff
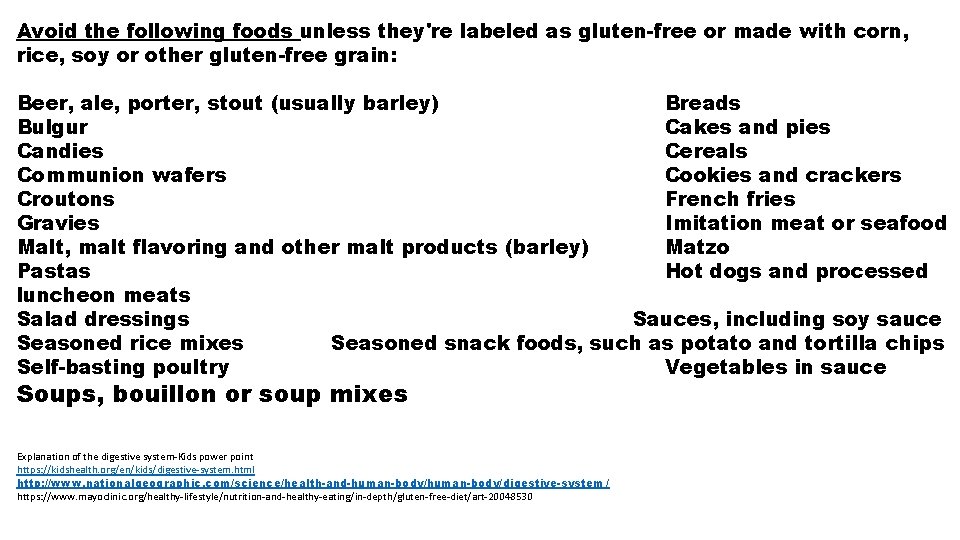
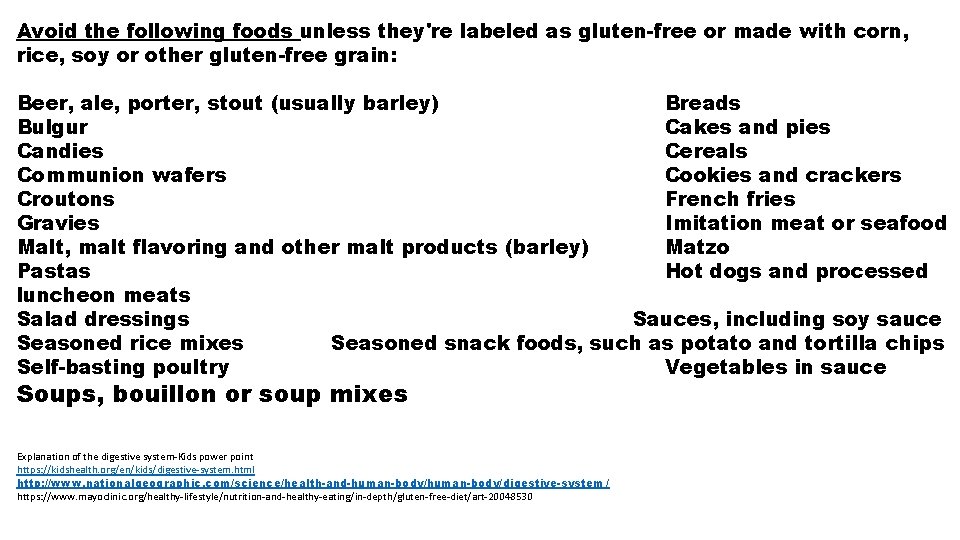
Avoid the following foods unless they're labeled as gluten-free or made with corn, rice, soy or other gluten-free grain: Beer, ale, porter, stout (usually barley) Breads Bulgur Cakes and pies Candies Cereals Communion wafers Cookies and crackers Croutons French fries Gravies Imitation meat or seafood Malt, malt flavoring and other malt products (barley) Matzo Pastas Hot dogs and processed luncheon meats Salad dressings Sauces, including soy sauce Seasoned rice mixes Seasoned snack foods, such as potato and tortilla chips Self-basting poultry Vegetables in sauce Soups, bouillon or soup mixes Explanation of the digestive system-Kids power point https: //kidshealth. org/en/kids/digestive-system. html http: //www. nationalgeographic. com/science/health-and-human-body/digestive-system / https: //www. mayoclinic. org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gluten-free-diet/art-20048530
Colorectal Cancer • Colorectal cancer is cancer that occurs in the colon or rectum. Sometimes it is called colon cancer, for short. • As the drawing shows, the colon is the large intestine or large bowel. The rectum is the passageway that connects the colon to the anus. • Sometimes abnormal growths, called polyps, form in the colon or rectum. • Over time, some polyps may turn into cancer. • Screening tests can find polyps so they can be removed before turning into cancer. • Screening also helps find colorectal cancer at an early stage, when treatment works best. https: //www. cdc. gov/cancer/colorectal/basic_info/what-is-colorectal-cancer. htm
Risk Of Getting Colorectal Cancer • Your risk of getting colorectal cancer increases as you get older. • More than 90% of cases occur in people who are 50 years old or older. • Other risk factors include having: • Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis. • A personal or family history of colorectal cancer or colorectal polyps. • A genetic syndrome such as familial adenomatous polyposis (FAP) external icon or Hereditary non polyposis • Colorectal Cancer-Lynch Syndrome • Lifestyle Factors that may contribute to an increased risk: • • • Lack of regular physical activity A diet low in fruit and vegetables. A low-fiber and high-fat diet, or a diet high in processed meats. Overweight and obesity Alcohol consumption Tobacco use
Risk Factors for Colon Cancer • Risk Factors People at increased risk for colorectal cancer may need to start screening at an earlier age and get tested more frequently than other people. • You may be at increased risk if: • You or a close relative had colorectal polyps or colorectal cancer. • You have inflammatory bowel disease, Crohn’s disease, or ulcerative colitis. • You have certain genetic syndromes, like familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (also known as Lynch syndrome). • Getting screened for colorectal cancer as recommended can reduce your risk for developing this disease. Screening finds precancerous polyps so they can be removed before they turn into cancer. • If you are 50 or older, talk to your doctor about getting screened. • Symptoms Don’t wait for symptoms to be tested for colorectal cancer. • Precancerous polyps and early-stage colorectal cancer don’t always cause symptoms. But if there are symptoms, they may include: • Blood in or on your stool (bowel movement). • Pains, aches, or cramps in your stomach that do not go away. • Losing weight and you don’t know why. They may be caused by something other than cancer, but the only way to know is to see your doctor. • If you have any of these symptoms, talk to your doctor. • https: //www. cdc. gov/cancer/colorectal/basic_info/risk_factors. htm
Colon Cancer Tests • Stool Tests • The guaiac-based fecal occult blood test (g. FOBT) uses the chemical guaiac to detect blood in the stool. It is done once a year. For this test, you receive a test kit from your health care provider. At home, you use a stick or brush to obtain a small amount of stool. You return the test kit to the doctor or a lab, where the stool samples are checked for the presence of blood. • The fecal immunochemical test (FIT) uses antibodies to detect blood in the stool. It is also done once a year in the same way as a g. FOBT. • The FIT-DNA test (also referred to as the stool DNA test) combines the FIT with a test that detects altered DNA in the stool. For this test, you collect an entire bowel movement and send it to a lab, where it is checked for cancer cells. It is done once every one or three years. • Flexible Sigmoidoscopy • For this test, the doctor puts a short, thin, flexible, lighted tube into your rectum. The doctor checks for polyps or cancer inside the rectum and lower third of the colon. • How often: Every 5 years, or every 10 years with a FIT every year. • Colonoscopy • This is similar to flexible sigmoidoscopy, except the doctor uses a longer, thin, flexible, lighted tube to check for polyps or cancer inside the rectum and the entire colon. During the test, the doctor can find and remove most polyps and some cancers. Colonoscopy also is used as a follow-up test if anything unusual is found during one of the other screening tests. • How often: Every 10 years (for people who do not have an increased risk of colorectal cancer). • CT Colonography (Virtual Colonoscopy) • Computed tomography (CT) colonography, also called a virtual colonoscopy, uses X-rays and computers to produce images of the entire colon, which are displayed on a computer screen for the doctor to analyze. • How often: Every 5 years.
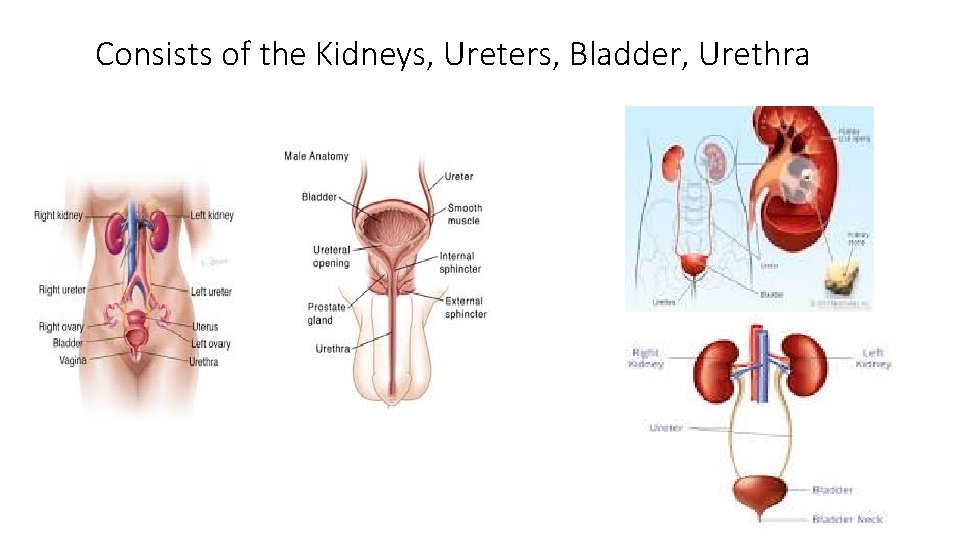
Urinary System What are the 5 Purposes of the Urinary System? • The urinary system, also known as the renal system or urinary tract. Consists of the kidneys, ureters, bladder, and the urethra. • The purpose of the urinary system is to: 1. Eliminate waste from the body 2. Regulate blood volume 3. Regulate blood pressure 4. Control levels of electrolytes and metabolites 5. Regulate blood p. H
The Four Main Functions Of The Urinary System 1. Filtration of the blood 750 -1, 000 pints filtered per day 120 pints per hour 2. Secretion-3 -4 pints per day 3. Reabsorption 4. Removal of Toxins a. Urea b. Ammonia c. Drugs d. Other toxins from the body
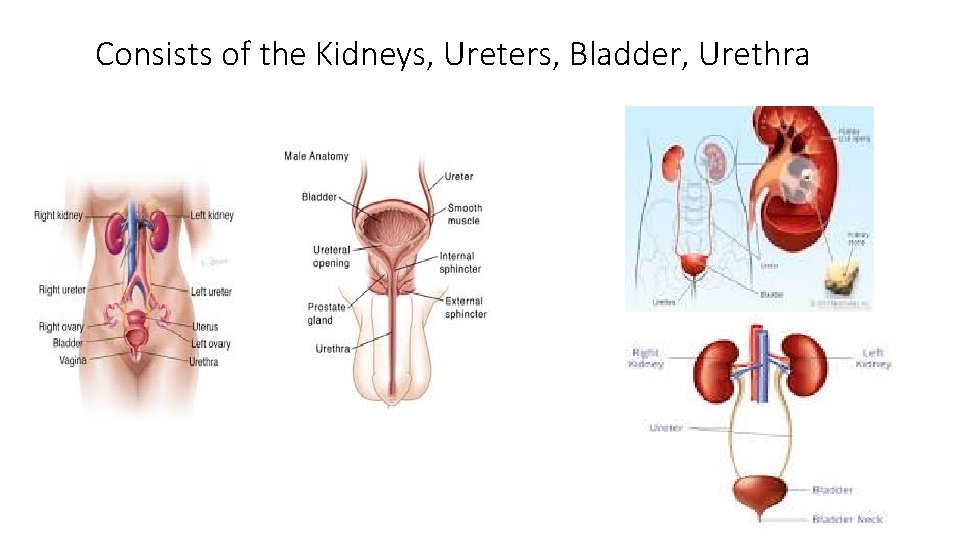
Consists of the Kidneys, Ureters, Bladder, Urethra
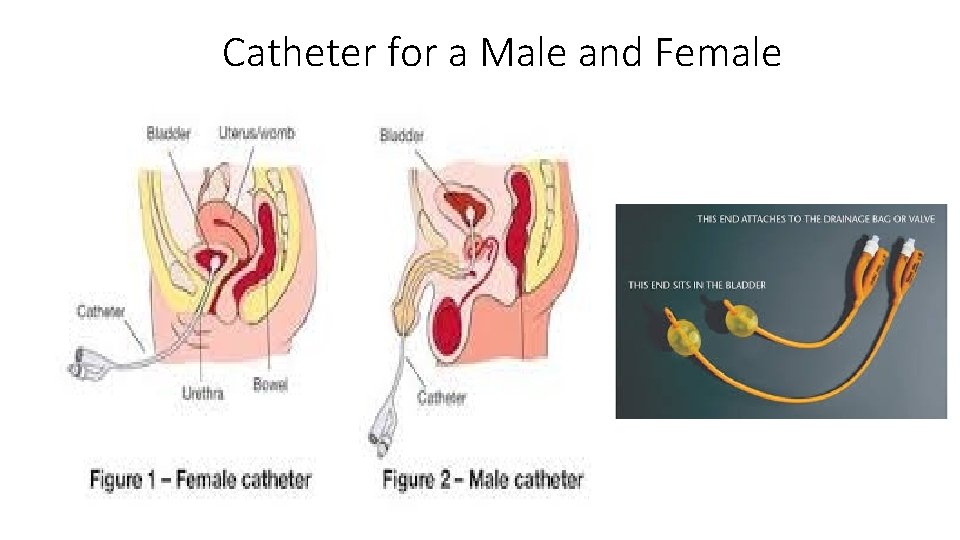
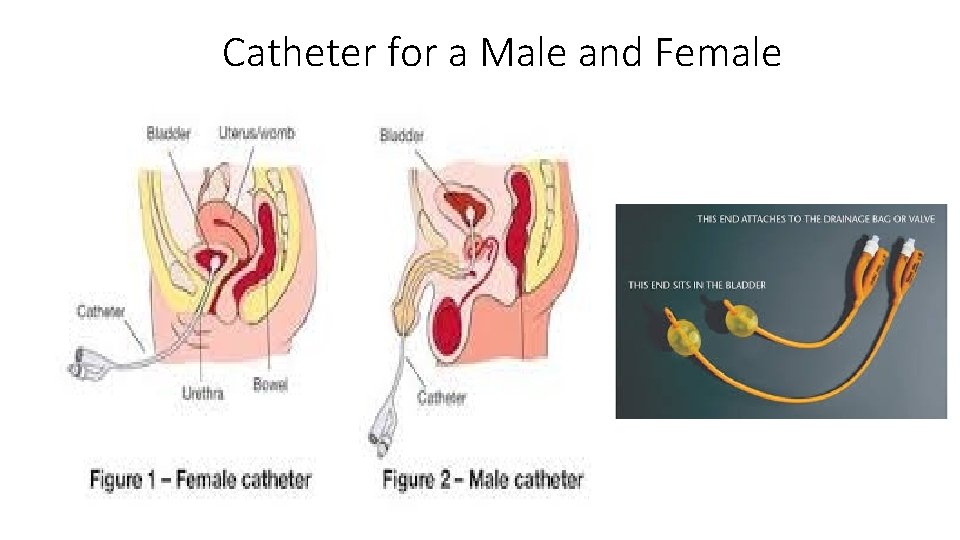
Catheter for a Male and Female