Digestion is the change of complex food substances
Ü Digestion is the change of complex food substances into a simpler form to be absorbed. Basic digestive processes: 4 process [1] Motility: Ü To mix & move forward the contents along the digestive tract [2] Secretion: Ü of Ø Ø Enzymes Mucous electrolytes & H 2 O Ü From Ø Salivary glands Ø Gastric glands Ø Intestinal glands Ø Pancreas Ø Liver Ü Accessory digestive system Ø Salivary glands Ø Liver Ø G. B. Ø Exocrine Ø Pancreas.

![[3] Digestion: Ü Breakdown of complex food substances of diet into simple Units to [3] Digestion: Ü Breakdown of complex food substances of diet into simple Units to](http://slidetodoc.com/presentation_image/544690dd4bcfd5a2f1c78f565d905218/image-3.jpg)
[3] Digestion: Ü Breakdown of complex food substances of diet into simple Units to be absorbed. Ø Proteins amino-acids Ø Fatty acids + Glycerol Ø Carbohydrate glucose [4] Absorption: Ü Transfer of the small digested units from G. I. T. into blood or lymph.
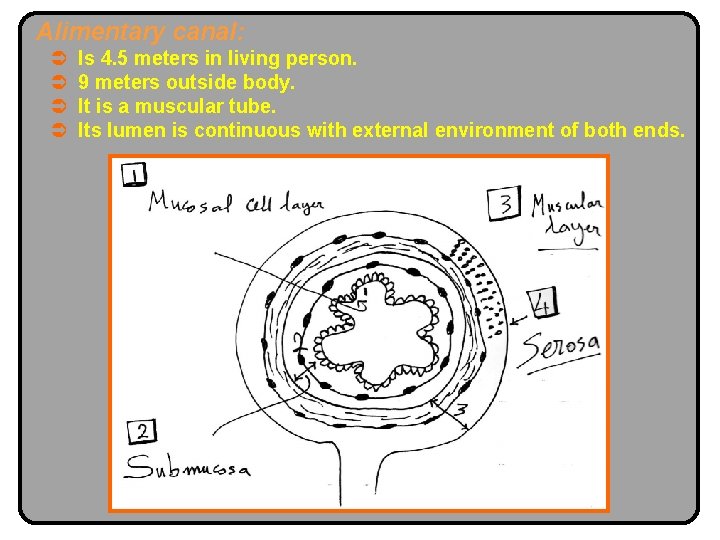
Alimentary canal: Ü Ü Is 4. 5 meters in living person. 9 meters outside body. It is a muscular tube. Its lumen is continuous with external environment of both ends.
1. Mucosal cell layer: Ü Its surface is folded with ridges & valleys to surface area. Ü Contains exocrine cells for secretion of enzymes & mucous. Ü Contains endocrine cells for secretion of hormones. 2. Submucosal layer: Ü Contains Ø Ø Ø Blood & lymph vessels. Connective tissue. Meissners plexus.

3. Muscular layer: Ü Inner Ü Ü Circular. to constrict diameter. Outer Longitudinal. to shorten length. In between Myentric plexus. = Auerbach’s plexus. Myenteric plexus is connected to Meissner’s plexus. Function: Propulsive & mixing movements. 4. Serosal layer: Ü Outer covering of G. I. T. to prevent friction with viscera exception: esophagus & distal rectum. Muscles of G. I. T. is Smooth except( i. e. striated): 1. Pharynx. 2. Upper 1/3 of esophagus. 3. External anal sphincter. Ü Middle 1/3 of esoph. is mixed. Ü Lower 1/3 is smooth.
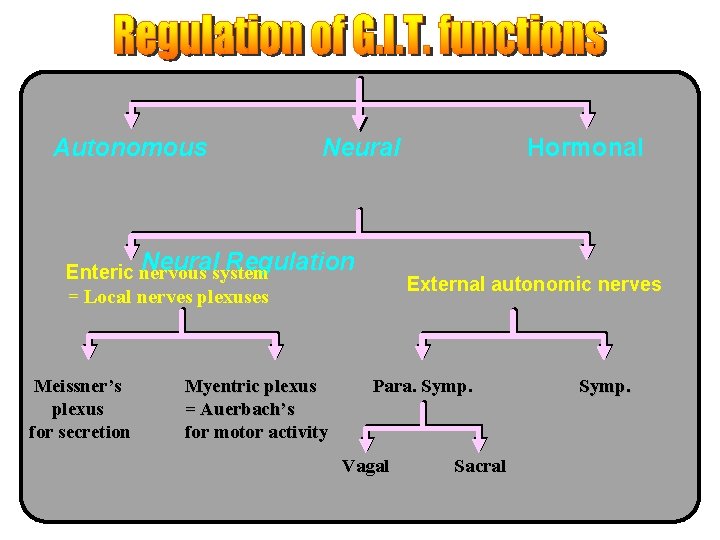
Autonomous Neuralsystem Regulation Enteric nervous = Local nerves plexuses Meissner’s plexus for secretion Myentric plexus = Auerbach’s for motor activity Hormonal External autonomic nerves Para. Symp. Vagal Sacral Symp.
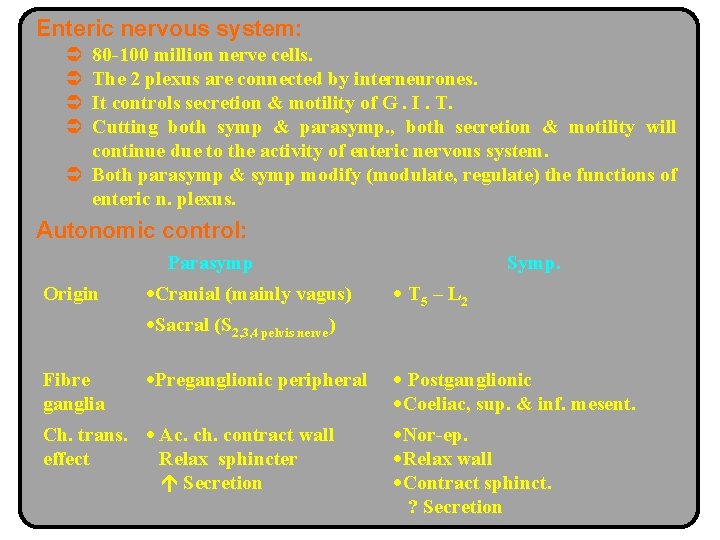
Enteric nervous system: Ü Ü 80 -100 million nerve cells. The 2 plexus are connected by interneurones. It controls secretion & motility of G. I. T. Cutting both symp & parasymp. , both secretion & motility will continue due to the activity of enteric nervous system. Ü Both parasymp & symp modify (modulate, regulate) the functions of enteric n. plexus. Autonomic control: Parasymp Origin Cranial (mainly vagus) Symp. T 5 – L 2 Sacral (S 2, 3, 4 pelvis nerve) Fibre ganglia Preganglionic peripheral Ch. trans. Ac. ch. contract wall effect Relax sphincter Secretion Postganglionic Coeliac, sup. & inf. mesent. Nor-ep. Relax wall Contract sphinct. ? Secretion
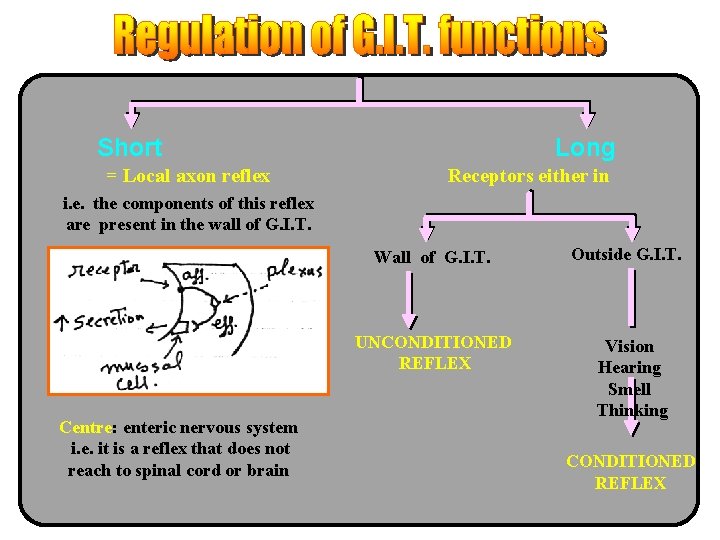
Short = Local axon reflex Long Receptors either in i. e. the components of this reflex are present in the wall of G. I. T. Wall of G. I. T. UNCONDITIONED REFLEX Centre: enteric nervous system i. e. it is a reflex that does not reach to spinal cord or brain Outside G. I. T. Vision Hearing Smell Thinking CONDITIONED REFLEX
![Types of Receptors in G. I. T. [1] Chemoreceptors [2] Mechanoreceptors [3] Osmoreceptors i. Types of Receptors in G. I. T. [1] Chemoreceptors [2] Mechanoreceptors [3] Osmoreceptors i.](http://slidetodoc.com/presentation_image/544690dd4bcfd5a2f1c78f565d905218/image-11.jpg)
Types of Receptors in G. I. T. [1] Chemoreceptors [2] Mechanoreceptors [3] Osmoreceptors i. e. receptors sensitive to chemical stimuli e. g. Acid (HCL), glucose, aminoacids, Fatty acids (Pressure receptors) Sensitive to distension (Stretch) Sensitive To Osmolality inside G. I. T. e. g. Hypertonic, Hypotonic solutions Neural Supply to bl. vessels of GIT: [1] No direct [2] Symp. [3] Enteric n. system Cholinergic fibres to splanchnic bl. v. N. B. : Parasymp. secretion end products of metabolism V. D. i. e. indirect nor-ep. VIP V. D. V. C.
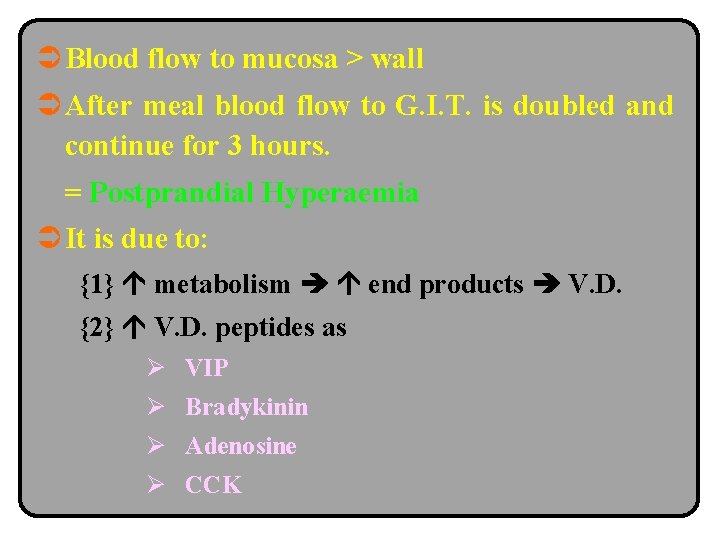
Ü Blood flow to mucosa > wall Ü After meal blood flow to G. I. T. is doubled and continue for 3 hours. = Postprandial Hyperaemia Ü It is due to: {1} metabolism end products V. D. {2} V. D. peptides as Ø VIP Ø Bradykinin Ø Adenosine Ø CCK
Ü All G. I. T. hormones are Polypeptides. Ü These hormones are secreted from mucosal cells called APUD cells. ( Amine Precursor Uptake & Decarboxylation. ) these cells can take up amine precursor and decarboxylate them. Ü These hormones will circulate in blood. Ü These hormones affect ( or ) both secretion & motility of G. I. T. Ü These hormones are released in response. Ü To 1. External autonomic nerves. 2. Enteric nervous system. Ü N. B. : Some hormones may act. Locally i. e. not pass to blood i. e. affected nearby cells. = Paracrine secretion.
Site of Release: 1. G-cells in mucosa of antrum of stomach. 1. TG cells in mucosa of Ø Stomach. Ø Duodenum. Mechanism: Local axons reflex. 2. Stimuli for release: 1. Products of proteins as peptides & a-a in stomach & duodenum. 2. Distension of the antrum of stomach & duodenum 3. vagal discharge Ü The chemical transmitter is GRP not ac. ch. Ü GRP i. e. gastrin releasing peptide. Ü N. B. : Atropine does not prevent gastrin release Hcl gastrin release by direct effect on G-cells.
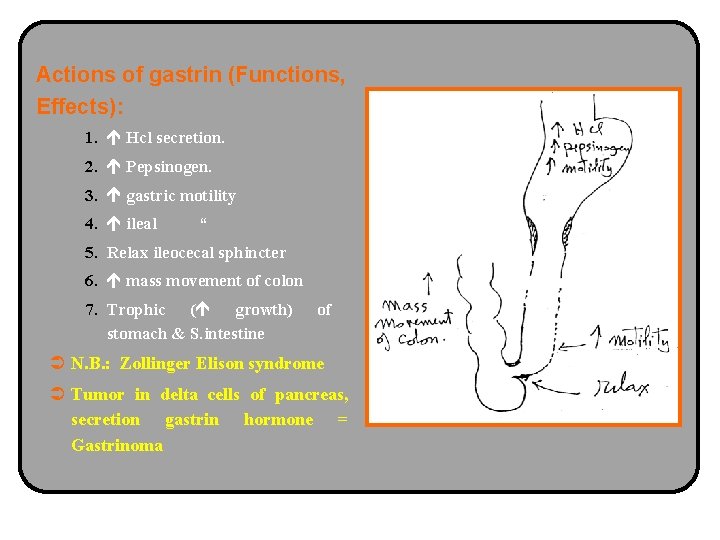
Actions of gastrin (Functions, Effects): 1. Hcl secretion. 2. Pepsinogen. 3. gastric motility 4. ileal “ 5. Relax ileocecal sphincter 6. mass movement of colon 7. Trophic ( growth) stomach & S. intestine of Ü N. B. : Zollinger Elison syndrome Ü Tumor in delta cells of pancreas, secretion gastrin hormone = Gastrinoma
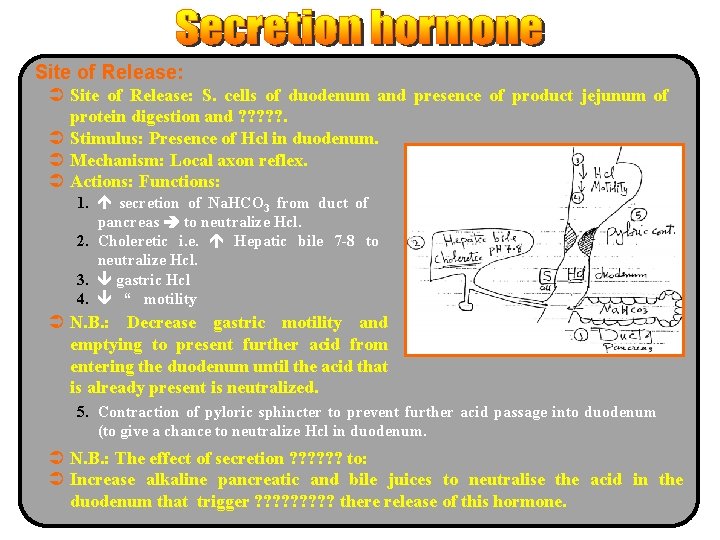
Site of Release: Ü Site of Release: S. cells of duodenum and presence of product jejunum of protein digestion and ? ? ? . Ü Stimulus: Presence of Hcl in duodenum. Ü Mechanism: Local axon reflex. Ü Actions: Functions: 1. secretion of Na. HCO 3 from duct of pancreas to neutralize Hcl. 2. Choleretic i. e. Hepatic bile 7 -8 to neutralize Hcl. 3. gastric Hcl 4. “ motility Ü N. B. : Decrease gastric motility and emptying to present further acid from entering the duodenum until the acid that is already present is neutralized. 5. Contraction of pyloric sphincter to prevent further acid passage into duodenum (to give a chance to neutralize Hcl in duodenum. Ü N. B. : The effect of secretion ? ? ? to: Ü Increase alkaline pancreatic and bile juices to neutralise the acid in the duodenum that trigger ? ? ? ? ? there release of this hormone.
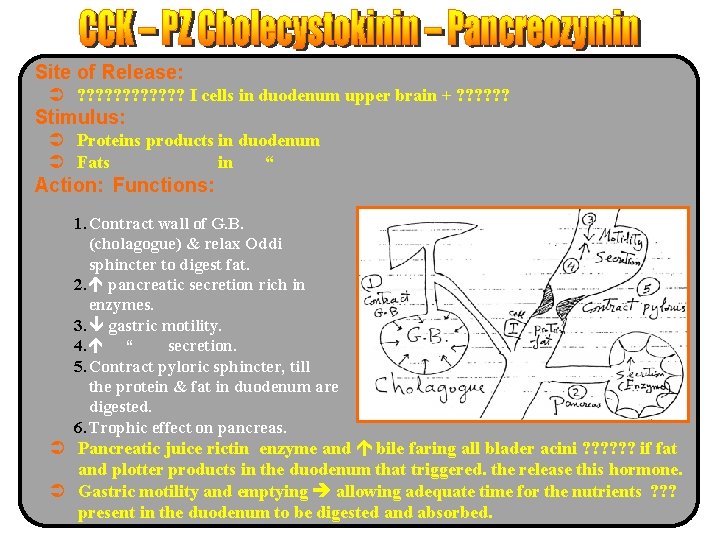
Site of Release: Ü ? ? ? I cells in duodenum upper brain + ? ? ? Stimulus: Ü Proteins products in duodenum Ü Fats in “ Action: Functions: 1. Contract wall of G. B. (cholagogue) & relax Oddi sphincter to digest fat. 2. pancreatic secretion rich in enzymes. 3. gastric motility. 4. “ secretion. 5. Contract pyloric sphincter, till the protein & fat in duodenum are digested. 6. Trophic effect on pancreas. Ü Pancreatic juice rictin enzyme and bile faring all blader acini ? ? ? if fat and plotter products in the duodenum that triggered. the release this hormone. Ü Gastric motility and emptying allowing adequate time for the nutrients ? ? ? present in the duodenum to be digested and absorbed.
- Slides: 17