Digestion and absorption Digestion Breakdown of large foodstuff
Digestion and absorption
Digestion • Break-down of large foodstuff – All components of food • Carbohydrates • Proteins • Fats – Monomer level – Process • Mechanical • Chemical
Absorption • Amount of absorption – Ingestion (1. 5 L) plus secretion (7 L) • 83 % absorbed in the small intestine • Site of absorption – Stomach • Very poor – No absorptive villi/membrane – Large intestine • Proximal half • Water and electrolytes
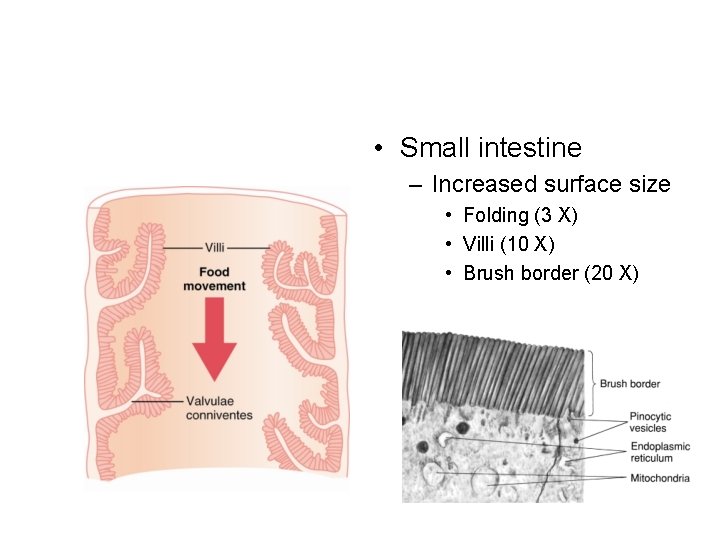
• Small intestine – Increased surface size • Folding (3 X) • Villi (10 X) • Brush border (20 X)

• Villus – Adaptation for increased nutrient absorption • Vasculature • Lymph vessel • Constant movement of microvilli
Hydrolysis • Universal process – Break down of large molecules by addition of water • Break of the polymers into smaller fragments – Break bonds – Process • Different enzymes based on the macromolecule
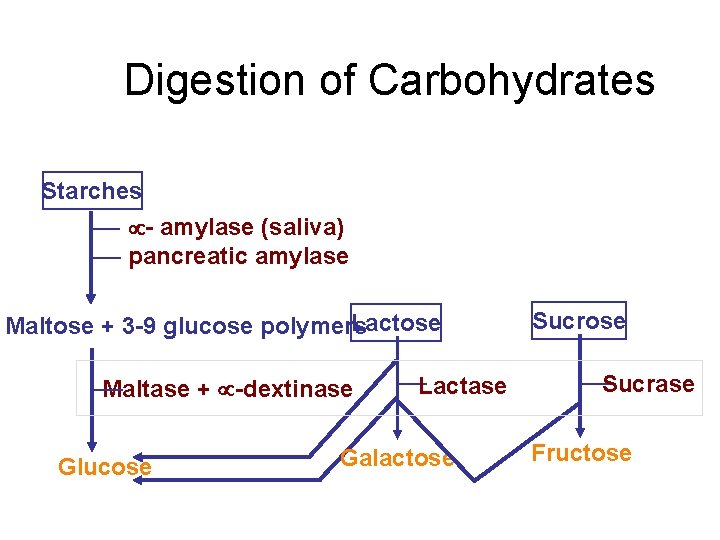
Digestion of Carbohydrates Starches - amylase (saliva) pancreatic amylase Lactose Maltose + 3 -9 glucose polymers Maltase + -dextinase Glucose Lactase Galactose Sucrase Fructose
• Location of digestion – Mouth • 5 % of all starches – Stomach • Inhibition of amylase activity (too acidic) • 30 -40 % of starch converted to maltose – Small intestine • Amylase from pancreas • Enzymes on the enterocytes of villi
Absorption of carbohydrates • Glucose – 80 % of carbohydrates being absorbed – Secondary active transport • Sodium-glucose co-transporter – Use of sodium concentration gradient as an energy – Concentration gradient generated by removal of sodium from intestinal epithelium to the blood
• Other monosaccharides – Absorbed as they are – Converted to glucose
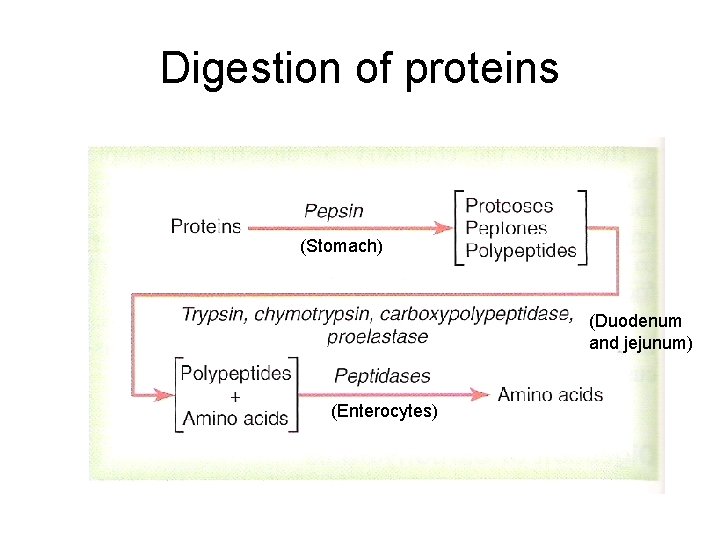
Digestion of proteins (Stomach) (Duodenum and jejunum) (Enterocytes)
Absorption of proteins • Individual amino acids – 99 % of final products of protein digestion – Transported via sodium-AA co-transporter • The same mechanism as glucose transport • Multiple transporter proteins to accommodate different amino acids – Some amino acids • Transported without co-transporters
Fat digestion • Dietary fats – Triglycerides • Majority – Phospholipids – Cholesterol • Site of digestion and absorption – Small intestine
• Process – Emulsification • Starts in the stomach • Majority takes place in the duodenum – Combination with bile products – Fragmentation of large molecules – Increased surface area
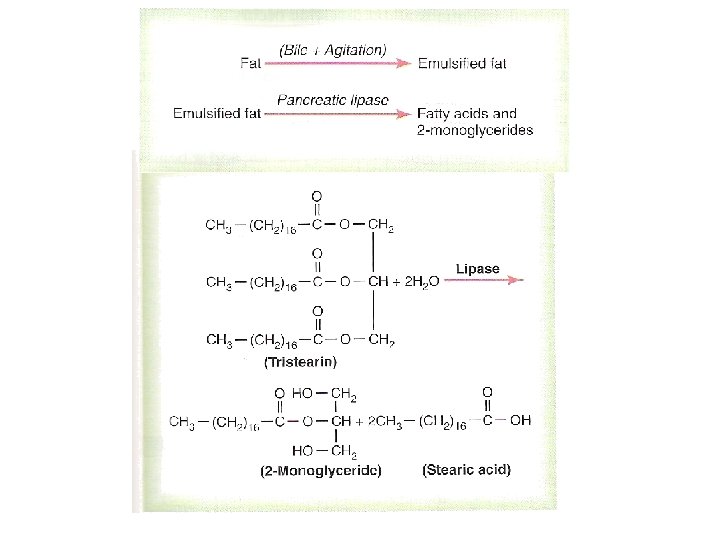
• Transport – Micelle • Cholesterol and phospholipids – Cholesterol esterase and phospholipase A 2
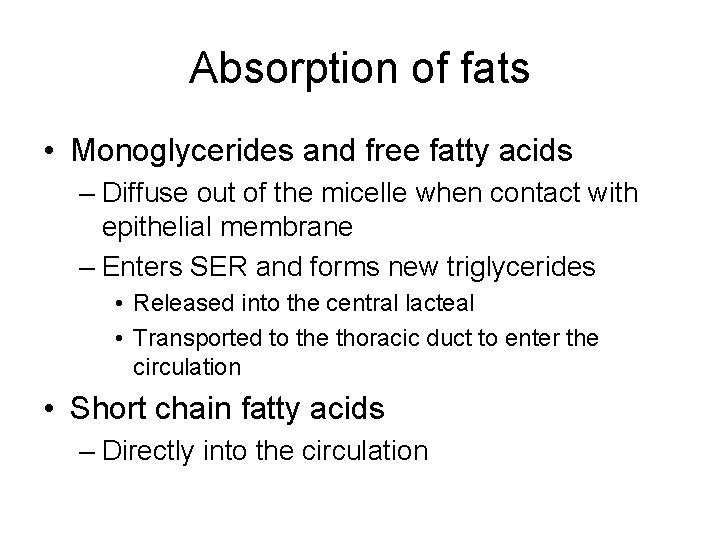
Absorption of fats • Monoglycerides and free fatty acids – Diffuse out of the micelle when contact with epithelial membrane – Enters SER and forms new triglycerides • Released into the central lacteal • Transported to the thoracic duct to enter the circulation • Short chain fatty acids – Directly into the circulation
Absorption of other materials • Water – Osmosis • Active transport – Calcium – Iron – Other ions
• Sodium ions – Active transport • Epithelium to paracellular spaces – Diffusion • From intestinal lumen to the epithelium – Increased by aldosterone
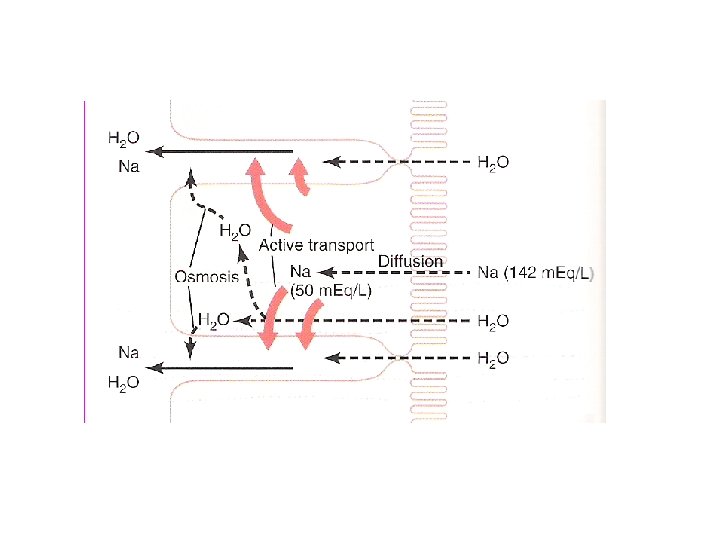
• Effects of sodium absorption – Increased chloride ion absorption – Increased osmosis – Secretion of hydrogen ions • Counter-transport • Formation of carbonic acid – CO 2 (dissolve in blood) – Water (excreted/reabsorved)
Absorption at the large intestine • Proximal half – Absorption • Sodium • Chloride • Water – Secretion • Bicarbonate ions – Counter-transport with chloride ions
• Feces – Dead bacteria (30 %) – Fat (10 -20 %) – Inorganic matter (10 -20 %) – Undigested plant matter (30 %) – Proteins (2 -3 %) – Metabolic waste (bilirubin metabolites)
Abnormalities • Esophagus – Swallowing problem – Entrance of food materials into the respiratory system • Closure of glottis – Entrance of food materials into the nasal cavity – Failure of lower sphincter to relax • Achalasia
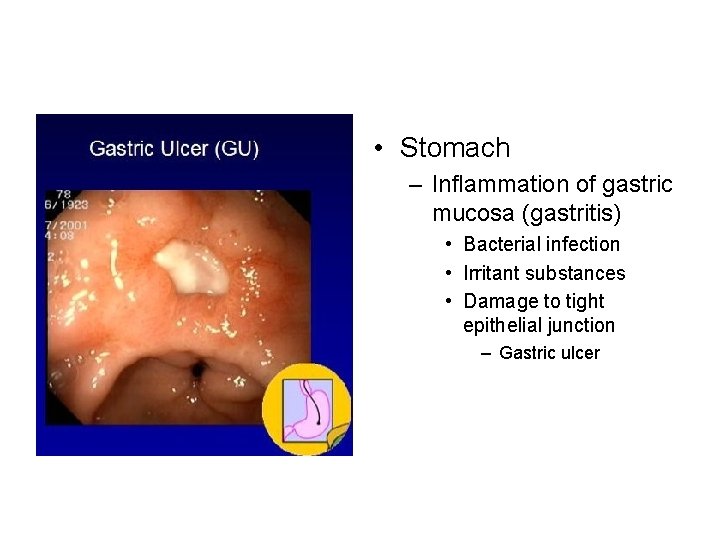
• Stomach – Inflammation of gastric mucosa (gastritis) • Bacterial infection • Irritant substances • Damage to tight epithelial junction – Gastric ulcer
• Gastric atrophy – Triggered by chronic gastritis – Loss of HCL secretion • Achlorohydria • Hypochlorohydria – Diminished secretion • Loss of pepsin function
Peptic ulcer • Imbalance between gastric secretion and gastric protection – Loss of mucosal barrier – Reduced acid neutralization – Excess gastric secretion • Causes – Chronic bacterial infections – Chemicals that increase gastric secretion and breakdown of mucosa
Small intestine • Loss of digestion – Pancreatitus • Excessive alcohol consumption – Blockage of ducts • Gallstone • Digestion of pancreas – Loss of pancreatic functions
• Malabsorption of nutrients – Spruce • Idiopathic – Gluten enteropathy • Inflammation caused by infection – Malabsorption • Lipids • Vitamin K, folic acid, and B 12 • Calcium
Large intestine • Constipation – Obstruction of intestinal passage – Irregular bowel habits – Spasm of a small segment within the sigmoid colon – Insufficient ganglions • Megacolon
• Diarrhea – Enteritis • Inflammation caused by infection – Irritation of mucosa – Excess secretion – Psychogenic • Excessive parasympathetic stimulation – Motility – Secretion

• Vomiting – Removal of materials from upper GI tract • Excessive irritation • Overdistention • Overexcitation – Sensory information • • Pharynx Esophagus Stomach Upper small intestine
• Nausea – Irritation impulse from the GI tract – Impulse from the lower brain associated with motion sickness – Impulse from the cerebral cortex to initiate vomiting – Excitation of medulla near the vomiting center
- Slides: 33