Diffuse arterial spasm in a young patient with

- Slides: 23
Diffuse arterial spasm in a young patient with Turner syndrome during Transcatheter Aortic Valve-in-Valve Replacement Sanchitha Guruchandrasekar, MBBS; Pedro Cox-Alomar, MD; Sylvia Oleck, MD; Steffan Sernich, MD; Kiran Mallula, MD

Disclosures • None
History • 24 yo F with Turner syndrome, h/o bicuspid aortic valve, aortic stenosis, coarctation of aorta • 1 month- Balloon valvuloplasty, coarctation repair • 4 years- Surgical bioprosthetic aortic valve replacement • 15 years- Aortic root replacement with 23 mm Magna-perimount valve and 26 mm Hemashield conduit, septal myectomy
History • Jehovah’s witnesses- bloodless surgeries • 17 years- Resection of arteriovenous malformation in the jejunum
Symptoms • Admitted for heart failure management • NYHA class III symptoms • Progressive shortness of breath • Orthopnea • Fatigue • Palpitations on exertion • Chest tightness on exertion
Investigations • NT-Pro. BNP- 17, 100 pg/ml TTE: • Severe aortic stenosis- Peak AV gradient 120 mm. Hg, mean AV gradient 80 mm. Hg • AVA- 0. 7 cm 2 (0. 4 cm 2/m 2) • Severe aortic insufficiency • Mild LV systolic dysfunction (EF 45 -50%)
Treatment options • Ross procedure • Surgical bioprosthetic aortic valve replacement • Surgical mechanical valve replacement • Vi. V TAVR
Final consensus • Vi. V TAVR ➢Previous sternotomies (2) ➢Potential need for future surgeries ➢Warfarin safety considering history of AVM
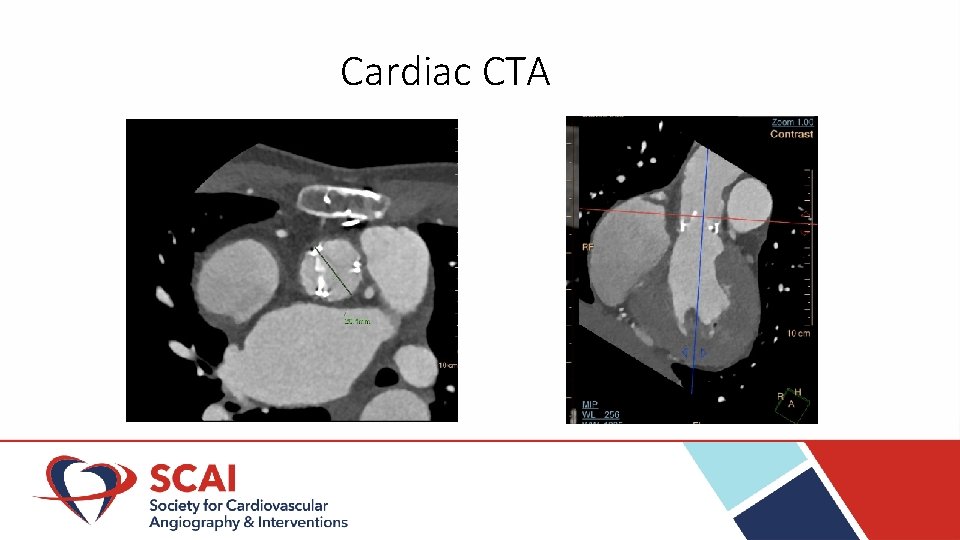
CT angiogram neck, chest, abdomen, pelvis • Partial calcification of AV • Right coronary cusp diameter- 27 mm, left coronary and non-coronary cusp diameter-26 mm • RCA and LCA were 23 mm and 17 mm above the bottom of prosthesis • Occlusion of right external iliac artery • Left iliofemoral artery patent
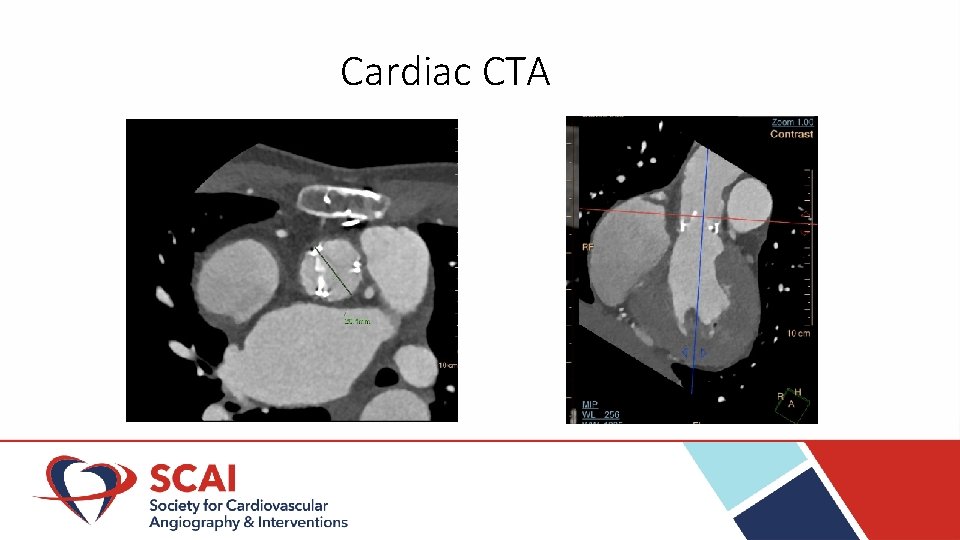
Cardiac CTA
CT angiogram neck, chest, abdomen, pelvis • Partial calcification of AV • Right coronary cusp diameter- 27 mm, left coronary and non-coronary cusp diameter-26 mm • RCA and LCA were 23 mm and 17 mm above the bottom of prosthesis • Occlusion of right external iliac artery • Left iliofemoral artery patent
Procedure • Patient in cath lab • 6 F sheath in right jugular vein for pacing catheter • 5 F sheath in left femoral artery • 6 F sheath in right brachial artery • Ascending aortic angiogram- Normal coronary arteries
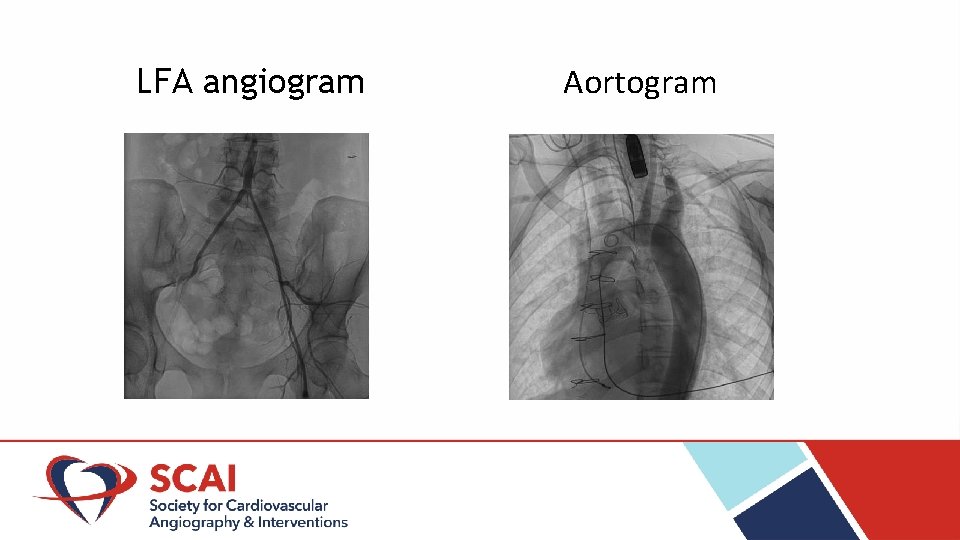
Arterial narrowing • Difficulty in advancing 8 F sheath in the LFA • Subsequent angiography: ➢ Severe stenosis of LFA ➢ Right common iliac artery- 2. 9 mm, left common iliac artery- 2. 3 mm ➢ Right subclavian artery- 4. 8 mm, left subclavian artery- 4. 2 mm ➢ Right carotid artery- 5. 6 mm, left carotid artery – 4. 7 mm
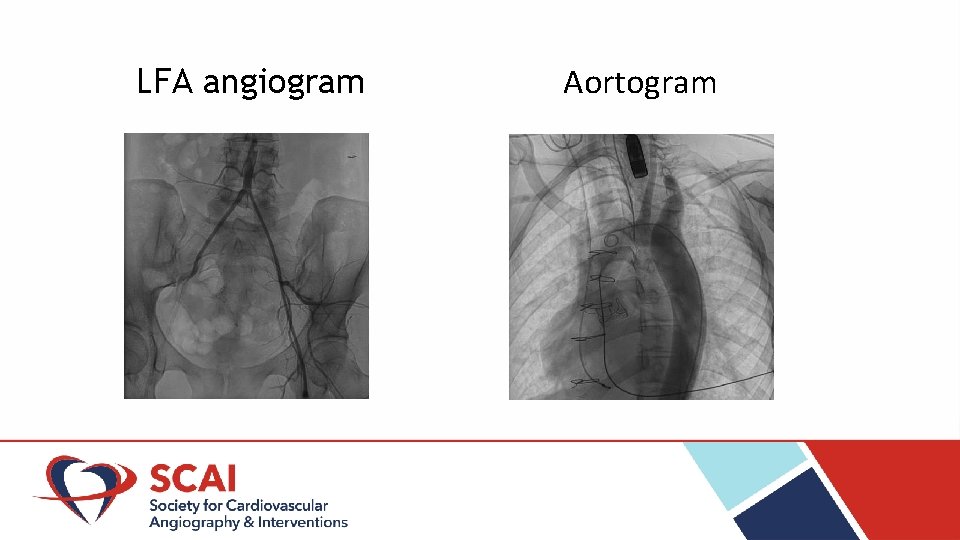
LFA angiogram Aortogram
Second attempt • • • 4 F and 6 F sheaths in right brachial artery and right femoral vein RV pacing catheter insertion 8 F sheath in LFA Papaverine administered Two perclose devices used in anticipation of securing hemostasis after procedure LFA dilated with 10 F dilator followed by placement of 14 F Edwards Esheath
Valve deployment • AV crossed with an AL-1 catheter followed by insertion of straight 300 cm stiff Amplatz wire that was positioned in the LV • 23 mm Edwards Sapien S 3 valve deployed under RV pacing and angiographic guidance.
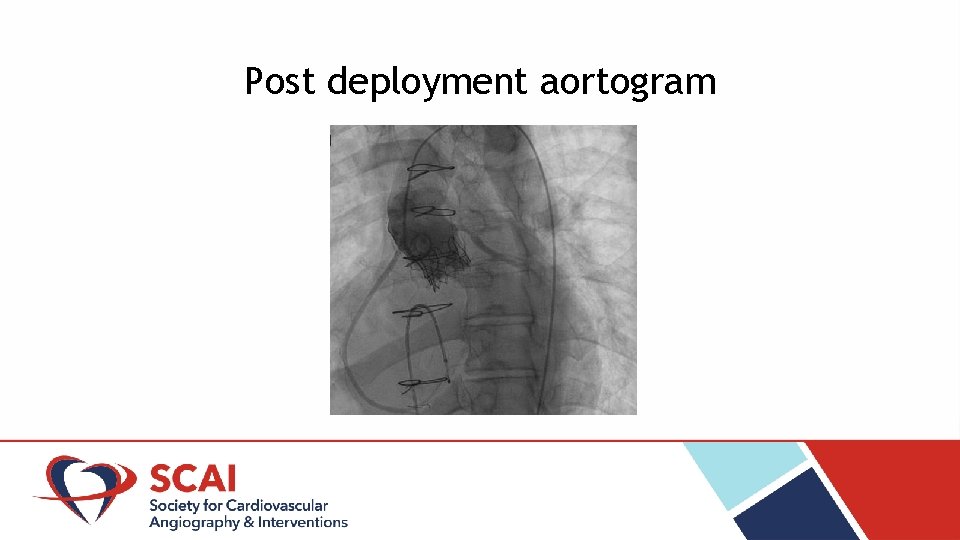
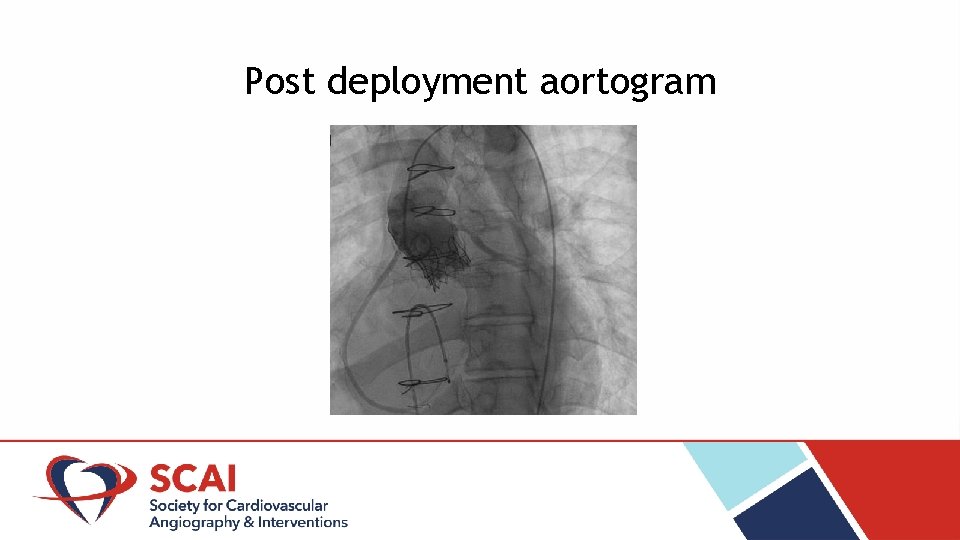
Post deployment aortogram
Post deployment TEE: • Resolution of aortic stenosis • Bioprosthetic valve peak gradient 38 mm. Hg, mean gradient 23 mm. Hg • Trivial insufficiency • No paravalvar leaks
Follow up 6 month follow up: • Significant clinical improvement TTE: • Mean gradient across bioprosthetic AV 21 mm. Hg (stable from prior) • No regurgitation • Normal left ventricular systolic function
Differential diagnosis of arterial narrowing* • Accordion effect • Arterial dissection • Arterial perforation • Vasospasm *Gallagher C, et al. Bilateral external iliac artery catheter-induced vasospasm during angiography. Angiology 2006; 57(1): 115 -118.
Arterial vasospasm • More common in small arteries • Vasospasm of large arteries - ergotamine, cocaine or catheter induced • Catheter induced vasospasm*: ➢ Mechanical irritation ➢ Release of vasoactive substances ➢ Endothelial denudation ➢ Sympathetic overactivity associated with Turner syndrome+ *Ergene O, et al. Catheter-induced vasospasm in the right external iliac and femoral arteries during a cardiac diagnostic procedure. International Journal of Cardiac Imaging 1999; 15: 189 -193. +Gravholt CH, et al. Nocturnal hypertension and impaired sympathovagal tone in Turner syndrome. Journal of Hypertension Feb 2006; 24(2): 353 -360.
Conclusion • Catheter induced arterial vasospasm is a rare but transient phenomenon • May be prevented by preemptive administration of vasodilators • Recognition of this phenomenon is important for planning procedural access in TAVR procedures
Thank you! If there are questions, please email me at sguruc@lsuhsc. edu.