Difficult Conversations Paul F Cook Ph D Marla

- Slides: 25
Difficult Conversations Paul F. Cook, Ph. D & Marla A. Corwin, LCSW, CAC III CU College of Nursing
OUR GOALS FOR YOU • Adopt a helpful attitude that will help defuse potentially difficult interactions with patients • Employ opening gambits that reduce the likelihood of confrontation and denial • Use motivational interviewing techniques to work through sustain talk or “ordinary resistance” • Recognize and respond to “change talk” to help patients keep moving through the process of change
What Makes a Conversation “Difficult”?
Motivational Interviewing “Spirit” • MI is not primarily a set of techniques; it is an attitude or a different way of being with people • MI is at the same time … • Empathic (caring) and • Guiding (directive) • Some characteristics of MI (ACCE): • Accepting • Collaborative / Person-Centered • Compassionate • Evoking and Strengthening Motivation to Change Miller et al. , 2013, Motivational Interviewing, 3 rd Ed.
LURE • Listen carefully so you can • Understand your patient’s motivation • Resist the urge to “fix it” • Empower the patient Lucy Bradley-Springer, CU School of Medicine (adapted from Rollnick et al. , 2011)

12 Roadblocks to Progress Gordon, 1970
Roadblocks • Ordering • Threatening • Persuading • Lecturing • Moralizing • Criticizing • Shaming • Psychoanalyzing • Sympathizing • Praising • Questioning • Changing the Subject Try It!
Motivational Interviewing • Developed for substance abuse counselors • Intended to motivate “resistant” patients • Based on social psychology principles • Social influence/persuasion • People resist efforts to change them • Person-centered counseling • MI is “a method for exploring and resolving ambivalence” • MI is “like dancing, not wrestling” Miller & Rollnick. (2002). Motivational Interviewing, 2 nd Ed. Try It!
Evidence for Motivational Interviewing • Review of 119 studies with almost 9, 000 participants, most with 3 -12 month follow-up data • Total amount of MI provided: 30 min to 4 hrs • Moderate changes in alcohol use, drug use, diet & exercise, emotional distress, treatment adherence • Smaller but still significant changes for smoking (about half as strong), based on 16 studies • Smaller numbers of studies on safe sex show weaker effects; strongest effects are for gambling • No difference by provider discipline or training Burke, et al. (2003). J Consult Clin Psych, 71, 843 -61; Hettema & Hendricks. (2010). J Consult Clin Psych, 78, 868 -84; Lundahl et al. (2010). Res Soc Work Pract, 20, 137 -60.
Opening Difficult Conversations • Make it about the piece of paper • “We ask everyone to take this survey …” • “I tell all my patients that …” • “You might be interested to know …” • Make it your issue • “Based on … I’m concerned about …” • “Because I’m your doctor, I have to say. . . ” • Give whenever you take away • “I admire …, and you might consider …” Rollnick et al. , 1999, Health Behavior Change
Conversations About Weight • Diet and exercise are the most sensitive information in people’s medical records! • Much more than diagnoses and treatments • Use “eating habits” &“physical activity” instead • Fat vs. overweight, obese vs increased BMI • Use person-centered language (“man with obesity” vs. “obese man” – or even “well-nourished man”? ) • Address comfort/need for accommodations • And what if you struggle with this yourself?
Sexual Risk Conversations • To assess risks specific to sex, ask about: • • • Partners Practices Protection from STDs Past history of STDs (recent matters most) Prevention in pregnancy • Do your patients with substance abuse disorders have some of these risk factors for HIV or other STDs? • What are your concerns in asking questions on these topics? Is asking about sex different from asking about other behaviors? • How can you ask about these topics in ways that make patients more comfortable?
Asking About Substance Use Try using the CAGE: • Have you ever felt the need to CUT DOWN on your drinking? • Have you ever felt ANNOYED by criticism of your drinking? • Have you ever felt GUILTY about your drinking? • Do you ever take a drink as a morning EYE-OPENER?
Giving Effective Feedback • Provide reference norms • Use visuals to show data • Actively reject labels • “I’m not saying you have a drinking problem” • Use neutral, normative words • Use: feeling down, stressed, confused • Not: being depressed, anxious, psychotic • Ask for a reaction, don’t assume one • Use scaling questions to gauge patient’s response
OARS • Open Ended Questions • Affirm • Reflect • Summarize
Recognizing Readiness Sustain Talk • Seeing benefits of current behavior • Seeing costs of new behavior Strategy: back off, build motivation (the “strong principle of change”: increase benefits) Change Talk • Seeing benefits of new behavior • Seeing costs of current behavior Strategy: support efforts for change (the “weak principle of change”: decrease barriers) Prochaska et al. (1995). Changing for Good
Rolling with Sustain Talk When people resist, you are probably pushing too hard for change! • Use reflection to communicate empathy • I hear that this is difficult for you • Find out what the patient already knows • Wait to offer new information until you are invited • Ask the patient her opinion about the new information • Summarize to communicate understanding • You see three barriers to moving forward: …. • What causes problems doesn’t matter as much as what you decide to do about them. • Use open-ended questions to refocus on change • What would you be doing if the situation were different?
Sustain Talk: Use FRAMES • Feedback about personal risks • Responsibility for change is the patient’s • Advice is given in a nonjudgmental way • Menus of options are suggested • Empathic counseling style (OARS) • Self-efficacy of the patient is encouraged Miller & Rollnick, 2002
A Helpful Attitude • Accepting – arguing won’t help • Empathic – the patient is trying • Absolute Worth – no conditions • Hopeful – change is possible • Collaborative – you don’t have all the answers • Eliciting – be curious, seek first to understand • Autonomy Supportive – patients’ answers are best • Partnership – you find solutions together Miller et al. , 2013, Motivational Interviewing, 3 rd Ed.
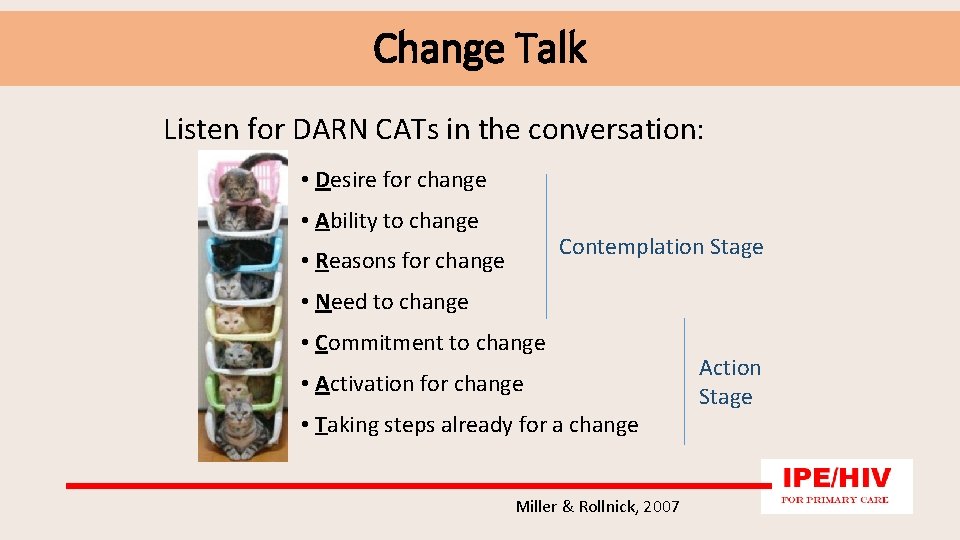
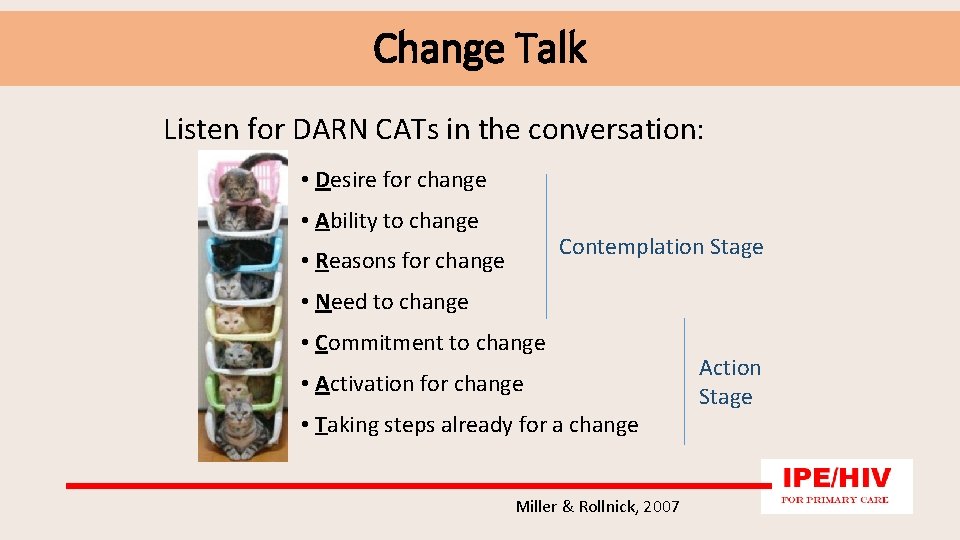
Change Talk Listen for DARN CATs in the conversation: • Desire for change • Ability to change Contemplation Stage • Reasons for change • Need to change • Commitment to change • Activation for change • Taking steps already for a change Miller & Rollnick, 2007 Action Stage
An Example: Comorbid Alcohol Use https: //www. youtube. com/watch? v=Max. Huf 17 A 44 • What seems helpful here? What doesn’t? • What (if anything) seems challenging or difficult? • Where did you see OARS techniques? • Where did you see the spirit of MI?
Red Light / Green Light • SUSTAIN TALK • LURE: listen, understand, resist the urge to “fix it, ” empathize • AMBIVALENCE • OARS: open-ended questions, affirm, reflect, summarize • Use elicit-provide-elicit to educate • CHANGE TALK • OARS to elaborate and develop ideas • Problem-solve to remove barriers • Challenge the change Dart, M. A. (2011). Motivational Interviewing in Nursing Practice
Learn More about MI • Miller & Rollnick (2012). Motivational Inteviewing: Helping People Change, 3 rd Ed. • Rollnick, Miller, & Butler (2007). Motivational Interviewing in Health Care • Rollnick, et al. (1999). Health Behavior Change • MI home page: www. motivationalinterviewing. org • Rosengren (2009). Building Motivational Interviewing Skills: A Practitioner Workbook • Seminars: professional. development@ucdenver. edu • Online MI courses: www. regonline. com/cumotivate
For More About IPE and HIV We can help you teach your students: • motivational interviewing / behavior change • interprofessional team communication • quality improvement methods We offer advanced training on: • HIV testing and prevention • treatment of HIV infection • primary care for patients with HIV Contact Laurra Aagaard at: laurra. aagaard@ucdenver. edu or by phone at: 303. 724. 5992