Differentiating Between Quality Improvement Evidencebased Practice and Research

Differentiating Between Quality Improvement, Evidence-based Practice, and Research Harris Health System, Houston, Texas
Objectives Describe Quality Improvement (QI) Describe Evidence‐based Practice (EBP) Describe Research in Nursing Differentiate between QI, EBP, and research in nursing harrishealth. org 2
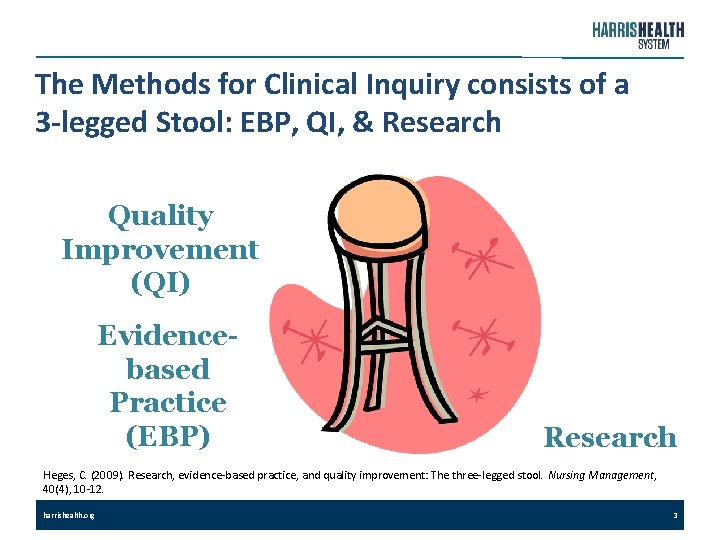
The Methods for Clinical Inquiry consists of a 3 -legged Stool: EBP, QI, & Research Quality Improvement (QI) Evidencebased Practice (EBP) Research Heges, C. (2009). Research, evidence‐based practice, and quality improvement: The three‐legged stool. Nursing Management, 40(4), 10‐ 12. harrishealth. org 3
Why is it important to know the difference between EBP, QI, and Research? Selecting the correct methodology is important when addressing a clinical question to improve nursing practice or patient outcomes. Organizations that exemplify excellence are able to identify sources of evidence (SOE) that demonstrate exemplary professional practice and application of new knowledge and innovation. (American Nurses Credentialing Center, 2014). harrishealth. org 4
How EBP, QI, & Research Contribute to Nursing Practice ANA Code of Ethics for Nurses: Provision 7 “The nursing profession should engage in scholarly inquiry to identify, evaluate, refine, and expand the body of knowledge that forms the foundation of its discipline and practice. ” “All nurses working alone or in collaboration with others can participate in the advancement of the profession through the development, evaluation, dissemination, & application of knowledge in practice. ” (American Nurses Association, current edition). harrishealth. org 5
Awareness of the differences in QI, EBP, & Research is important. … harrishealth. org • So nurses can appropriately explore the safest and best practices for their patients and practice environment. • So nurses can continually improve nursing practice and patient outcomes. • So nurses are able to generate new knowledge. 6

t n e m e v o r p m I y t i l Qua ibili s n o p s 's re yone r e v e s i y “Qualit ards Deming w ‐ W. Ed ty. "
What is Quality Improvement (QI)? Q U A L I T Y I M P R O V E M E N T “Quality improvement (QI) consists of systematic and continuous actions that lead to measurable improvement in health care services and the health status of targeted patient groups. ” (Health Resources & Services Administration, 2016 a) harrishealth. org 8
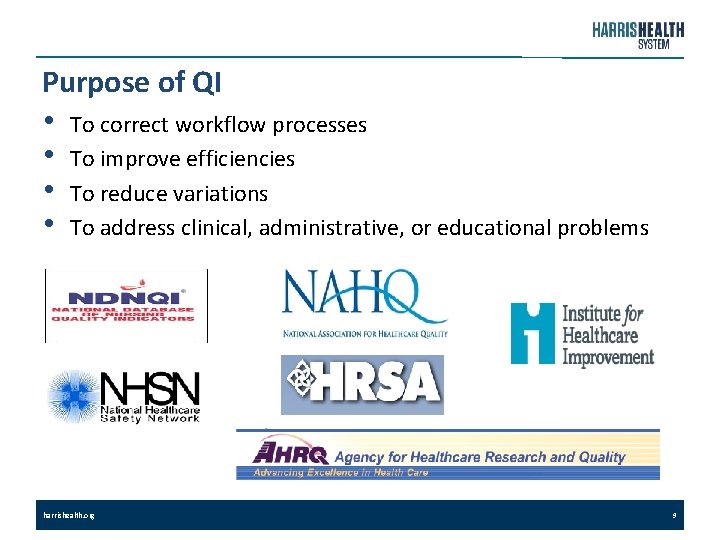
Purpose of QI • • To correct workflow processes To improve efficiencies To reduce variations To address clinical, administrative, or educational problems harrishealth. org 9
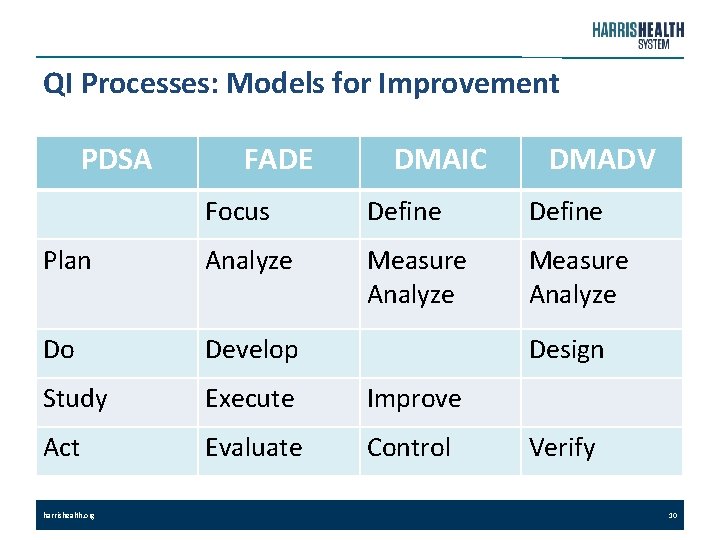
QI Processes: Models for Improvement PDSA FADE DMAIC DMADV Focus Define Plan Analyze Measure Analyze Do Develop Study Execute Improve Act Evaluate Control harrishealth. org Design Verify 10
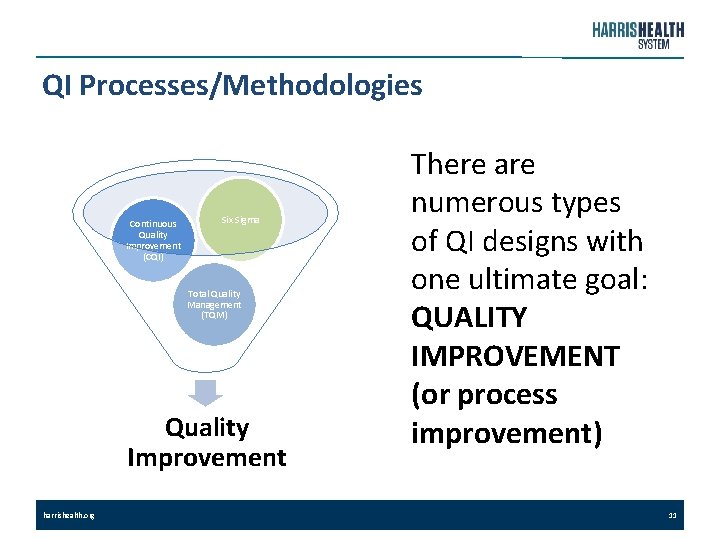
QI Processes/Methodologies Continuous Quality Improvement (CQI) Six Sigma Total Quality Management (TQM) Quality Improvement harrishealth. org There are numerous types of QI designs with one ultimate goal: QUALITY IMPROVEMENT (or process improvement) 11
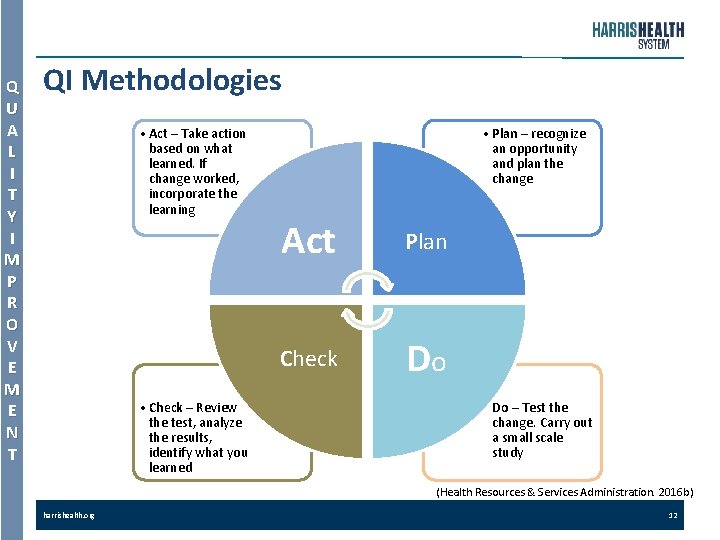
Q U A L I T Y I M P R O V E M E N T QI Methodologies • Act – Take action based on what learned. If change worked, incorporate the learning • Check – Review the test, analyze the results, identify what you learned • Plan – recognize an opportunity and plan the change Act Plan Check Do • Do – Test the change. Carry out a small scale study (Health Resources & Services Administration. 2016 b) harrishealth. org 12
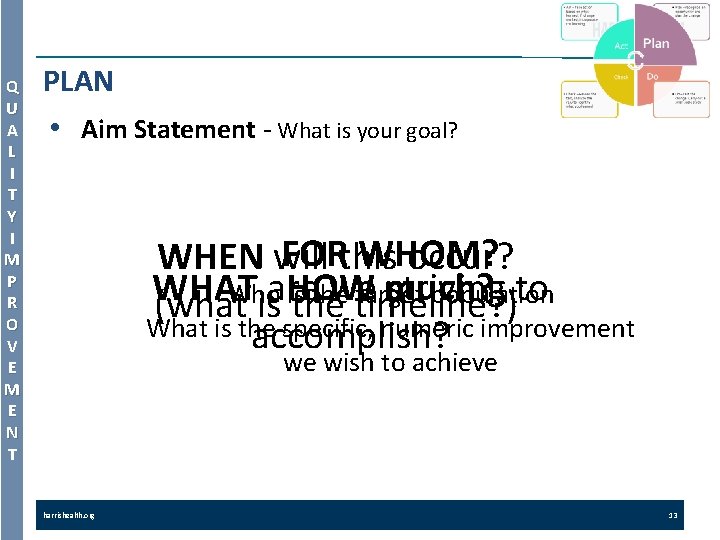
Q U A L I T Y I M P R O V E M E N T PLAN • Aim Statement ‐ What is your goal? FOR WHOM? WHEN will this occur? WHAT are we striving to Who HOW much? is the target population (what is the timeline? ) What is the specific, numeric improvement accomplish? we wish to achieve harrishealth. org 13
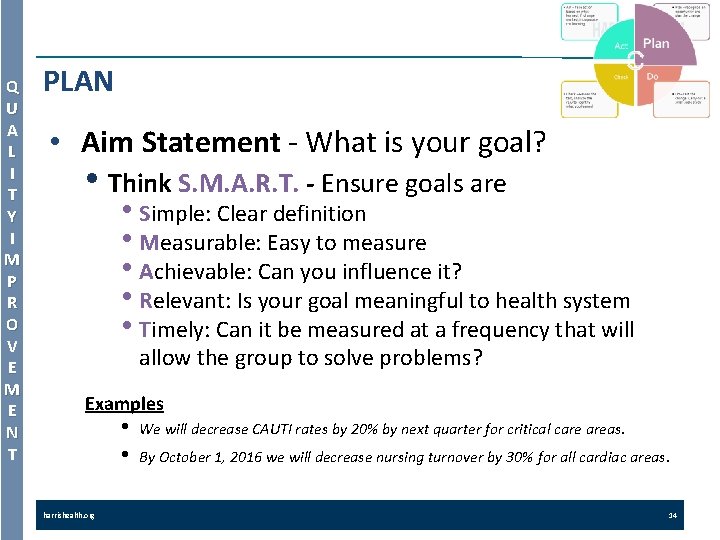
Q U A L I T Y I M P R O V E M E N T PLAN • Aim Statement ‐ What is your goal? • Think S. M. A. R. T. - Ensure goals are • Simple: Clear definition • Measurable: Easy to measure • Achievable: Can you influence it? • Relevant: Is your goal meaningful to health system • Timely: Can it be measured at a frequency that will allow the group to solve problems? Examples • • harrishealth. org We will decrease CAUTI rates by 20% by next quarter for critical care areas. By October 1, 2016 we will decrease nursing turnover by 30% for all cardiac areas. 14
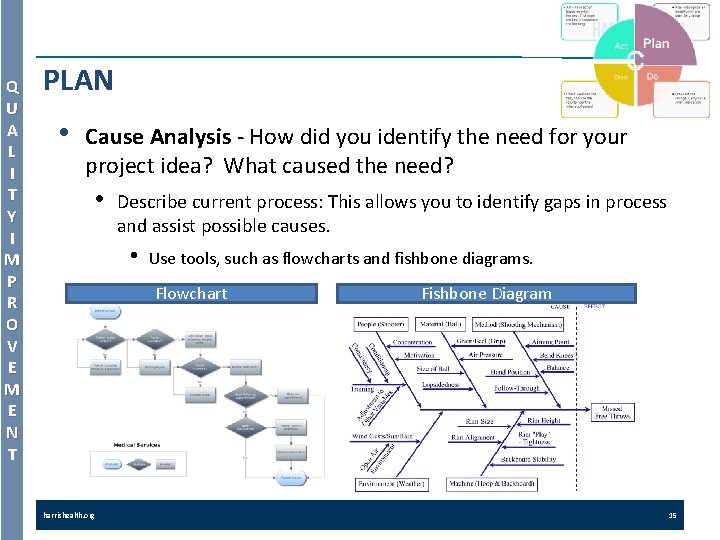
Q U A L I T Y I M P R O V E M E N T PLAN • Cause Analysis ‐ How did you identify the need for your project idea? What caused the need? • Describe current process: This allows you to identify gaps in process and assist possible causes. • Use tools, such as flowcharts and fishbone diagrams. Flowchart harrishealth. org Fishbone Diagram 15
Q U A L I T Y I M P R O V E M E N T PLAN • • Baseline Measure ‐ What is the baseline measure of your goal? What is happening before you try your idea? You will not know the success of the change if you don't have a baseline measurement for comparison The data may address, time, people, space, cost, number of steps, adverse events, patient satisfaction, or nurse satisfaction Data can be displayed via scorecards, run charts, etc. The data collected must be aligned with the measures listed in the aim statement. harrishealth. org 16
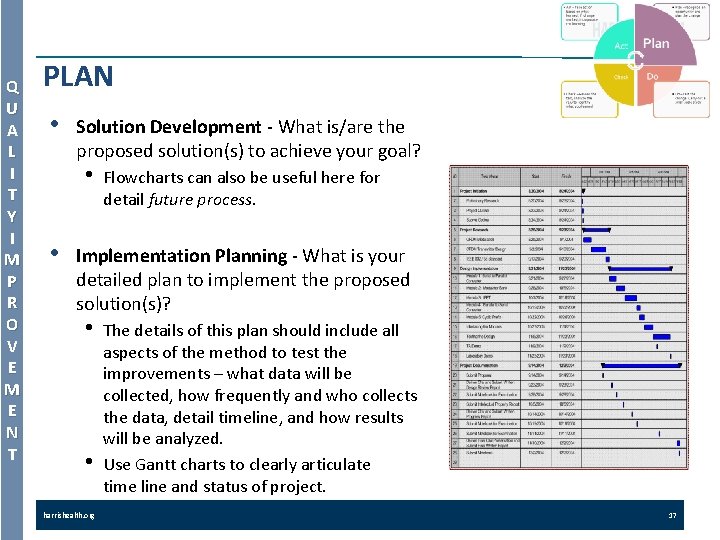
Q U A L I T Y I M P R O V E M E N T PLAN • Solution Development ‐ What is/are the proposed solution(s) to achieve your goal? • • Flowcharts can also be useful here for detail future process. Implementation Planning ‐ What is your detailed plan to implement the proposed solution(s)? • • harrishealth. org The details of this plan should include all aspects of the method to test the improvements – what data will be collected, how frequently and who collects the data, detail timeline, and how results will be analyzed. Use Gantt charts to clearly articulate time line and status of project. 17
Q U A L I T Y I M P R O V E M E N T DO • Implement the Solution § Communicate your plan. § Conduct your pilot: implement the improvement. § Collect and document the data § Document problems, unexpected observations, lessons learned and knowledge gained. harrishealth. org 18
Q U A L I T Y I M P R O V E M E N T CHECK (or STUDY) • Evaluate the Result • Describe how you will determine • harrishealth. org that your idea makes an improvement. Did your implemented solution achieve the Aim Statement? 19
Q U A L I T Y I M P R O V E M E N T ACT • Follow-up Plan - What is your plan to ensure your improvement can be sustained over time? • What lessons did you learn? Determine if the solution should be: • Adopted: standardize the improvement • Adapted: Repeat the pilot with modifications based on lesson • • harrishealth. org learned and cycle back to “Do” phase Abandoned: If the changes made to the process did not result in an improvement, consider lessons learned from the initial test, and return to the “Plan” phase Remember … this is an improvement cycle! 20
e c i t c a r P d e s a B e c n e d i v E
E V I D E N C E B A S E D P R A C T I C E What is Evidence-Based Practice (EBP)? Evidence‐Based Practice (EBP) is the ". . . conscientious, explicit, and judicious use of current best evidence. . . " in making clinical practice and policy decisions (Sacket et al. , 2000). EBP integrates clinical expertise with the best available external clinical research evidence and patients’ unique values and circumstances. harrishealth. org 22
E V I D E N C E B A S E D P R A C T I C E Evidence-based Practice • • EBP is a problem‐solving approach that integrates a systematic search for and critical appraisal of the most recent and relevant evidence to answer a burning clinical, educational, or administrative question. EBP integrates the best available evidence, clinical judgment, and patient preferences. (Melynk & Fineout‐Overholt, 2005; Stetler, 2001; & Titler et al. , 2001). harrishealth. org 23

E V I D E N C E B A S E D P R A C T I C E What are the elements of EBP? EBP integrates … best research evidence … with clinical expertise … and patient values. Best Research Clinical Expertise Patient Values (Sackett, 1996) harrishealth. org 24

E V I D E N C E B A S E D P R A C T I C E Samples of EBP Models Stevens, K. R. (2004). ACE Start Model of EBP: Knowledge Transformation. Academic Center for Evidence‐based Practice. San Antonio, TX: University of Texas Health Science Center. Stetler, C. (2001). The Stetler Model of Research Utilization to Facilitate Evidence‐ based Practice. Nursing Outlook, 49, 272‐ 279. harrishealth. org ACE Star Model Johns Hopkins Model Stetler Model IOWA Model Dearholt, S. & Dang, D. (2012). Johns Hopkins Nursing Evidence‐based Practice: Model and Guidelines. (2 nd ed. ). Titler et al. (2001). The IOWA Model of Evidence‐based Practice. To Promote Quality Care. Critical Care Nursing Clinics of North America, 13(4), 497‐ 509. 25
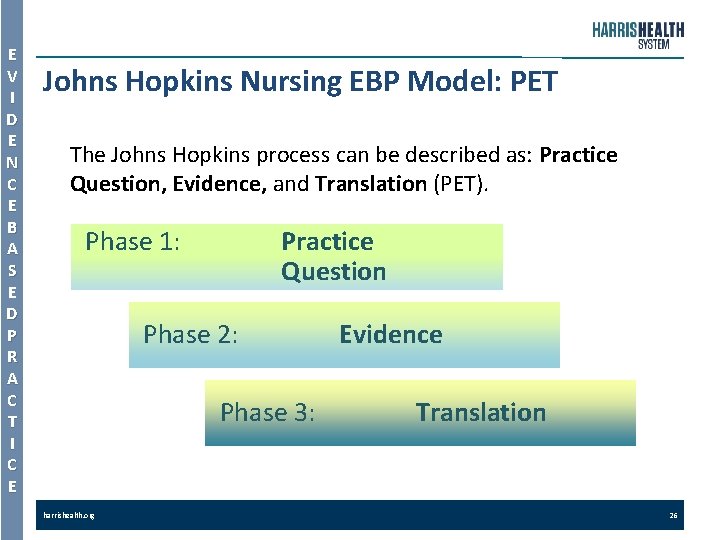
E V I D E N C E B A S E D P R A C T I C E Johns Hopkins Nursing EBP Model: PET The Johns Hopkins process can be described as: Practice Question, Evidence, and Translation (PET). Phase 1: Practice Question Phase 2: Phase 3: harrishealth. org Evidence Translation 26
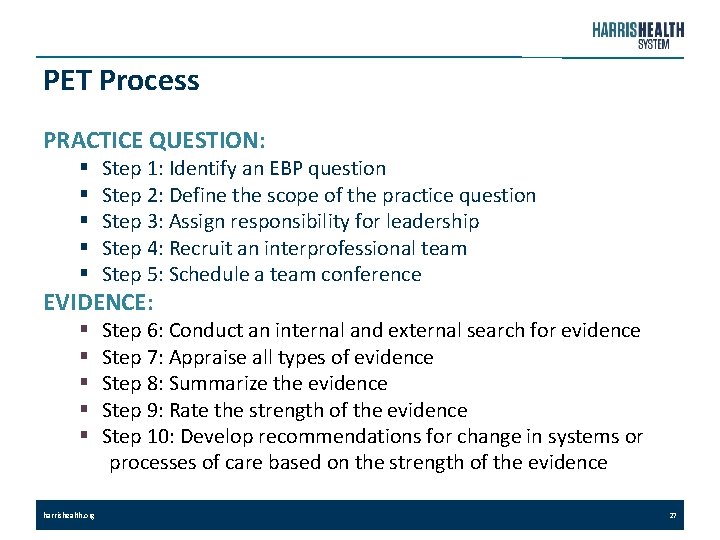
PET Process PRACTICE QUESTION: § § § Step 1: Identify an EBP question Step 2: Define the scope of the practice question Step 3: Assign responsibility for leadership Step 4: Recruit an interprofessional team Step 5: Schedule a team conference EVIDENCE: § § § harrishealth. org Step 6: Conduct an internal and external search for evidence Step 7: Appraise all types of evidence Step 8: Summarize the evidence Step 9: Rate the strength of the evidence Step 10: Develop recommendations for change in systems or processes of care based on the strength of the evidence 27
PET Process (cont’d) TRANSLATION: § Step 11: Determine the appropriateness and feasibility of translating recommendations into the specific practice setting § Step 12: Create an action plan § Step 13: Implement the change § Step 14: Evaluate outcomes § Step 15: Report the results of the preliminary evaluation to decision makers § Step 16: Secure support from decision makes to implement the recommended change internally § Step 17: Identify the next steps § Step 18: Communicate the findings harrishealth. org 28
E V I D E N C E B A S E D P R A C T I C E Phase 1: Practice Question Ask a focused clinical question using the mnemonic: PICO Ø P = Patient population or problem. Ø I = Intervention or treatment. Ø C = Comparison, when warranted. Ø O = Outcome desired (improve nursing practice or patient outcomes). harrishealth. org 29
E V I D E N C E B A S E D P R A C T I C E Phase 2: Evidence Ø There are various evidence pyramids or levels of evidence used by the scientific community. Ø Iowa Model (also known as Translation Research Model) Ø Highlights the importance of considering the entire healthcare system from the provider, to the patient, to the infrastructure, using research within these contexts to guide practice decisions. Ø The Johns Hopkins EBP Model (JHEBPM) Ø Provides a five‐level system for “grading” the evidence. Ø Oxford Centre for Evidence-Based Medicine Ø Uses a numbering scheme ranging from 1 a, homogenous systematic Ø harrishealth. org reviews of randomized controlled trials, to 5, expert opinion. Can be useful when comparing articles with similar study designs. 30
E V I D E N C E B A S E D P R A C T I C E Phase 2: Evidence (cont’d) Ø When reviewing evidence to support practice, the nurse should carefully consider the evidence. Since the quality of research is different based on its methodology and number of study designs in the literature, the rigor of evidence may vary. Ø There can be value in all levels of evidence, but quality can vary in any study. harrishealth. org 31
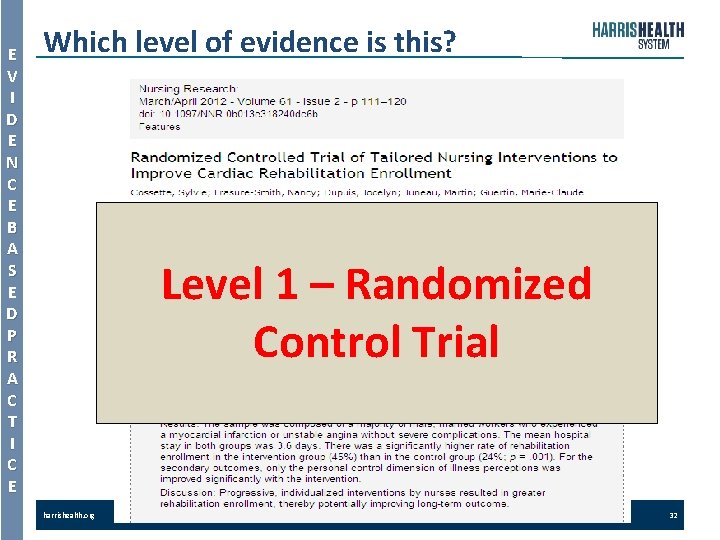
E V I D E N C E B A S E D P R A C T I C E Which level of evidence is this? Level 1 – Randomized Control Trial harrishealth. org 32
E V I D E N C E B A S E D P R A C T I C E The Levels of Evidence (cont’d) Ø Though finding research studies at Level I is preferred, evidence‐based nursing may need to draw upon research designs lower in the evidence hierarchy (Levels II or III). Ø Occasionally, nothing but case reports or even bench research may exist on a topic. Ø When making evidence‐based decisions for patient care, it is essential to select the strongest level research design available for the specific question of interest. harrishealth. org 33
E V I D E N C E B A S E D P R A C T I C E Is it “Best Practice” or EBP? • The terms “best practice” and “evidence‐ based practice” are sometimes used interchangeably, but the two are different. § Best practice is a generic or general phrase for a process of infusing nursing practice with research‐based knowledge. § EBP (derived from evidence‐based medicine) is a more formalized process of conscientiously, explicitly, and judiciously using current best evidence in making decisions about patient care. EBP means integrating individual clinical expertise with the best available external clinical evidence from systematic research. (Sackett et al. , 1996). harrishealth. org 34
E V I D E N C E B A S E D P R A C T I C E Is it “Best Practice” or EBP? • Best Practices are • • “Nursing practices that are based on the ‘best evidence’ available from nursing research. ” (The University of Iowa, 2013). “Knowledge transfer of credible research evidence. ” (Thompson, Estabrooks, & Degner, 2006). The goal of “best practices” is to apply the most recent, relevant, and helpful nursing interventions, based on research, in real-life practice. harrishealth. org 35
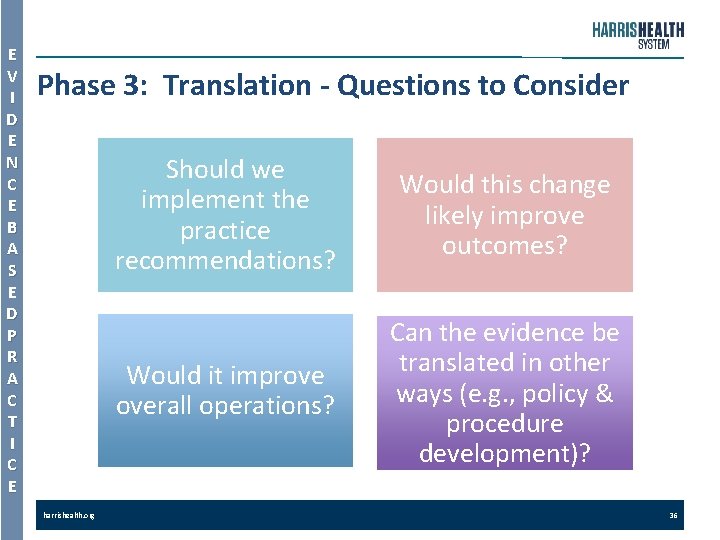
E V I D E N C E B A S E D P R A C T I C E Phase 3: Translation - Questions to Consider harrishealth. org Should we implement the practice recommendations? Would this change likely improve outcomes? Would it improve overall operations? Can the evidence be translated in other ways (e. g. , policy & procedure development)? 36
E V I D E N C E B A S E D P R A C T I C E Phase 3 – Translation (cont’d) • Determine (with data collection and analysis), if the current or changed practice is achieving the best possible patient outcome. harrishealth. org 37
E V I D E N C E B A S E D P R A C T I C E Disseminate Project Findings Share information with potential users in the healthcare system so nursing practice and patient outcomes can be improved in other settings. • Internally: newsletters, town hall meetings, or other institutional meetings. • Locally: professional nursing organization meetings. • Nationally: professional nursing conference or poster. • Publish: article in a peer‐reviewed, professional journal. harrishealth. org 38
h c r a e Res ld wou t i , g n i ere do w e w t it was uld it? ” a h w new , wo “If we k lled research ca not be instein t. E ‐ Alber
What is Research? R E S E A R C H The Code of Federal Regulations defines research as “A systematic investigation designed to develop and contribute to generalizable knowledge” (U. S Department of Health and Human Services, 2009). The website on the Office for Human Research Protections provides a wealth of information about the research process and policies. harrishealth. org 40
What is Nursing Research? • R E S E A R C H A systematic inquiry designed to develop knowledge about issues of importance to the nursing profession (Polit & Beck, 2012). harrishealth. org 41
What is Nursing Research? R E S E A R C H • The purposes of research are to: • • • harrishealth. org Generate new knowledge. Validate existing knowledge. Conduct a systematic review of the literature to identify knowledge gaps. Use systematic, scientific inquiry and rigorous methods to answer a research question. Identify variables that can be measured or manipulated to describe, explain, and/or predict. 42
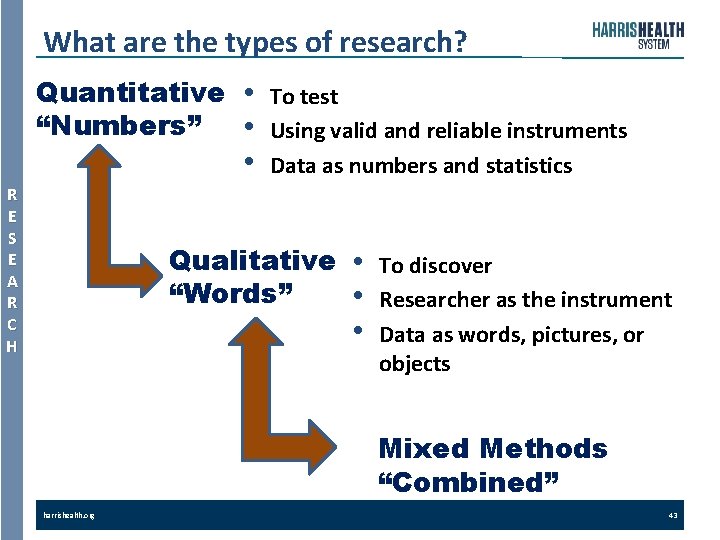
What are the types of research? Quantitative “Numbers” R E S E A R C H • • • To test Using valid and reliable instruments Data as numbers and statistics Qualitative “Words” • • • To discover Researcher as the instrument Data as words, pictures, or objects Mixed Methods “Combined” harrishealth. org 43
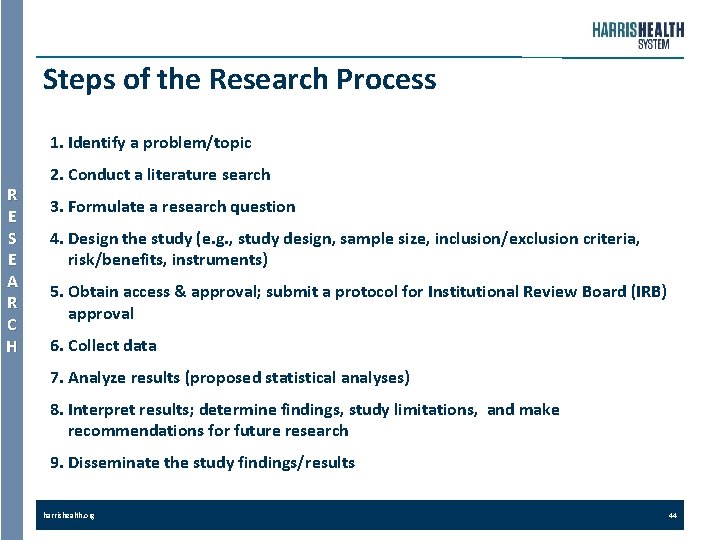
Steps of the Research Process 1. Identify a problem/topic R E S E A R C H 2. Conduct a literature search 3. Formulate a research question 4. Design the study (e. g. , study design, sample size, inclusion/exclusion criteria, risk/benefits, instruments) 5. Obtain access & approval; submit a protocol for Institutional Review Board (IRB) approval 6. Collect data 7. Analyze results (proposed statistical analyses) 8. Interpret results; determine findings, study limitations, and make recommendations for future research 9. Disseminate the study findings/results harrishealth. org 44
3 e h t n e e w t e b g n i t a i t n y e r r i e u f f q i n i D l a c i n i l c f o s d o h t e m
Comparing EBP, QI, & Research R E S E A R C H • Review the following slides that contain tables comparing EBP, QI, & Research: § Intent § § § harrishealth. org Methodology Design Regulating Bodies Additional Burden or Risks IRB Approval Dissemination 46
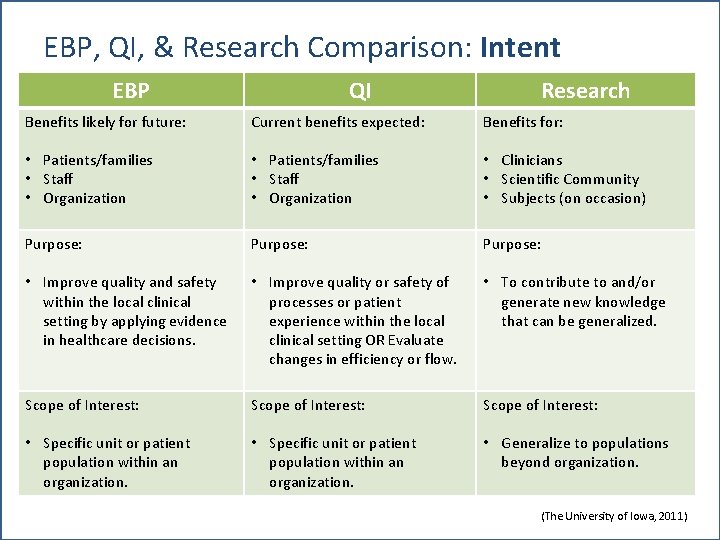
EBP, QI, & Research Comparison: Intent EBP QI Research Benefits likely for future: Current benefits expected: Benefits for: • Patients/families • Staff • Organization • Clinicians • Scientific Community • Subjects (on occasion) Purpose: • Improve quality and safety within the local clinical setting by applying evidence in healthcare decisions. • Improve quality or safety of processes or patient experience within the local clinical setting OR Evaluate changes in efficiency or flow. • To contribute to and/or generate new knowledge that can be generalized. Scope of Interest: • Specific unit or patient population within an organization. • Generalize to populations beyond organization. harrishealth. org 47 (The University of Iowa, 2011)

EBP, QI, & Research Comparison: Methodology EBP Processes or Outcomes Measurement: QI Processes or Outcomes Measurement: Research Processes or Outcomes Measurement: • Measure of key indicators • Measures are simple, easy • Measures are complex. using tools with face to use and administer. validity and may be • Increased time is required without established • Measures for key to fill out the measure. validity or reliability. indicators only. • Measures require a • Measures include detailed administration knowledge, attitude, plan. behavior/practices, and outcomes. • Estimates of reliability, validity, specificity, and/or sensitivity are required. harrishealth. org 48 (The University of Iowa, 2011)

EBP, QI, & Research Comparison: Design EBP QI Examples: • Iowa Model • Johns Hopkins Nursing EBP Model • ACE Star Model • Rosswurm & Larrabee Model • Stetler’s Model • • [Note: The Johns Hopkins Nursing Evidence‐Based Practice Model is used at Harris Health System. ] Other terms: Performance Improvement or Process Improvement (PI) harrishealth. org Plan Do Check Act (PDCA) Plan Do Study Act (PDSA) LEAN Six Sigma Focus Analyze Develop Execute (FADE) • Continuous Quality Improvement (CQI) • Total Quality Management (TQM) Research Examples: • Quantitative ü Randomized Control Trials (RCTs) ü Quasi‐experimental ü Non‐experimental • Longitudinal • Retrospective • Prospective • Correlational • Surveys • Qualitative ü Ethnography ü Grounded Theory ü Phenomenological 49 (The University of Iowa, 2011)
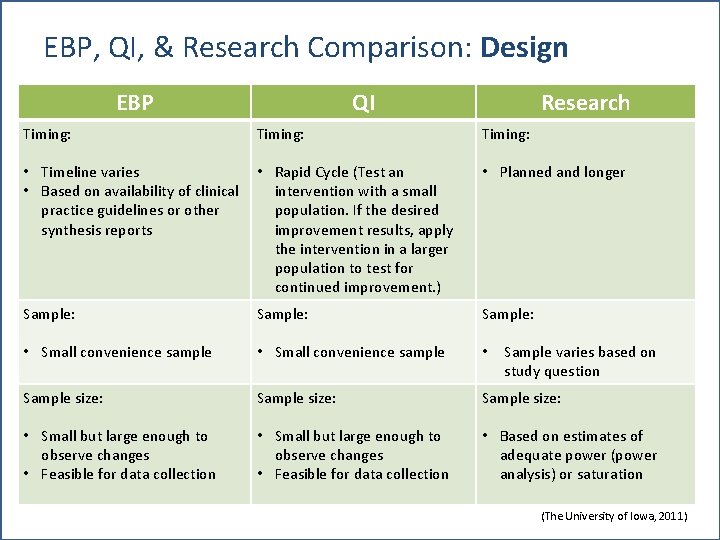
EBP, QI, & Research Comparison: Design EBP QI Research Timing: • Timeline varies • Based on availability of clinical practice guidelines or other synthesis reports • Rapid Cycle (Test an intervention with a small population. If the desired improvement results, apply the intervention in a larger population to test for continued improvement. ) • Planned and longer Sample: • Small convenience sample • Sample size: • Small but large enough to observe changes • Feasible for data collection • Based on estimates of adequate power (power analysis) or saturation harrishealth. org Sample varies based on study question 50 (The University of Iowa, 2011)

EBP, QI, & Research Comparison: Design EBP QI Research Data Collection: • Minimal time, resources, costs • Complex, tightly controlled plan constructed for resources to maintain consistency Extraneous variables: • Acknowledged, but not measured • Controlled and/or measured Data Analysis: • Descriptive statistics or statistical process control charts for trended data • Complex with inferential statistics to promote generalizability of results harrishealth. org 51 (The University of Iowa, 2011)
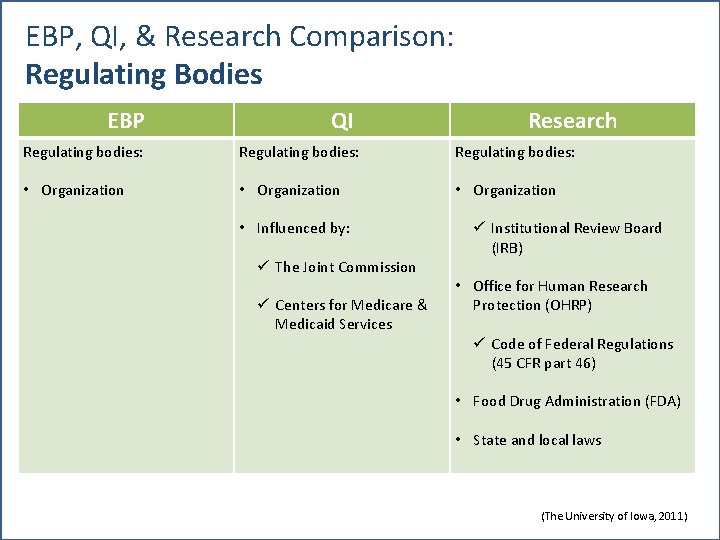
EBP, QI, & Research Comparison: Regulating Bodies EBP QI Research Regulating bodies: • Organization • Influenced by: ü The Joint Commission ü Centers for Medicare & Medicaid Services ü Institutional Review Board (IRB) • Office for Human Research Protection (OHRP) ü Code of Federal Regulations (45 CFR part 46) • Food Drug Administration (FDA) • State and local laws harrishealth. org 52 (The University of Iowa, 2011)
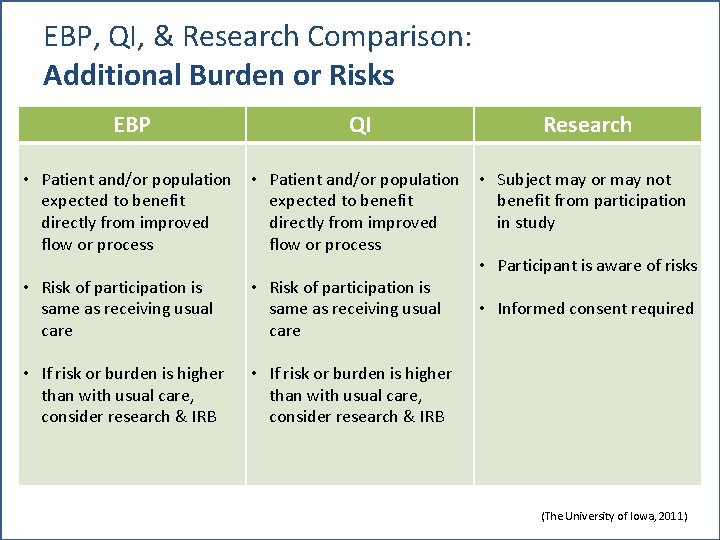
EBP, QI, & Research Comparison: Additional Burden or Risks EBP QI Research • Patient and/or population expected to benefit directly from improved flow or process • Subject may or may not benefit from participation in study • Risk of participation is same as receiving usual care • If risk or burden is higher than with usual care, consider research & IRB harrishealth. org • Participant is aware of risks • Informed consent required 53 (The University of Iowa, 2011)

EBP, QI, & Research Comparison: IRB Approval EBP • IRB approval not required (unless required by organizational policy) harrishealth. org QI • IRB approval not required (unless required by organizational policy) Research • IRB approval required 54 (The University of Iowa, 2011)
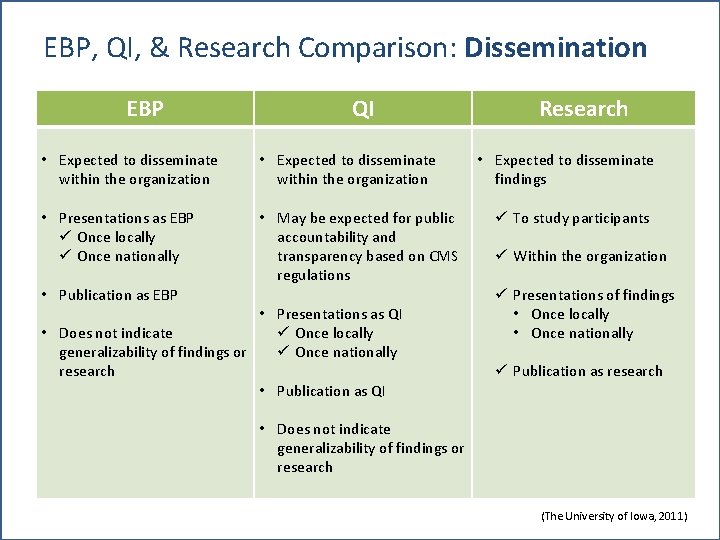
EBP, QI, & Research Comparison: Dissemination EBP QI • Expected to disseminate within the organization • Presentations as EBP ü Once locally ü Once nationally • May be expected for public accountability and transparency based on CMS regulations • Publication as EBP • Presentations as QI • Does not indicate ü Once locally generalizability of findings or ü Once nationally research • Publication as QI Research • Expected to disseminate findings ü To study participants ü Within the organization ü Presentations of findings • Once locally • Once nationally ü Publication as research • Does not indicate generalizability of findings or research harrishealth. org 55 (The University of Iowa, 2011)
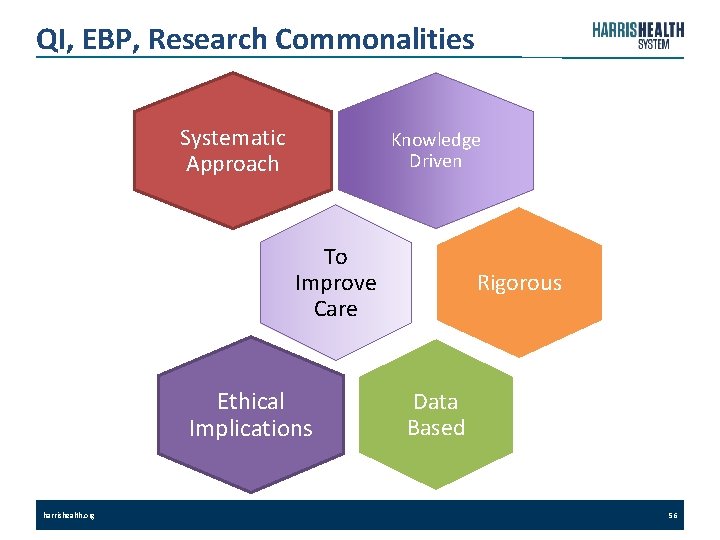
QI, EBP, Research Commonalities Systematic Approach Knowledge Driven To Improve Care Ethical Implications harrishealth. org Rigorous Data Based 56
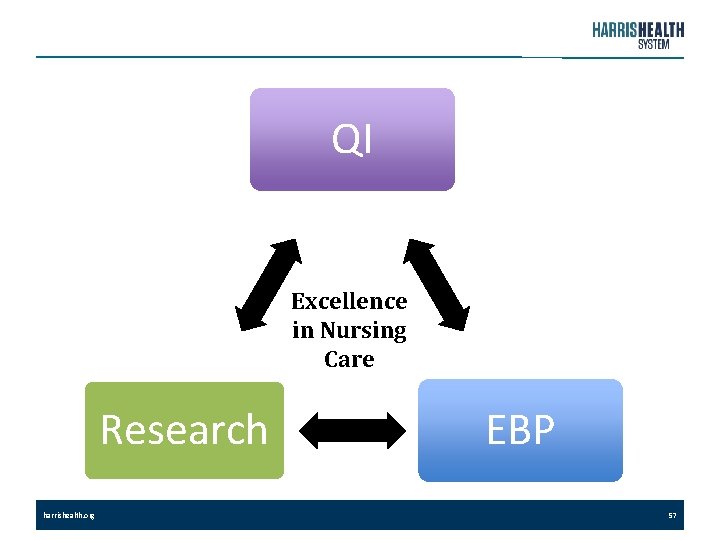
QI Excellence in Nursing Care Research harrishealth. org EBP 57
References American Nurses Association. (Current Edition). Code of Ethics for Nursing. Silver Springs, MD. American Nurses Credentialing Center. (2014). 2014 Magnet Application Manual. Silver Spring, MD: American Nurses Credentialing Center. Dearholt, S. , & Dang, D. (2012). Johns Hopkins Nursing Evidence‐based Practice: Model and Guidelines. (2 nd ed. ). Indianapolis, IN: Sigma Theta Tau International. Fineout‐Overholt, E. , Hofstettler, S. , Shell, L. , & Johnson, L. (2005). Teaching EBP: Getting to the gold: How to search for the best evidence. Worldviews on Evidence‐Based Nursing, 2(4), 207‐ 21. Heges, C. (2009). Research, evidence‐based practice, and quality improvement: The three‐legged stool. Nursing Management, 40(4), 10‐ 12. Health Resources and Services Administration. (2016 a). Quality improvement. In U. S. Department of Health and Human Services. Retrieved from http: //www. hrsa. gov/quality/toolbox/methodology/qualityimprovement/ Health Resources and Services Administration. (2016 b). Testing for improvement. In U. S. Department of Health and Human Services. Retrieved from http: //www. hrsa. gov/quality/toolbox/methodology/testingforimprovement/part 2. html harrishealth. org 58
References (cont’d) Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 2 st century. National Academies Press. Retrieved from https: //www. nationalacademies. org/hmd/~/media/Files/Report%20 Files/2001/Crossing‐the‐ Quality‐Chasm/Quality%20 Chasm%202001%20%20 report%20 brief. pdf Melnyk, B. , & Fineout‐Overholt, E. (2011). Evidence‐Based Practice in Nursing & Healthcare. (2 nd ed. ). Philadelphia, PA: Lippincott Williams & Wilkins. Newhouse, R. , Dearholt, S. , Poe, S. , Pugh, L. , & White, K. (2007). Johns Hopkins Nursing Evidence‐Based Practice Model and Guidelines. Indianapolis, IN: Sigma Theta Tau International. Pearson, A. , Weeks, S. , & Stern, C. (2011). Translation Science and The JBI Model of Evidence‐based Healthcare. Philadelphia, PA: Lippincott Williams & Wilkins. Polit, D. F. , & Beck, C. T. (2012). Nursing Research: Generating and Assessing Evidence for Nursing Practice (9 th ed. ). Philadelphia, PA: Lippincott Williams & Wilkins and Wolters Kluwer. Sackett, D. (1996). Evidence‐based medicine ‐ What it is and what it isn't. BMJ. 312: 71‐ 72. http: //www. bmj. com/cgi/content/full/312/7023/71 Salmond, S. W. (2007). Advancing evidence‐based practice: A primer. Orthopedic Nursing, 26(2), 114‐ 123. Stetler, C. (1994). Refinement of the Stetler/Marram model for application of research findings to practice. Nursing Outlook, 42(1), 15‐ 25. harrishealth. org 59
References (cont’d) Stevens, K. (2004). ACE Star model of EBP: Knowledge transformation. Academic Center for Evidence‐Based Practice. Retrieved 20 January 2012, from http: //www. acestar. uthscsa. edu Thompson, G. N. , Estabrooks, C. A. , & Degner, L. F. (2006). Clarifying the concepts in knowledge transfer: a literature review. Journal of Advanced Nursing, 53: 691– 701. doi: 10. 1111/j. 1365‐ 2648. 2006. 03775. x Titler, M. G. , Kleiber, C. , Steelman, V. J. , Rahel, B. A. , Budreau, G. Everett, L. Q. , et al. (2001). The IOWA Model of evidence‐based practice to promote quality care. Critical Care Clinics of North America, 13(4), 497‐ 509. The University of Iowa. (2011). Csomay Center ‐ Best practices for healthcare professionals. In College of Nursing. Retrieved May 30, 2013, from https: //nursing. uiowa. edu/hartford/best‐practices‐for‐healthcare‐professionals U. S Department of Health and Human Services. (2009). Code of federal regulations Title 45, Part 46. Office for Human Research Protections. Retrieved from http: //www. hhs. gov/ohrp/regulations‐and‐policy/regulations/45‐cfr‐ 46/ harrishealth. org 60
- Slides: 60