Differences in Pelvic Exam Performance by Less Versus
Differences in Pelvic Exam Performance by Less Versus More Experienced Primary Care Providers: Implications for Medical Education and Future Practice Jennifer B. Manning & Jani R. Jensen, MD Mayo Clinic College of Medicine April 27 th, 2015 © 2012 MFMER | slide-1
Disclosures • None © 2012 MFMER | slide-2
Aim: Better tailor pelvic exam education for undifferentiated medical students Image from: Undergraduate Medical Education Committee Faculty. Association of Professors of Gynecology and Obstetrics. Clinical Skills Curriculum: Pelvic Exam. 2011. Available at: https: //www. apgo. org/education/clinical/pelvic-exam. html. Accessed January 20, 2014. © 2012 MFMER | slide-3
www. APGO. org © 2012 MFMER | slide-4
© 2012 MFMER | slide-5
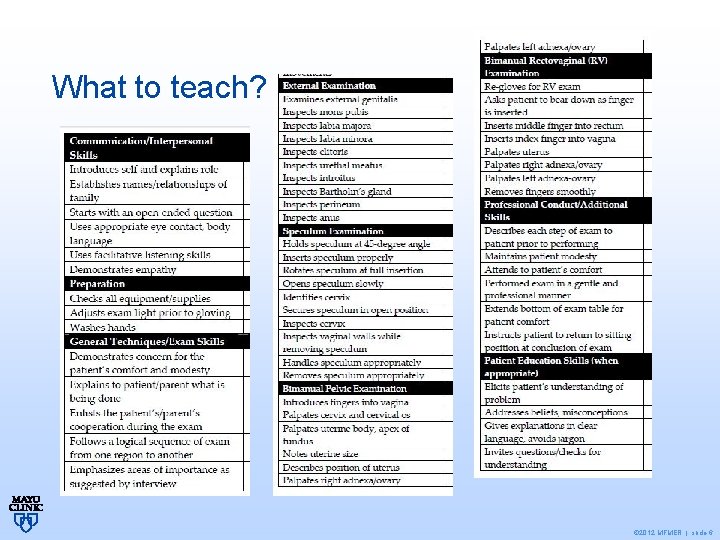
What to teach? © 2012 MFMER | slide-6
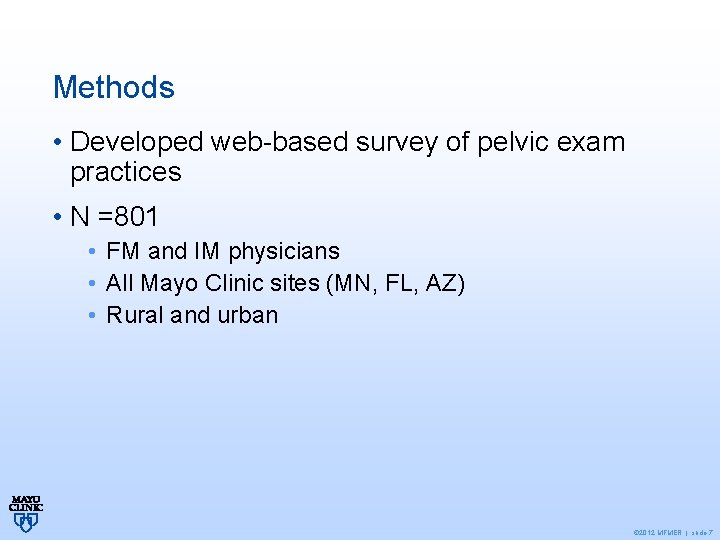
Methods • Developed web-based survey of pelvic exam practices • N =801 • FM and IM physicians • All Mayo Clinic sites (MN, FL, AZ) • Rural and urban © 2012 MFMER | slide-7
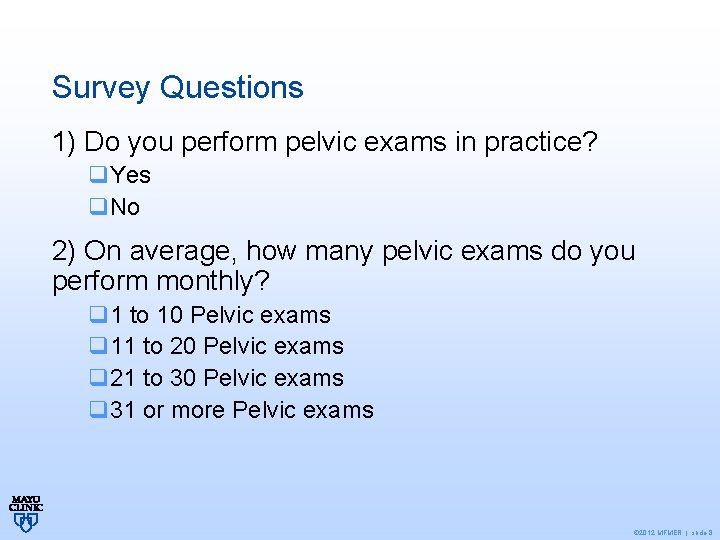
Survey Questions 1) Do you perform pelvic exams in practice? q. Yes q. No 2) On average, how many pelvic exams do you perform monthly? q 1 to 10 Pelvic exams q 11 to 20 Pelvic exams q 21 to 30 Pelvic exams q 31 or more Pelvic exams © 2012 MFMER | slide-8
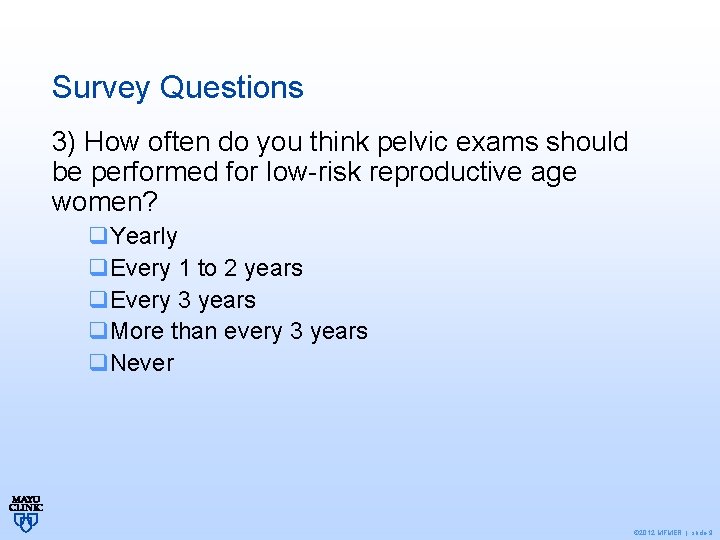
Survey Questions 3) How often do you think pelvic exams should be performed for low-risk reproductive age women? q. Yearly q. Every 1 to 2 years q. Every 3 years q. More than every 3 years q. Never © 2012 MFMER | slide-9
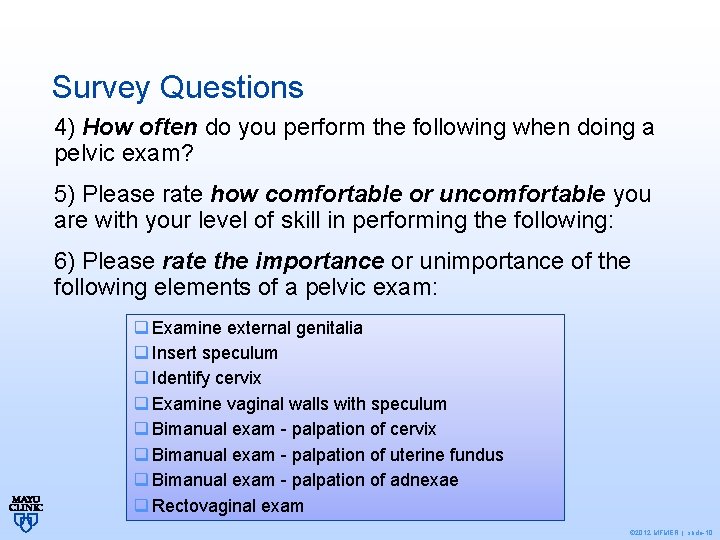
Survey Questions 4) How often do you perform the following when doing a pelvic exam? 5) Please rate how comfortable or uncomfortable you are with your level of skill in performing the following: 6) Please rate the importance or unimportance of the following elements of a pelvic exam: q Examine external genitalia q Insert speculum q Identify cervix q Examine vaginal walls with speculum q Bimanual exam - palpation of cervix q Bimanual exam - palpation of uterine fundus q Bimanual exam - palpation of adnexae q Rectovaginal exam © 2012 MFMER | slide-10
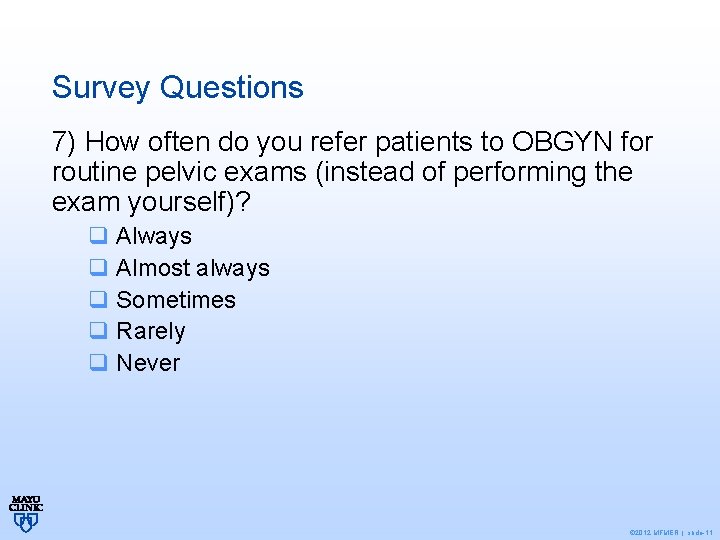
Survey Questions 7) How often do you refer patients to OBGYN for routine pelvic exams (instead of performing the exam yourself)? q Always q Almost always q Sometimes q Rarely q Never © 2012 MFMER | slide-11
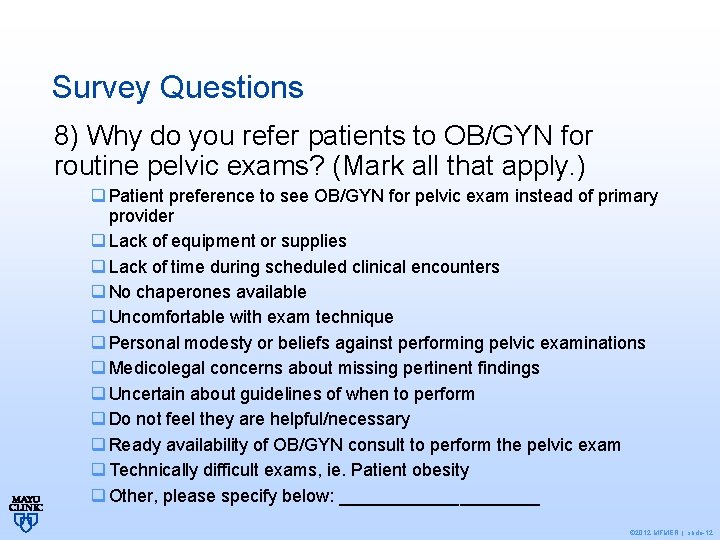
Survey Questions 8) Why do you refer patients to OB/GYN for routine pelvic exams? (Mark all that apply. ) q Patient preference to see OB/GYN for pelvic exam instead of primary provider q Lack of equipment or supplies q Lack of time during scheduled clinical encounters q No chaperones available q Uncomfortable with exam technique q Personal modesty or beliefs against performing pelvic examinations q Medicolegal concerns about missing pertinent findings q Uncertain about guidelines of when to perform q Do not feel they are helpful/necessary q Ready availability of OB/GYN consult to perform the pelvic exam q Technically difficult exams, ie. Patient obesity q Other, please specify below: __________ © 2012 MFMER | slide-12
Methods • <5 years experience = “less experienced” (LE) • >5 years = “more experienced” (ME) • Scaled items combined for analysis: • Frequency: “always” + “most of the time” • Comfort: “Very comfortable” + “somewhat comfortable” • Importance: “Very important” + “somewhat important” • LE vs. ME providers compared with Wilcoxon rank-sum tests • P <0. 05 considered significant © 2012 MFMER | slide-13
Results • 284 responses (36% response rate) • FM = 154 vs. IM = 130 • 38% LE vs. 62% ME • 97% routinely perform pelvic exams • 10% refer to Ob/Gyn solely for routine exams • Most common reasons for referral: • patient preference (N=81) • technically difficult exams (N=66) • lack of time (N=20) © 2012 MFMER | slide-14
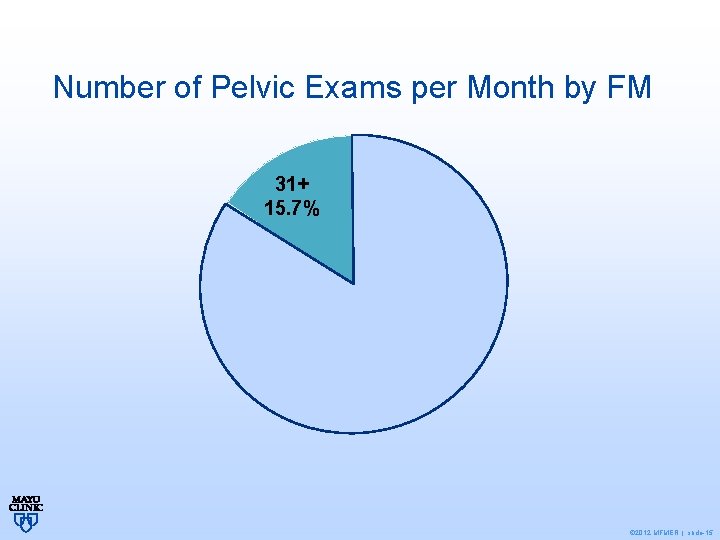
Number of Pelvic Exams per Month by FM 31+ 15. 7% 1 to 10 39. 2% 21 to 30 19. 0% 11 to 20 26. 1% © 2012 MFMER | slide-15
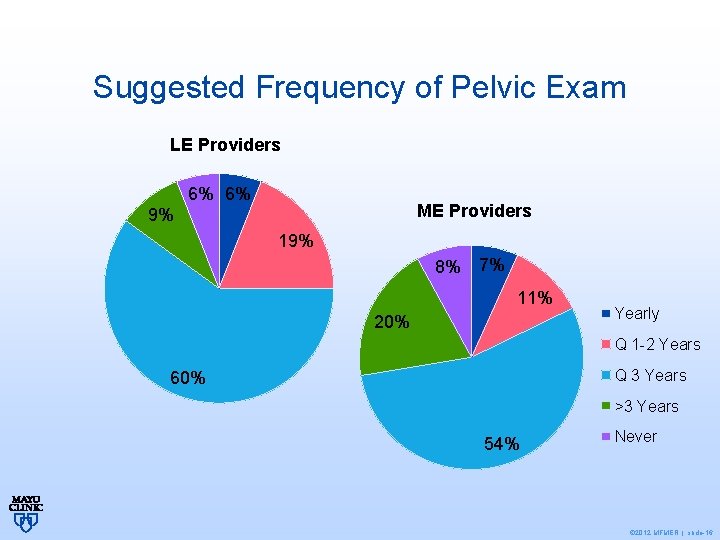
Suggested Frequency of Pelvic Exam LE Providers 6% 6% ME Providers 9% 19% 8% 7% 11% 20% Yearly Q 1 -2 Years Q 3 Years 60% >3 Years 54% Never © 2012 MFMER | slide-16
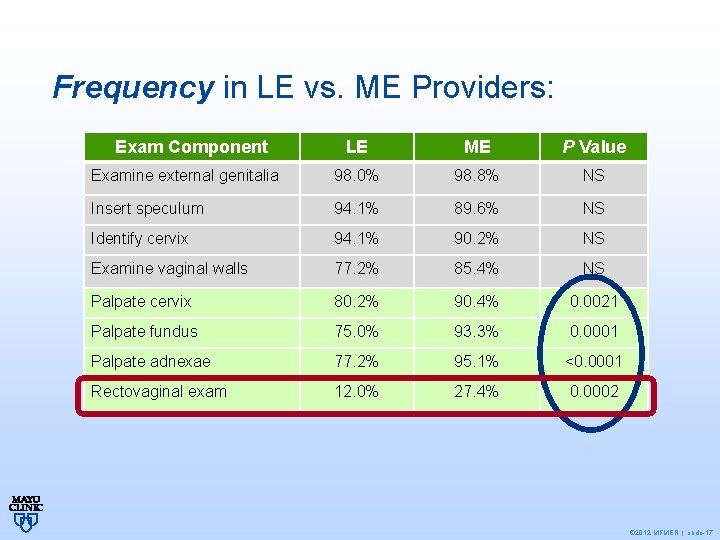
Frequency in LE vs. ME Providers: Exam Component LE ME P Value Examine external genitalia 98. 0% 98. 8% NS Insert speculum 94. 1% 89. 6% NS Identify cervix 94. 1% 90. 2% NS Examine vaginal walls 77. 2% 85. 4% NS Palpate cervix 80. 2% 90. 4% 0. 0021 Palpate fundus 75. 0% 93. 3% 0. 0001 Palpate adnexae 77. 2% 95. 1% <0. 0001 Rectovaginal exam 12. 0% 27. 4% 0. 0002 © 2012 MFMER | slide-17
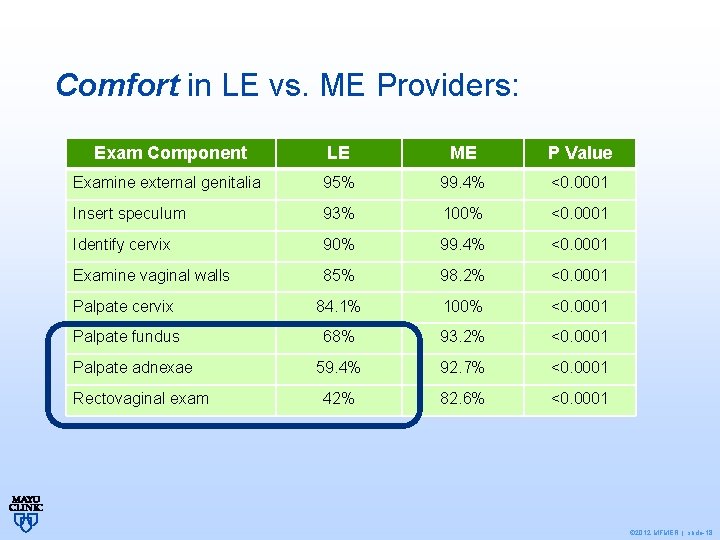
Comfort in LE vs. ME Providers: Exam Component LE ME P Value Examine external genitalia 95% 99. 4% <0. 0001 Insert speculum 93% 100% <0. 0001 Identify cervix 90% 99. 4% <0. 0001 Examine vaginal walls 85% 98. 2% <0. 0001 Palpate cervix 84. 1% 100% <0. 0001 Palpate fundus 68% 93. 2% <0. 0001 59. 4% 92. 7% <0. 0001 42% 82. 6% <0. 0001 Palpate adnexae Rectovaginal exam © 2012 MFMER | slide-18
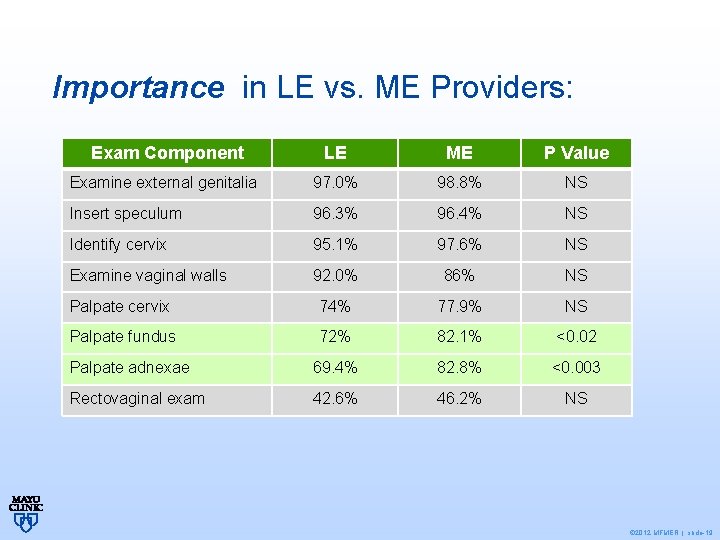
Importance in LE vs. ME Providers: Exam Component LE ME P Value Examine external genitalia 97. 0% 98. 8% NS Insert speculum 96. 3% 96. 4% NS Identify cervix 95. 1% 97. 6% NS Examine vaginal walls 92. 0% 86% NS Palpate cervix 74% 77. 9% NS Palpate fundus 72% 82. 1% <0. 02 Palpate adnexae 69. 4% 82. 8% <0. 003 Rectovaginal exam 42. 6% 46. 2% NS © 2012 MFMER | slide-19
Conclusions • Most PCPs perform pelvic exams • Experience matters • Better exam education more quality exams • Training should familiarize learner with all components • Training should focus on increasing comfort with high-yield pelvic exam components • Evolving guidelines may decrease learning opportunities for LE providers © 2012 MFMER | slide-20
Rectovaginal exam • Overall performance is low • Possible reasons: • fear of causing discomfort • concern over accuracy of exam findings • Low sensitivity of rectovaginal examination? © 2012 MFMER | slide-21
Discussion • Which components are truly high yield? • Less bimanual and rectovaginal exam by LE providers: good or bad? • When to train? • How to train? © 2012 MFMER | slide-22
Teaching Modalities • Videos • NEJM Pelvic Examination 1 https: //www. youtube. com/watch? v=CCHPcl. A 9 Vmk • ACP “Patient Centered Pelvic Exam” ($49. 95) • Plastic Models • Standardized patients • Trained laywomen educators (“Gynecologic teaching associate”) • Combination 1. Edelman A, Anderson J, Lai S, Braner DAV, Tegtmeyer K. Pelvic Examination. NEJM 2007; 356: e 26 © 2012 MFMER | slide-23
Acknowledgements • Co-authors: Dr. Emily P. Barnard, Sarah M. Jenkins, Dr. Doug J. Creedon • Grant from Mayo Clinic Department of Obstetrics & Gynecology Image from: Undergraduate Medical Education Committee Faculty. Association of Professors of Gynecology and Obstetrics. Clinical Skills Curriculum: Pelvic Exam. 2011. Available at: https: //www. apgo. org/education/clinical/pelvic-exam. html. Accessed January 20, © 2012 MFMER 2014. | slide-24
- Slides: 24