DIC 1 Stephanie Emily Kevin TF DIC is



- Slides: 27
DIC 1 Stephanie, Emily, Kevin
T/F: DIC is a life-threatening disease. A. True B. False 2
T/F: The primary threat with DIC is widespread clotting throughout the body. A. True B. False 3
An RN is assessing a pt being tested for DIC. Which symptom would not be noted? A. HTN B. Oliguria C. SOB D. Paralytic ileus 4 : 15
All of the following statements regarding DIC are true except. ? A. B. C. D. The rapidity and intensity of onset is triggered by condition of patients liver, endothelium and bone marrow. The early phase may include symptoms of thrombosis. Excessive blood loss rarely results in shock Early identification is the most critical intervention 5 : 15
Coagulopathy ¢ a. k. a. a clotting disorder or bleeding disorder ¢ Impaired coagulation hemorrhage ¢ e. g. Hemophilia Thrombocytopenia Heparin overdose DIC 6
DIC - definition ¢ Disseminated intravascular coagulopathy is a bleeding disorder characterized by: 1. 2. 3. 4. inappropriate clotting trigger = the underlying disease widespread clotting = thrombosis exhaustion of normal clotting mechanisms uncontrolled bleeding = hemorrhage 7
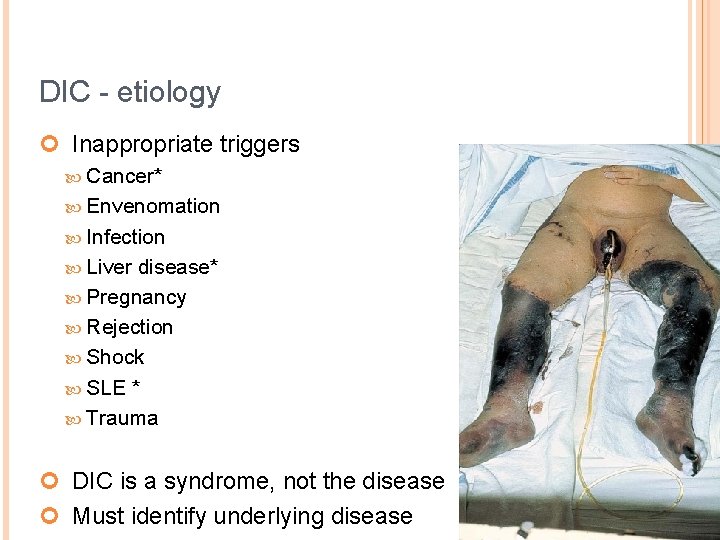
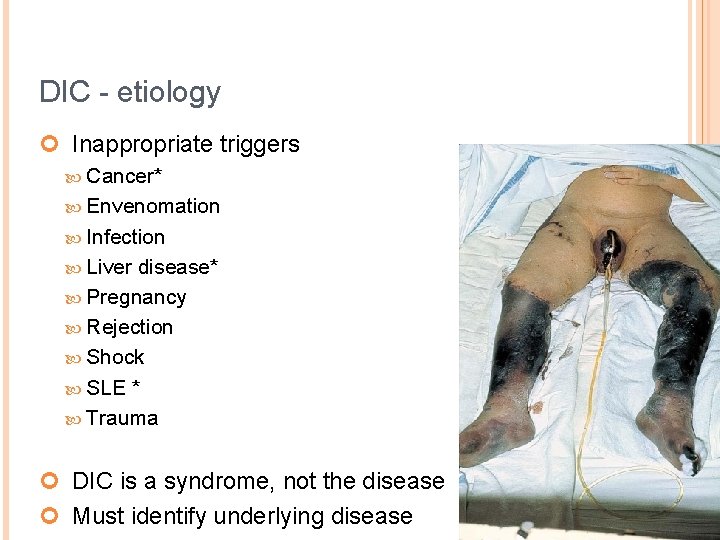
DIC - etiology ¢ Inappropriate triggers Cancer* Envenomation Infection Liver disease* Pregnancy Rejection Shock SLE * Trauma ¢ DIC is a syndrome, not the disease ¢ Must identify underlying disease 8
DIC - pathophysiology ¢ How it should work ¢ Coagulation Local damage to endothelium Platelets bind to exposed collagen Release of Tissue Factor Clotting factor cascade fibrin ¢ Fibrinolysis Plasmin cleaves fibrin Fibrin degradation products (FDPs) released ¢ e. g. , d-dimer 9
DIC - pathophysiology ¢ What happens instead ¢ Coagulation Inappropriate trigger Tissue Factor released in excess Widespread clotting Widespread ischemia, necrosis ¢ Fibrinolysis More clots means more clot busting Excess of FDPs released ¢ anticoagulant 10
DIC - pathophysiology ¢ Clotting mechanism exhausted Platelets consumed faster than replaced Clotting factors consumed faster than replaced Inability to form new clots when needed ¢ r/f hemorrhage 11
Clinical Manifestations S/S of DIC depend on cause, and whether condition is acute or chronic ¢ Acute DIC: clotting usually occurs first, followed by bleeding. But bleeding is often the first obvious sign. With acute blood loss, emergency care is needed. ¢ Blood clotting occurs with chronic DIC, and doesn’t always lead to bleeding. The condition lasts longer and may have no signs, so it wont be recognized as quickly as acute DIC ¢ 12
DIC - Clinical manifestations - Clotting ¢ Systemic clotting throughout the body’s small blood vessels. ¢ Respiratory: tachypnea, dyspnea, SOB, S/S of PE and ARDS ¢ Cardio: chest pain, EKG changes, S/S MI ¢ GI: abdominal pain, paralytic ileus ¢ GU: kidney damage, oliguria, ARF ¢ DVT: pain, redness, warmth, edema ¢ CVA: headaches, speech changes, paralysis ¢ Skin: cyanosis, ischemic tissue necrosis 13
DIC - Clinical manifestations - Bleeding ¢ Internal bleeding can occur in any organ and the bleeding can be life threatening ¢ Respiratory: tachypnea, hemoptysis, orthopnea ¢ Neuro: vision changes, dizziness, headache, change in mental status ¢ Cardio: hypotension, tachycardia ¢ GU: hematuria ¢ GI: frank/occult stool, upper and lower GI bleed ¢ Skin: purpura, petechiae, pallor, oozing, hematomas, bruising, prolonged bleeding from minor cuts ¢ Epistaxis, bleeding gums, heavy menstrual bleed 14
Diagnostic Testing CBC with blood smear ¢ APTT ¢ PT/INR ¢ Serum fibrinogen: Fibrinogen is a protein that helps the blood clot. ¢ Fibrin degradation products (fibrin split products): Product left behind when clots dissolve ¢ D-dimer: a polymer from the breakdown of fibrin ¢ Factor assays: for factors V, VIII, X, XIII ¢ 15
Nursing Assessments ¢ ¢ ¢ Petechiae, purpura, hematomas IV sites, wound sites, drains GI and GU bleeding Hemoptysis Mentation Vital Signs (hypotension, tachycardia) ¢ Pain 16

Nursing Interventions Monitor PT/INR ¢ Bleeding precautions ¢ Injury prevention ¢ Turn and Position q 2 hours to prevent pressure ¢ Administer Heparin to inhibit coagulation ¢ Decrease anxiety ¢
Nursing Diagnoses Ineffective peripheral tissue perfusion ¢ Acute Pain ¢ Decreased Cardiac Output ¢ Anxiety ¢ Risk for Injury ¢
Collaborative Care ¢ Bleeding Chronic DIC with no active bleeding-Treat underlying cause DIC with bleeding-Supportive treatment for symptom management and blood transfusion therapy and treatment of underlying cause/disease ¢ Thrombosis Heparin or Lovenox
What does the Evidence show? Transfusion therapy should be reserved for patients with life threatening hemorrhage only ¢ Patients with DIC have activated coagulation and blood transfusions pose major risks. ¢ Early identification can reduce complications ¢ Treatment of underlying disease must occur ¢ Manage inflammatory-immune response ¢ Stabilize patient and achieve hemostasis ¢ Inflammation activates coagulation so all patients with injury, sepsis, trauma or systemic inflammation have altered coagulation and require careful and close monitoring ¢ ¢ (Dressler, 2012)
DIC Summary slide 1. DIC includes 2 life-threatening conditions: widespread clotting uncontrollable hemorrhage*** 2. 3. Clinical s/s include both clotting and bleeding. Be aware of the changes that occur in both situations Identify and treat the underlying condition Supportive care for human needs related to bleeding (Transfusion for critical cases only) Anticoagulants for Thrombosis DIC. 21
T/F: DIC is a life-threatening disease. A. B. True False 22

T/F: The primary threat with DIC is widespread clotting throughout the body. A. B. True False 23
An RN is assessing a pt being tested for DIC. Which symptom would not be noted? A. B. C. D. HTN Oliguria SOB Paralytic ileus 24 : 15
Something about DIC collaborative care? 25 : 15
Q&A ¢ Anything needing further explanation? ¢ Feelings to be shared? 26

References ¢ Dressler, D. (2012). Coagulopathy in the intensive care unit. Critical Care Nurse, 32 (5). 48 -60. ¢ Frazier, T. (2012). Disseminated intravascular coagulation and implications for medical-surgical nurses. Med-Surg Matters, 21(3/4), 8 -11. ¢ Hinds, M. H. , Hyland, J. R. , Lovric, A. , Nibert, Ainslie, & Upchurch, S. (2011). HESI comprehensive review for the NCLEX-RN examination (3 rd ed. ). St. Louis, MO: Elsevier. ¢ Lewis, S. L. , Dirksen, S. R. , Heitkemper, M. M. , Bucher, L. , & Camera, I. M. (2011). Medical-surgical nursing: Assessment and management of clinical problems. Saint Louis, MO: Elsevier Mosby. ¢ NIH/Medline. Plus. (2014, February 5). Disseminated Intravascular Coagulation (DIC). Retrieved from http: //www. nlm. nih. gov/medlineplus/ency/article/000573. htm 27