Diathermy Kenny Low Dec 2009 Urology registrar Thursday

- Slides: 12
Diathermy Kenny Low Dec 2009 Urology registrar Thursday teaching
Overview n n n Electrical properties Mechanism of electrosurgery Cutting versus coagulation Return pad Capacitors Ligasure/Argon beam coagulators

Electrical terms n n Voltage: potential difference providing force to push current through resistance Current: flow of electrons during a period of time Resistance: obstacle to current flow Circuit: pathway for current flow
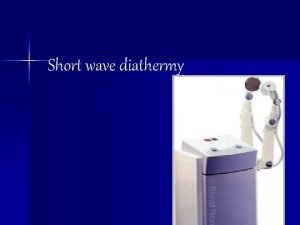
Mechanism of eletrosurgery n Frequency of current flow ¡ ¡ ¡ n n Power point 50 Hz (50 cycles/s) Nerve and muscle stimulation – cease at 100 k. Hz Electrosurgery – frequency 200 k. Hz + (300 -3000 k. Hz) (allows current flow without stimulation of nerve and muscles) Circuit (monopolar) – generator, active electrode (diathermy pen), patient, return electrode (diathermy pad) Bipolar – active and return electrode between two tines of forceps
Cutting versus coagulation n n Different waveforms create different tissue effects Cutting current ¡ ¡ n Coagulation current ¡ ¡ ¡ n Intermittent waveform (“on” time reduced) Less heat produced – coagulum rather than vaporisation Higher voltages Blends ¡ ¡ ¡ n Constant waveform Heat produced quickly – vaporisation of tissue Modification of on/off time Blend 1 50/50 (on/off) Blend 2 40/60 Blend 3 25/75 Coagulation 6/94 Cutting/fulguration/dessication ¡ ¡ ¡ Cutting – spark, producing maximal current density Fulguration – sparking with coagulation waveform, char and coagulum over wide area Dessication – contact with tissue. Current density reduced by doing this – cell drying
Return pad n n Vital to safety: completes the circuit to allow current back to ground Current will always seek ground through the most conductive object – may not be the return pad ¡ Problems n n RF current division (part of current returns to ground through an alternative circuit). Leads to alternate site burns (e. g. ECG electrodes) Solution: isolated systems – circuit must be completed by the generator
Return pad n Pad site burns ¡ Problems: burn = current X time / area n n n Pad site needs sufficient area and conductivity to safely remove current without producing excess heat Only difference between active electrode and return electrode is relative size and conductivity Solution: Return electrode monitoring (REM) ¡ ¡ Actively monitor impedence at pad site, direct relationship between impedence and pad site contact area Seen with the split return pads (two separate areas – impendence current/a second circuit flows through return pad)
Dangers and Precautions n n n n aim of diathermy safety should be to prevent mains voltage from entering the patient circuit care with use on pedunculated structures flammable anaesthetic gases – sparks prohibited within 25 cm of gases electrocution alcohol preps gas accumulation within the bladder poor plate to patient contact – thermoelectric burn
Dangers and Precautions n suboptimal effectiveness – do not increase power, check ¡ ¡ ¡ n n n n n faulty foot switch connection faulty active electrode poor plate / patient contact cable problem internal failure of the machine incorrect solution diathermy burns with earthed machine – ECG dots noise activation care with placement of plate and place as close as possible to operative site all parts of cable insulated avoid saline – conducts current and therefore no cutting effect other OT equipment metallic parts of light cables, video cameras are earth free and therefore safe pacemakers usually show little or no response to diathermy however 2 types may give rise to problems ¡ ¡ the demand pacemaker synchronous P wave pacemaker for heartblock
Minimal access surgery n n n Direct coupling – e. g. touching diathermy to forceps in open surgery, accidentally energising secondary instrument out of view Insulation failures: sparks through insulation, worse with high voltages (i. e. high coagulation settings) Capacitor: can occur when a two conductors are separated by a non conductor (e. g. metal electrode tip, insulation, metal cannula) ¡ ¡ Current through electrode tip and induce current in metal cannula via electrostatic field Plastic systems reduce capacitance but the patients body can act as the seconductor
Ligasure/ABC n n Ligasure Bipolar technology – feedback response, reliable seal created for vessels up to 7 mm n n n Initial resistance measured Pulsed energy with continuous feedback Ceased when tissue response complete Said to have less thermal spread than conventional bipolar and comparable to ultrasonic coagulation Comparable seal to sutures or clips (mechanical ligation)
Ligasure/ABC n n n ABC (argon beam coagulation) Argon – noble gas, heavier than air, cheap, non combustable Ionises with radiofrequency energy Provides a stream of electrical current to the tissues Advantages ¡ ¡ ¡ Less smoke Non contact coagulation Decreased blood loss, argon gas blows away blood at bleeding site Less tissue damage Flexible eschar