Diarrhoea and vomiting in children under 5 Implementing

- Slides: 17
Diarrhoea and vomiting in children under 5 Implementing NICE guidance 2009 NICE clinical guideline 84
What this presentation covers Background Key priorities for implementation Costs and savings Discussion Find out more
Background • Approximately 10% of children younger than 5 years present to healthcare services each year with gastroenteritis. This puts a significant burden on health service resources. • Parents and carers need to know how to recognise dehydration and shock. • There is variation in clinical practice.
Key priorities for implementation • Diagnosis • Assessing dehydration and shock • Fluid management • Nutritional management • Information and advice for parents and carers
Diagnosis Perform stool microbiological investigations if: • you suspect septicaemia or • there is blood and/or mucus in the stool or • the child is immunocompromised.
Assessing dehydration and shock: those at increased risk • Infants, especially < 6 months • Infants who were of low birth weight • Children who have passed six or more diarrhoeal stools or vomited three or more times in the previous 24 hours • Children who have not had/not tolerated supplementary fluids • Infants who have stopped breastfeeding during the illness • Children with signs of malnutrition
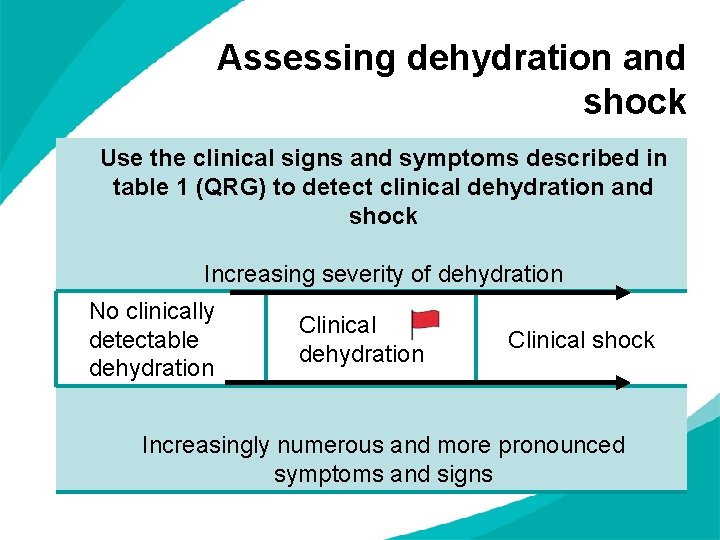
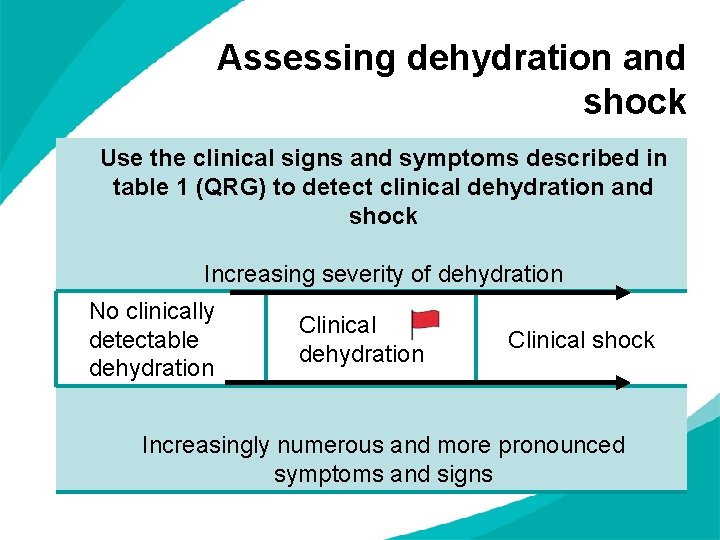
Assessing dehydration and shock Use the clinical signs and symptoms described in table 1 (QRG) to detect clinical dehydration and shock Increasing severity of dehydration No clinically detectable dehydration Clinical shock Increasingly numerous and more pronounced symptoms and signs
Fluid management: children without dehydration In children with gastroenteritis but without clinical dehydration: • continue breastfeeding and other milk feeds • encourage fluid intake • discourage the drinking of fruit juices and carbonated drinks, especially in those at increased risk • offer oral rehydration salt (ORS) solution as supplemental fluid to those at increased risk.
Fluid management: children with dehydration In children with clinical dehydration, including hypernatraemic dehydration: • use low-osmolarity ORS solution frequently and in small amounts • give 50 ml/kg for fluid deficit replacement over 4 hours as well as maintenance fluid • consider supplementation with their usual fluids • Consider a nasogastric tube if they cannot drink ORS solution or vomit persistently • monitor response regularly.
Fluid management: when to use intravenous fluid Use intravenous fluid therapy for clinical dehydration if: • shock is suspected or confirmed • a child with red flag symptoms or signs shows clinical evidence of deterioration despite oral rehydration therapy • a child persistently vomits the ORS solution, given orally or via a nasogastric tube.
Fluid management: giving intravenous fluid therapy • use isotonic solution for fluid deficit replacement and maintenance • in addition to maintenance fluid requirements, add the following amounts for fluid deficit replacement: 100 ml/kg for those who were initially shocked 50 ml/kg for those who were not shocked at presentation • monitor blood plasma levels at the outset and regularly, and review administration rate • consider providing intravenous potassium once the plasma potassium level is known.

Nutritional management After rehydration: • give full-strength milk straight away • reintroduce the child’s usual solid food • avoid giving fruit juice and fizzy drinks until the diarrhoea has stopped.
Information and advice: hygiene Advise parents and carers to: • wash and carefully dry hands as this is the best way to prevent the spread of gastroenteritis • wash hands after going to the toilet or changing nappies and before preparing, serving or eating food • avoid sharing towels used by infected children.
Information and advice: school, childcare and activities Advise parents and carers to keep children away from: • school or other childcare facility - while they have diarrhoea or vomiting caused by gastroenteritis and - for at least 48 hours after the last episode • swimming in swimming pools for 2 weeks after the last episode
Costs and savings It is unlikely this guideline will result in a significant change in resource use in the NHS. There may be future reduction in hospital admissions and laboratory investigations of the stool, which should be more selective. There is expected to be an increase in the use of ORS relative to intravenous therapy with the emphasis on administration of ORS either orally or via nasogastric tube.
Discussion • How can we ensure that only necessary stool microbiological testing is requested? • How can we promote the appropriate use of oral rehydration therapy and reduce inappropriate intravenous therapy? • How can we ensure that primary and secondary care work together to put these recommendations into practice? • Which audiences need information about the condition and how to prevent the spread of infection, and how can we reach them?
Find out more Visit www. nice. org. uk/CG 84 for: • • the guideline the quick reference guide ‘Understanding NICE guidance’ costing statement audit support assessing dehydration chart advice for parents