DIAGNSTICO Y TRATAMIENTO DE DENGUE CHIKUNGUNYA Y ZIKA
- Slides: 47
DIAGNÓSTICO Y TRATAMIENTO DE DENGUE, CHIKUNGUNYA Y ZIKA LUIS J. LUGO VÉLEZ M. D. J. D. LL. M. FCLM ASSISTANT PROFESSOR PONCE HEALTH SCIENCES UNIVERSITY SCHOOL OF MEDICINE ADJUNCT FACULTY PONTIFICAL CATHOLIC UNIVERSITY SCHOOL OF LAW
DENGUE THE VIRUS • Dengue virus (DEN) is a small single-stranded RNA virus comprising four distinct serotypes (DEN-1 to -4). • These closely related serotypes of the dengue virus belong to the genus Flavivirus, family Flaviviridae.
CHIKUNGUNYA • Chikungunya virus (CHIKV), an alphavirus in the family Togaviriade, was first discovered in Tanzania in 1953. • It is closely related to Ross River Virus, O’Nyong virus, and Semliki Forest Virus. • CHIKV is transmitted in a personto-mosquito-to-person transmission cycle.
VIRUS DEL ZIKA • • ARN de cadena simple • Familia Flaviviridae • Estrechamente relacionado a otros virus: • Dengue • Virus del Nilo Occidental • Fiebre amarilla • Encefalitis japonesa • Primer reporte en 1947, Uganda en el Bosque de Zika (monos) Género Flavivirus
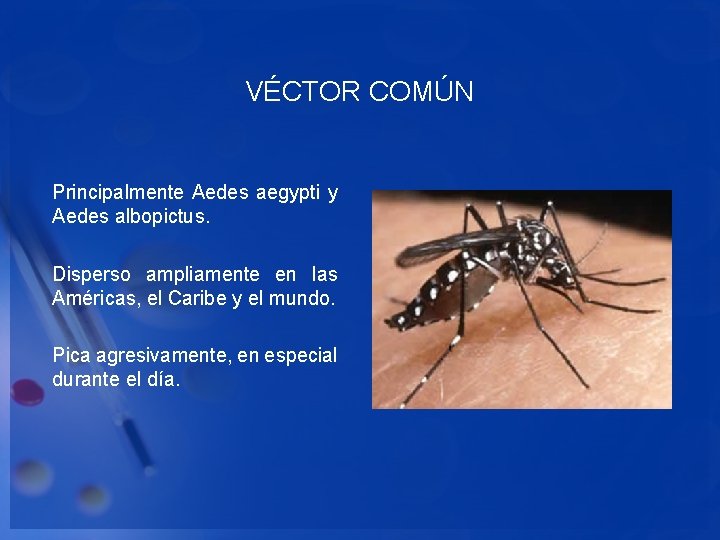
VÉCTOR COMÚN Principalmente Aedes aegypti y Aedes albopictus. Disperso ampliamente en las Américas, el Caribe y el mundo. Pica agresivamente, en especial durante el día.
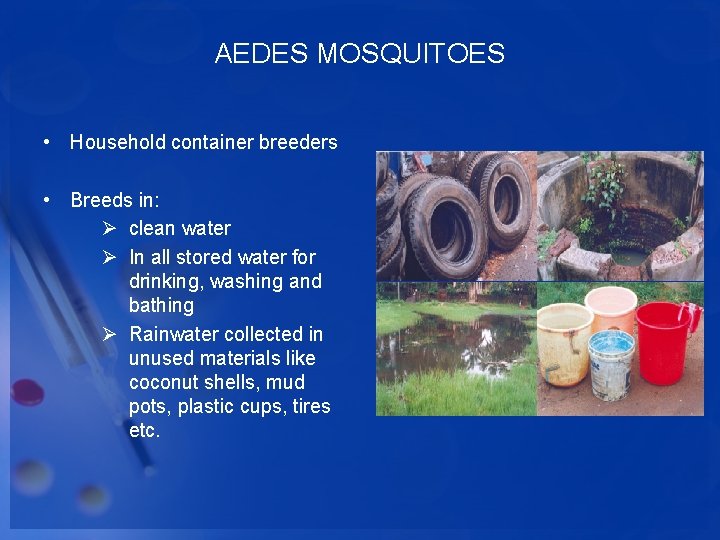
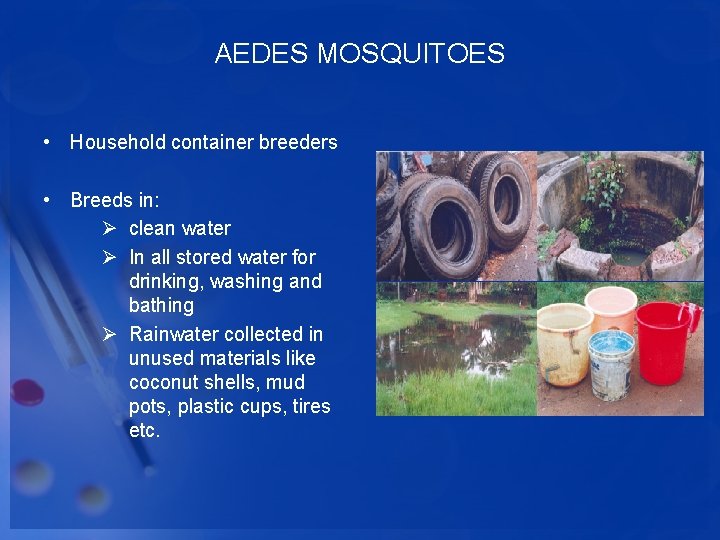
AEDES MOSQUITOES • Household container breeders • Breeds in: Ø clean water Ø In all stored water for drinking, washing and bathing Ø Rainwater collected in unused materials like coconut shells, mud pots, plastic cups, tires etc.
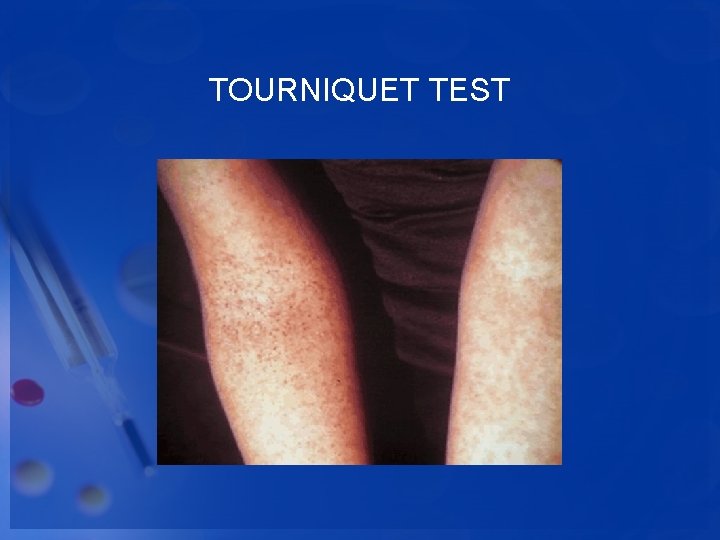
DENGUE Febrile phase • Patients typically develop high-grade fever suddenly. • This acute febrile phase usually lasts 2– 7 days and is often accompanied by facial flushing, skin erythema, generalized body ache, myalgia, arthralgia and headache. Some patients may have sore throat, injected pharynx and conjunctival injection. Anorexia, nausea and vomiting are common. • It can be difficult to distinguish dengue clinically from non-dengue febrile diseases in the early febrile phase. • A positive tourniquet test in this phase increases the probability of dengue
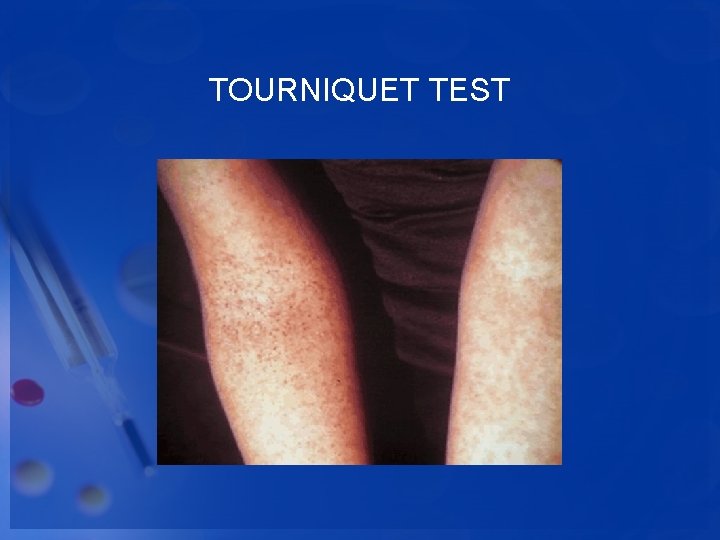
TOURNIQUET TEST
DENGUE Febrile phase • Mild hemorrhagic manifestations like petechiae and mucosal membrane bleeding (e. g. nose and gums) may be seen. • Massive vaginal bleeding (in women of childbearing age) and gastrointestinal bleeding may occur during this phase but is not common. • The liver is often enlarged and tender after a few days of fever. • The earliest abnormality in the full blood count is a progressive decrease in total white cell count, which should alert the physician to a high probability of dengue.
DENGUE Critical Phase Around the time of de-fervescence, when the temperature drops to 37. 5– 38°C or less and remains below this level, usually on days 3– 7 of illness, an increase in capillary permeability in parallel with increasing hematocrit levels may occur. This marks the beginning of the critical phase. The period of clinically significant plasma leakage usually lasts 24– 48 hours.
DENGUE Critical Phase • Progressive leukopenia followed by a rapid decrease in platelet count usually precedes plasma leakage. • At this point patients without an increase in capillary permeability will improve, while those with increased capillary permeability may become worse as a result of lost plasma volume. • The degree of increase above the baseline hematocrit often reflects the severity of plasma leakage.
DENGUE • Shock occurs when a critical volume of plasma is lost through leakage. It is often preceded by warning signs. • The body temperature may be subnormal when shock occurs. With prolonged shock, the consequent organ hypoperfusion results in progressive organ impairment, metabolic acidosis and disseminated intravascular coagulation. • This in turn leads to severe hemorrhage causing the hematocrit to decrease in severe shock. Instead of the leukopenia usually seen during this phase of dengue, the total white cell count may increase in patients with severe bleeding.
DENGUE • Those who improve after de-fervescence are said to have nonsevere dengue. • Some patients progress to the critical phase of plasma leakage without de-fervescence and, in these patients, changes in the full blood count should be used to guide the onset of the critical phase and plasma leakage. • Those who deteriorate will manifest with warning signs. This is called dengue with warning signs. • Cases of dengue with warning signs will probably recover with early intravenous rehydration. Some cases will deteriorate to severe dengue.
DENGUE Recovery phase • If the patient survives the 24– 48 hour critical phase, a gradual reabsorption of extravascular compartment fluid takes place in the following 48– 72 hours. • General well-being improves, appetite returns, gastrointestinal symptoms abate, haemodynamic status stabilizes and diuresis ensues. Some patients may have a rash of “isles of white in the sea of red” . Some may experience generalized pruritus. Bradycardia and electrocardiographic changes are common during this stage. • The hematocrit stabilizes or may be lower due to the dilutional effect of reabsorbed fluid. White blood cell count usually starts to rise soon after de-fervescence but the recovery of platelet count is typically later than that of white blood cell count.
SEVERE DENGUE • Severe dengue is defined by one or more of the following: Ø plasma leakage that may lead to shock (dengue shock) and/or fluid accumulation, with or without respiratory distress, and/or Ø severe bleeding, and/or Ø severe organ impairment.
SEVERE DENGUE • Severe dengue should be considered if the patient is from an area of dengue risk presenting with fever of 2– 7 days plus any of the following features: • There is evidence of plasma leakage such as: – high or progressively rising haematocrit; – pleural effusions or ascites; clammy extremities, capillary refill time greater than three seconds, weak or undetectable pulse, narrow pulse pressure or, in late shock, un-recordable blood pressure).
SEVERE DENGUE • There is significant bleeding. • There is an altered level of consciousness (lethargy or restlessness, coma, convulsions). • There is severe GI involvement (persistent vomiting, increasing or intense abdominal pain, jaundice). • There is severe organ impairment (acute liver failure, acute renal failure, encephalopathy or encephalitis, or other unusual manifestations, cardiomyopathy
DENGUE DIAGNOSIS • Laboratory diagnosis methods for confirming dengue virus infection may involve detection of the virus, viral nucleic acid, antigens or antibodies, or a combination of these techniques.
DENGUE TREATMENT • Fortunately, this viral disease is usually self-limited and usually adequate hydration and pain control will help the person through the infection. • NSAIDs and aspirin should be avoided because of the tendency of the dengue viruses to cause hemorrhages. • More severe variations of dengue fever (hemorrhagic and shock syndrome) usually require additional supportive treatments; these patients often require hospitalization. IV hydration, blood transfusions, platelet transfusions, blood pressure support, and other intensive-care measures may need to be utilized in these patients.
CHIKUNGUNYA • Not every person infected with CHIKV exhibits symptoms. • It is estimated that 3% to 28% of those infected are asymptomatic. • However, these people are still capable of transmitting the disease.
CHIKUNGUNYA: CLINICAL “Dengue with arthritis” • Incubation period: 3‐ 7 days (range: 2‐ 12) • Symptoms Ø Fever ‐usually ends abruptly after 2 days Ø Arthralgia/arthritis, insomnia and prostration ‐last up to a week Ø rash, conjunctivitis, photophobia, fatigue • In middle age, joint pains may last 4‐ 10 weeks, longer in elderly • Rarely fatal
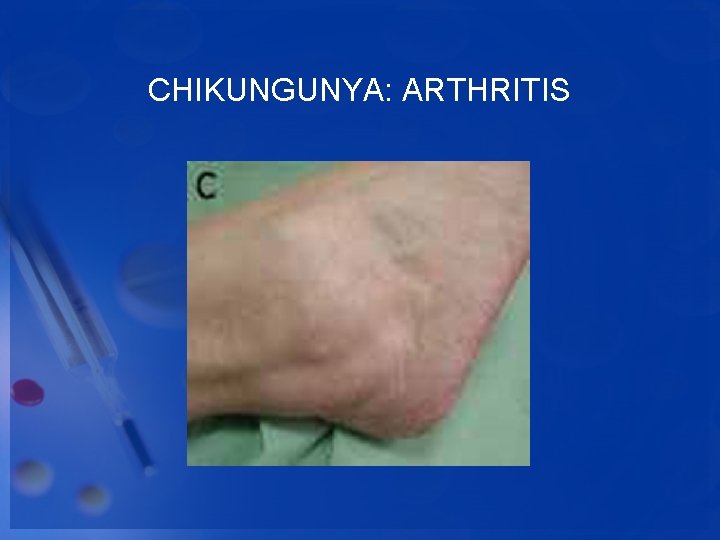
CHIKUNGUNYA: CLINICAL ARTHRITIS & ARTHRALGIA • Painful swelling of the joints tends to occur bilaterally on the extremities. • Polyarthralgias and arthritis most commonly occur in joints of the hands, feet, wrists, ankles, elbows or knees. • Chikungunya fever often causes arthralgia or arthritis (pain with swelling) that is more severe than that caused by dengue fever.
CHIKUNGUNYA: CLINICAL ARTHRITIS & ARTHRALGIA • Neck pain and lower back pain is also more common than with dengue fever. • Swelling may be visible and can be a sign of arthritis. • Tenosynovitis (inflammation of the sheaths that surround tendons) may also occur. • Patients are often bed-ridden and completely incapacitated
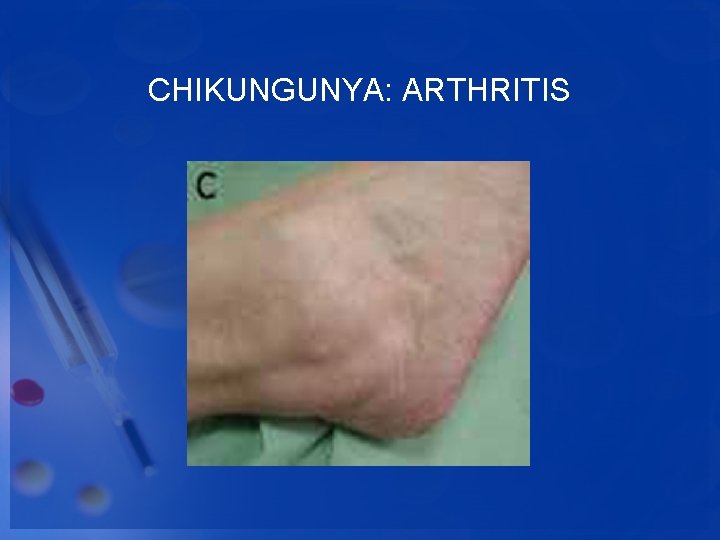
CHIKUNGUNYA: ARTHRITIS
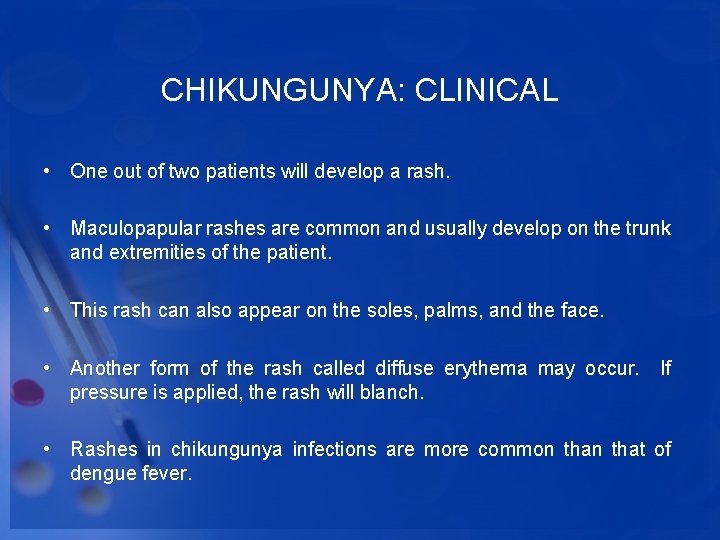
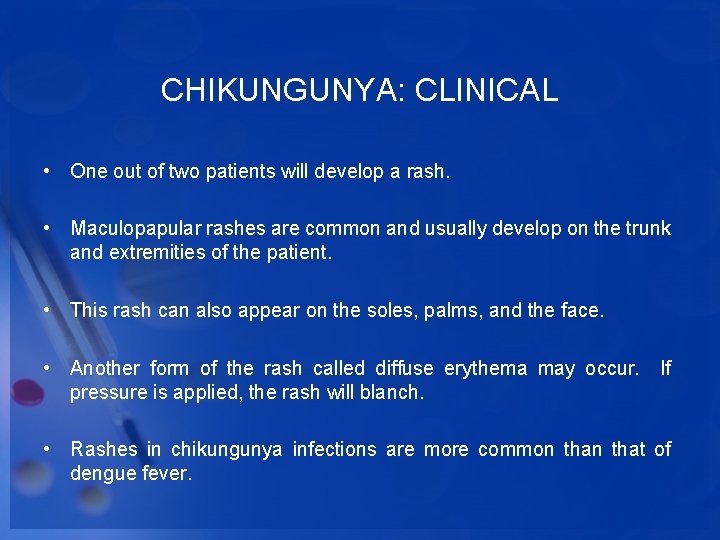
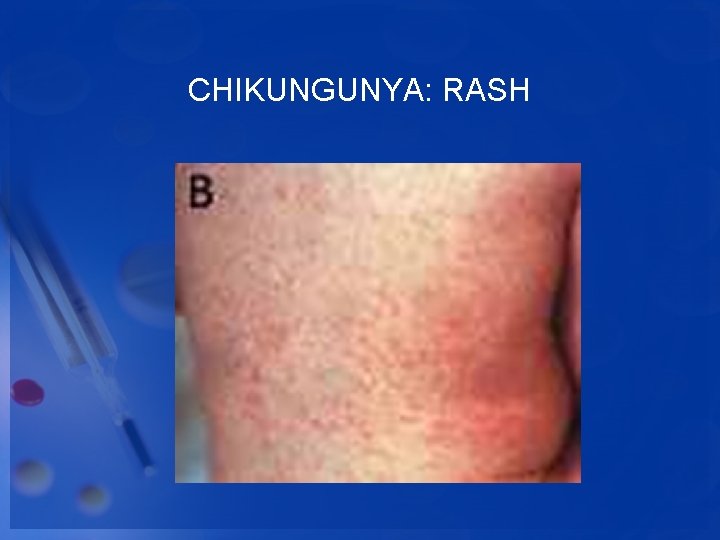
CHIKUNGUNYA: CLINICAL • One out of two patients will develop a rash. • Maculopapular rashes are common and usually develop on the trunk and extremities of the patient. • This rash can also appear on the soles, palms, and the face. • Another form of the rash called diffuse erythema may occur. If pressure is applied, the rash will blanch. • Rashes in chikungunya infections are more common that of dengue fever.
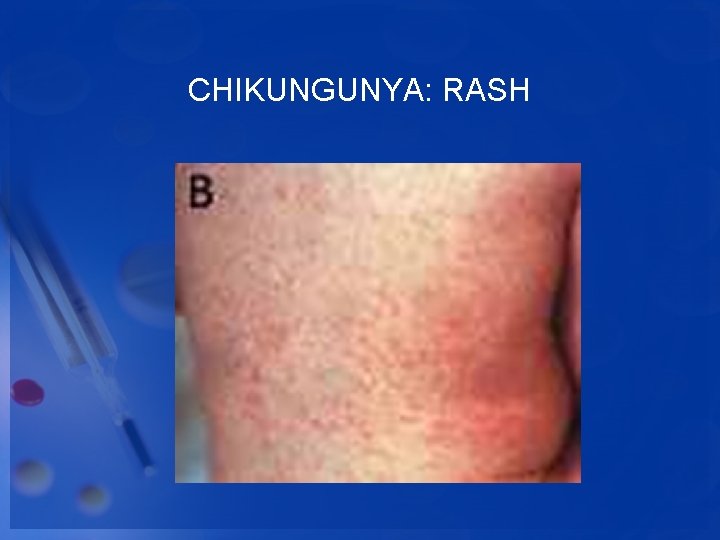
CHIKUNGUNYA: RASH
CHIKUNGUNYA: CLINICAL • Fever usually disappears after 2 -3 days. • Muscle and joint pain, which can be very severe usually lasts for about 5 -7 days but in some cases for much longer periods. • Elderly patients in particular may suffer muscle and joint pain for several months.
CHIKUNGUNYA DIAGNOSIS • Laboratory diagnosis is generally accomplished by testing serum or plasma to detect virus, viral nucleic acid, or virus-specific immunoglobulin (Ig) M and neutralizing antibodies.
CHIKUNGUNYA TREATMENT • There is no vaccine or specific treatment available against CHIK V infection. • Fortunately, the illness is usually self-limiting and resolves with time. • Supportive therapy with antipyretics are used to control fever and joint pain.
CHIKUNGUNYA • • PUERTO RICO-OCTUBRE 2014 18, 000 casos sospechosos 5 muertes • 4 personas que al fallecer estaban contagiadas con el virus, lo que no quiere decir que ésta fuera la causa directa del deceso • 1 recién nacido que murió al contagiarse con el virus durante el parto; la madre presentaba síntomas 3, 383 casos doblemente comprobados con el CDC 31 casos que se cree fueron contraídos fuera de P. R.
Zika • 1 de cada 5 (80%) personas infectadas desarrollan síntomas • Afecta todos los grupos de edad • Rara vez enfermedad severa, hospitalizaciones, o muerte • Periodo de incubación usualmente 3– 12 días • Síntomas típicamente duran 2 -7 días
ZIKA CICLO PRIMARIO DE TRANSMISIÓN • • • Transmisión antroponótica • persona a mosquito a persona Otras modalidades de transmisión de Zika • Materno -fetal • Intra-uterino • Perinatal • Contacto sexual: hombre-mujer • Transfusión de sangre • Exposición laboratorio No hay evidencia de transmisión • Trasplante de órganos o tejido • Lactancia • Saliva • Orina
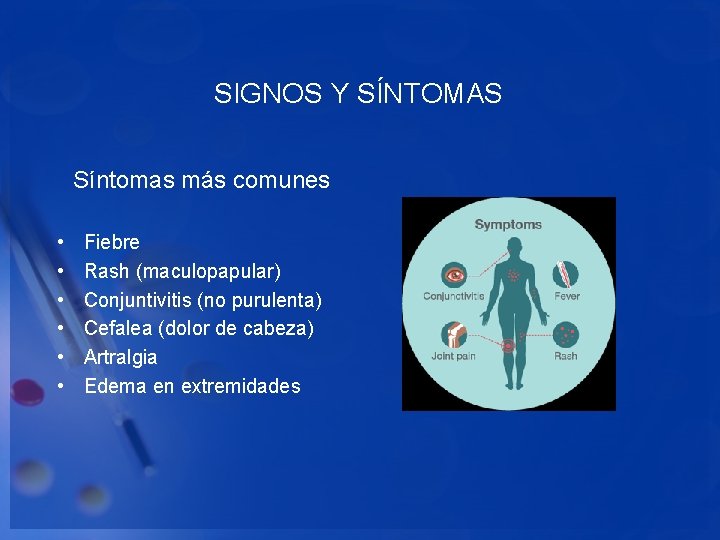
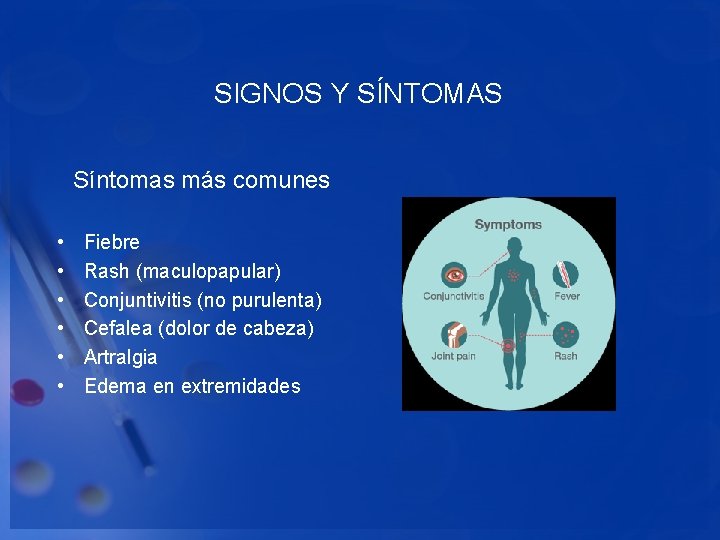
SIGNOS Y SÍNTOMAS Síntomas más comunes • • • Fiebre Rash (maculopapular) Conjuntivitis (no purulenta) Cefalea (dolor de cabeza) Artralgia Edema en extremidades
OTROS SIGNOS Y SÍNTOMAS • Mialgia • Nausea / Vómitos • Anorexia • Dolor abdominal • Dolor retro-orbital
MANEJO CLÍNICO • No hay terapia antiviral específica • Hidratación y estabilidad hemodinámica • Otras condiciones que pudiesen comprometer el tratamiento o manejo del caso • Muestras para diagnóstico • Manejar como dengue hasta descartar la posibilidad de infección por dengue • Reduce riesgo de enfermedad severa y muerte • NO usar aspirina y anti-inflamatorios no esteroidales (NSAIDs), aumentan el riesgo de hemorragias en pacientes con dengue
DESPUÉS DE UNA INFECCIÓN CON ZIKA • Inmunidad de por vida • Conocimiento limitado sobre secuela tras infección • Defectos congénitos: Microcefalia • Guillian-Barré
ORGANIZACIÓN MUNDIAL DE LA SALUD 1/FEBRERO/2016 • Emergencia de Salud Pública de Importancia Internacional • Motivos convincentes para sospechar una relación causal entre la microcefalia y la infección por el virus de Zika en el embarazo, aunque todavía no se ha demostrado científicamente. • Necesidad urgente de coordinar los esfuerzos internaciones para investigar y entender mejor esta relación. • Las medidas de protección más importantes son el control de los mosquitos y la prevención de sus picaduras a las personas en riesgo, especialmente las embarazadas.
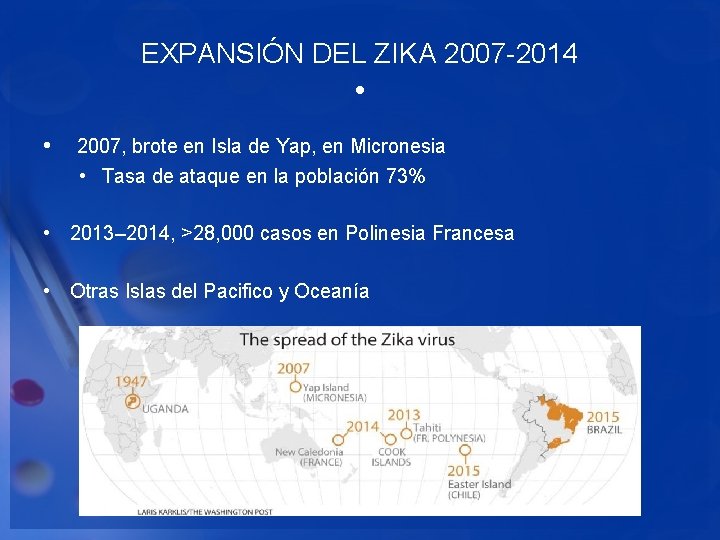
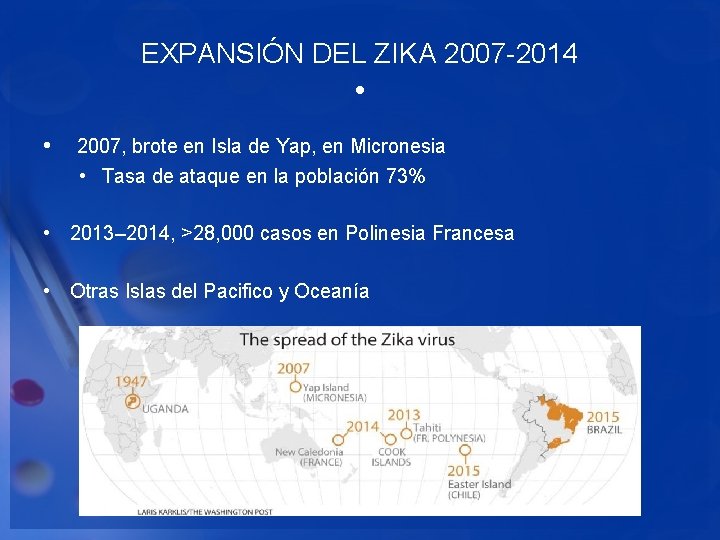
EXPANSIÓN DEL ZIKA 2007 -2014 • • 2007, brote en Isla de Yap, en Micronesia • Tasa de ataque en la población 73% • 2013– 2014, >28, 000 casos en Polinesia Francesa • Otras Islas del Pacifico y Oceanía
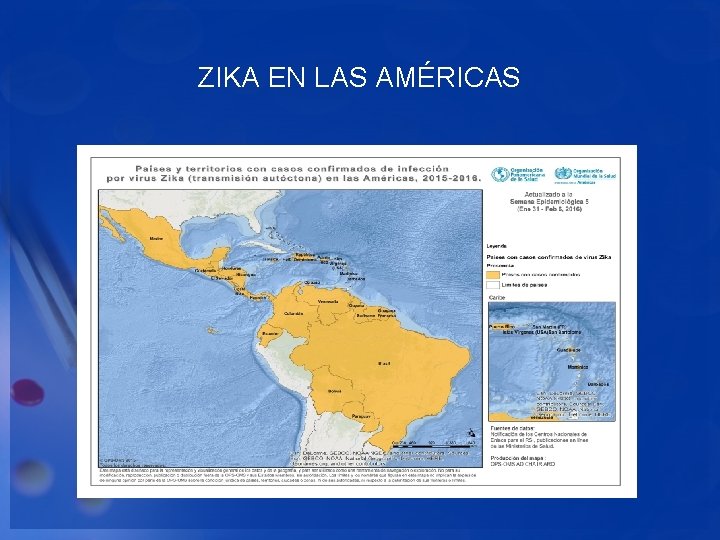
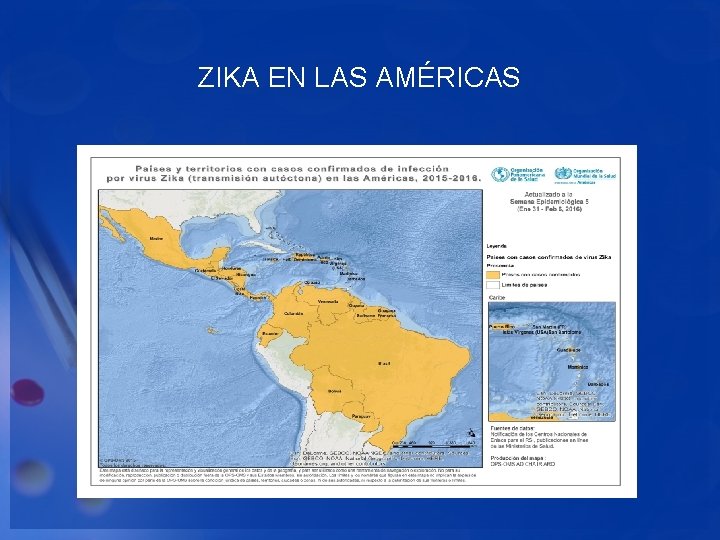
ZIKA EN LAS AMÉRICAS
ZIKA EN PUERTO RICO • 1, 352 casos confirmados al 6/3/2016 • 168 casos en embarazadas • 35, 422 casos al 5/6/2017 • 325 donantes de sangre presuntivos virémicos • 2, 591 casos en embarazadas al 12/23/2016
ZIKA VIRUS IN PREGNANCY • A pregnant woman can pass Zika virus to her fetus. Infection during pregnancy can cause serious birth defects. CDC recommends special precautions for the following groups: • Women who are pregnant: • Should not travel to Puerto Rico. • If you must travel, talk to your doctor first and strictly follow steps to prevent mosquito bites during your trip. • Because Zika can also be spread by sex, if you have a partner who lives in or has traveled to Puerto Rico, either use condoms or do not have sex (vaginal, anal, or oral) or share sex toys during your pregnancy.
ZIKA VIRUS IN PREGNANCY • Women who are trying to become pregnant: • Before you or your partner travel, talk to your doctor about your plans to become pregnant and the risk of Zika virus infection. • See CDC guidance for how long you should wait to get pregnant after travel to Puerto Rico. • You and your partner should strictly follow steps to prevent mosquito bites. • If you have traveled to Puerto Rico and have a pregnant partner, use condoms or don’t have sex (vaginal, anal, or oral) or share sex toys during the pregnancy.
ZIKA & PREGNANCY IN PUERTO RICO • Right now, Zika is spreading rapidly in Puerto Rico and pregnant women are at risk for becoming infected with Zika. If current trends continue, at least 1 in 4 people, including women who become pregnant, may become infected with Zika. Since Zika causes microcephaly and other birth defects, it is more important than ever to consider if now is the right time for you to get pregnant. If you decide that now isn’t the right time for you to have a baby, there are contraceptive methods that are safe and effective. If you decide to get pregnant, there are important steps you should take to try to protect yourself from getting Zika.
MEDIDAS PREVENTIVAS • No existe vacuna o medicamento • Prevención primaria es reducir la exposición a mosquitos • Evitar la picadura del mosquito en personas infectadas, particularmente la primera semana de enfermedad • Uso de condones, particularmente parejas de mujeres embarazadas (todo el embarazo)
PREVENCIÓN Y CONTROL DEL MOSQUITO • Vacíe o elimine los contenedores que acumulan agua • Use aire acondicionado o tela metálica en puertas y ventanas • Use repelentes de mosquito en la piel expuesta • Use ropa de manga y pantalón largo • Apoye los esfuerzos de los programas de control de mosquitos
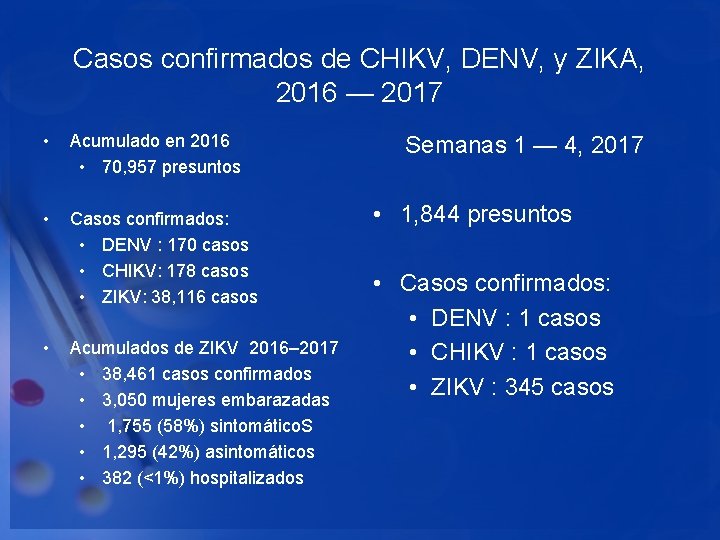
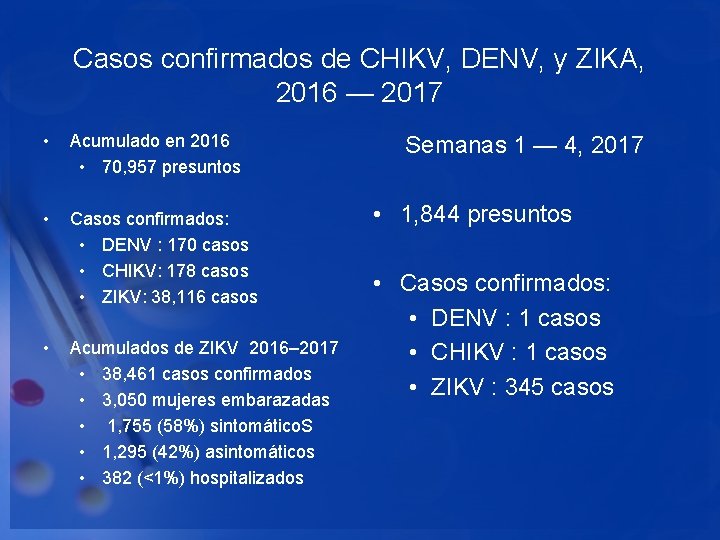
Casos confirmados de CHIKV, DENV, y ZIKA, 2016 — 2017 • Acumulado en 2016 • 70, 957 presuntos • Casos confirmados: • DENV : 170 casos • CHIKV: 178 casos • ZIKV: 38, 116 casos • Acumulados de ZIKV 2016– 2017 • 38, 461 casos confirmados • 3, 050 mujeres embarazadas • 1, 755 (58%) sintomático. S • 1, 295 (42%) asintomáticos • 382 (<1%) hospitalizados Semanas 1 — 4, 2017 • 1, 844 presuntos • Casos confirmados: • DENV : 1 casos • CHIKV : 1 casos • ZIKV : 345 casos