Diagnosis Very important Helps to decide the treatment
- Slides: 16
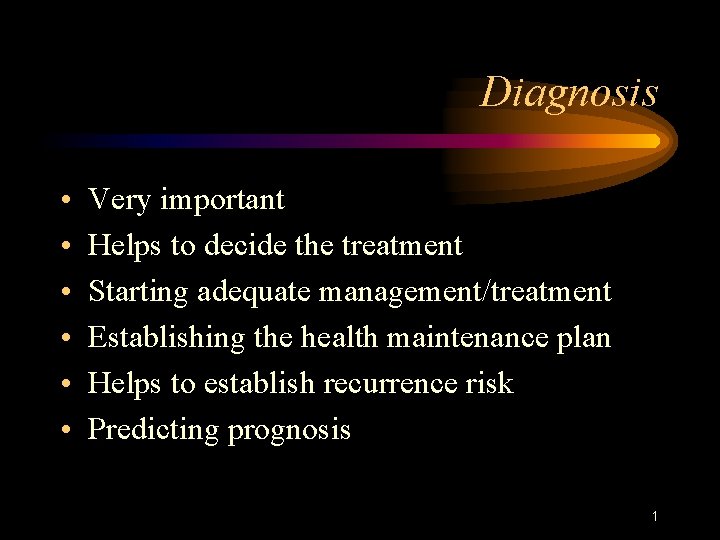
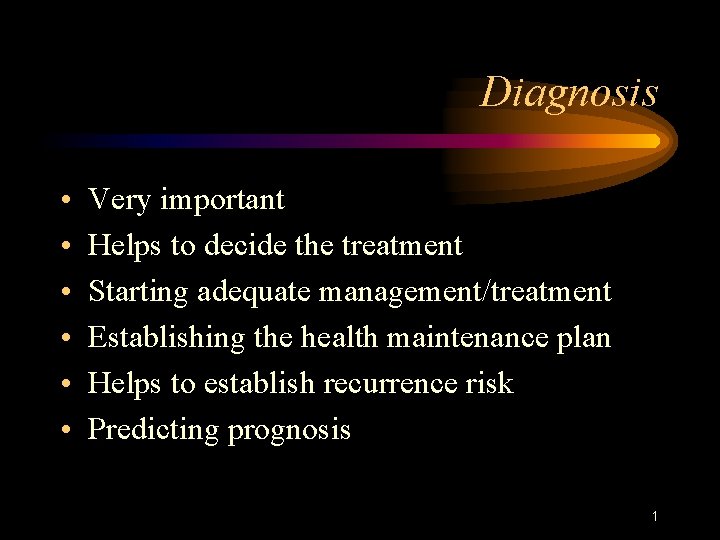
Diagnosis • • • Very important Helps to decide the treatment Starting adequate management/treatment Establishing the health maintenance plan Helps to establish recurrence risk Predicting prognosis 1
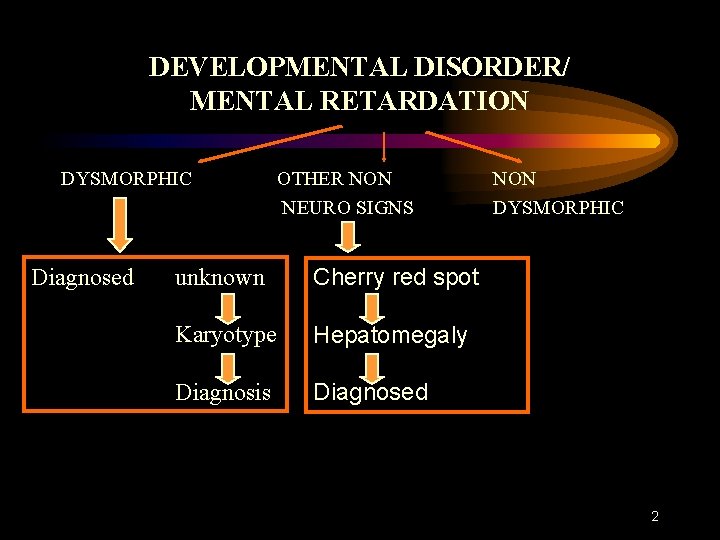
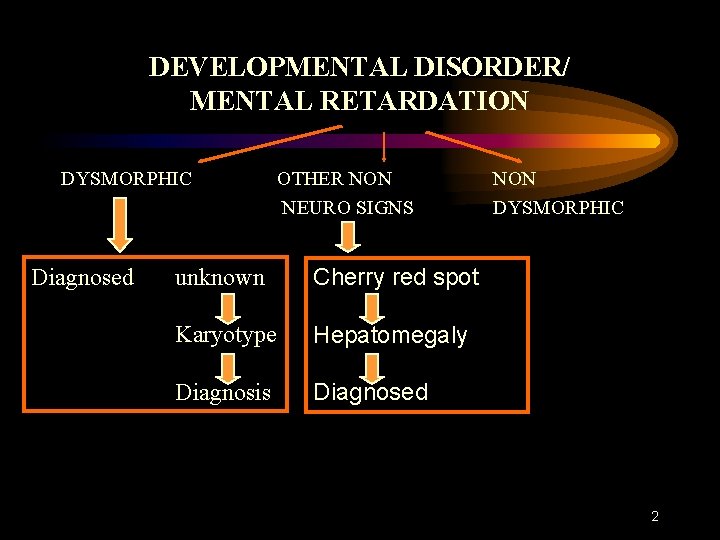
DEVELOPMENTAL DISORDER/ MENTAL RETARDATION DYSMORPHIC Diagnosed OTHER NON NEURO SIGNS unknown Cherry red spot Karyotype Hepatomegaly Diagnosis Diagnosed NON DYSMORPHIC 2
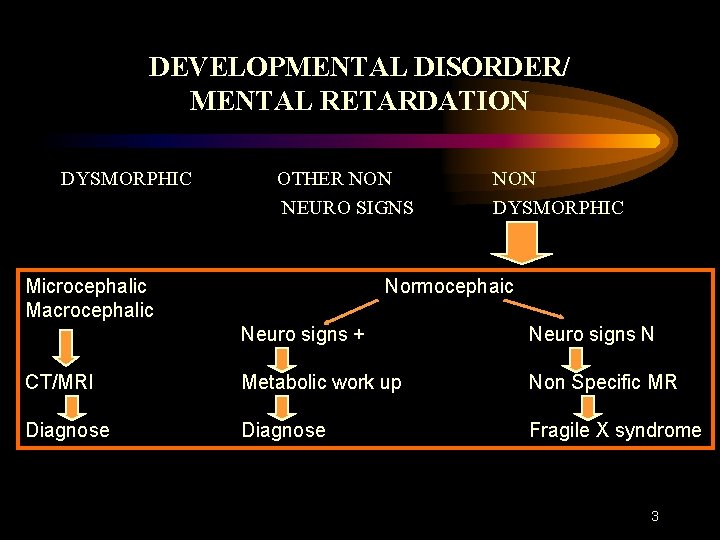
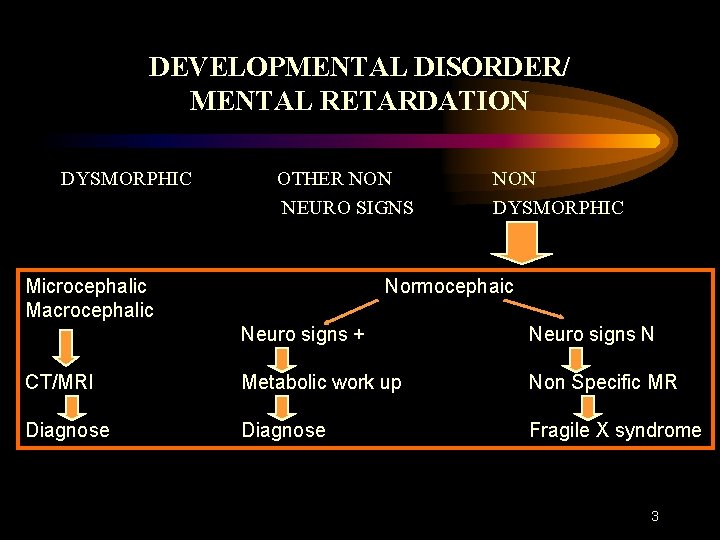
DEVELOPMENTAL DISORDER/ MENTAL RETARDATION DYSMORPHIC OTHER NON NEURO SIGNS Microcephalic Macrocephalic NON DYSMORPHIC Normocephaic Neuro signs + Neuro signs N CT/MRI Metabolic work up Non Specific MR Diagnose Fragile X syndrome 3
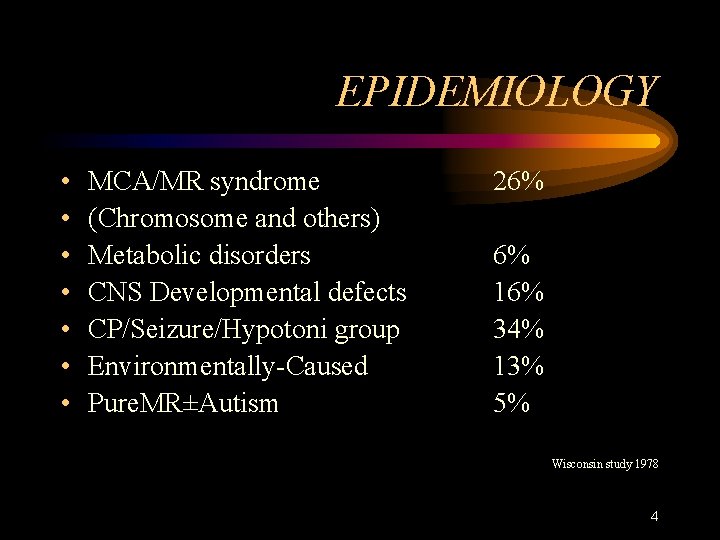
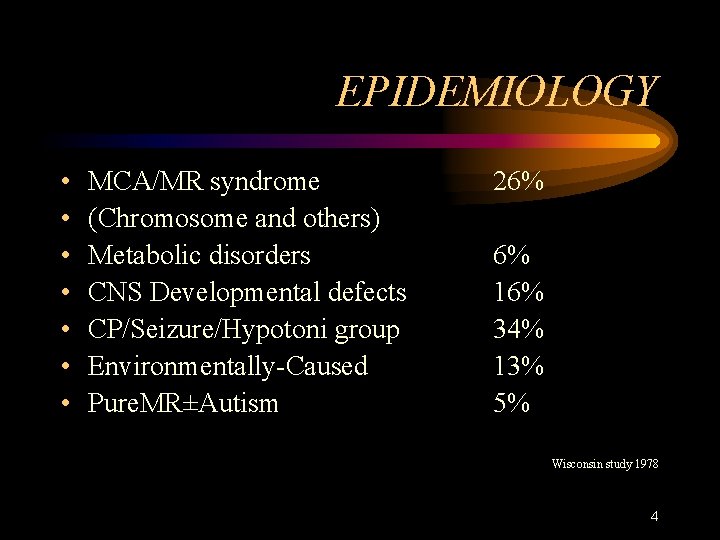
EPIDEMIOLOGY • • MCA/MR syndrome (Chromosome and others) Metabolic disorders CNS Developmental defects CP/Seizure/Hypotoni group Environmentally-Caused Pure. MR±Autism 26% 6% 16% 34% 13% 5% Wisconsin study 1978 4
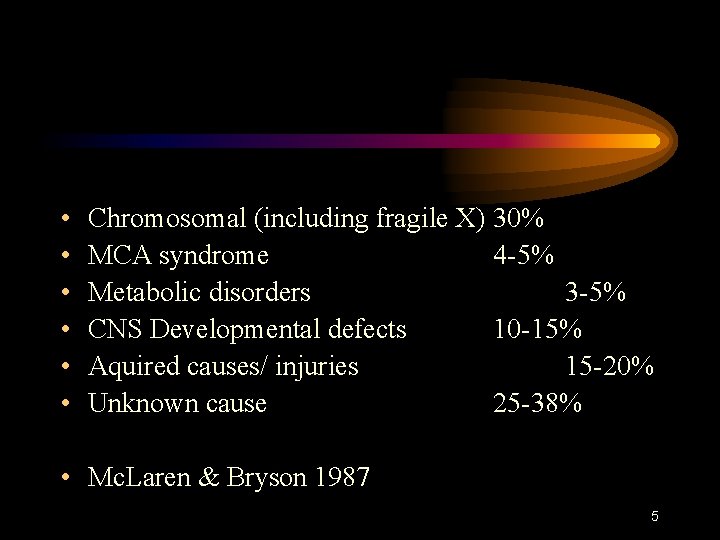
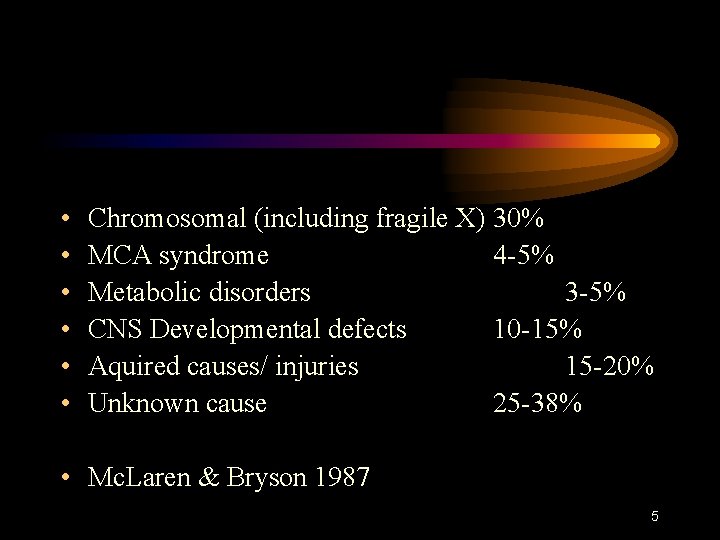
• • • Chromosomal (including fragile X) 30% MCA syndrome 4 -5% Metabolic disorders 3 -5% CNS Developmental defects 10 -15% Aquired causes/ injuries 15 -20% Unknown cause 25 -38% • Mc. Laren & Bryson 1987 5
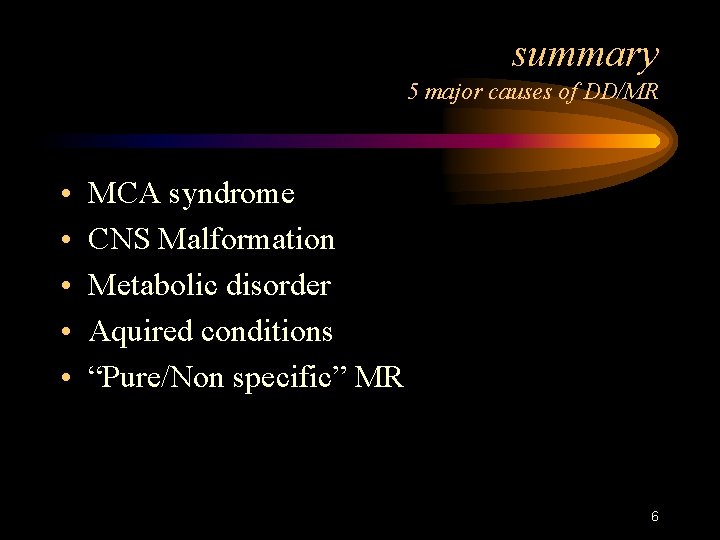
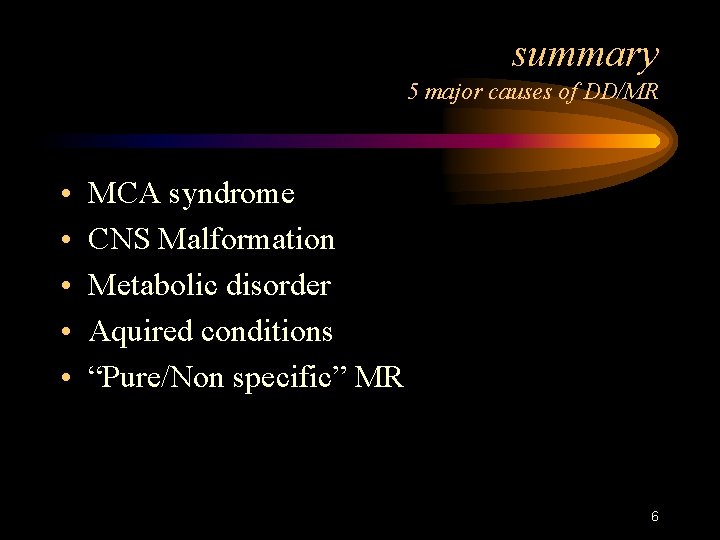
summary 5 major causes of DD/MR • • • MCA syndrome CNS Malformation Metabolic disorder Aquired conditions “Pure/Non specific” MR 6
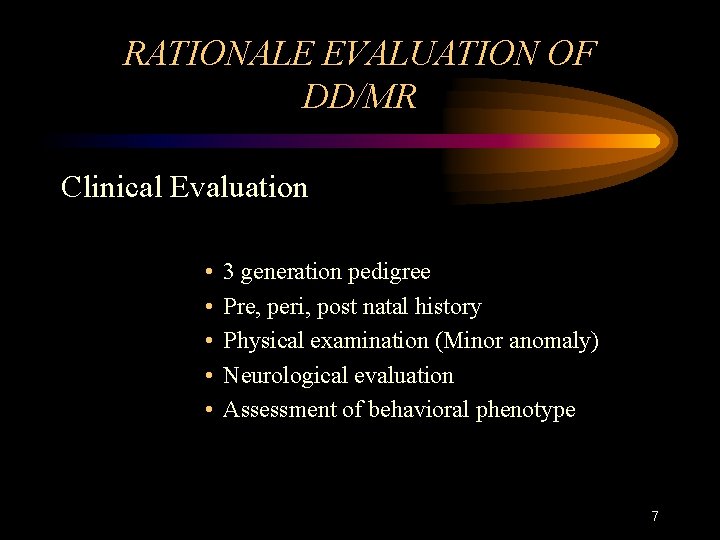
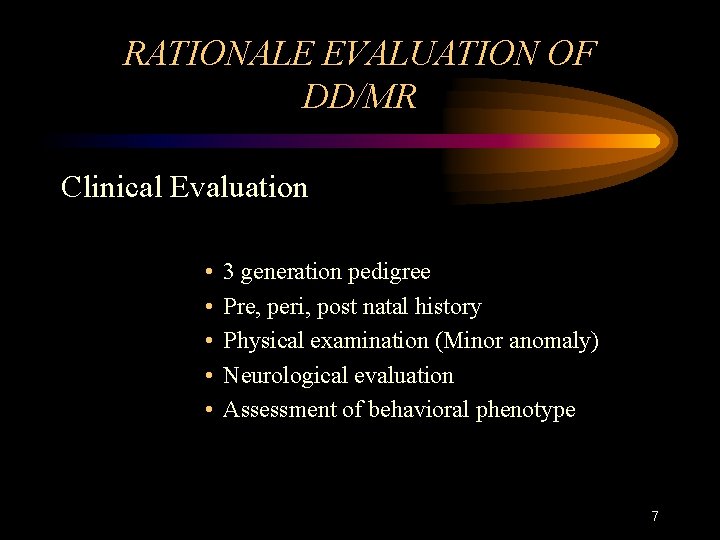
RATIONALE EVALUATION OF DD/MR Clinical Evaluation • • • 3 generation pedigree Pre, peri, post natal history Physical examination (Minor anomaly) Neurological evaluation Assessment of behavioral phenotype 7
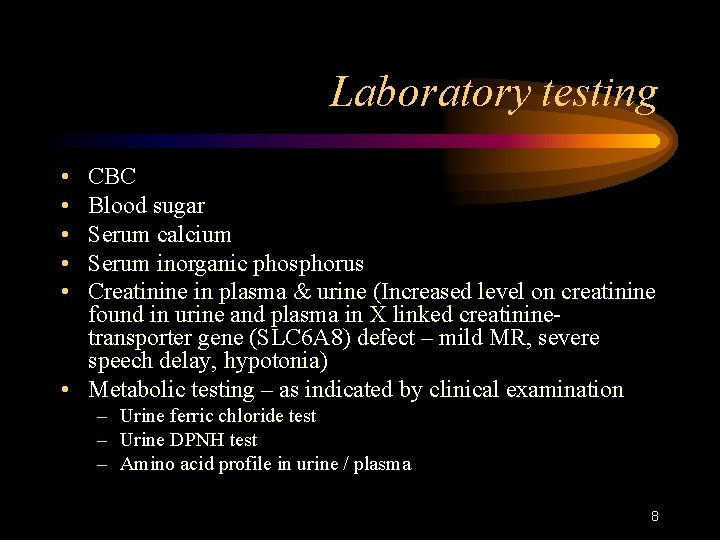
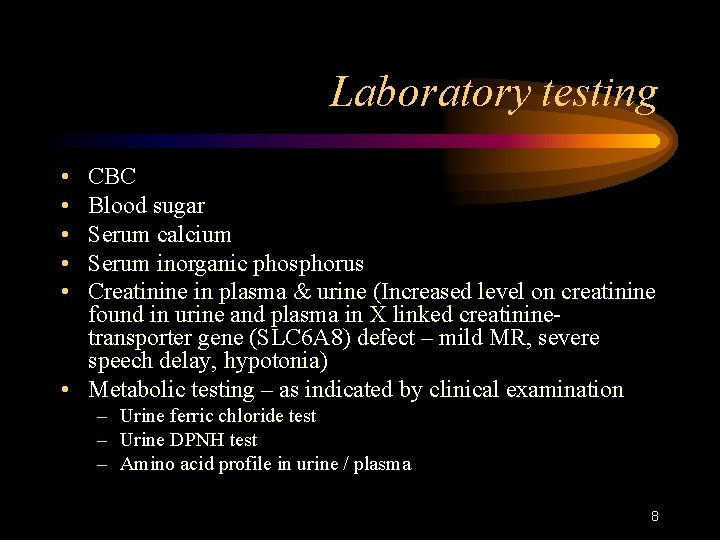
Laboratory testing • • • CBC Blood sugar Serum calcium Serum inorganic phosphorus Creatinine in plasma & urine (Increased level on creatinine found in urine and plasma in X linked creatininetransporter gene (SLC 6 A 8) defect – mild MR, severe speech delay, hypotonia) • Metabolic testing – as indicated by clinical examination – Urine ferric chloride test – Urine DPNH test – Amino acid profile in urine / plasma 8
Laboratory testing • SPECT HMPAO/ ECD • Karyotyping • Fish analysis • Fibroblast karyotype • Fragile X in both male and female • Neuroimaging • Fundus examination 9
Laboratory testing • Arginine: Glycine amidinotransferase deficiency: • (Mild MR. Severe speech delay, with normal examination/OFC and blood creatinine levels. MRS disclosed the total absence of creatinine/phosphocreatinine peak in multiple brain areas Creatinine monohydrate oral administration restored brain creatinine levels along with improvement of the patient disability 10
X linked Mental retardation • • 5 – 14% of MR 130 X – Linked syndromes MRX – 75 gene loci Fragile X ¼ - 6, 000 males • Am J Med Genet 2000, 97 (3): 1 11
Good indicators for subtelomeric defects • • • Family history of MR Prenatal onset of growth retardation Post natal poor growth/over growth 2 or more facial dysmorphic features 1 or more non facial dysmorphic features and/or congenital abnormalities 12
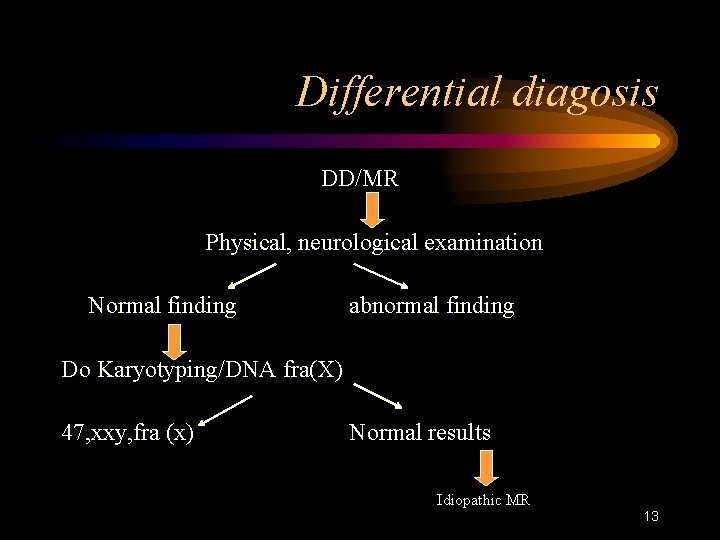
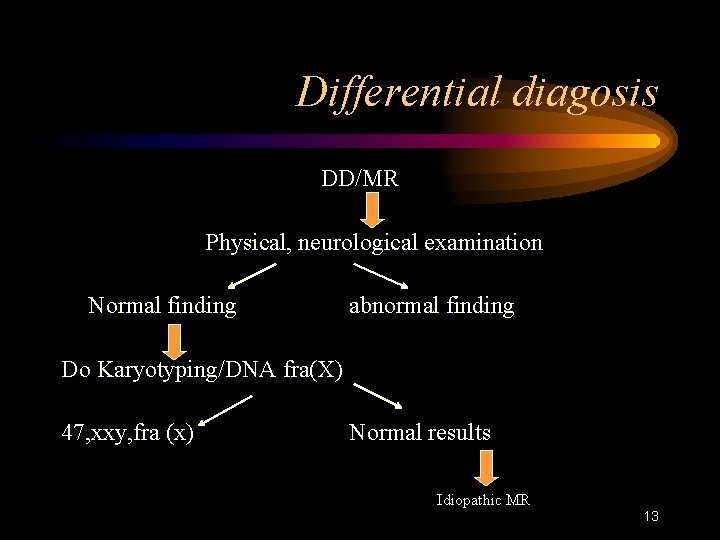
Differential diagosis DD/MR Physical, neurological examination Normal finding abnormal finding Do Karyotyping/DNA fra(X) 47, xxy, fra (x) Normal results Idiopathic MR 13
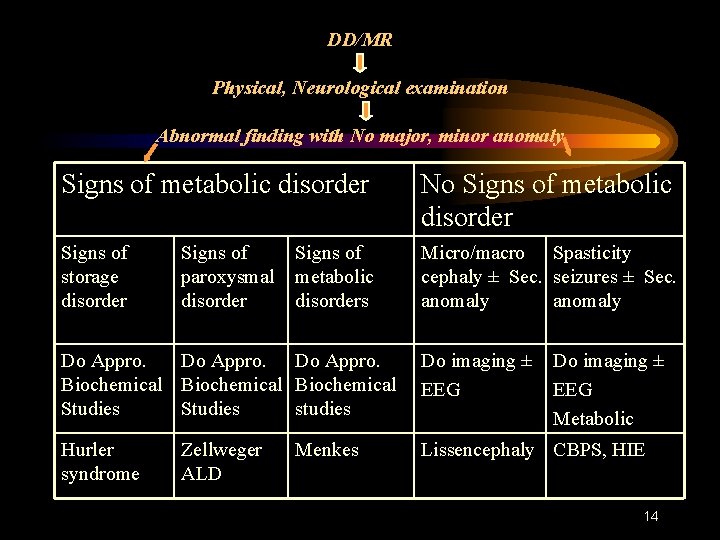
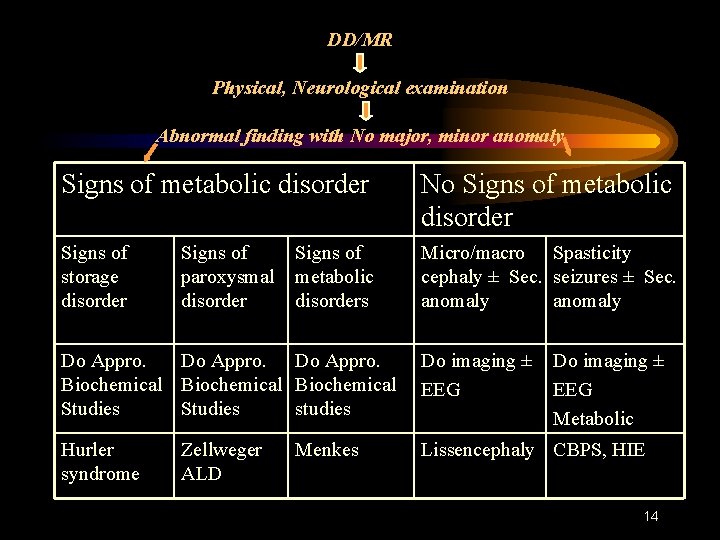
DD/MR Physical, Neurological examination Abnormal finding with No major, minor anomaly Signs of metabolic disorder No Signs of metabolic disorder Signs of storage disorder Micro/macro Spasticity cephaly ± Sec. seizures ± Sec. anomaly Signs of paroxysmal disorder Signs of metabolic disorders Do Appro. Biochemical Studies studies Do imaging ± EEG Hurler syndrome Lissencephaly CBPS, HIE Zellweger ALD Menkes Do imaging ± EEG Metabolic 14
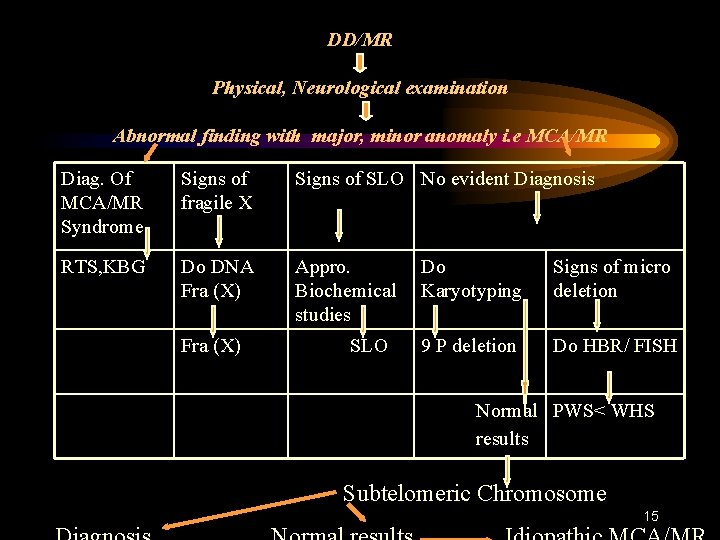
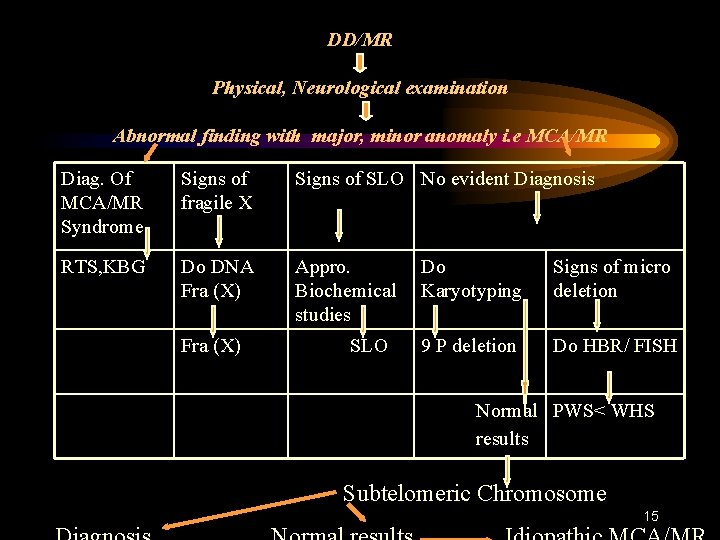
DD/MR Physical, Neurological examination Abnormal finding with major, minor anomaly i. e MCA/MR Diag. Of MCA/MR Syndrome Signs of fragile X Signs of SLO No evident Diagnosis RTS, KBG Do DNA Fra (X) Appro. Biochemical studies Fra (X) SLO Do Karyotyping Signs of micro deletion 9 P deletion Do HBR/ FISH Normal PWS< WHS results Subtelomeric Chromosome 15
RATIONALE EVALUATION OF DD/MR CONCLUSIONS • Through physical examination + awareness of the existence of definite patterns of malformations Newer diagnostic techniques Diagnosis 16