Diagnosis of Acute Ischemic and Hemorrhagic Stroke Ischemic
- Slides: 22
Diagnosis of Acute Ischemic and Hemorrhagic Stroke
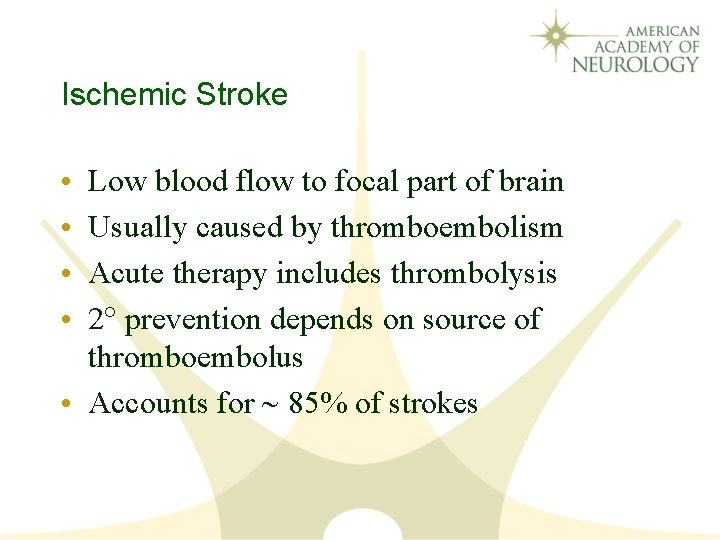
Ischemic Stroke • • Low blood flow to focal part of brain Usually caused by thromboembolism Acute therapy includes thrombolysis 2 prevention depends on source of thromboembolus • Accounts for 85% of strokes
Transient Ischemic Attack (TIA) • Reversible focal dysfunction, usually lasts minutes • Among TIA pts who go to ED: – 5% have stroke in next 2 days – 25% have recurrent event in next 3 months • Stroke risk decreased with proper therapy
Intracerebral Hemorrhage • Bleeding into brain tissue • Usually caused by chronic hypertension • Non-hypertension cause more likely if: – No past history of hypertension – Lobar (i. e. , peripheral, not subcortical) • May require emergency surgery • Accounts for 10% of strokes
Subarachnoid Hemorrhage • Bleeding around brain • Usually caused by ruptured aneurysm • Surgical emergency – Cerebral angiography – Aneurysmal clipping • Accounts for 5% of strokes
Five Major Stroke Syndromes for Rapid Recognition in the ED • • • All Occur Suddenly in Stroke Patients Left (dominant) cerebral hemisphere Right (nondominant) cerebral hemisphere Brainstem Cerebellum Hemorrhage Note: The dominant cerebral hemisphere is the side that controls language function.
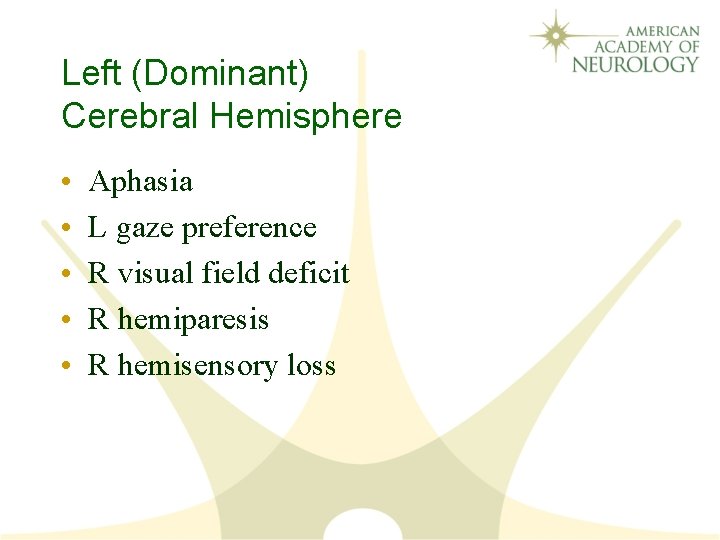
Left (Dominant) Cerebral Hemisphere • • • Aphasia L gaze preference R visual field deficit R hemiparesis R hemisensory loss
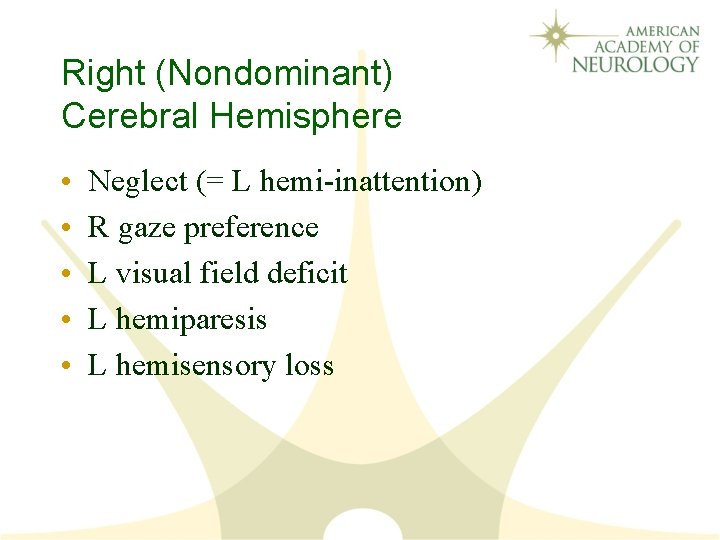
Right (Nondominant) Cerebral Hemisphere • • • Neglect (= L hemi-inattention) R gaze preference L visual field deficit L hemiparesis L hemisensory loss
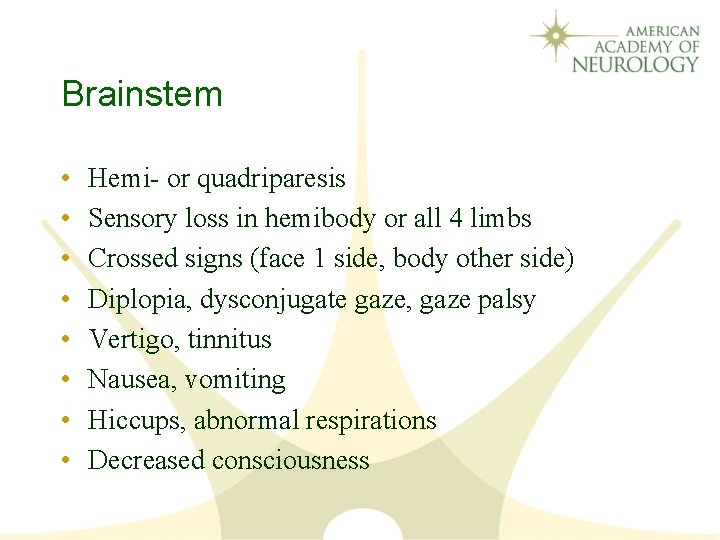
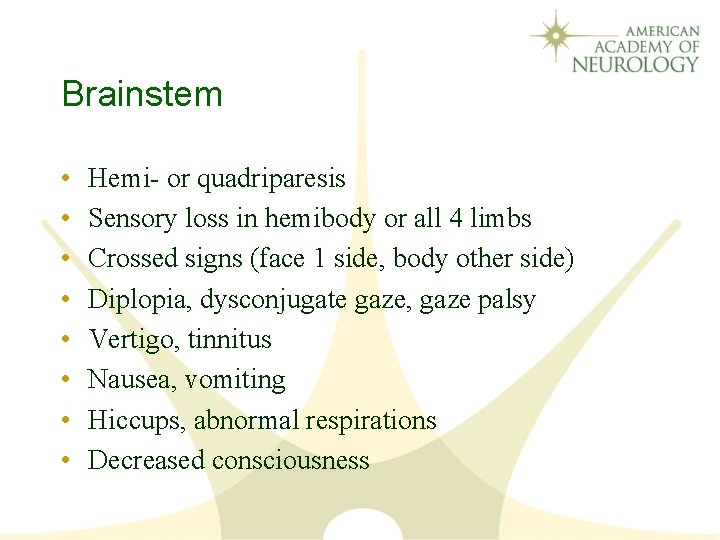
Brainstem • • Hemi- or quadriparesis Sensory loss in hemibody or all 4 limbs Crossed signs (face 1 side, body other side) Diplopia, dysconjugate gaze, gaze palsy Vertigo, tinnitus Nausea, vomiting Hiccups, abnormal respirations Decreased consciousness
Cerebellum • Truncal = gait ataxia • Limb ataxia
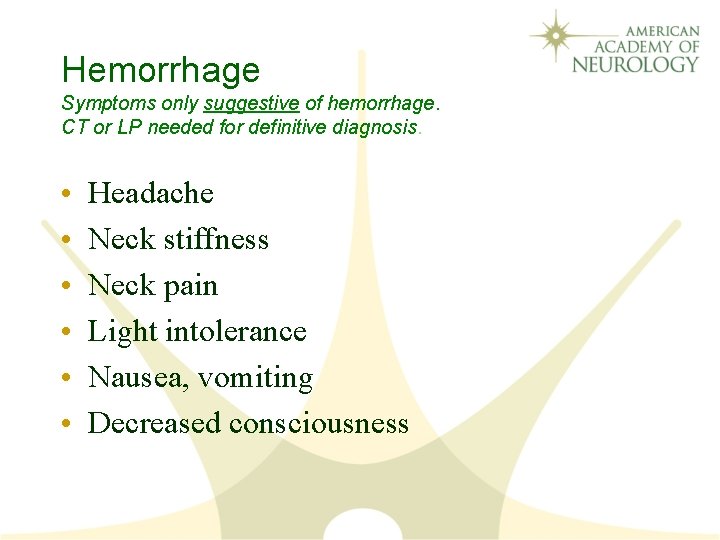
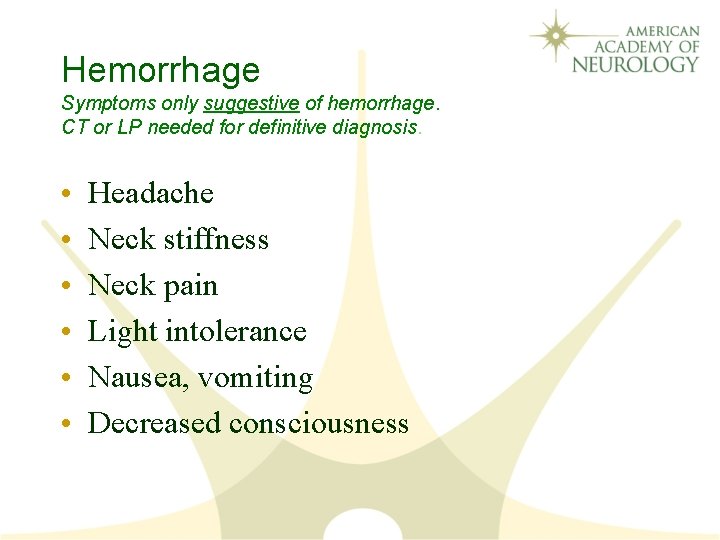
Hemorrhage Symptoms only suggestive of hemorrhage. CT or LP needed for definitive diagnosis. • • • Headache Neck stiffness Neck pain Light intolerance Nausea, vomiting Decreased consciousness
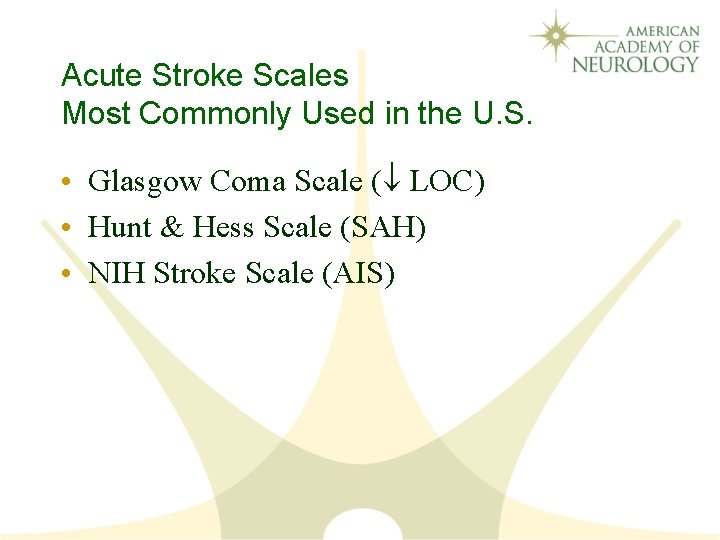
Acute Stroke Scales Most Commonly Used in the U. S. • Glasgow Coma Scale ( LOC) • Hunt & Hess Scale (SAH) • NIH Stroke Scale (AIS)
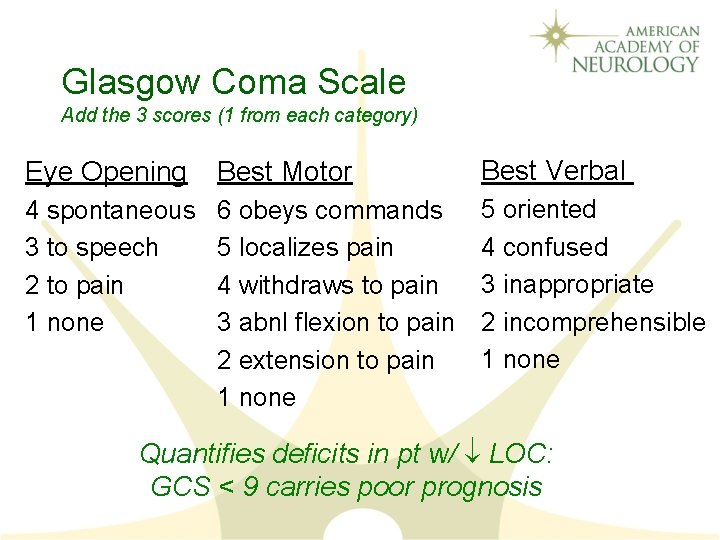
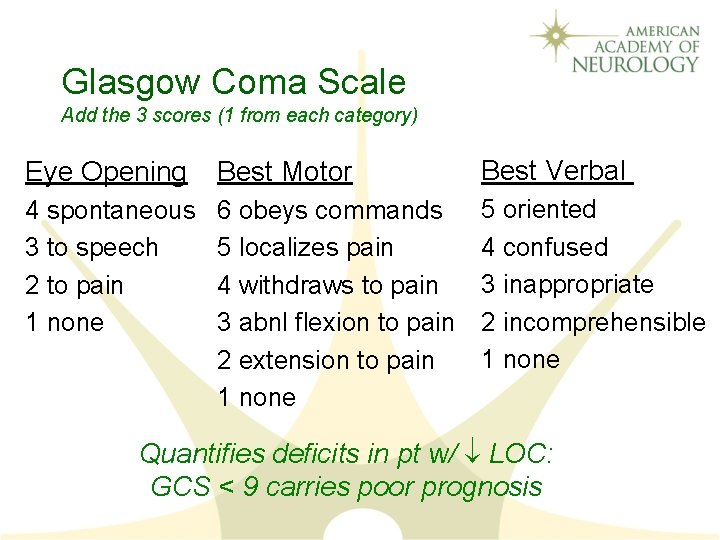
Glasgow Coma Scale Add the 3 scores (1 from each category) Eye Opening Best Motor Best Verbal 4 spontaneous 3 to speech 2 to pain 1 none 6 obeys commands 5 localizes pain 4 withdraws to pain 3 abnl flexion to pain 2 extension to pain 1 none 5 oriented 4 confused 3 inappropriate 2 incomprehensible 1 none Quantifies deficits in pt w/ LOC: GCS < 9 carries poor prognosis
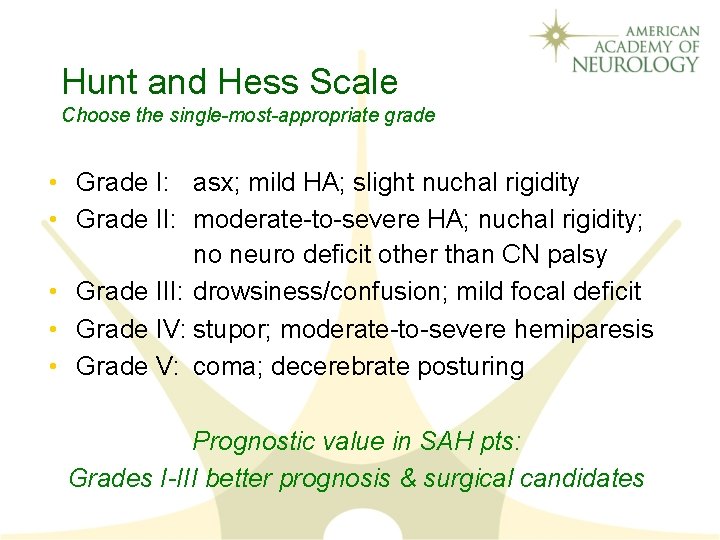
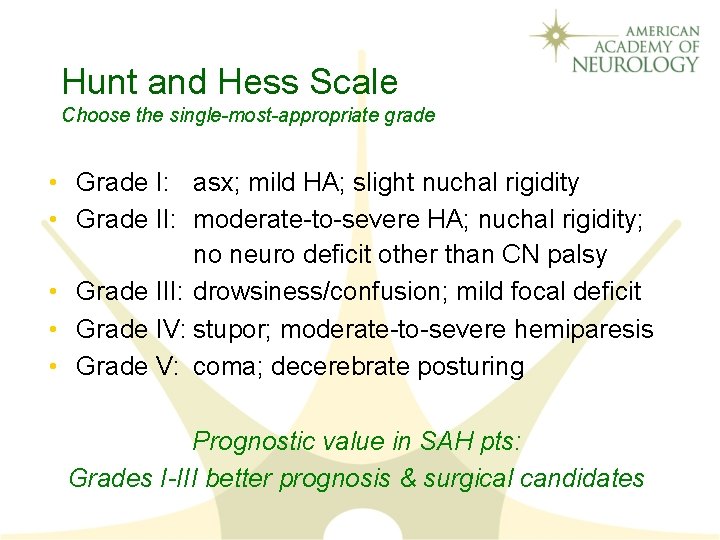
Hunt and Hess Scale Choose the single-most-appropriate grade • Grade I: asx; mild HA; slight nuchal rigidity • Grade II: moderate-to-severe HA; nuchal rigidity; no neuro deficit other than CN palsy • Grade III: drowsiness/confusion; mild focal deficit • Grade IV: stupor; moderate-to-severe hemiparesis • Grade V: coma; decerebrate posturing Prognostic value in SAH pts: Grades I-III better prognosis & surgical candidates
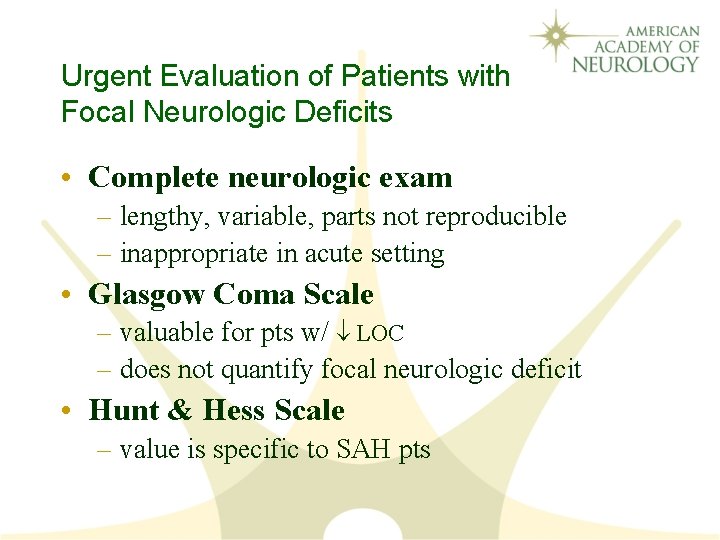
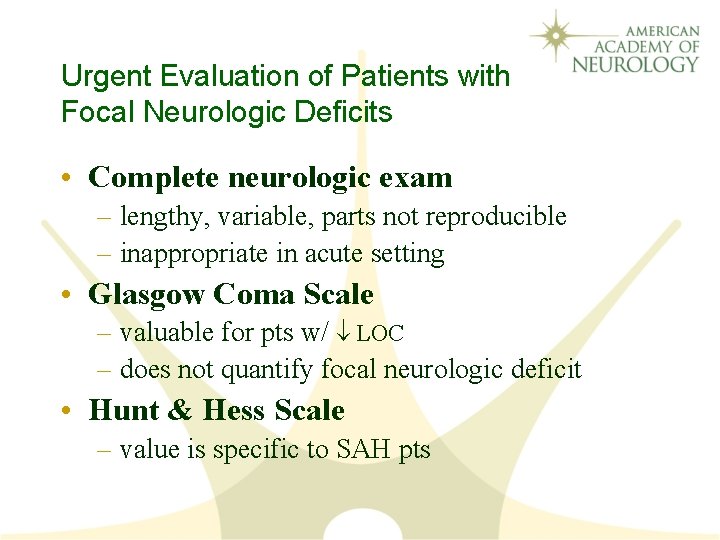
Urgent Evaluation of Patients with Focal Neurologic Deficits • Complete neurologic exam – lengthy, variable, parts not reproducible – inappropriate in acute setting • Glasgow Coma Scale – valuable for pts w/ LOC – does not quantify focal neurologic deficit • Hunt & Hess Scale – value is specific to SAH pts
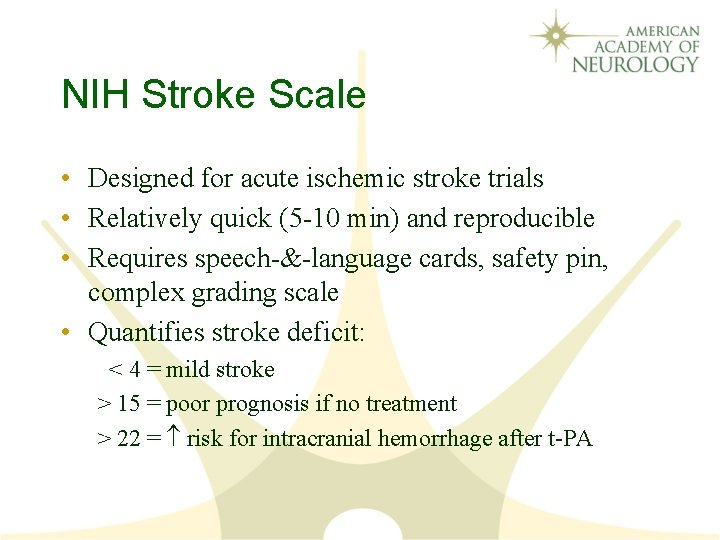
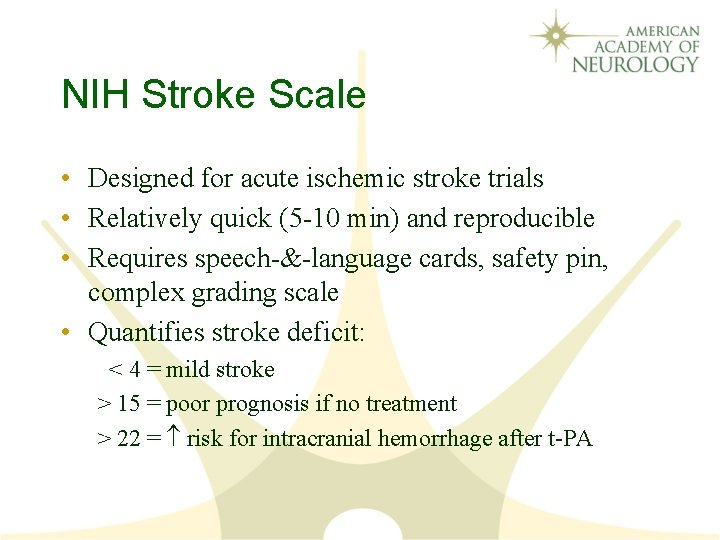
NIH Stroke Scale • Designed for acute ischemic stroke trials • Relatively quick (5 -10 min) and reproducible • Requires speech-&-language cards, safety pin, complex grading scale • Quantifies stroke deficit: < 4 = mild stroke > 15 = poor prognosis if no treatment > 22 = risk for intracranial hemorrhage after t-PA
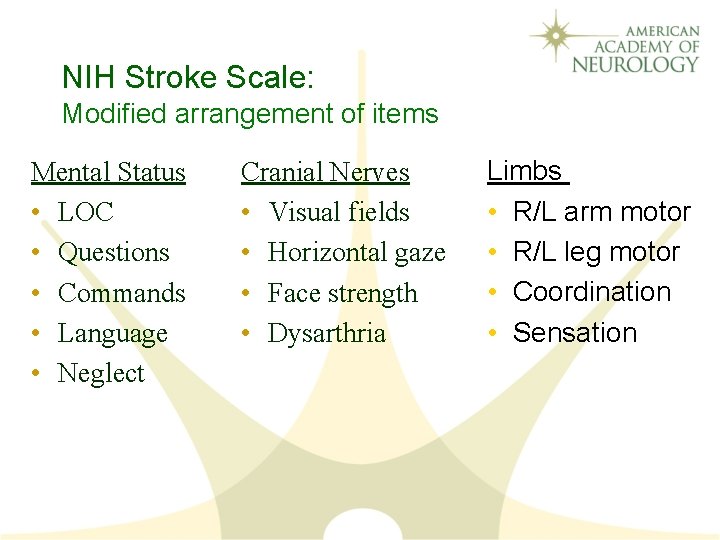
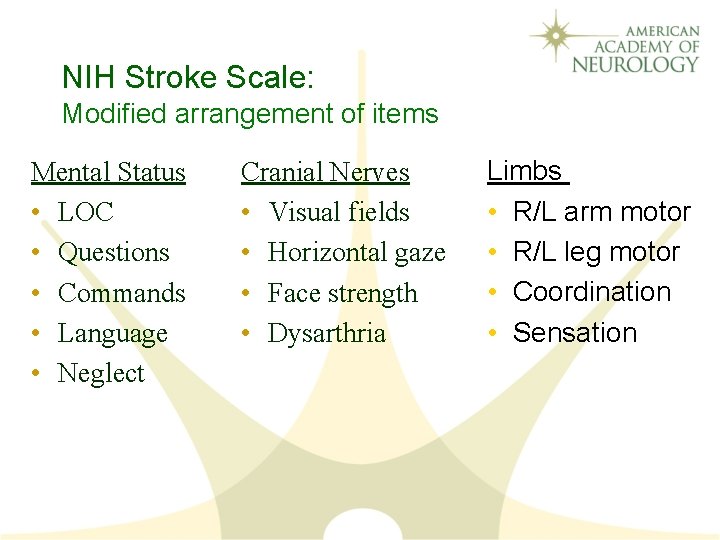
NIH Stroke Scale: Modified arrangement of items Mental Status • LOC • Questions • Commands • Language • Neglect Cranial Nerves • Visual fields • Horizontal gaze • Face strength • Dysarthria Limbs • R/L arm motor • R/L leg motor • Coordination • Sensation
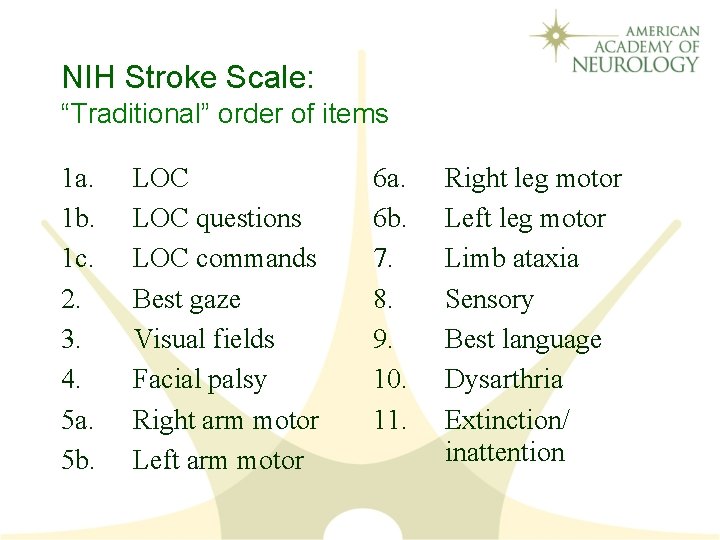
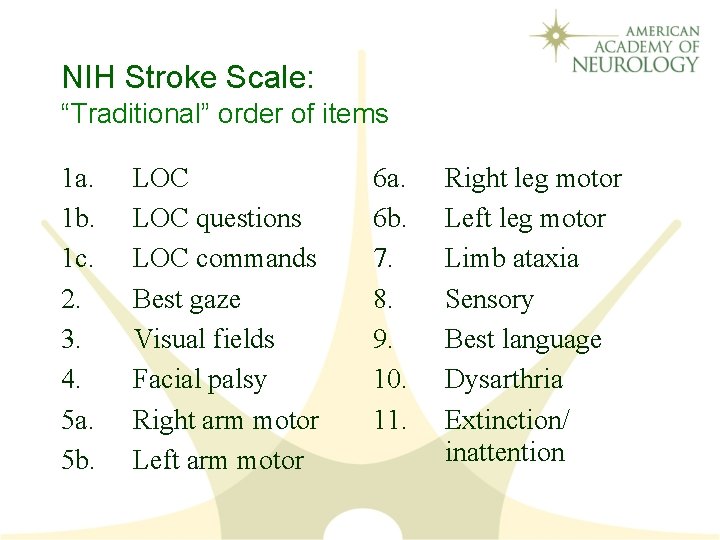
NIH Stroke Scale: “Traditional” order of items 1 a. 1 b. 1 c. 2. 3. 4. 5 a. 5 b. LOC questions LOC commands Best gaze Visual fields Facial palsy Right arm motor Left arm motor 6 a. 6 b. 7. 8. 9. 10. 11. Right leg motor Left leg motor Limb ataxia Sensory Best language Dysarthria Extinction/ inattention
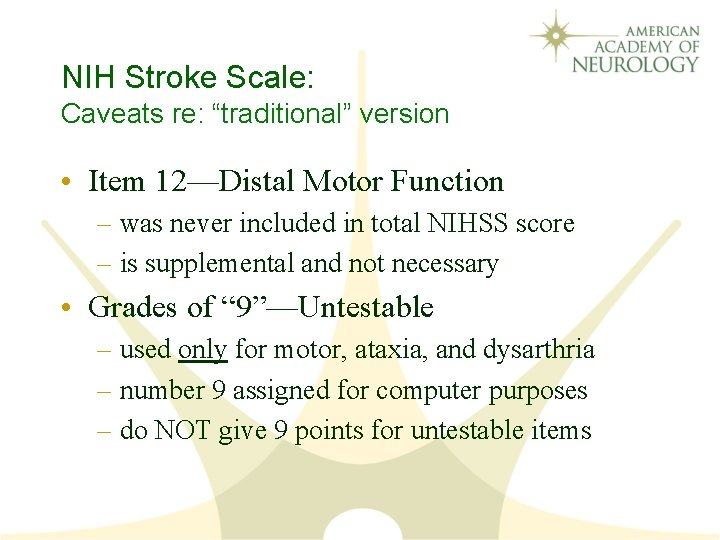
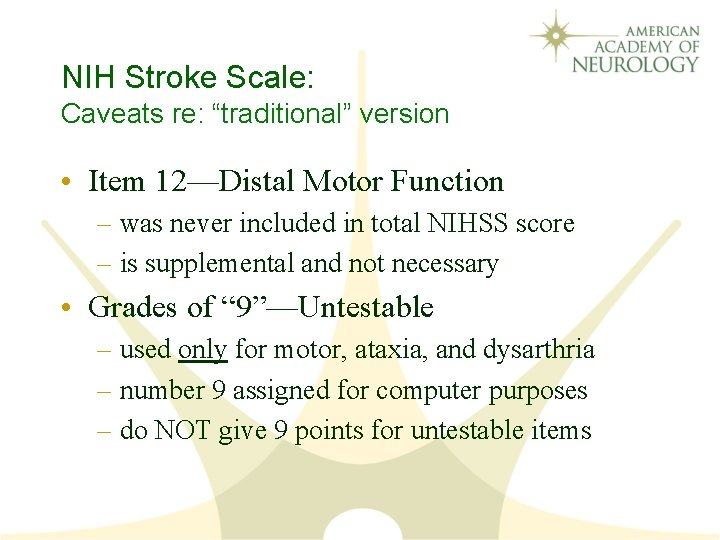
NIH Stroke Scale: Caveats re: “traditional” version • Item 12—Distal Motor Function – was never included in total NIHSS score – is supplemental and not necessary • Grades of “ 9”—Untestable – used only for motor, ataxia, and dysarthria – number 9 assigned for computer purposes – do NOT give 9 points for untestable items
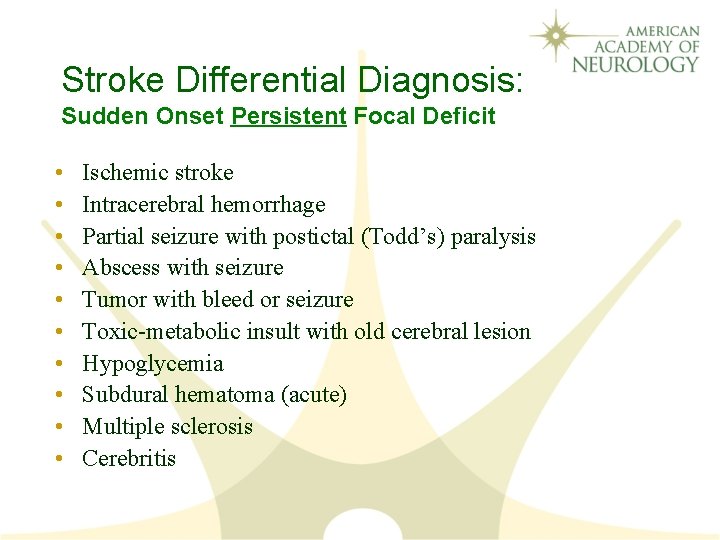
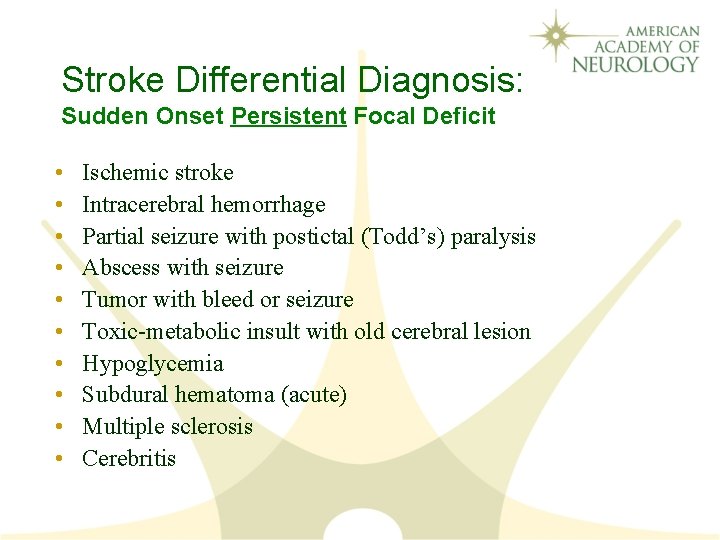
Stroke Differential Diagnosis: Sudden Onset Persistent Focal Deficit • • • Ischemic stroke Intracerebral hemorrhage Partial seizure with postictal (Todd’s) paralysis Abscess with seizure Tumor with bleed or seizure Toxic-metabolic insult with old cerebral lesion Hypoglycemia Subdural hematoma (acute) Multiple sclerosis Cerebritis
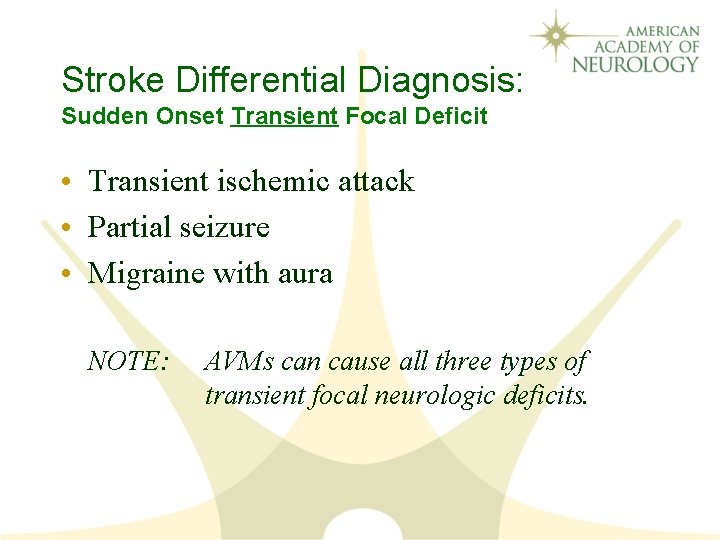
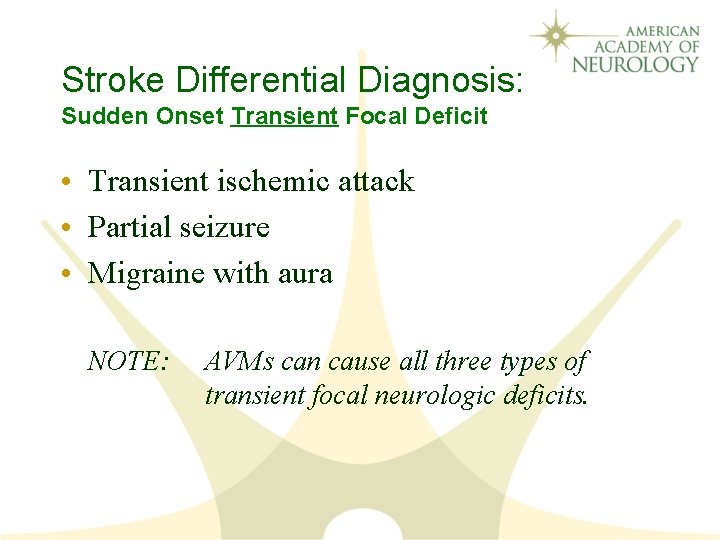
Stroke Differential Diagnosis: Sudden Onset Transient Focal Deficit • Transient ischemic attack • Partial seizure • Migraine with aura NOTE: AVMs can cause all three types of transient focal neurologic deficits.
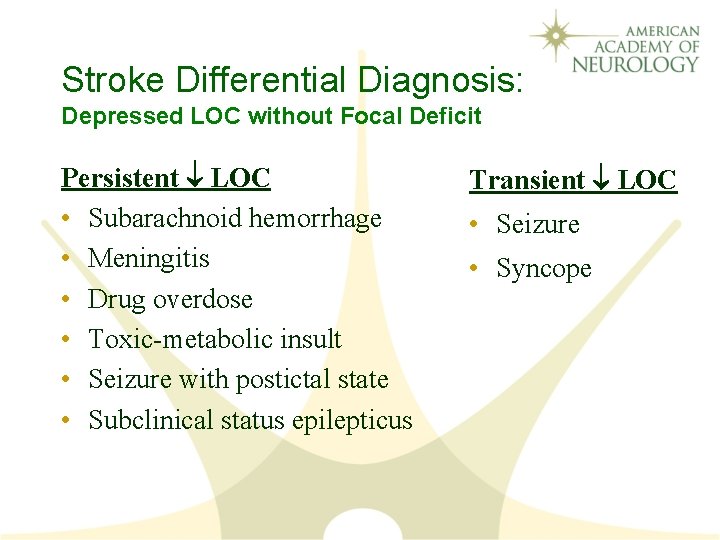
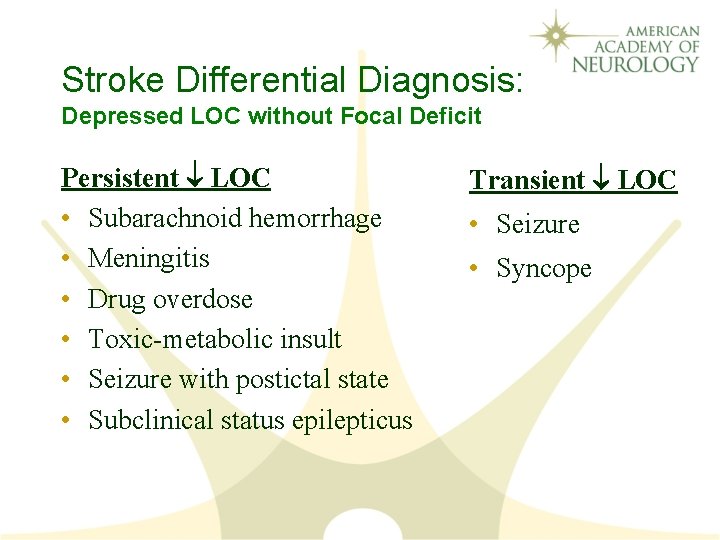
Stroke Differential Diagnosis: Depressed LOC without Focal Deficit Persistent LOC • Subarachnoid hemorrhage • Meningitis • Drug overdose • Toxic-metabolic insult • Seizure with postictal state • Subclinical status epilepticus Transient LOC • Seizure • Syncope