Diagnosis First Visit Overall Appraisal of the Patient
- Slides: 37
Diagnosis First Visit - Overall, Appraisal of the Patient This includes consideration of the patient's mental and emotional status, temperament, attitude, and physiologic age.
Medical History The importance of the medical history should be explained to the patient because patients often omit information that they cannot relate to their dental problems. The patient should be made aware of (1) the possible role that some systemic diseases, conditions or behavioral factors may play in the cause of periodontal disease. (2) oral infection may have a powerful influence on the occurrence and severity of a variety of systemic diseases and conditions
The nature and duration of the problem and therapy Details on hospitalization and operations, including diagnosis, kind of operation, and untoward events such as anesthetic, hemorrhagic, or infectious complications,
. all medications being taken and whether they were prescribed or obtained over the counter. . All the possible effects of these medications should be carefully analyzed to determine their effect, if any, on the oral tissues and also to. avoid administering medications that would interact adversely with them.
• History should be taken of all medical problems (cardiovascular, hematologic, endocrine, etc. ), including infectious diseases and. high-risk behavior for human immunodeficiency. virus (HIV) infection. . Any possibility of occupational disease
• Abnormal bleeding tendencies such as nosebleeds, • prolonged bleeding from minor cuts, spontaneous ecchymoses, • tendency toward excessive bruising, and. • History of allergy should be taken, including hay • fever, asthma, sensitivity to foods, or sensitivity to • drugs such as aspirin, codeine, barbiturates, sulfonamides, antibiotics, procaine, and laxatives, to dental • materials such as eugenol or acrylic resins.
• Family medical history should be taken, including • bleeding disorders and diabetes. . Kidney disorders.
H/O Current illness. • Some patients may be unaware of any problems but many may report bleeding gums; loose teeth; spreading of the teeth with the appearance of spaces where none existed before; • foul taste in the mouth; • itchy feeling in the gums, relieved by digging with a toothpick. -There may also be pain of varied types and duration, including constant, dull, gnawing pain, dull pain after eating; deep, radiating pains in the jaws; acute throbbing pain; -sensitivity when chewing; sensitivity to heat and cold; -burning sensation in the gums; and extreme sensitivity to inhaled air.
• Dental Treatments • Any orthodontic treatment including duration and approximate date of termination, should be noted. • patient's general dental habits? If there is any grinding or clenching of the teeth during the • day or at night,
• previous periodontal problems should be • noted, including the nature of the condition and, if • previously treated, the type of treatment received • (surgical or nonsurgical) and approximate period of • termination of previous treatment.
• A bad taste in the mouth and areas of food impaction should be recorded. . Do the teeth feel "loose" or insecure? Is there difficulty in chewing? Any tooth mobility should be recorded.
• patient's general dental habits? • grinding or clenching of the teeth • other habits, such as tobacco smoking or chewing, • nail biting, or biting on foreign objects?
• History of previous periodontal problems should be • noted, including the nature of the condition and, if • previously treated, the type of treatment received
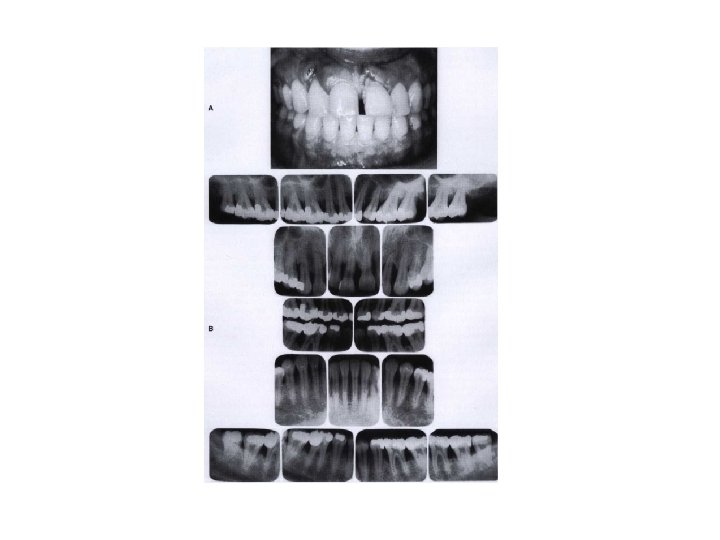
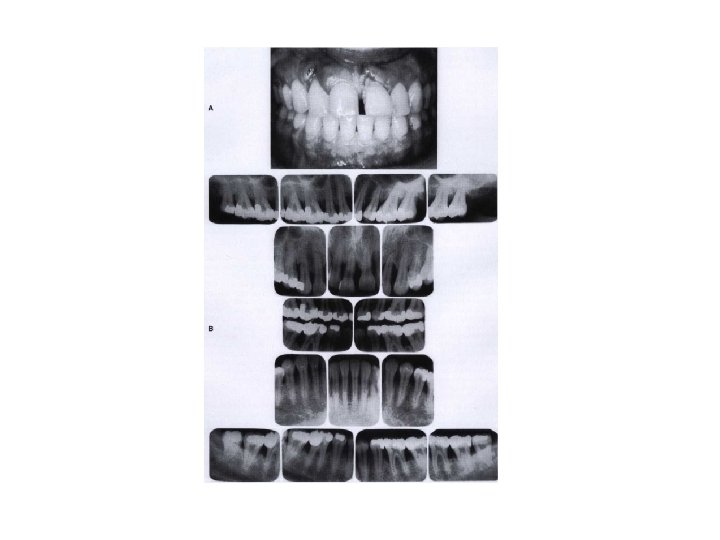
• I ntraoral Radiographic Surveys • consist of a minimum of 14 intraoral films and four posterior bite-wing films • Panoramic radiographs are a simple and convenient method of obtaining a survey for the detection of developmental anomalies, pathologic lesions of the teeth and jaws, and fractures.
Castsindicate the position of the gingival margins and the position and inclination of the teeth, proximal contact relationships, and food impaction areas. In addition, they provide a view of lingual-cuspal relationship. • visual aids in discussions with the patient • useful for pre- and post-treatment comparisons,
• Clinical Photographs • for recording the appearance of the tissue before and after • treatment. • Review of the Initial Examination • I f no emergency care is required, the patient is dismissed • instructed as to when to report for the second visit.
SECOND VISIT Oral Examination Oral Hygiene. The cleanliness of the oral cavity is appraised in terms of the extent of accumulated food debris, plaque, materia alba, and tooth surface stains Disclosing solution may be used to detect plaque to be unnoticed
• Mouth Odors. • Local sources of mouth odors • Extraoral sources of mouth odors include various infections or lesions of the respiratory tract (bronchitis, • pneumonia, bronchiectasis, or others) and odors that are excreted through the lungs from aromatic substances in the bloodstream, such as metabolites from ingested foods or excretory products of cell metabolism. Alcoholic breath, the acetone odor of diabetes, and the uremic breath that accompanies kidney dysfunction are examples.
• Examination of the Oral Cavity. • The entire oral cavity should be carefully examined. The examination should include the lips, floor of the mouth, tongue, palate, and oropharyngeal region, as well as the quality and quantity of saliva. Examination of Lymph Nodes. Because periodontal, periapical, and other oral diseases may result in lymph node changes,
• Examination of the Teeth • The teeth are examined for caries, developmental defects, anomalies of tooth form, wasting, hypersensitivity, and proximal contact relationships • Wasting Disease of the Teeth. • Wasting is defined as any gradual loss o f tooth substance characterized by the formation of smooth, polished surfaces, without regard to the possible mechanism of this loss. The forms of wasting are erosion, abrasion, and attrition.
• Dental Stains. • These are pigmented deposits on the teeth. They should be carefully examined to determine their origin Hypersensitivity. Root surfaces exposed by gingival recession may be hypersensitive to thermal changes or tactile stimulation.
• Proximal Contact Relations. • . Slightly open contacts permit food impaction. The tightness of contacts should be checked by means of clinical observation and with dental floss • Tooth Mobility. • All teeth have a slight degree of physiologic mobility, which varies for different teeth and at different times of the day. " It is greatest on arising in the morning and progressively decreases.
• Tooth mobility occurs in two stages: 1. The initial or intrasocket stage is where the tooth moves within the confines of the periodontal ligament. This is associated with viscoelastic distortion of the ligament and redistribution of the periodontal fluids, 2. This initial movement occurs with forces of about 100 lb and is of the order of 0. 05 to 0. 10 mm (50 to 100 microns).
• The secondary stage, which occurs gradually and entails elastic deformation of the alveolar bone in response to increased horizontal force. • When a force such as that applied to teeth in occlusion is discontinued, the teeth return to their original position in two stages: 1. is an immediate, springlike elastic recoil; 2 is a slow, asymptomatic recovery movement. The recovery movement is pulsating and is apparently associated with the normal pulsation of the periodontal vessels,
• Examination of the Periodontium • The periodontal examination should be systematic, starting in the molar region in either the maxilla or the mandible and proceeding around the arch. • A method for periodontal screening and recording (PSR) has been developed jointly by the American Academy of Periodontology and the American Dental Association, with the support of the Procter & Gamble Com • Use of Clinical Indices-Gingival Index, Bleeding Index indices to measure Plaque and Calculus.
produce two basic types of tissue response: edematous and fibrotic. Edematous tissue response is characterized by a smooth, glossy, soft, red gingiva. In the fibrotic tissue response, some of the characteristics of normalcy persist; the gingiva is more firm, stippled, and opaque, although it is usually thicker, and its margin appears rounded
• When to explore the pdl pkt. Probing of pockets is done at various times for diagnosis, and for monitoring the course of treatment and maintenance. • With the main purpose of determining whether the tooth can be saved or should be extracted. • The only accurate method of detecting and measuring periodontal pockets is careful exploration with a periodontal probe , • Gutta percha points or calibrated silver points can be used with the radiograph to assist in determining the level of attachment of periodontal pockets.
• Probe can vary depending on the force of introduction, the shape and size of the probe tip and the degree of tissue inflammation. ' • The force For Pdl pkt is 25 -30 gm The depth of penetration of the probe in the connective tissue apical to the junctional epithelium in a periodontal pocket is about 0. 3 mm.
PROBING TECHNIQUE. • The probe should be inserted parallel to the vertical axis of the tooth and "walked" circumferentially around each surface of each tooth to detect the areas of deepest defect. To detect an interdental crater, the probe should be placed obliquely from both the facial and lingual surfaces so as to explore the deepest point of the pocket located beneath the contact point Nabers probe- is used to detect furcation areas. • THE PERIODONTAL SCREENING AND RECORDING SYSTEM
DETERMINING THE LEVEL OF ATTACHMENT. • When the gingival margin is located on the anatomic crown, the level of attachment is determined by subtracting from the depth of the pocket the distance from the gingival margin to the cementoenamel junction. • If both are the same, the loss of attachment is zero. • When the gingival margin coincides with the cementoenamel junction, the loss of attachment equals the pocket depth.
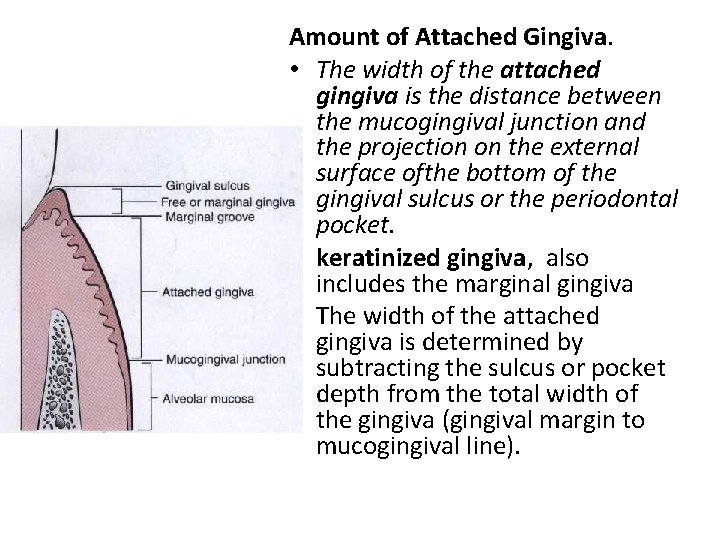
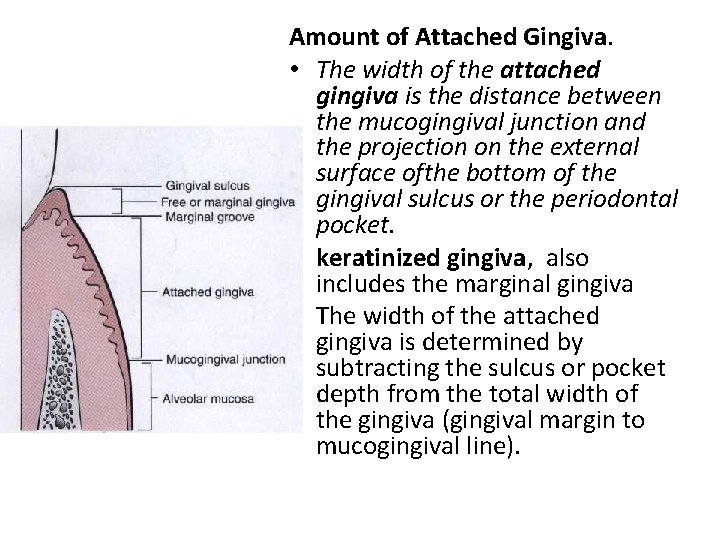
Amount of Attached Gingiva. • The width of the attached gingiva is the distance between the mucogingival junction and the projection on the external surface ofthe bottom of the gingival sulcus or the periodontal pocket. • keratinized gingiva, also includes the marginal gingiva • The width of the attached gingiva is determined by subtracting the sulcus or pocket depth from the total width of the gingiva (gingival margin to mucogingival line).
Degree of Gingival Recession. • During periodontal examination, it is necessary to record the data regarding the amount of gingival recession. This measurement is taken with a periodontal probe from the cementoenamel junction to the gingival crest. • . Alveolar Bone Loss. Alveolar bone levels are evaluated by clinical and radiographic examination. Probing is helpful for determining (1) the height and contour of the facial and lingual bones obscured on the radiograph by the dense roots and (2) the architecture of the interdental bone. Transgingival probing, performed after the area is anesthetized, .
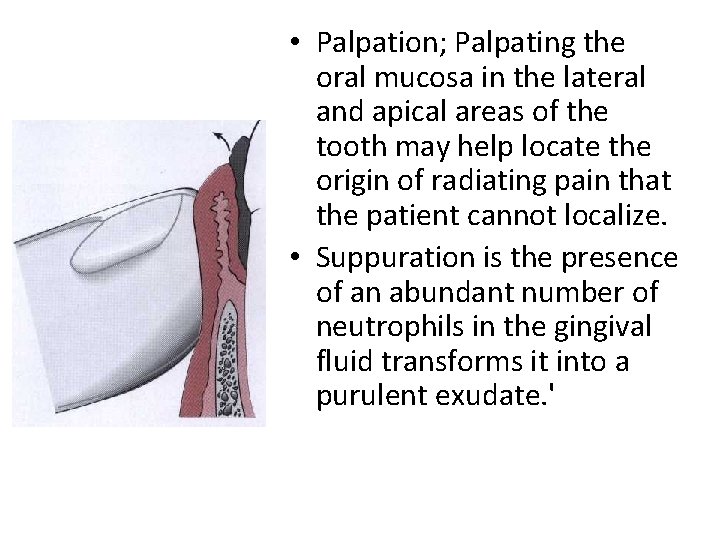
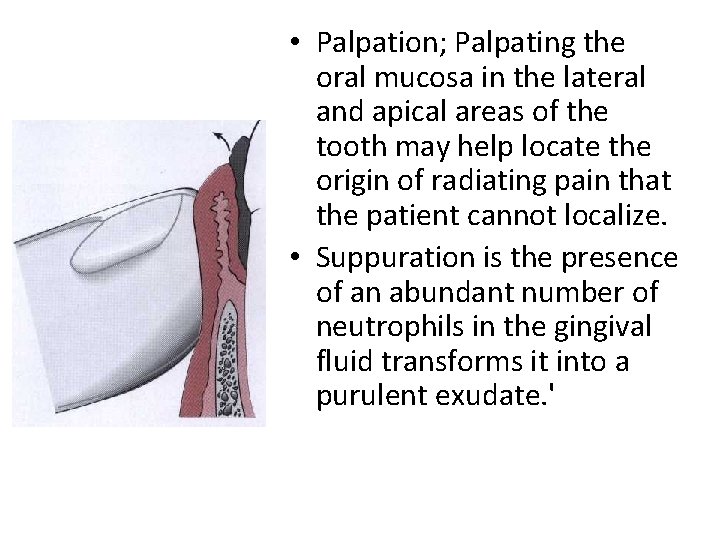
• Palpation; Palpating the oral mucosa in the lateral and apical areas of the tooth may help locate the origin of radiating pain that the patient cannot localize. • Suppuration is the presence of an abundant number of neutrophils in the gingival fluid transforms it into a purulent exudate. '
• The acute periodontal abscess is accompanied by symptoms such as throbbing, radiating pain; exquisite tenderness of the gingiva to palpation; sensitivity of the tooth to palpation; tooth mobility; lymphadenitis; and, • less frequently, systemic effects such as fever
• LABORATORY AIDS TO CLINICAL DIAGNOSIS • Analyses of blood smears, red and white blood cell counts, white blood cell differential counts, and erythrocyte sedimentation rates are used to evaluate the presence of blood dyscrasias and generalized infections. Determination of coagulation time, bleeding time, clot retraction time, prothrombin time, capillary fragility test, and bone marrow studies may be required at times. • They may be useful aids in the differential diagnosis of certain types of periodontal diseases;
Patients on salt-free diets • should not be given saline mouthwashes, nor should they be treated with saline preparations without consulting their physician. Diabetes, gallbladder disease, and hypertension are examples of conditions in which particular care should be taken to avoid the prescription of contraindicated foodstuffs.