Diagnosis and Treatment of Deep Venous Thrombosis and
Diagnosis and Treatment of Deep Venous Thrombosis and Pulmonary Embolism Beth Stuebing, MD, MPH
History n Susruta (Ayurveda physician and surgeon, 600 -1000 B. C. ) – patient with a “swollen and painful leg that was difficult to treat” n Giovanni Battista Morgagni, 1761 – recognized clots in pulmonary arteries after sudden death, but didn’t make the connection to DVT
Virchow Strikes Again n “Discovered” PE in 1846 – “the detachment of larger or smaller fragments from the end of a softening thrombus which are carried along the current of blood and driven into remote vessels. This gives rise to the very frequent process on which I have bestowed the name Embolia”
Deep Venous Thrombosis - Epidemiology n 1969 paper by Kakker – 30% of post-op patients develop clot in calf veins – 35% of these lysed within 72 hrs – 15% of pts with persistent thrombosis developed PE n n Recent studies put incidence at 50 per 100, 000 person years Incidence greatly increases with age, 18% of 80 yr old patients have asymptomatic DVT

DVT Diagnosis n n n Wells clinical prediction rules D dimer ELISA assay >90% sensitive, but 4050% specific When D dimer is negative and clinical suspicion low, further studies are unwarranted Ultrasound most sensitive and specific (>90%) for symptomatic, proximal vein US only 50 -70% sensitive for asymptomatic pts Sens. And spec. much lower for symptomatic arm DVT (60 -90%)

DVT Treatment (medicine) n n n n Initial treatment with UFH or LMWH Goal aptt (with heparin) 1. 5 -2. 5 x nl 25% pts resistant to heparin, better to monitor anti-factor Xa instead LMWH monitoring not necessary, but can be done with goal anti Xa level 0. 6 -1 U/ml (drawn 4 hr after dose) Age increases bleeding risk Some studies suggest lower mortality with LMWH in elderly Transition to warfarin (goal INR 2 -3), or continue with LMWH Starting with large doses (10 mg) NOT recommended 3 months treatment with temporary, known risk factor (fracture, pregnancy, air travel) At least 6 months treatment with no discernible cause Hypercoagulable workups not necessary in the elderly Length of treatment a risk: benefit analysis Major bleeding risk 1 -3% per year with INR 2 -3

DVT Treatment - Filters n n Consider in pts with contraindications to anticoagulation or develop recurrent DVT or PE despite adequate medical therapy Randomized trial of anticoagulation +/- IVCF: – PE at day 12 reduced with filter, but benefit didn’t persist – Double risk of recurrent DVT with IVCF
Pulmonary Embolism Epidemiology n n 1/3 of people with DVT may develop symptomatic PE 1975 paper – – – Incidence 630, 000 per year Death within 1 hour in 11% Undiagnosed 1 hr survivors: eventual 30% mortality – Diagnosed 1 hr survivors (treated): 8% mortality
PE Diagnosis n n n n Clinical diagnosis is nonsensitive and nonspecific ECG ABG CXR Angiogram VQ scan ECHO CT chest

ECG Changes n n n n “S 1 Q 3 T 3” S wave in lead I Q wave in lead III Flipped T in lead III Possible RBBB Signs of cor pulmonale Classic, but uncommon
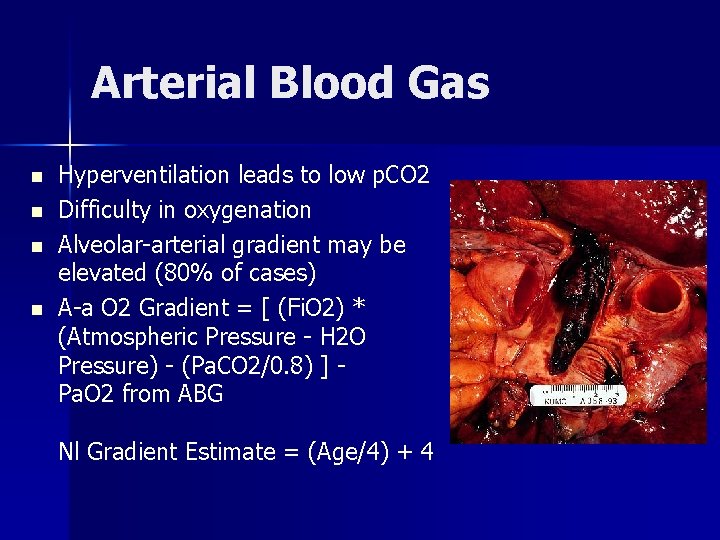
Arterial Blood Gas n n Hyperventilation leads to low p. CO 2 Difficulty in oxygenation Alveolar-arterial gradient may be elevated (80% of cases) A-a O 2 Gradient = [ (Fi. O 2) * (Atmospheric Pressure - H 2 O Pressure) - (Pa. CO 2/0. 8) ] - Pa. O 2 from ABG Nl Gradient Estimate = (Age/4) + 4

CXR – even post mortem! n Westermark sign - ischemia appeared as a clarified Westermark sign - area with diminished vascularity corresponding to the extent of the embolized artery
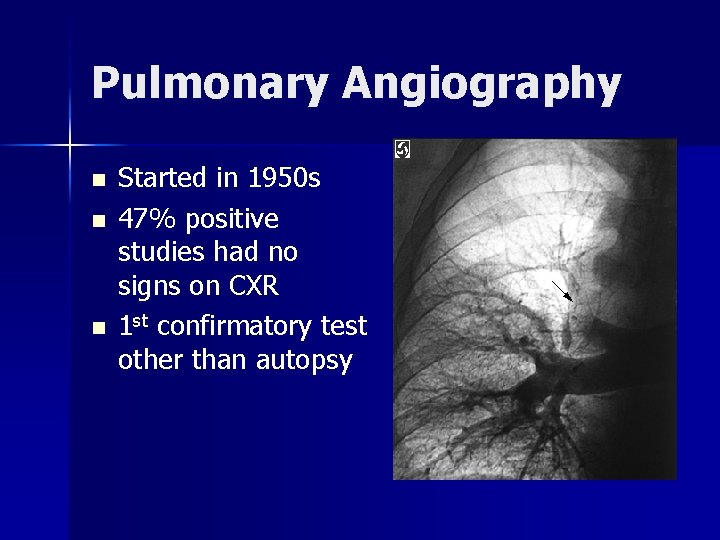
Pulmonary Angiography n n n Started in 1950 s 47% positive studies had no signs on CXR 1 st confirmatory test other than autopsy

VQ scan n n Started in 1960 s Correlated well with angiogram and autopsy “High probability” scans: 41% sensitive, 97% specific Adequate for diagnosis in a minority of patients

ECHO for PE RV dilates and LV is smaller in most patients n Unreliable in pts with prior cardiac dysfunction n TEE reported to be >90% sensitive and specific n Right heart dysfunction resolves after thrombolytic therapy n
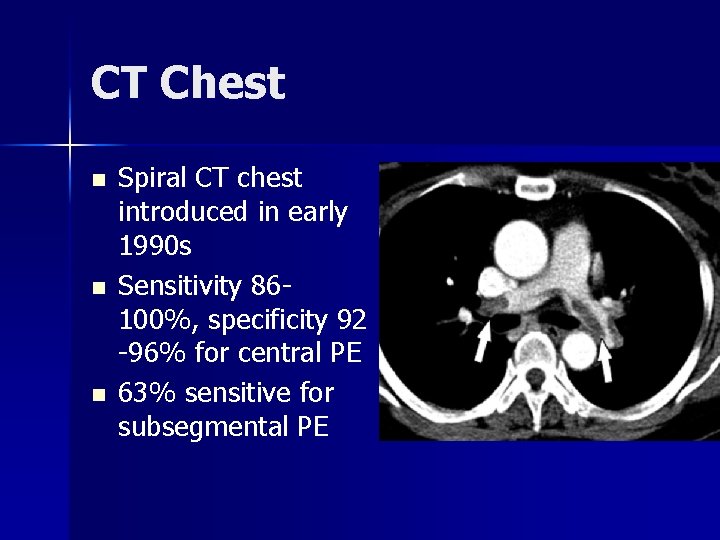
CT Chest n n n Spiral CT chest introduced in early 1990 s Sensitivity 86100%, specificity 92 -96% for central PE 63% sensitive for subsegmental PE
PE Treatment Heparin n Embolectomy n Thrombolytics n Venous interruption n IVC filter n
Heparin - Warfarin Not used until 1940 s n Only prospective randomized trial in 1960 s n – 2 weeks of anticoagulation after PE – No deaths or nonfatal PE in treatment group n 1990 s - LMWH found equally effective

Trendelenburg’s Procedure n n n Thromboembolectomy, described in 1908 First survivor of the procedure not until 1924 Via left chest thoracotomy
Thrombolytics Introduced in 1960 s n Unclear benefit over heparin, significant bleeding risk n Now used for massive PE with hemodynamic deterioration n Can be direct or systemic n 2 -3% risk intracranial hemorrhage n

Venous Interruption Started with femoral vein ligation in 1930 s n 1940 s, Homan suggested IVC ligation instead n Led to the first IVC nonextractable filter in 1969 n

IVC Filters n Decousus, et. al. , 1998 randomized trial for DVT: heparin/warfarin alone versus heparin/warfarin plus IVCF – No difference in 2 year mortality – Less PE but more recurrent DVT in filter group
Prevention 1960 s study: heparin q 12 h for 7 days after major surgery decreased DVT from 42% to 8% n Established as standard of care after 1975 study with similar results n 60 -70% relative risk reduction for DVT and fatal PE post-op n

DVT and PE in the ICU n n One study: routine Doppler shows DVT in up to 30 -40% of all ICU patients, regardless of prophylaxis Much less likely to have physical exam findings One study showed 38% of ICU pts with known DVT had undiagnosed PE on VQ scan One autopsy study: 84% of PE were not diagnosed antemortem
DVT and PE in the ICU n n Chemical prevention has similar risk reduction of 60 -70%, variety of meds studied CT chest is higher risk (contrast load, travel with critical patient) and often unfeasible VQ scans essentially uninterpretable given multitude of pulmonary pathology Higher risk: personal or family history, renal failure, platelet transfusion, vasopressor use, longer time on ventilator
Thanks, and Questions?
- Slides: 26