Diagnosis and Treatment of Celiac Disease in Children

- Slides: 40
Diagnosis and Treatment of Celiac Disease in Children Dr. Fawaz ALRefaee, MBBS FAAP FRCPC Pediatric Gastroenterologist, Al-Adan Hospital KMA Conferance March 18, 2016
Outline -Case presentation -Definition -Epidemiology -Clinical features -Pathogenesis -Diagnosis -Treatment
Case presentation � 14 month old F with FTT �Watery diarrhea x 2 months; 3 -10 episodes per day; stool infectious work-up by PCP negative �No nausea, vomiting, abdominal pain, abdominal distention, hematochezia, melena �No improvement in symptoms with change to soy milk �No significant PMH or FH �PE: Pale skin, abdomen distended but soft and nontender, normal bowel sounds, no organomegaly
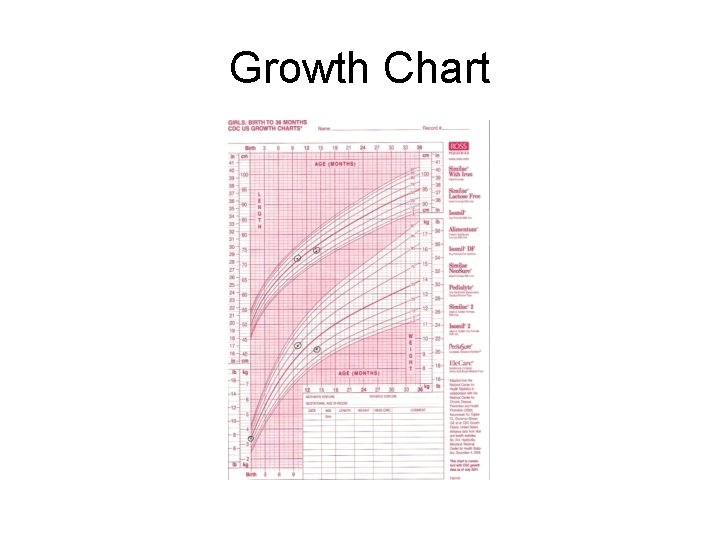
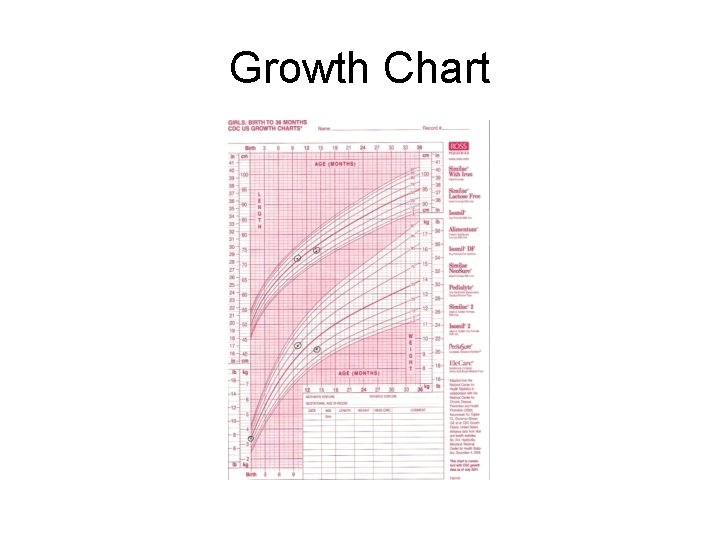
Growth Chart
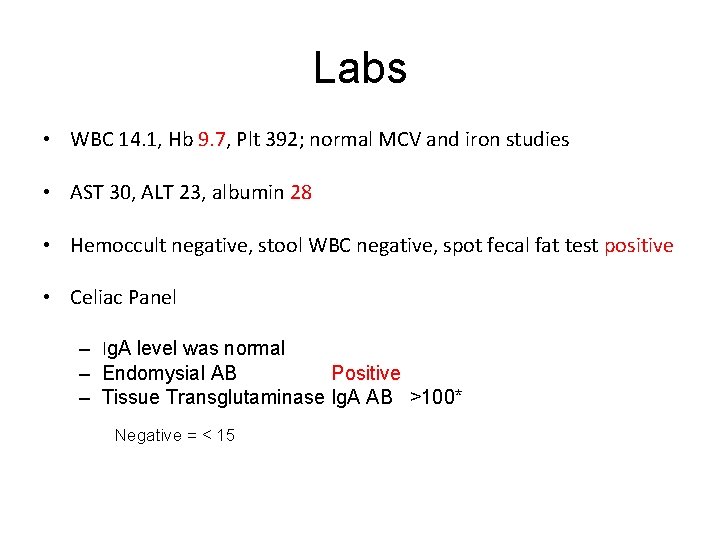
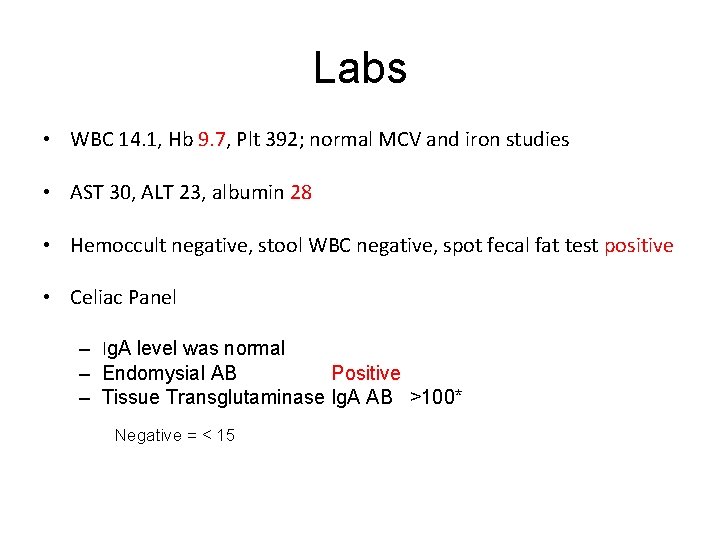
Labs • WBC 14. 1, Hb 9. 7, Plt 392; normal MCV and iron studies • AST 30, ALT 23, albumin 28 • Hemoccult negative, stool WBC negative, spot fecal fat test positive • Celiac Panel – Ig. A level was normal – Endomysial AB Positive – Tissue Transglutaminase Ig. A AB >100* Negative = < 15
What is Celiac Disease? • Auto-immune condition • Occurs in genetically susceptible individuals • A unique autoimmune disorder because… – Environmental trigger (gluten) and the autoantigen (tissue-transglutaminase) are known – Elimination of the environmental trigger leads to a complete resolution of the disease – Permanent sensitivity to gluten
Why is it Important? • If untreated it poses long-term adverse health consequences including: – Malabsorption – Anemia – Poor growth – Osteopenia – Intestinal lymphoma – Nutritional Deficiencies • Iron, zinc, calcium, Vitamin A, D, E, and K
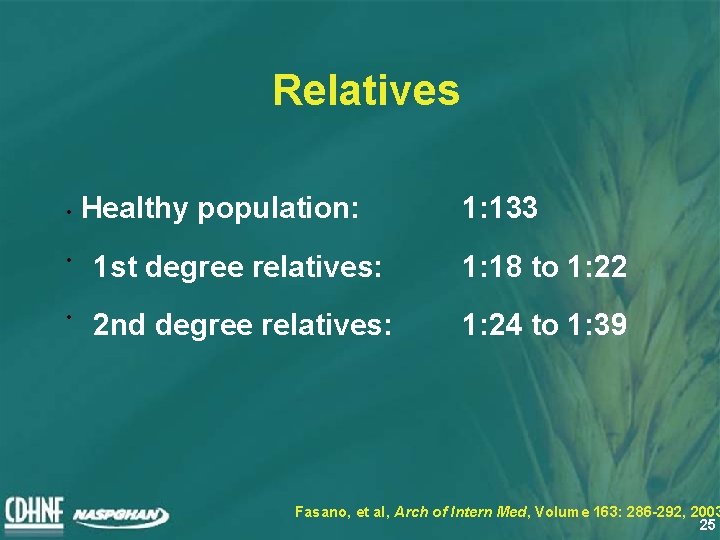
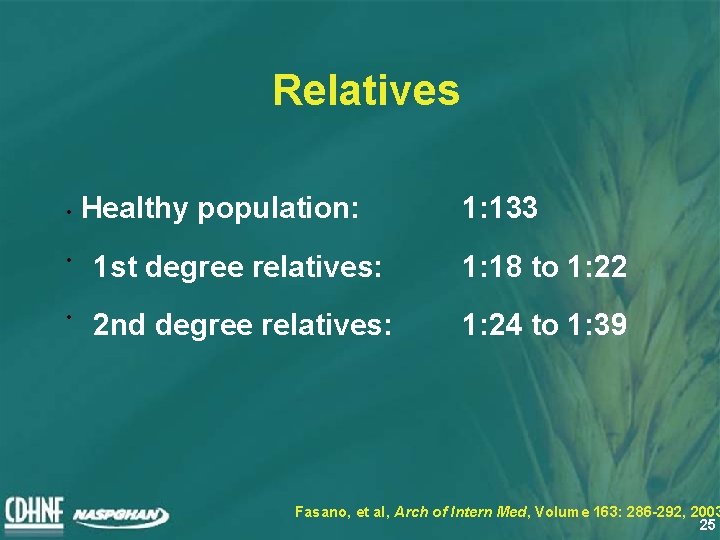
Relatives • Healthy population: 1: 133 • 1 st degree relatives: 1: 18 to 1: 22 • 2 nd degree relatives: 1: 24 to 1: 39 Fasano, et al, Arch of Intern Med, Volume 163: 286 -292, 2003 25
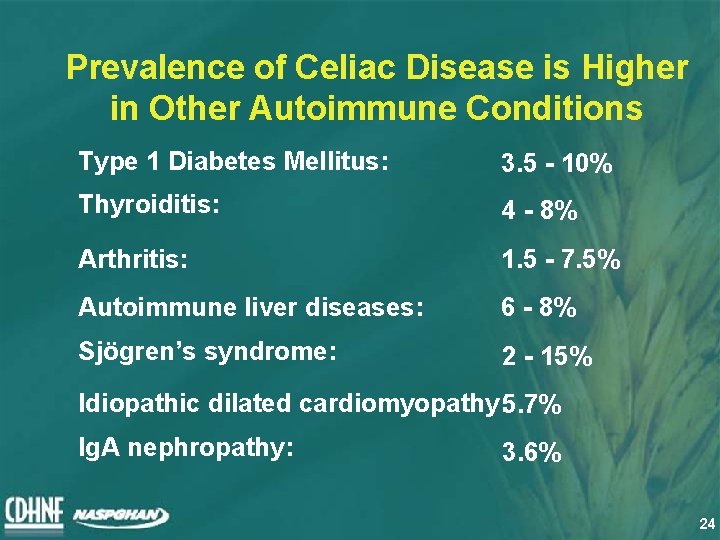
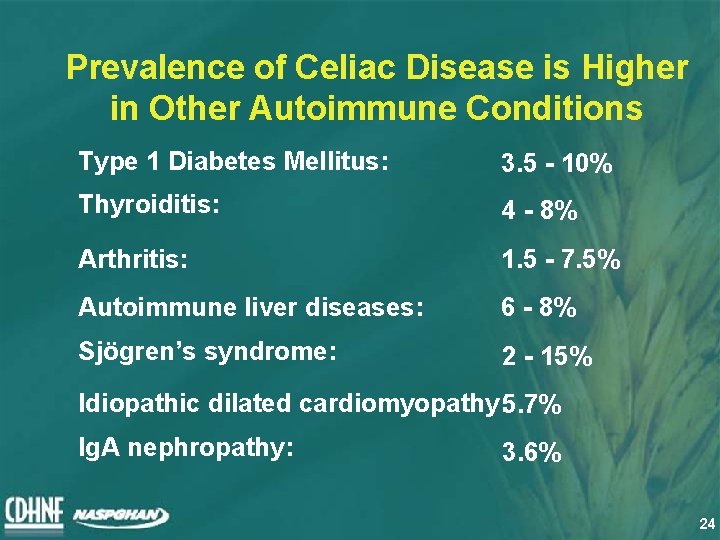
Prevalence of Celiac Disease is Higher in Other Autoimmune Conditions Type 1 Diabetes Mellitus: 3. 5 - 10% Thyroiditis: 4 - 8% Arthritis: 1. 5 - 7. 5% Autoimmune liver diseases: 6 - 8% Sjögren’s syndrome: 2 - 15% Idiopathic dilated cardiomyopathy: 5. 7% Ig. A nephropathy: 3. 6% 24
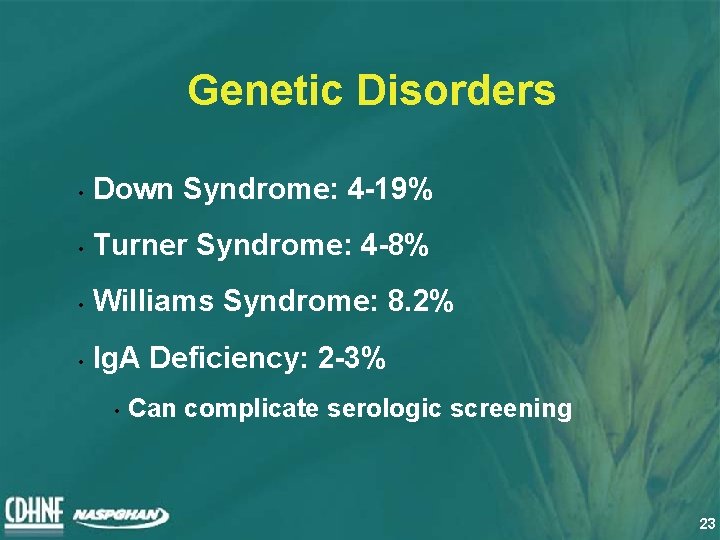
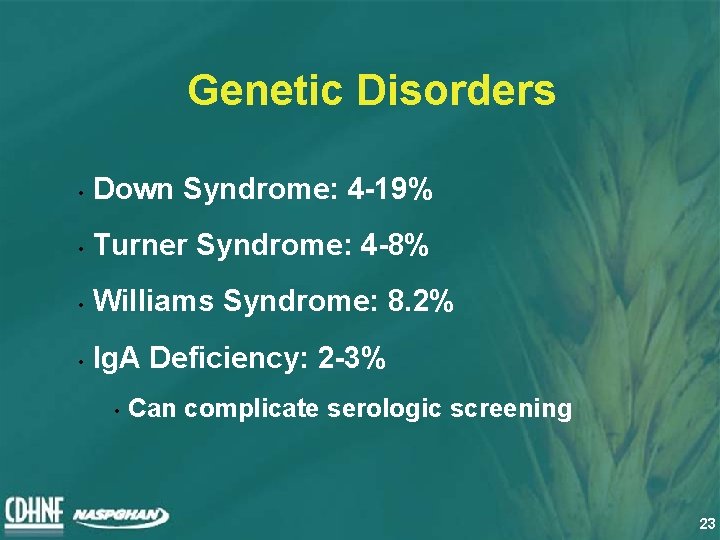
Genetic Disorders • Down Syndrome: 4 -19% • Turner Syndrome: 4 -8% • Williams Syndrome: 8. 2% • Ig. A Deficiency: 2 -3% • Can complicate serologic screening 23
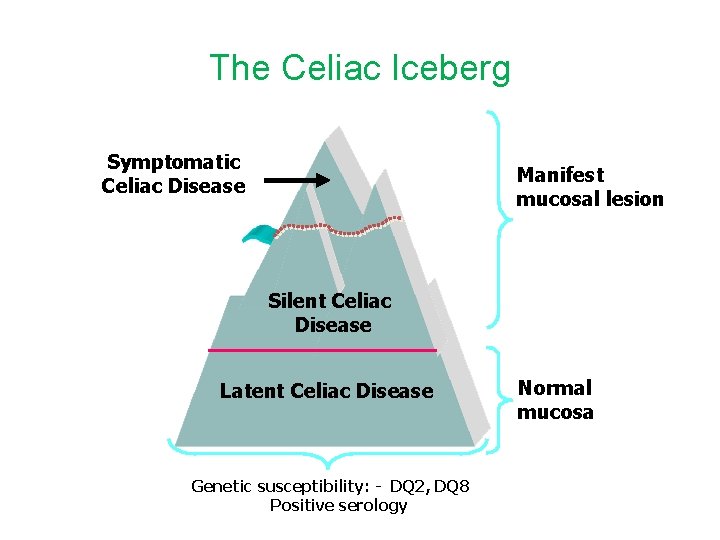
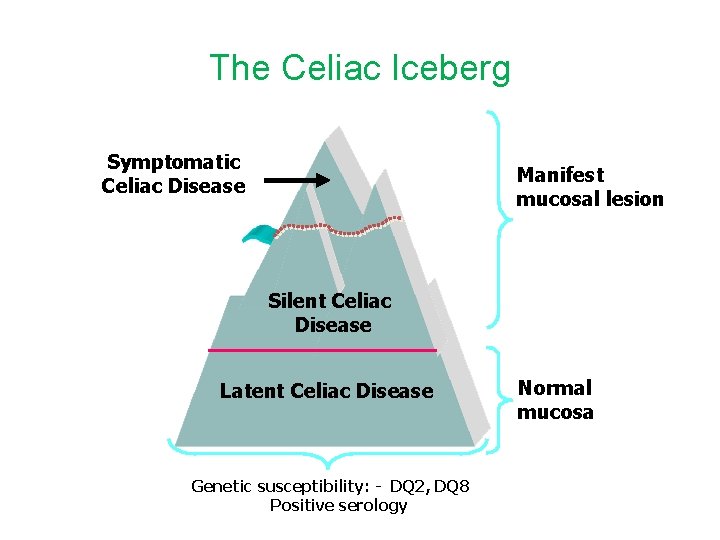
The Celiac Iceberg Symptomatic Celiac Disease Manifest mucosal lesion Silent Celiac Disease Latent Celiac Disease Genetic susceptibility: - DQ 2, DQ 8 Positive serology Normal mucosa
Risk Factors for Celiac Disease The Grains The Genes
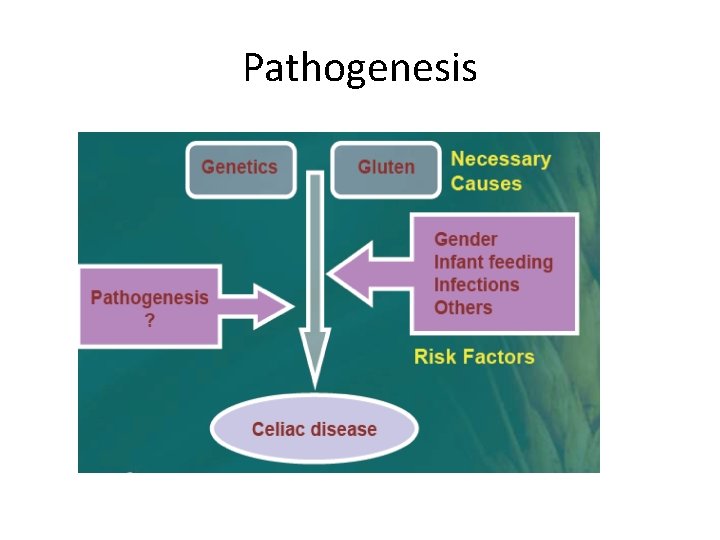
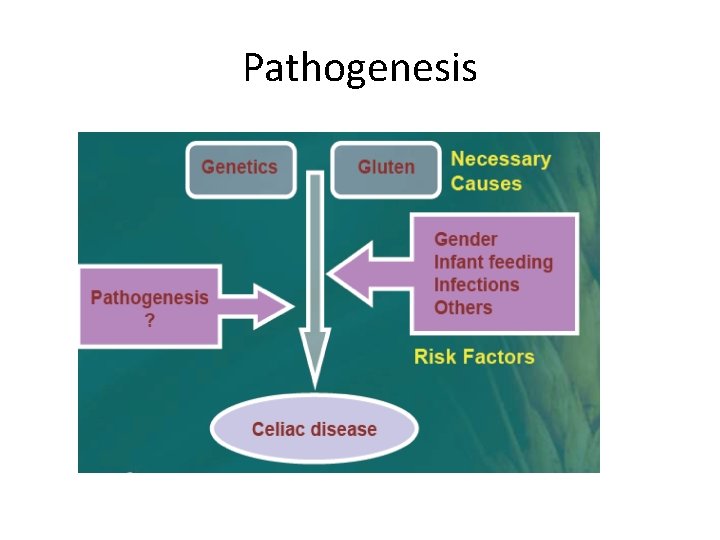
Pathogenesis
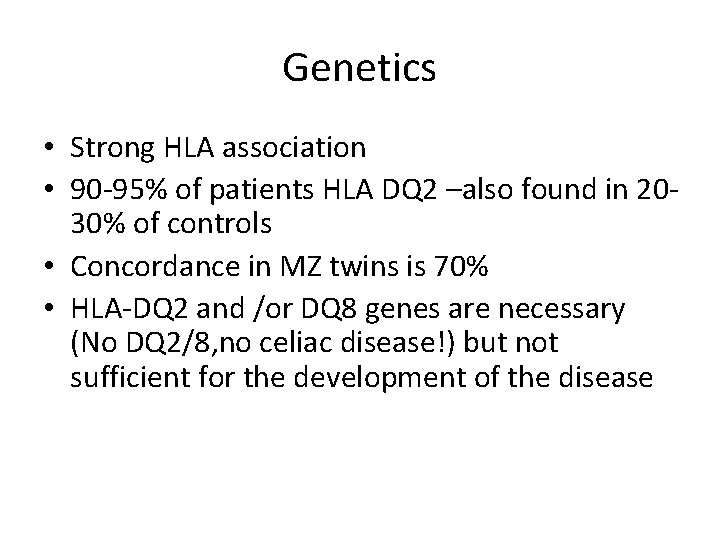
Genetics • Strong HLA association • 90 -95% of patients HLA DQ 2 –also found in 2030% of controls • Concordance in MZ twins is 70% • HLA-DQ 2 and /or DQ 8 genes are necessary (No DQ 2/8, no celiac disease!) but not sufficient for the development of the disease
Clinical Manifestations • Gastrointestinal Symptoms (“Classic”) • Chronic or recurrent diarrhea • Abdominal distention • Abdominal pain • Vomiting • Anorexia • Failure to thrive or weight loss • Constipation • Irritability
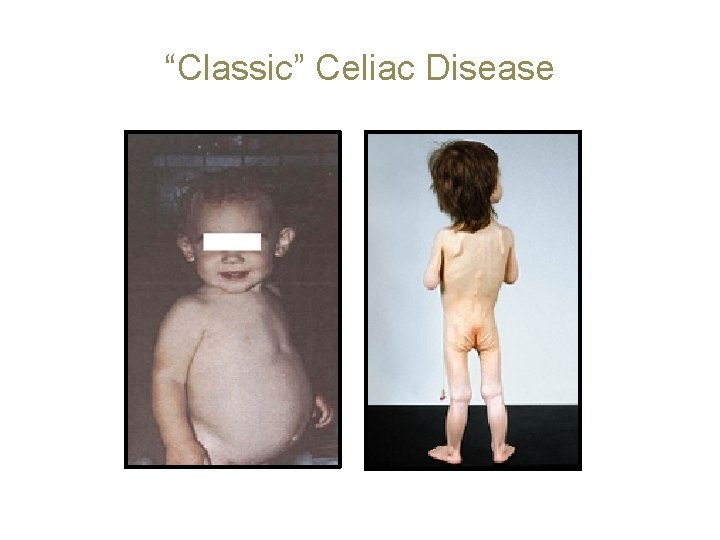
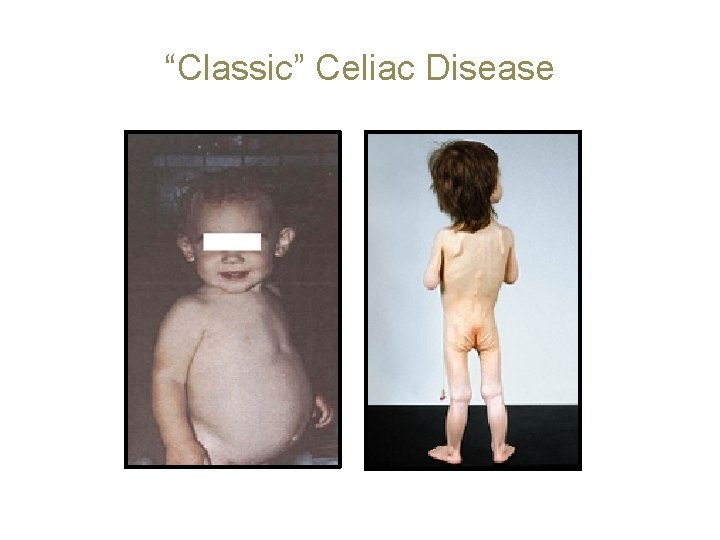
“Classic” Celiac Disease
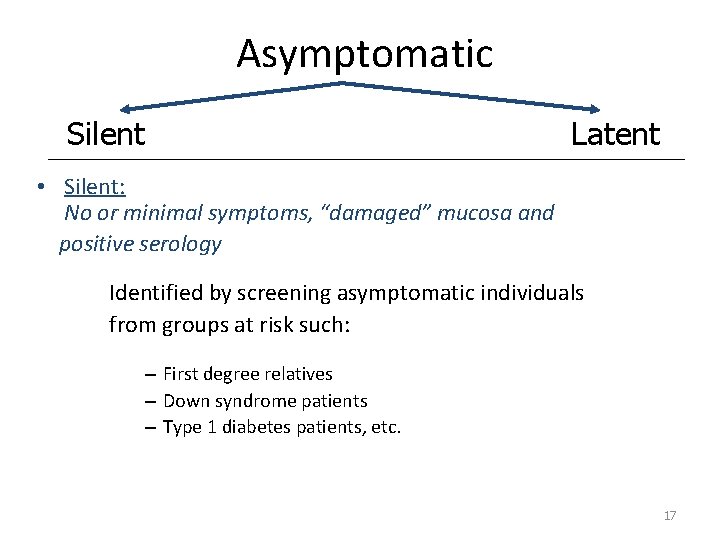
Asymptomatic Silent Latent • Silent: No or minimal symptoms, “damaged” mucosa and positive serology Identified by screening asymptomatic individuals from groups at risk such: – First degree relatives – Down syndrome patients – Type 1 diabetes patients, etc. 17
Asymptomatic Silent • Latent: No symptoms, normal mucosa – May show positive serology. Identified by following in time asymptomatic individuals previously identified at screening from groups at risk. These individuals, given the “right” circumstances, will develop at some point in time mucosal changes (± symptoms) 18
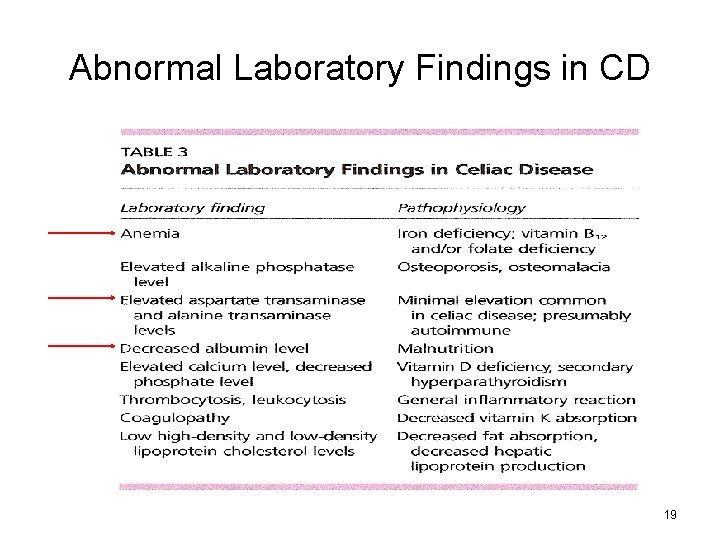
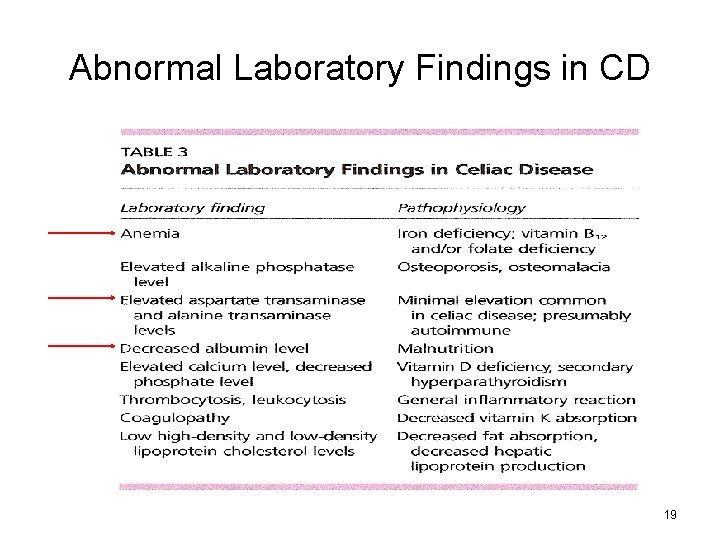
Abnormal Laboratory Findings in CD 19
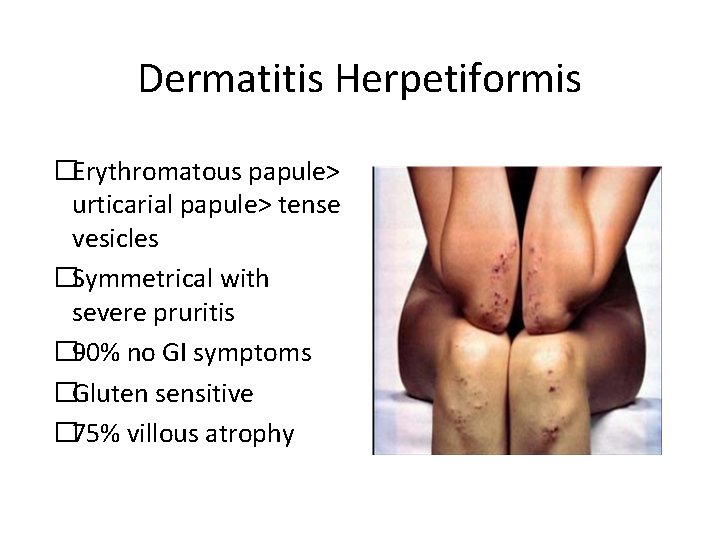
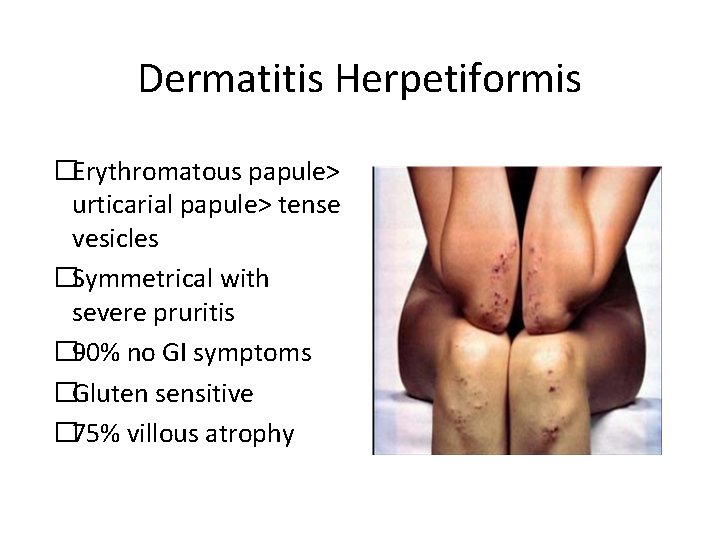
Dermatitis Herpetiformis �Erythromatous papule> urticarial papule> tense vesicles �Symmetrical with severe pruritis � 90% no GI symptoms �Gluten sensitive � 75% villous atrophy
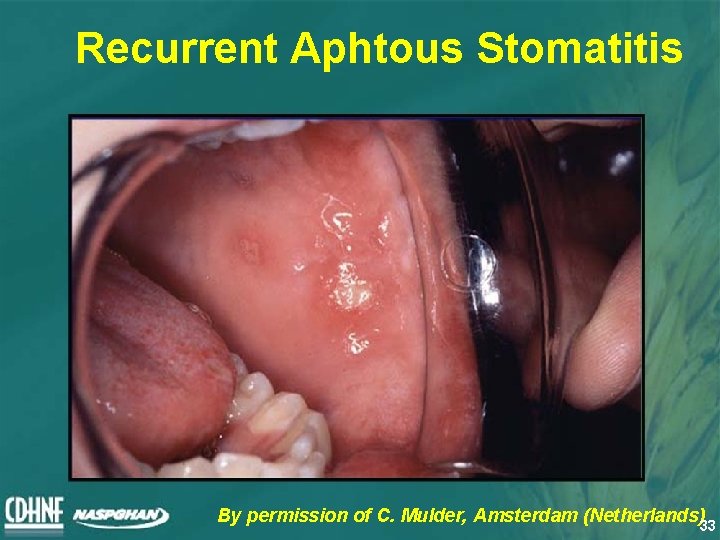
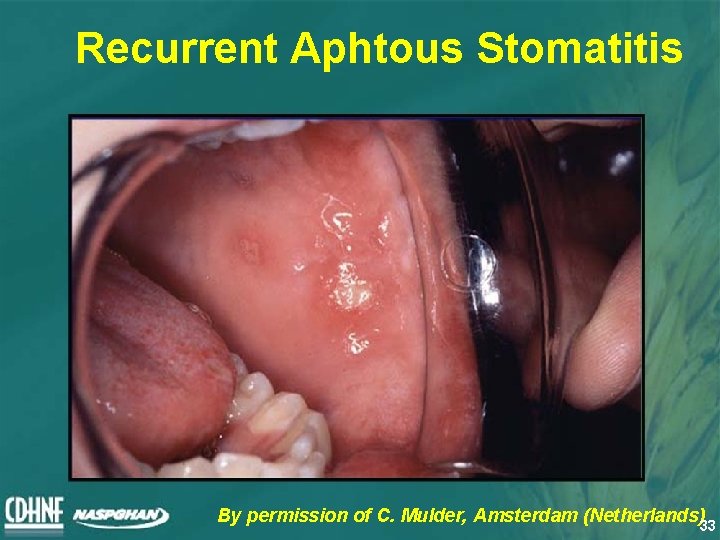
Recurrent Aphtous Stomatitis By permission of C. Mulder, Amsterdam (Netherlands)33
Short Stature/Delayed Puberty • Short stature in children/teens: • About 10% of short children and teens have evidence of celiac disease • Delayed menarche • Higher prevalence in teens with untreated celiac disease
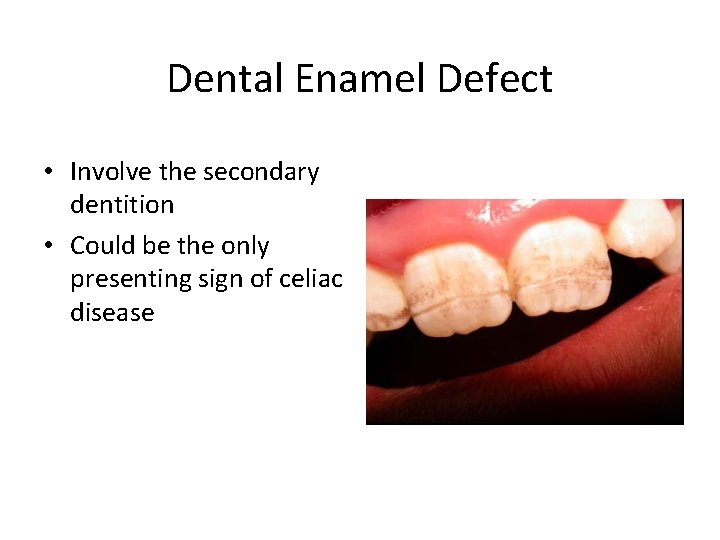
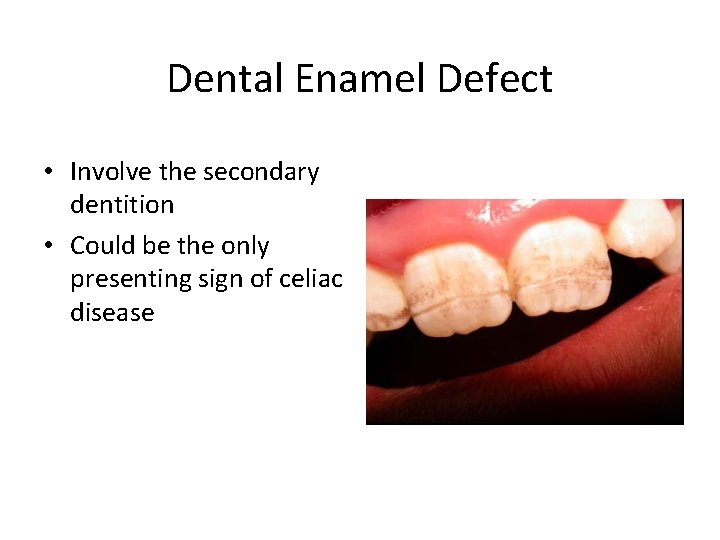
Dental Enamel Defect • Involve the secondary dentition • Could be the only presenting sign of celiac disease
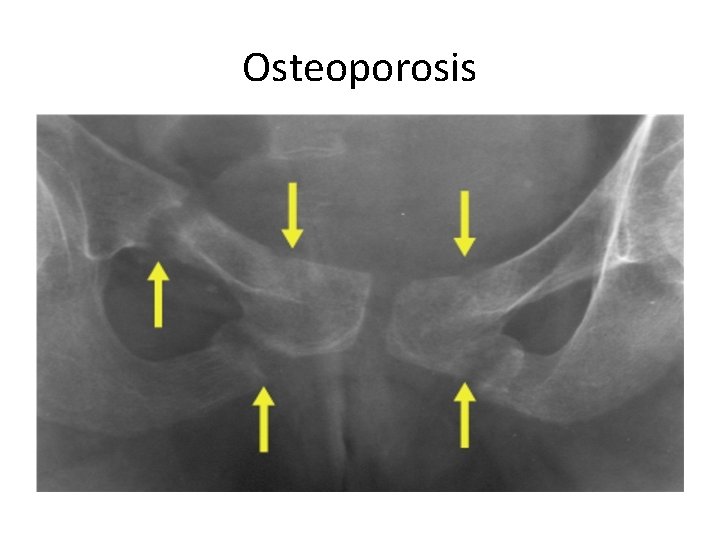
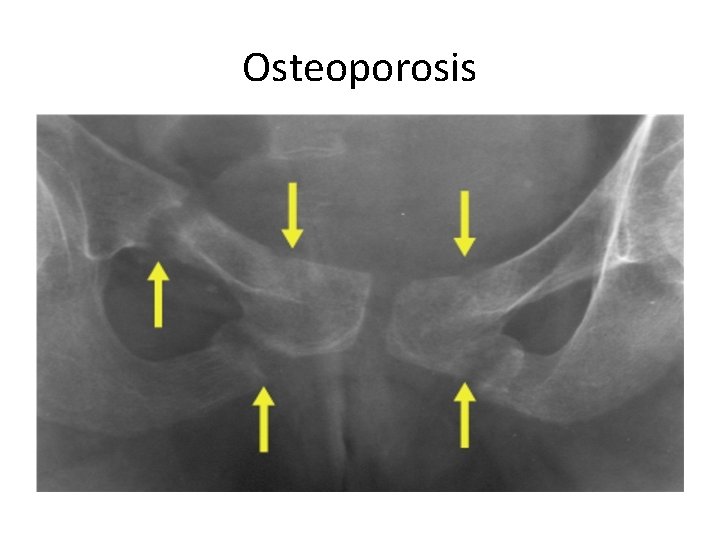
Osteoporosis
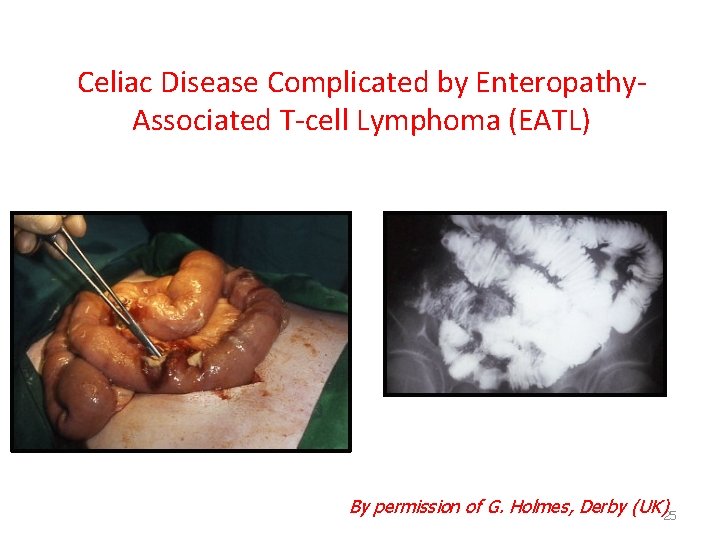
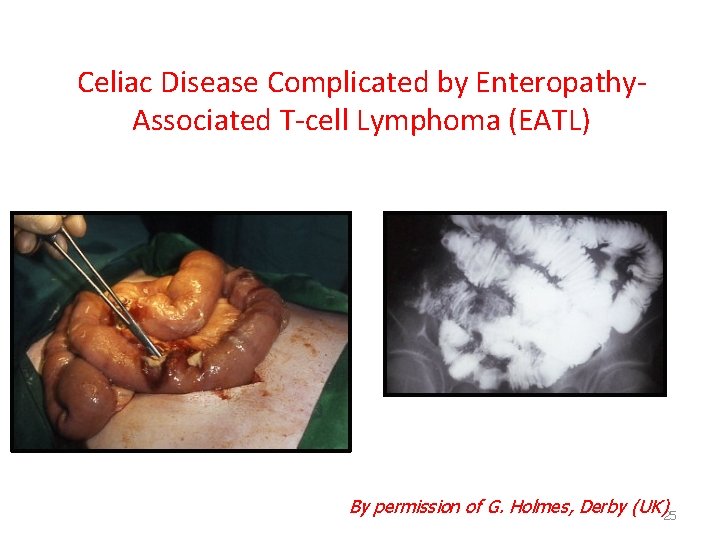
Celiac Disease Complicated by Enteropathy. Associated T-cell Lymphoma (EATL) By permission of G. Holmes, Derby (UK)25
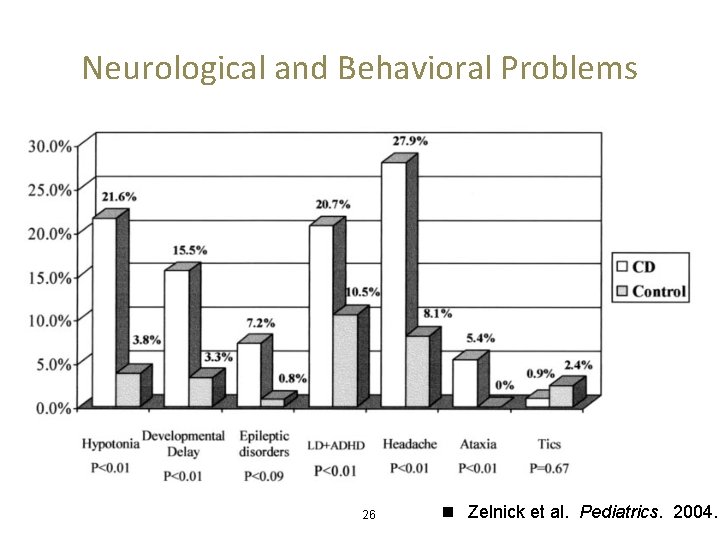
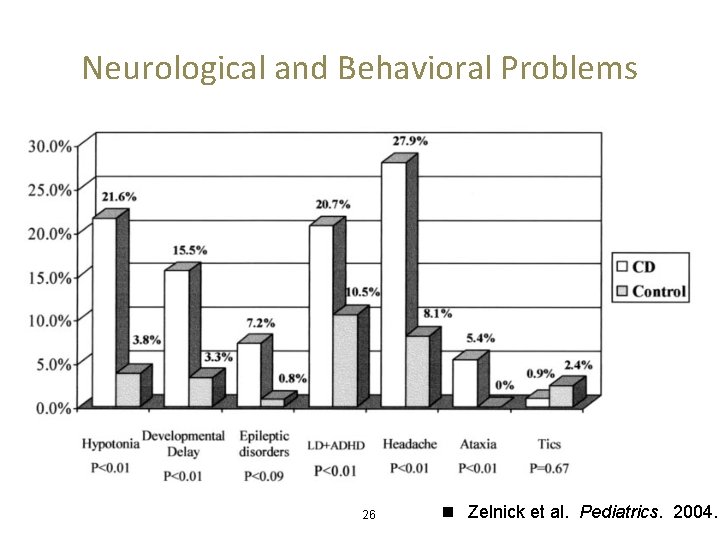
Neurological and Behavioral Problems 26 n Zelnick et al. Pediatrics. 2004.
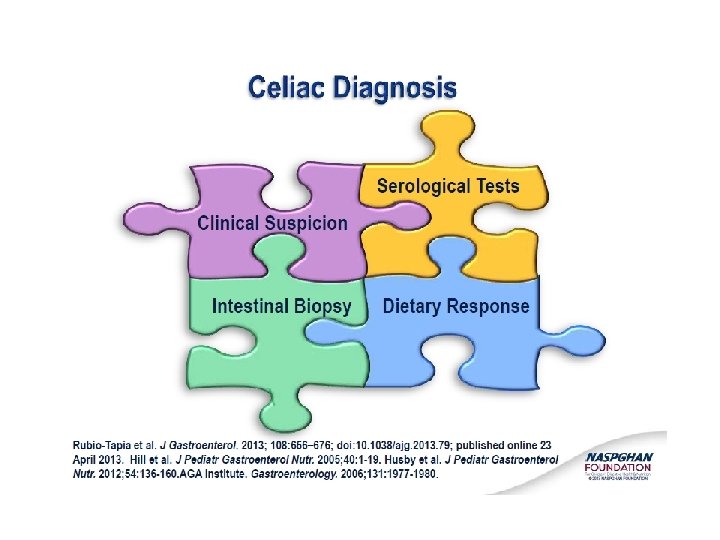
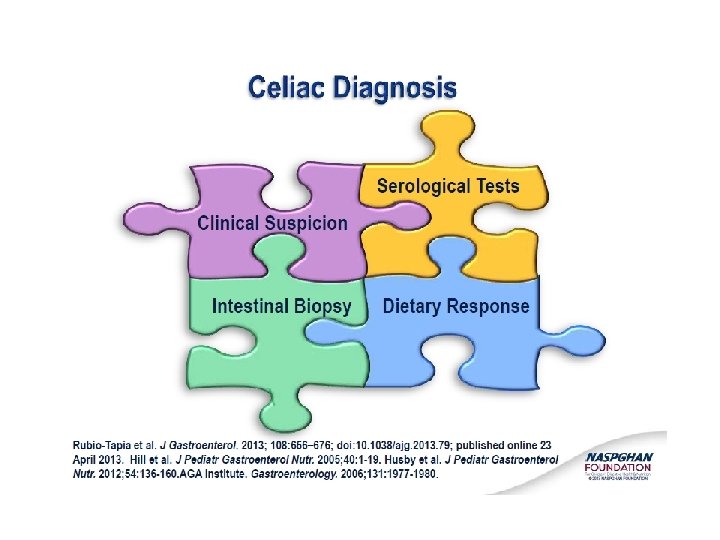
Serological Tests Role of serological tests: • Identify symptomatic individuals who need a biopsy • Screening of asymptomatic “at risk” individuals • Supportive evidence for the diagnosis • Monitoring dietary compliance 28
Tissue Transglutaminase - TTG • Ig. A based antibody against tissue transglutaminase (Celiac Disease autoantigen) • Advantages – high sensitivity and specificity (human TTG) – non operator dependent (ELISA/RIA) – relatively cheap • Disadvantages – false negative in young children – false negative in Ig. A deficiency – possibly less specific than EMA 29
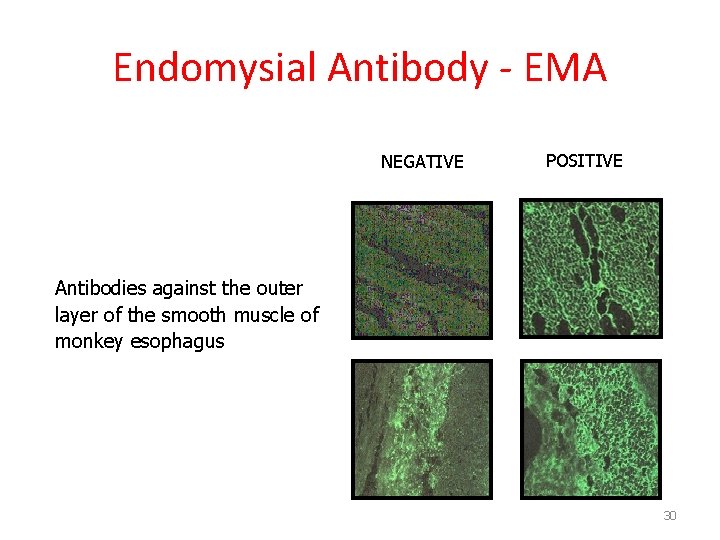
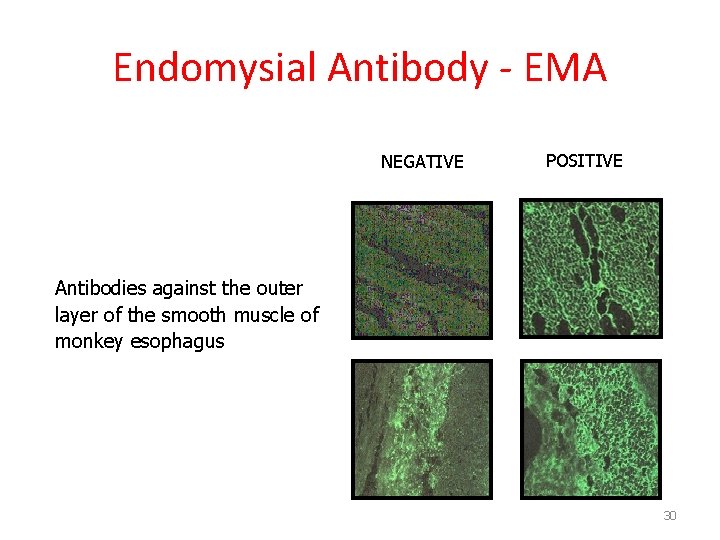
Endomysial Antibody - EMA NEGATIVE POSITIVE Antibodies against the outer layer of the smooth muscle of monkey esophagus 30
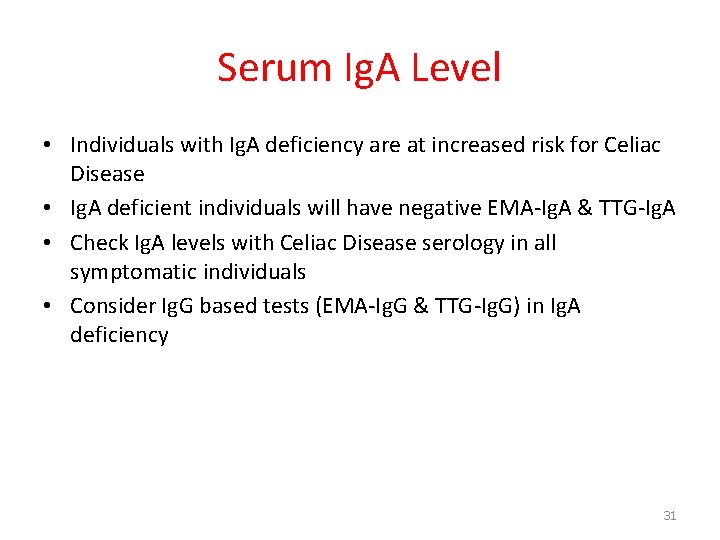
Serum Ig. A Level • Individuals with Ig. A deficiency are at increased risk for Celiac Disease • Ig. A deficient individuals will have negative EMA-Ig. A & TTG-Ig. A • Check Ig. A levels with Celiac Disease serology in all symptomatic individuals • Consider Ig. G based tests (EMA-Ig. G & TTG-Ig. G) in Ig. A deficiency 31
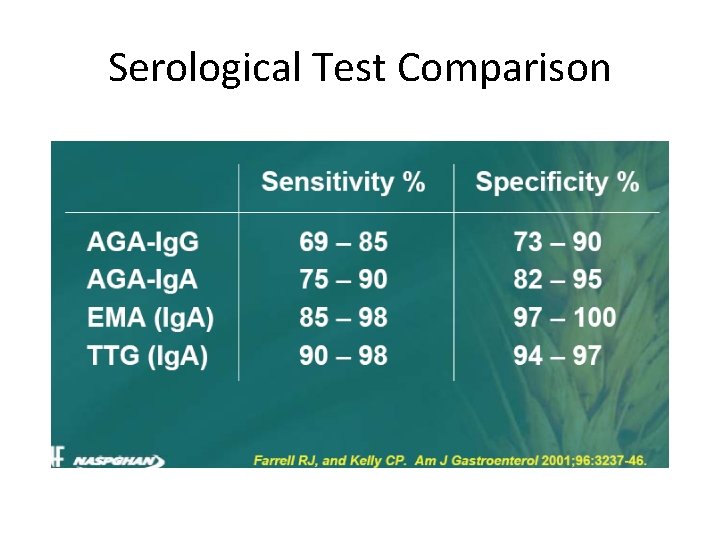
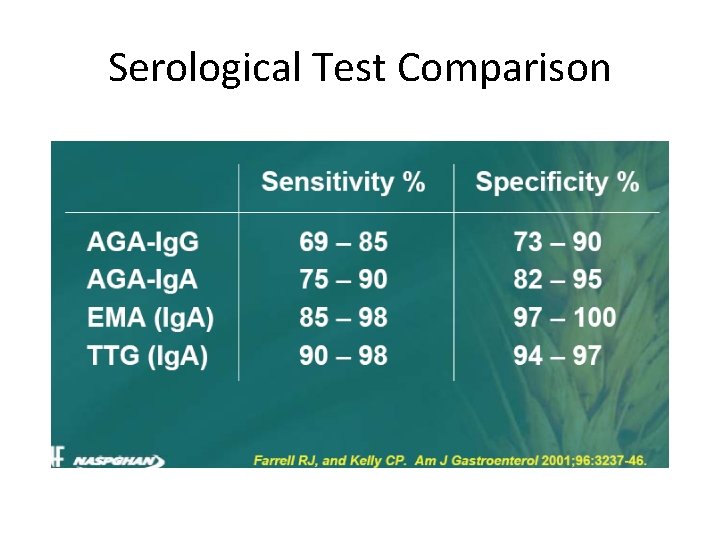
Serological Test Comparison
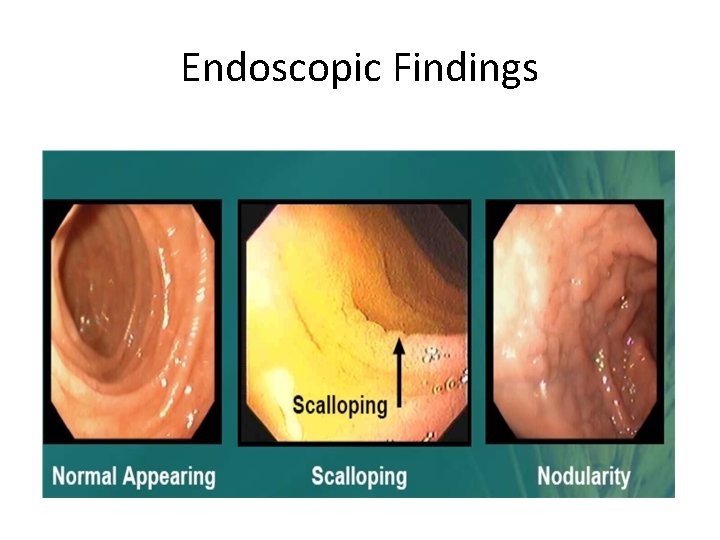
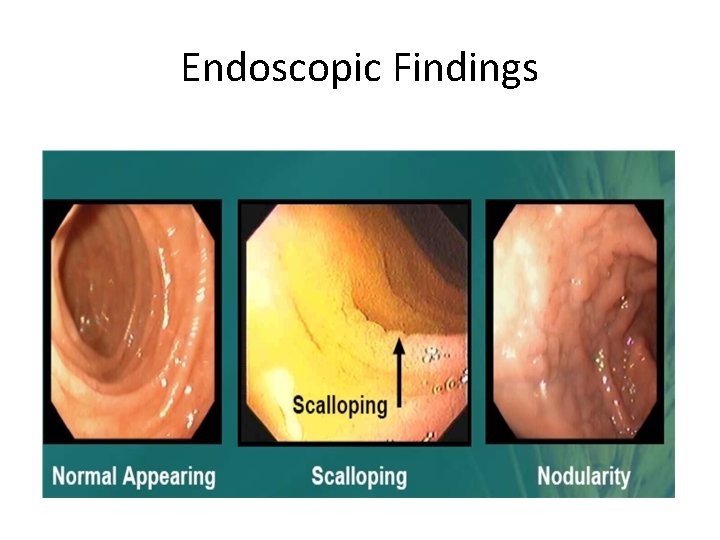
Endoscopic Findings
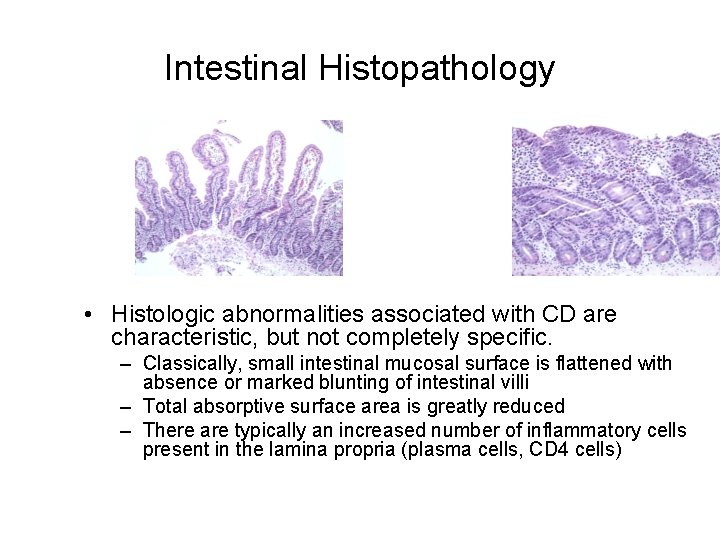
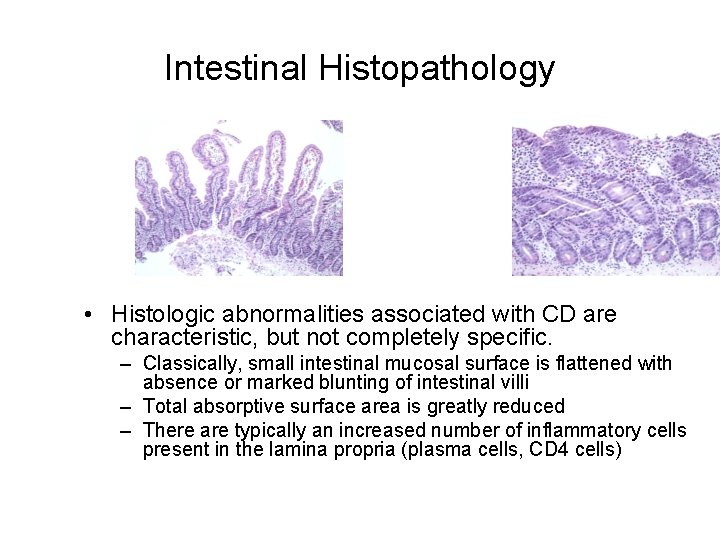
Intestinal Histopathology • Histologic abnormalities associated with CD are characteristic, but not completely specific. – Classically, small intestinal mucosal surface is flattened with absence or marked blunting of intestinal villi – Total absorptive surface area is greatly reduced – There are typically an increased number of inflammatory cells present in the lamina propria (plasma cells, CD 4 cells)
HLA Tests • Potential role for DQ 2/DQ 8 • Asymptomatic relatives • Trisomy 21, Turner & Williams syndrome • Type 1 diabetes • Diagnostic dilemmas • TTG +, EMA -, Bx -, Symptoms + 35

Treatment • Only treatment for Celiac Disease is a gluten-free diet (GFD) – Strict, lifelong diet – Avoid: • Wheat • Rye • Barley • Oats? 36
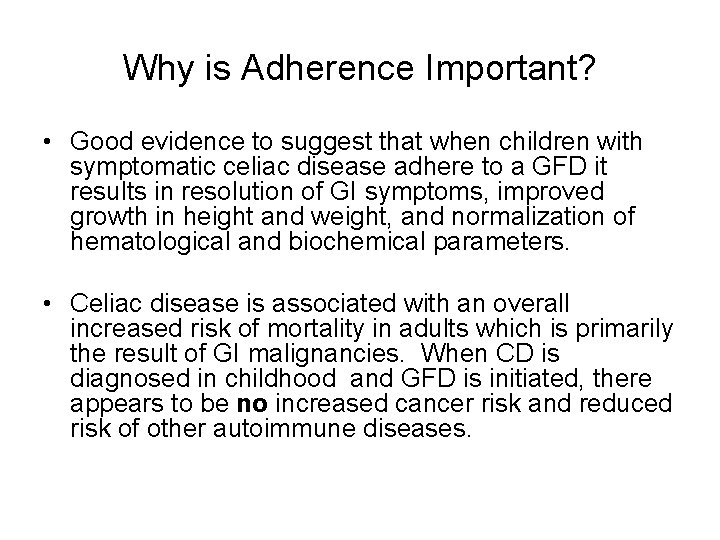
Why is Adherence Important? • Good evidence to suggest that when children with symptomatic celiac disease adhere to a GFD it results in resolution of GI symptoms, improved growth in height and weight, and normalization of hematological and biochemical parameters. • Celiac disease is associated with an overall increased risk of mortality in adults which is primarily the result of GI malignancies. When CD is diagnosed in childhood and GFD is initiated, there appears to be no increased cancer risk and reduced risk of other autoimmune diseases.
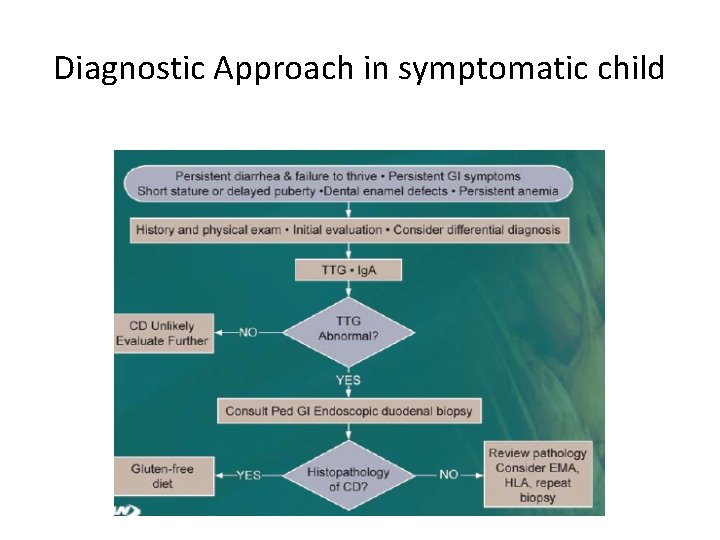
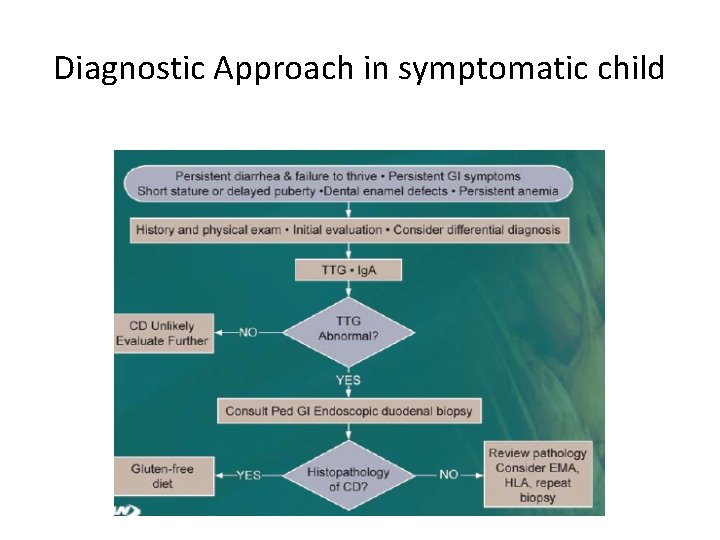
Diagnostic Approach in symptomatic child
Summary n Celiac Disease is a common, subtle enteropathy with variable presentation. n Active, appropriate screening is needed to avoid long-term complications of untreated CD. n Life long adherence to the diet is important
Thanks Questions!