Diagnosing a Noisy Breather Stridor in infants Joshua
Diagnosing a Noisy Breather: Stridor in infants Joshua Bedwell, MD, FAAP, FACS Texas Children’s Hospital
Objectives 1. Identify common causes of stridor in children 2. Discuss the appropriate evaluation and workup 3. Discuss the management options
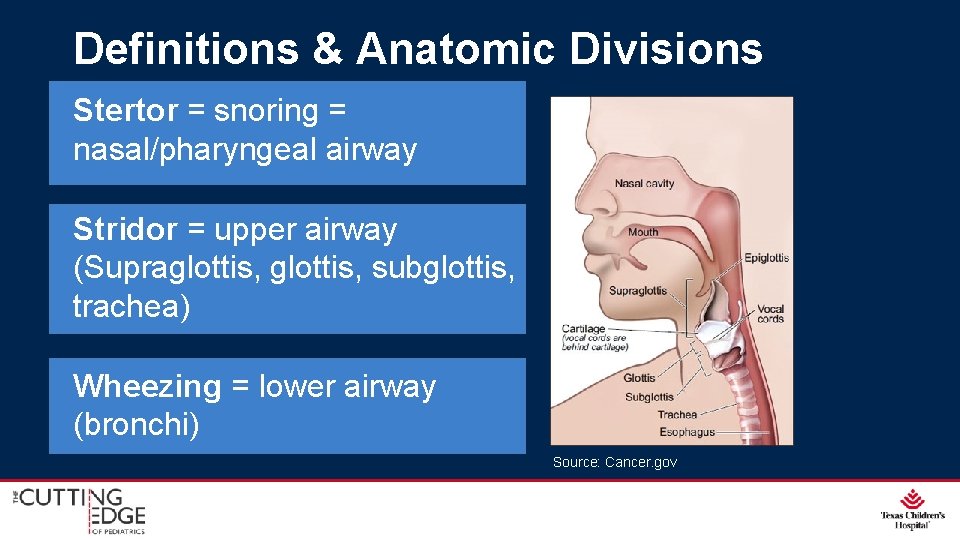
Definitions & Anatomic Divisions Stertor = snoring = nasal/pharyngeal airway Stridor = upper airway (Supraglottis, subglottis, trachea) Wheezing = lower airway (bronchi) Source: Cancer. gov
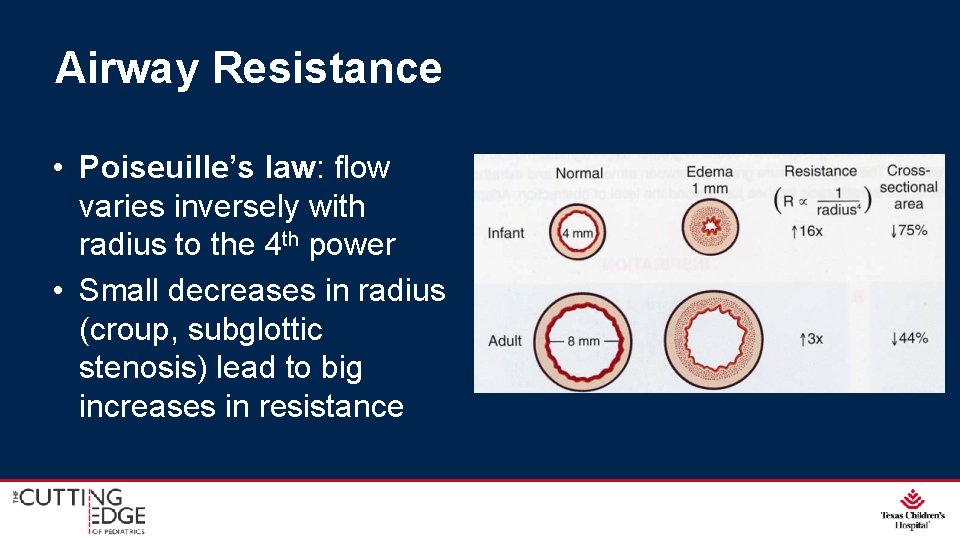
Airway Resistance • Poiseuille’s law: flow varies inversely with radius to the 4 th power • Small decreases in radius (croup, subglottic stenosis) lead to big increases in resistance

Airway Resistance Turbulent flow increases resistance
Characterizing the Problem • Age at onset: congenital, acquired • Onset: gradual, worsening, abrupt • Severity: respiratory distress, increased WOB, retractions • Timing: With feeds? Constant? Positional?
Characterizing the Problem • Birth/intubation history • Associated Findings – Apneas/Cyanotic Episodes – Voice changes – Reflux – Aspiration
Physical Findings • Retractions, tachypnea, distress • Nature of stridor – Gives an idea for anatomic site of obstruction – Inspiratory: Supraglottic – Biphasic: Glottic/subglottic/fixed tracheal – Expiratory: Tracheobronchial
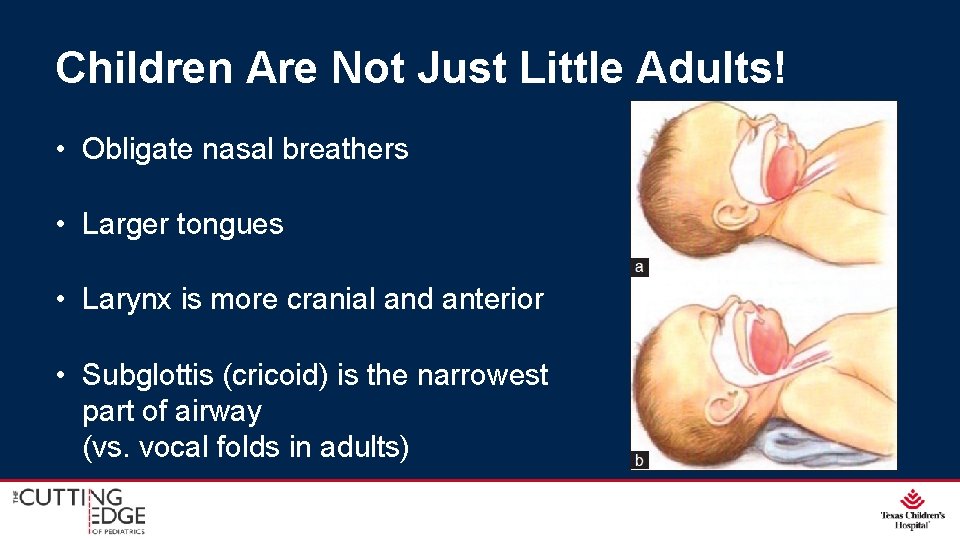
Children Are Not Just Little Adults! • Obligate nasal breathers • Larger tongues • Larynx is more cranial and anterior • Subglottis (cricoid) is the narrowest part of airway (vs. vocal folds in adults)
Workup Options
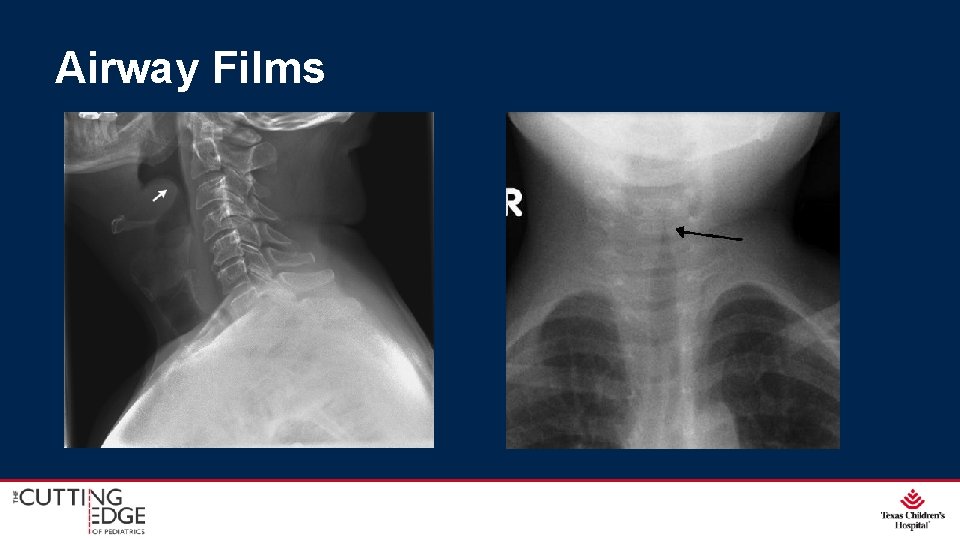
Airway Films
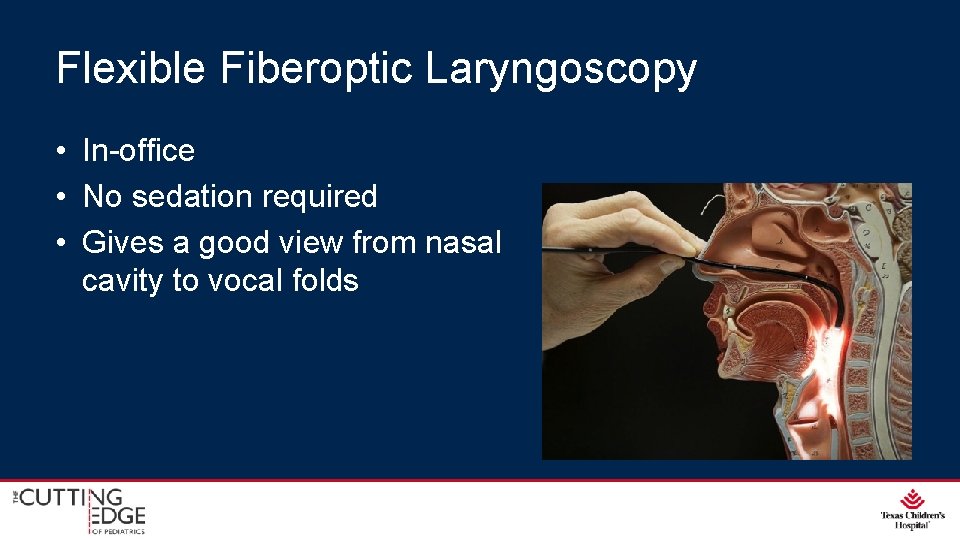
Flexible Fiberoptic Laryngoscopy • In-office • No sedation required • Gives a good view from nasal cavity to vocal folds

Direct Laryngoscopy and Bronchoscopy
What Do You Hear? A. Stertor B. Inspiratory Stridor C. Biphasic Stridor D. Expiratory Stridor
What Do You Hear? • • A. Stertor B. Inspiratory Stridor C. Biphasic Stridor D. Expiratory Stridor
What Do You Hear? • • A. Stertor B. Inspiratory Stridor C. Biphasic Stridor D. Expiratory Stridor
Audience Question What is the most common cause of stridor in infants? A. B. C. D. Vocal fold paralysis Subglottic stenosis Hemangioma Laryngomalacia
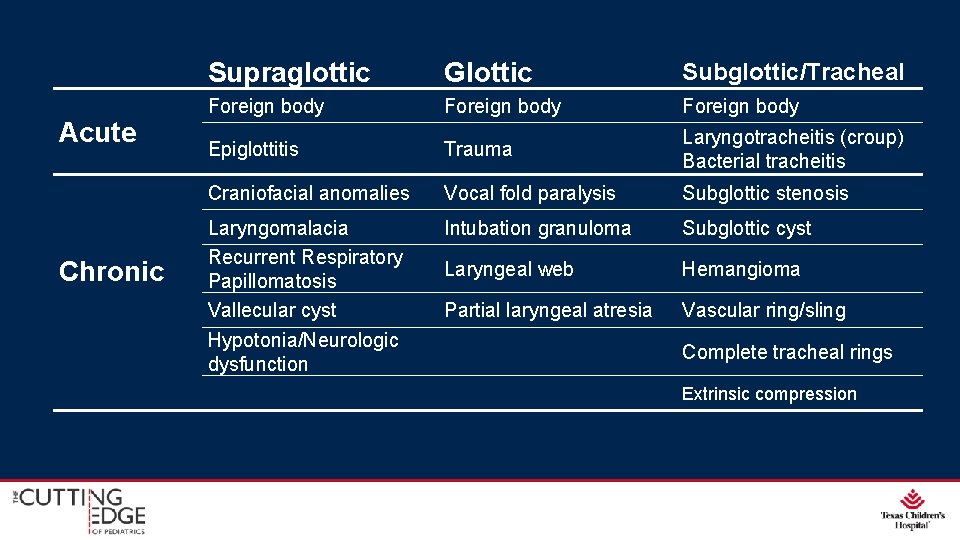
Acute Chronic Supraglottic Glottic Subglottic/Tracheal Foreign body Epiglottitis Trauma Laryngotracheitis (croup) Bacterial tracheitis Craniofacial anomalies Vocal fold paralysis Subglottic stenosis Laryngomalacia Recurrent Respiratory Papillomatosis Vallecular cyst Hypotonia/Neurologic dysfunction Intubation granuloma Subglottic cyst Laryngeal web Hemangioma Partial laryngeal atresia Vascular ring/sling Complete tracheal rings Extrinsic compression

Case Presentation
HPI • 2 week old male with noisy breathing since birth • Increases when feeding and when lying supine vs. sitting upright • Nursing takes a long time, with frequent need for breaks and gagging • Spits up after nearly every feed • No apneic spells or cyanosis PMH • Full-term, uncomplicated delivery • Otherwise healthy
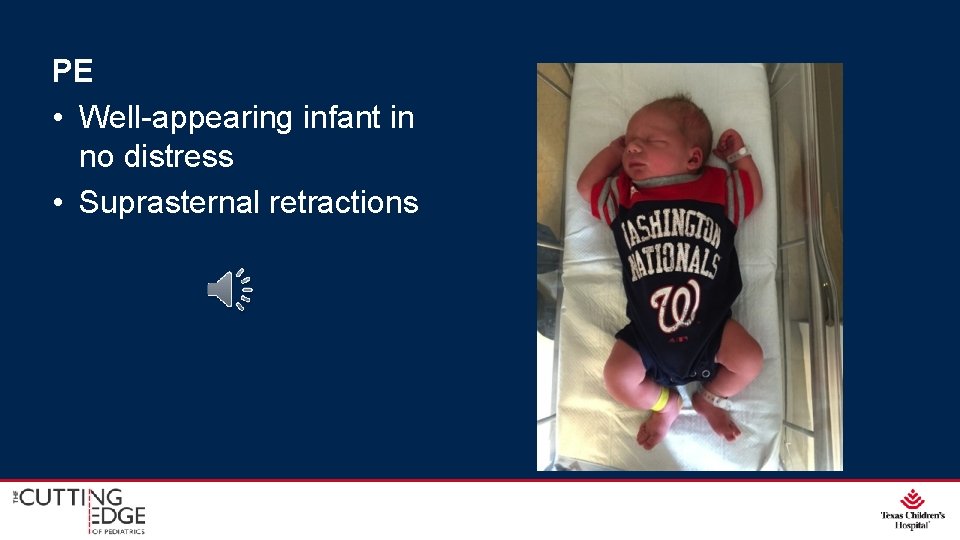
PE • Well-appearing infant in no distress • Suprasternal retractions
Laryngomalacia
• Most common cause of stridor in infants (up to 75%) • Average at presentation: 2 weeks • High-pitched, “fluttery, ” inspiratory stridor worse w/ feeding, agitation, and supine position
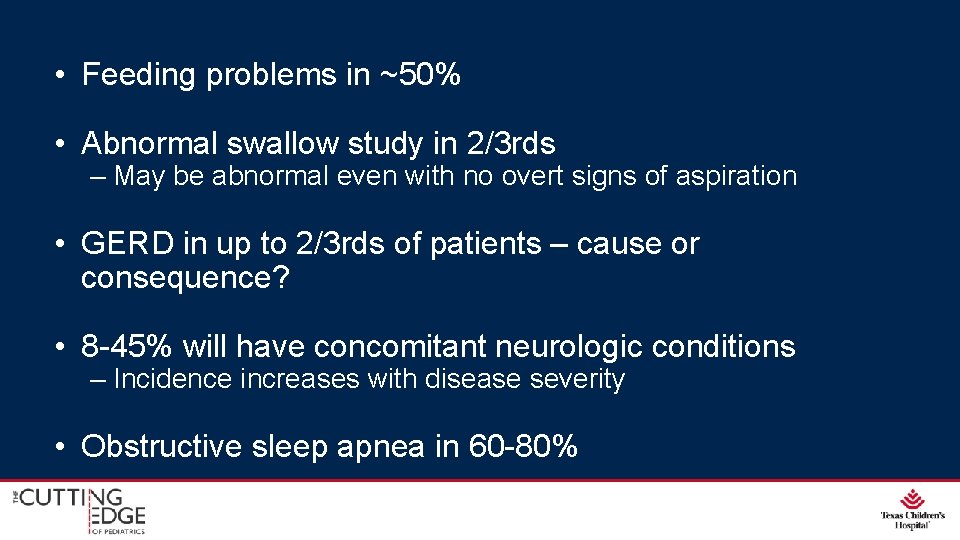
• Feeding problems in ~50% • Abnormal swallow study in 2/3 rds – May be abnormal even with no overt signs of aspiration • GERD in up to 2/3 rds of patients – cause or consequence? • 8 -45% will have concomitant neurologic conditions – Incidence increases with disease severity • Obstructive sleep apnea in 60 -80%
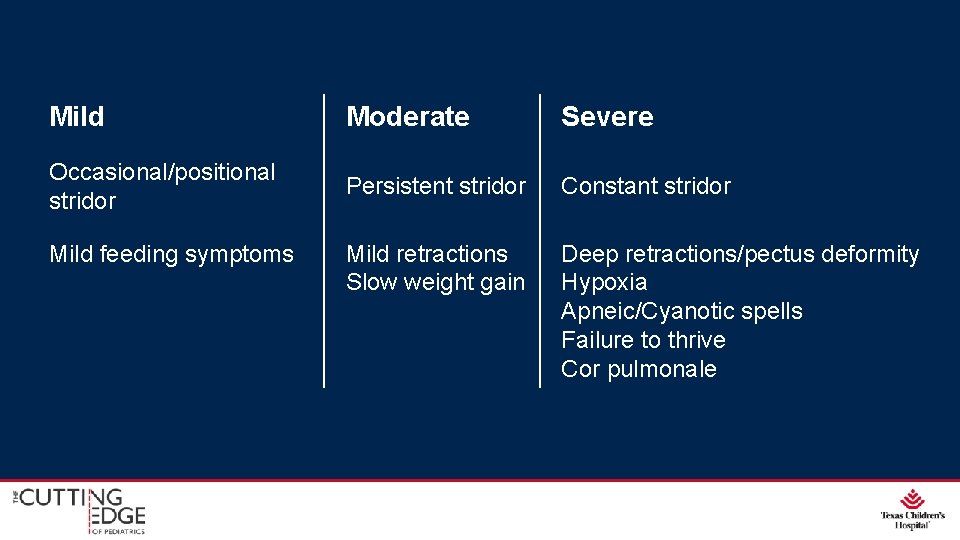
Mild Moderate Severe Occasional/positional stridor Persistent stridor Constant stridor Mild retractions Slow weight gain Deep retractions/pectus deformity Hypoxia Apneic/Cyanotic spells Failure to thrive Cor pulmonale Mild feeding symptoms
Referral to ENT generally appropriate for all kids with suspected laryngomalacia • Up to 50% can have a 2 nd airway lesion Workup • Flexible Fiberoptic Laryngoscopy (FFL) • In-office • No sedation required
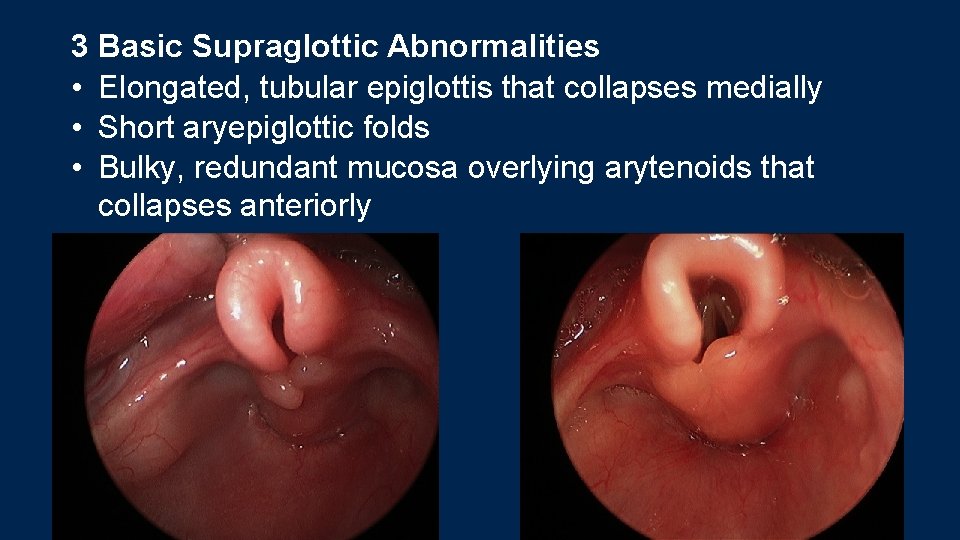
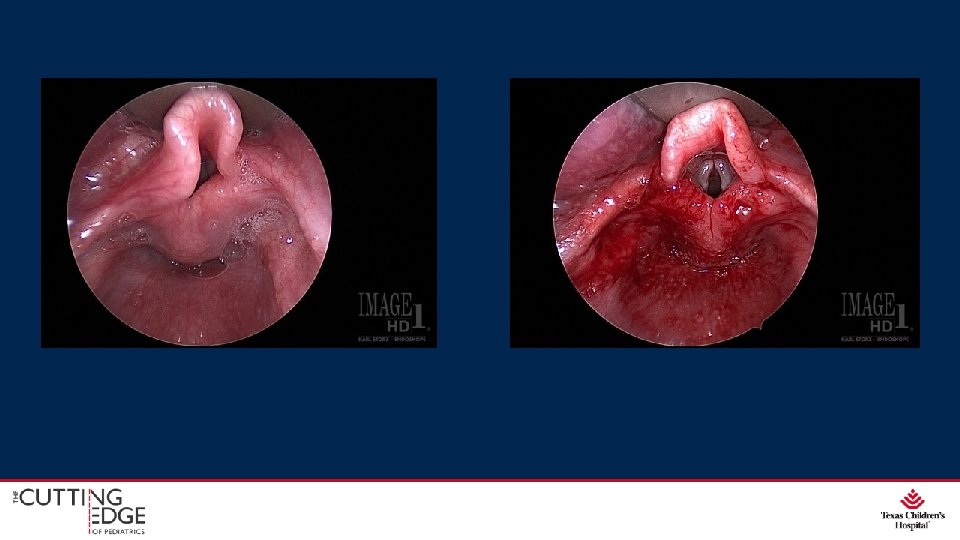
3 Basic Supraglottic Abnormalities • Elongated, tubular epiglottis that collapses medially • Short aryepiglottic folds • Bulky, redundant mucosa overlying arytenoids that collapses anteriorly

Source: www. csurgeries. com
Management • Watchful waiting: resolution by 18 -24 months of age • Anti-reflux medication: H 2 -blocker vs. PPI vs. both • Surgery?
Audience Question What percentage of infants with laryngomalacia have severe enough symptoms that require surgery? A. 5% B. 10% C. 25% D. 50%
Surgical Management Supraglottoplasty • Release aryepiglottic folds • Trim redundant arytenoid tissue • +/- epiglottopexy
Surgical Outcomes • Post-op aspiration in 15 -25% of patients • Supraglottic scarring and stenosis in 4% • Success rate 50 -95% • Children with comorbidities at 7 x risk of failure (especially syndromic) • Tracheostomy reserved for supraglottoplasty failures or children with severe comorbidities


THANK YOU!
- Slides: 35