Diabetic Ketoacidosis DKA Hyperglycemic Hyperosmolar Syndrome HHS Endocrine
Diabetic Ketoacidosis (DKA) & Hyperglycemic Hyperosmolar Syndrome (HHS) Endocrine Emergencies & Management
Learning Goals 1. Understand the physiology of DKA and HHS. 2. Apply the revised Insulin infusion nomogram to patients experiencing DKA and HHS.
DKA Triad: Medical Emergency Diabetic Ketoacidosis (DKA) can occur in both type 1 & 2 diabetes mellitus. It presents with three common characteristics: Ø Hyperglycemia Ø Hyperketonemia Ø Metabolic Acidosis
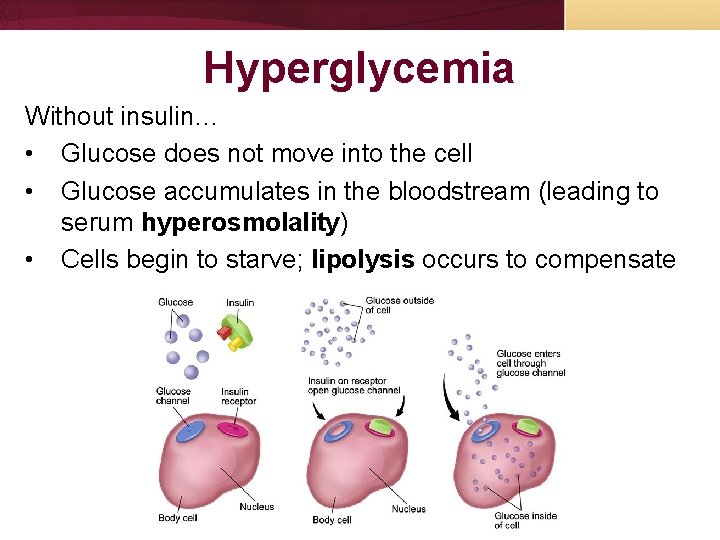
Hyperglycemia Without insulin… • Glucose does not move into the cell • Glucose accumulates in the bloodstream (leading to serum hyperosmolality) • Cells begin to starve; lipolysis occurs to compensate
Hyperosmolality As glucose concentration increases in the bloodstream, the kidneys attempt to excrete the glucose (along with water, potassium, phosphate, and magnesium) Leads to: Polyuria Polydipsia Dehydration Electrolyte imbalances
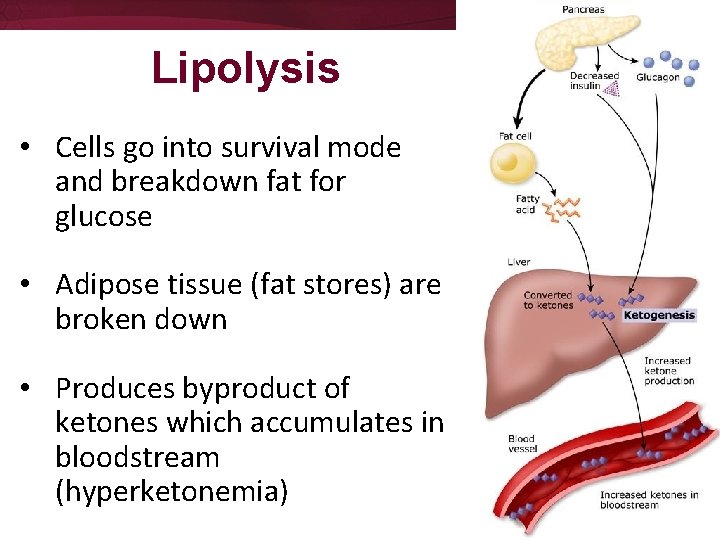
Lipolysis • Cells go into survival mode and breakdown fat for glucose • Adipose tissue (fat stores) are broken down • Produces byproduct of ketones which accumulates in bloodstream (hyperketonemia)
Hyperketonemia • Cells use insulin to break down ketones • Without sufficient insulin, ketones accumulate in bloodstream along with the glucose (exacerbating serum hyperosmolality) • Excessive ketones changes the p. H of blood to become more acidic (metabolic acidosis)
Metabolic Acidosis • Blood p. H < 7. 3 • Anion gap of 10 -12 m. Eq/L • Body tries to compensate: • Hyperventilating (Kussmaul respirations) to decrease CO 2 levels in blood and correct p. H • Excrete ketones through renal system • Mental status changes, lethargy, and hypotension (LATE SIGNS! TREAT AGRESSIVELY!)
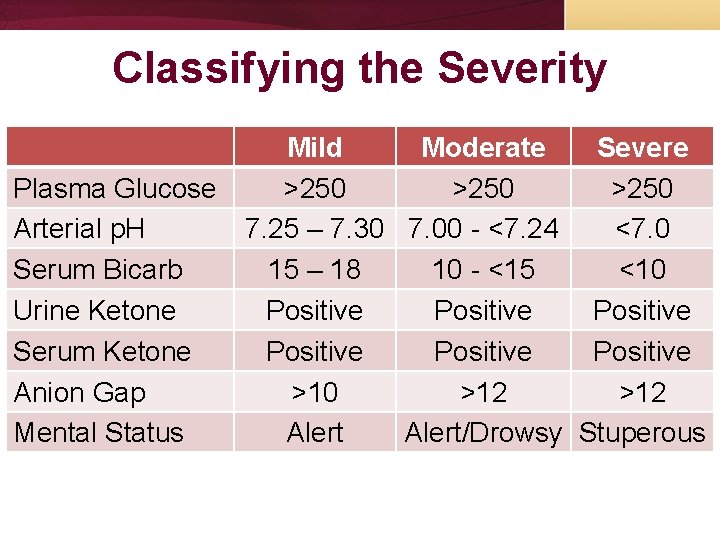
Classifying the Severity Mild Moderate Severe Plasma Glucose >250 Arterial p. H 7. 25 – 7. 30 7. 00 - <7. 24 <7. 0 Serum Bicarb 15 – 18 10 - <15 <10 Urine Ketone Positive Serum Ketone Positive Anion Gap >10 >12 Mental Status Alert/Drowsy Stuperous
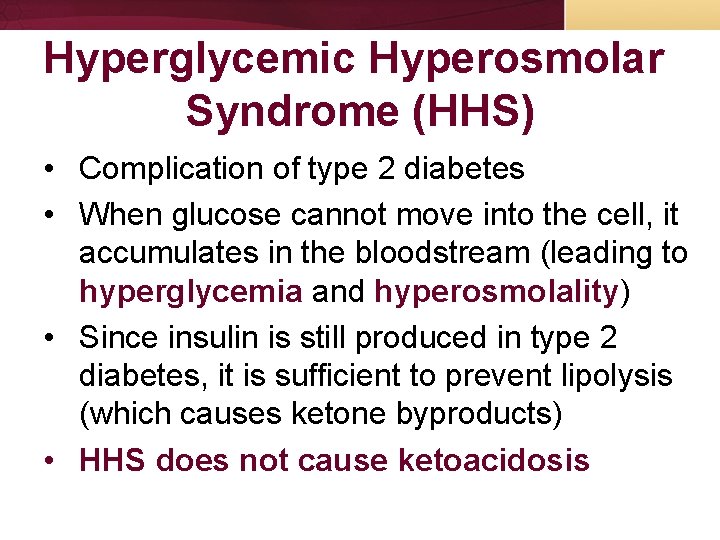
Hyperglycemic Hyperosmolar Syndrome (HHS) • Complication of type 2 diabetes • When glucose cannot move into the cell, it accumulates in the bloodstream (leading to hyperglycemia and hyperosmolality) • Since insulin is still produced in type 2 diabetes, it is sufficient to prevent lipolysis (which causes ketone byproducts) • HHS does not cause ketoacidosis
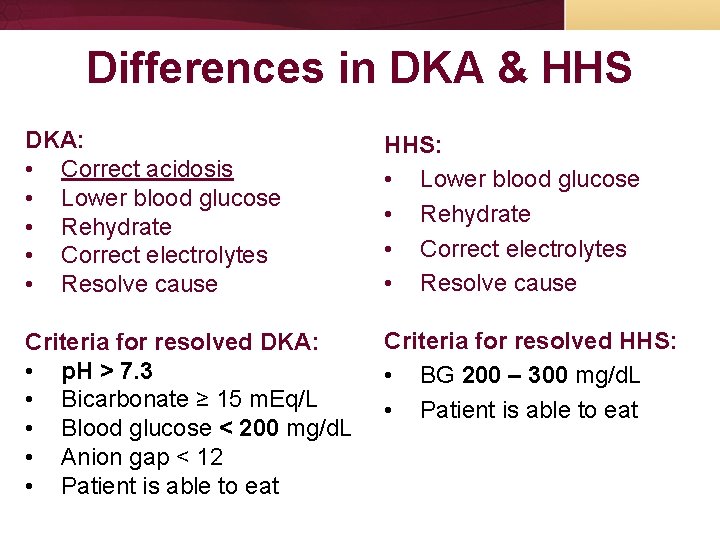
Differences in DKA & HHS DKA: • Correct acidosis • Lower blood glucose • Rehydrate • Correct electrolytes • Resolve cause HHS: • Lower blood glucose • Rehydrate • Correct electrolytes • Resolve cause Criteria for resolved DKA: • p. H > 7. 3 • Bicarbonate ≥ 15 m. Eq/L • Blood glucose < 200 mg/d. L • Anion gap < 12 • Patient is able to eat Criteria for resolved HHS: • BG 200 – 300 mg/d. L • Patient is able to eat
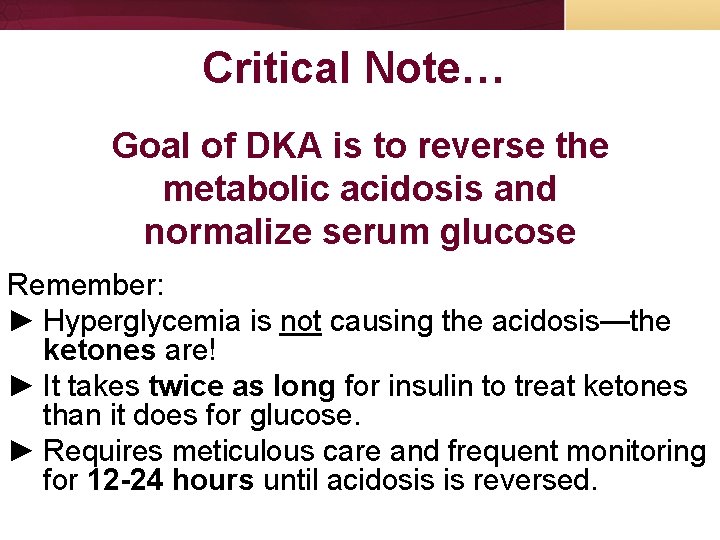
Critical Note… Goal of DKA is to reverse the metabolic acidosis and normalize serum glucose Remember: ► Hyperglycemia is not causing the acidosis—the ketones are! ► It takes twice as long for insulin to treat ketones than it does for glucose. ► Requires meticulous care and frequent monitoring for 12 -24 hours until acidosis is reversed.
Treatment 1) 2) 3) 4) 5) Rehydrate Correct electrolyte deficits & acidosis Restore glucose metabolism Provide glucose when necessary Prevent complications
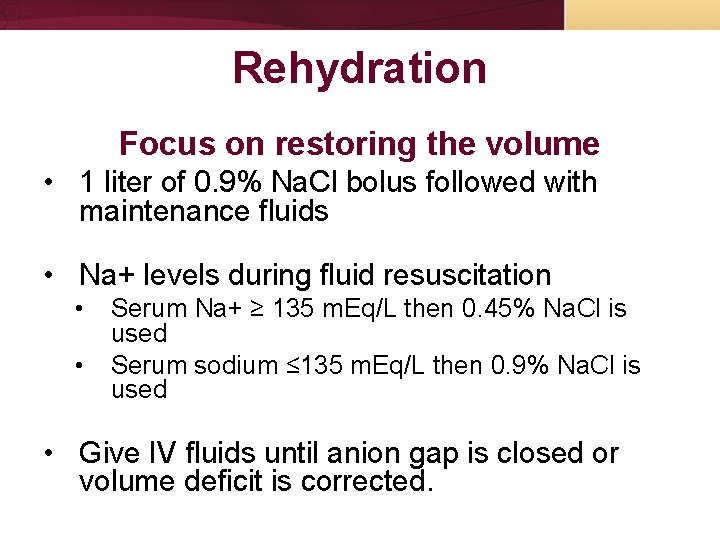
Rehydration Focus on restoring the volume • 1 liter of 0. 9% Na. Cl bolus followed with maintenance fluids • Na+ levels during fluid resuscitation • • Serum Na+ ≥ 135 m. Eq/L then 0. 45% Na. Cl is used Serum sodium ≤ 135 m. Eq/L then 0. 9% Na. Cl is used • Give IV fluids until anion gap is closed or volume deficit is corrected.
Correcting Electrolyte Deficits & Acidosis Correcting labs are crucial to your patient’s outcome • Chem 10, Magnesium & Phosphate are routinely ordered every 2 hours • ABG/VBG will show you if your acidosis is correcting
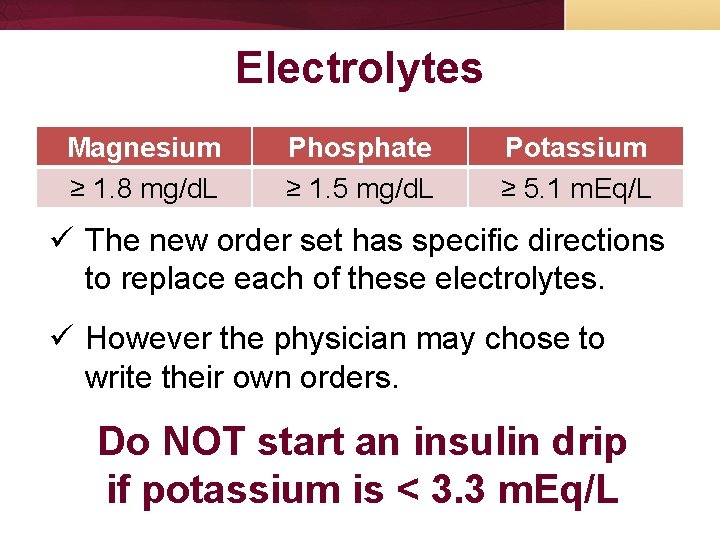
Electrolytes Magnesium ≥ 1. 8 mg/d. L Phosphate ≥ 1. 5 mg/d. L Potassium ≥ 5. 1 m. Eq/L ü The new order set has specific directions to replace each of these electrolytes. ü However the physician may chose to write their own orders. Do NOT start an insulin drip if potassium is < 3. 3 m. Eq/L

ABG / VBG Test p. H p. CO 2 p. O 2 Sat HCO 3 - Normal Ranges 7. 35 – 7. 45 35 – 45 mm. Hg 80 – 100 mm. Hg 95 – 100% 22 – 26 mm. Hg p. H CO 2 HCO 3 Respiratory Acidosis < 7. 35 > 45 mm. Hg Normal Metabolic Acidosis < 7. 35 Normal < 22 m. Eq/L Respiratory Alkalosis > 7. 45 < 35 mm. Hg Normal Metabolic Alkalosis > 7. 45 Normal > 26 m. Eq/L
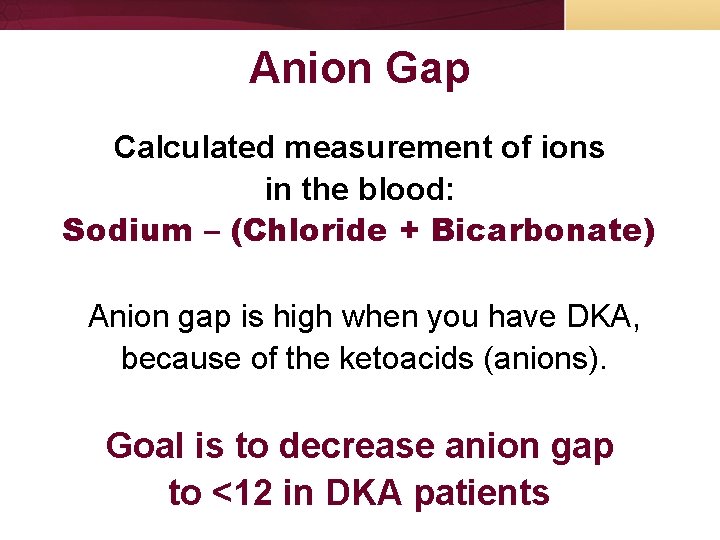
Anion Gap Calculated measurement of ions in the blood: Sodium – (Chloride + Bicarbonate) Anion gap is high when you have DKA, because of the ketoacids (anions). Goal is to decrease anion gap to <12 in DKA patients
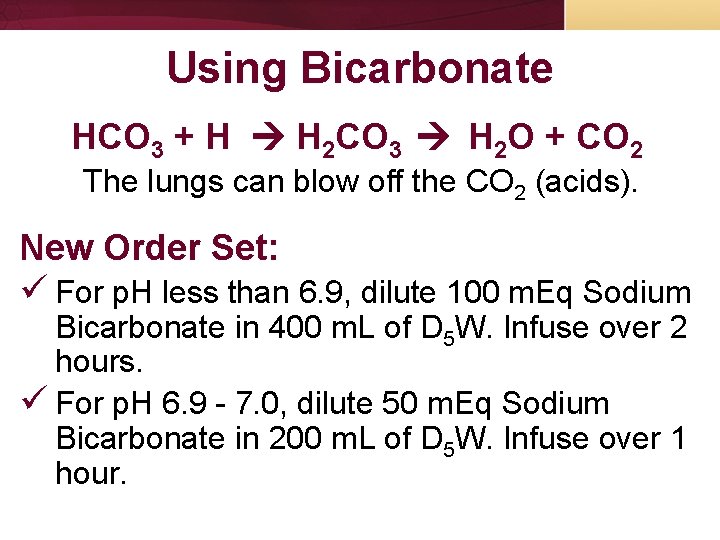
Using Bicarbonate HCO 3 + H H 2 CO 3 H 2 O + CO 2 The lungs can blow off the CO 2 (acids). New Order Set: ü For p. H less than 6. 9, dilute 100 m. Eq Sodium Bicarbonate in 400 m. L of D 5 W. Infuse over 2 hours. ü For p. H 6. 9 - 7. 0, dilute 50 m. Eq Sodium Bicarbonate in 200 m. L of D 5 W. Infuse over 1 hour.
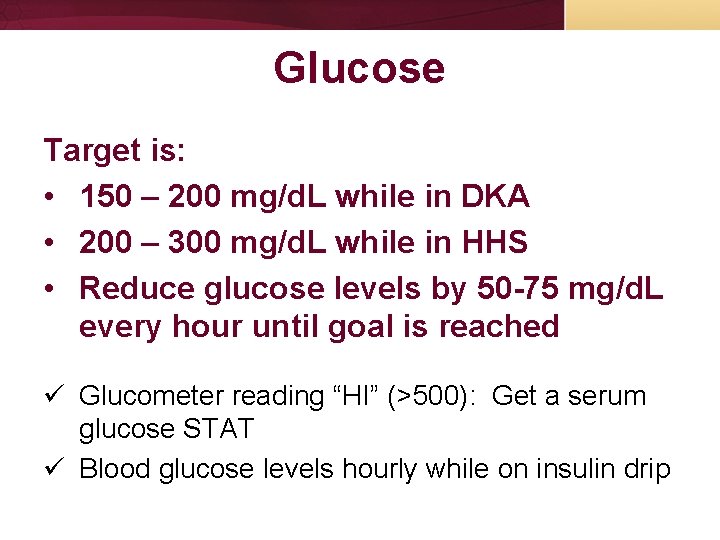
Glucose Target is: • 150 – 200 mg/d. L while in DKA • 200 – 300 mg/d. L while in HHS • Reduce glucose levels by 50 -75 mg/d. L every hour until goal is reached ü Glucometer reading “HI” (>500): Get a serum glucose STAT ü Blood glucose levels hourly while on insulin drip
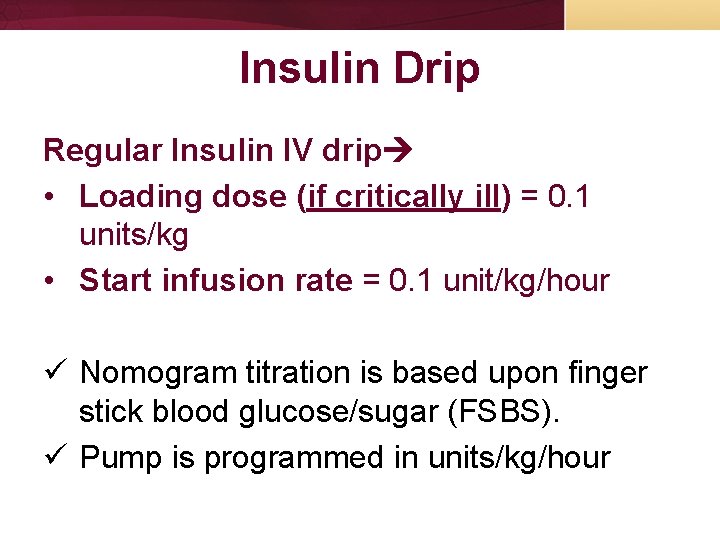
Insulin Drip Regular Insulin IV drip • Loading dose (if critically ill) = 0. 1 units/kg • Start infusion rate = 0. 1 unit/kg/hour ü Nomogram titration is based upon finger stick blood glucose/sugar (FSBS). ü Pump is programmed in units/kg/hour
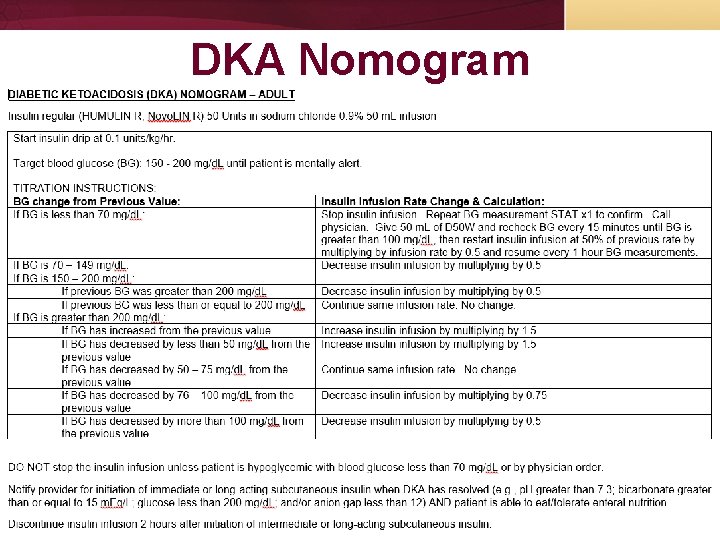
DKA Nomogram
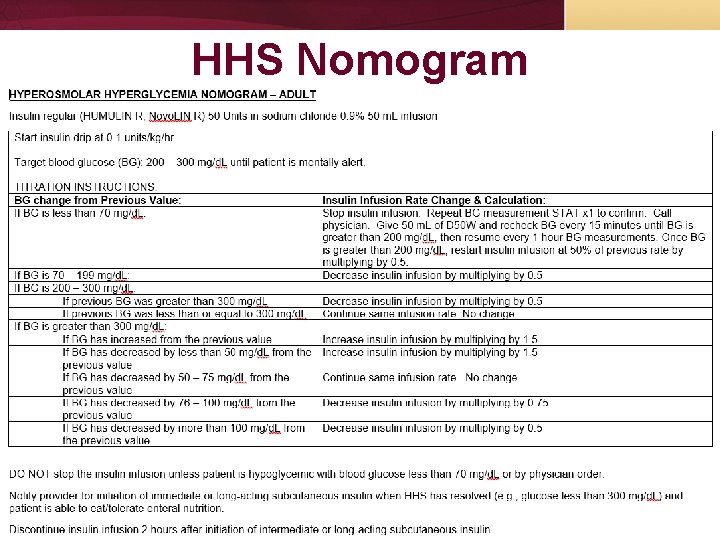
HHS Nomogram

Insulin Management Do NOT stop insulin infusion unless you have hypoglycemia (< 70 mg/d. L) or DKA is resolved Criteria for resolved DKA: • Venous p. H > 7. 3 • Bicarbonate ≥ 15 m. Eq/L • Blood glucose < 200 mg/d. L • Anion gap < 12 • Patient is able to eat
Converting Insulin IV to Sub. Q Call physician to initiate subcutaneous insulin AND Wait to discontinue your insulin IV drip until 2 hours after subcutaneous insulin is initiated
Glucose Administration Ø Use dextrose-based IV fluids once target glucose has been reached Ø When blood glucose reaches 200 mg/d. L, change IV fluids to D 51/2 NS per MD order Ø Remember…Glucose levels correct faster than ketonemia. Need to correct the ketones that are causing the acidosis!
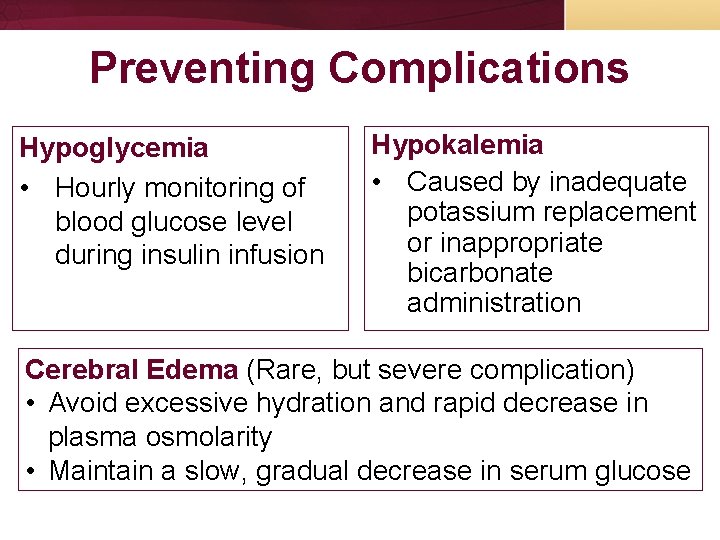
Preventing Complications Hypoglycemia • Hourly monitoring of blood glucose level during insulin infusion Hypokalemia • Caused by inadequate potassium replacement or inappropriate bicarbonate administration Cerebral Edema (Rare, but severe complication) • Avoid excessive hydration and rapid decrease in plasma osmolarity • Maintain a slow, gradual decrease in serum glucose
- Slides: 27