DIABETES MELLITUS AND DIABETIC KETOACIDOSIS DKA DM diagnosis
DIABETES MELLITUS AND DIABETIC KETOACIDOSIS (DKA)
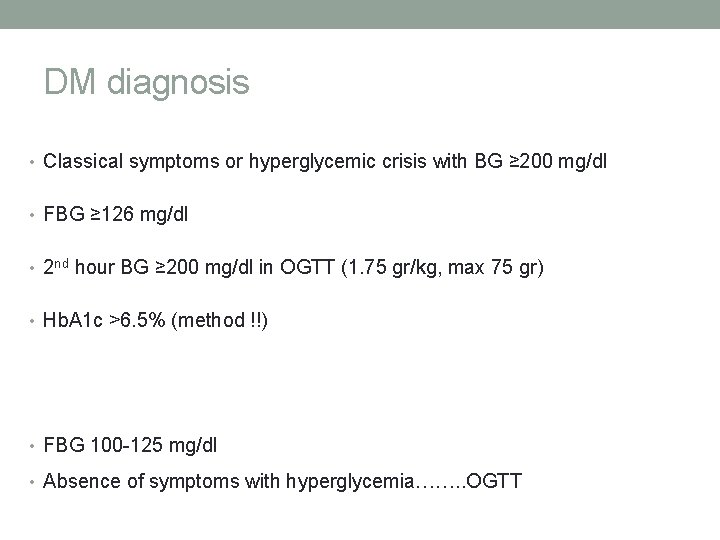
DM diagnosis • Classical symptoms or hyperglycemic crisis with BG ≥ 200 mg/dl • FBG ≥ 126 mg/dl • 2 nd hour BG ≥ 200 mg/dl in OGTT (1. 75 gr/kg, max 75 gr) • Hb. A 1 c >6. 5% (method !!) • FBG 100 -125 mg/dl • Absence of symptoms with hyperglycemia……. . OGTT

OGTT • FBG <100 mg/dl Normal • FBG 100 -125 mg/dl IFG • FBG ≥ 126 mg/dl DM • 2 nd hour BG <140 mg/dl Normal 140 -200 mg/dl IGT ≥ 200 mg/dl DM
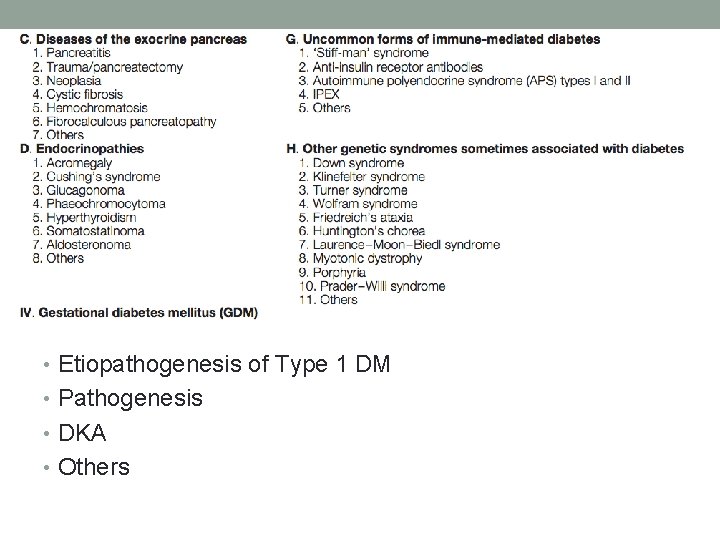
• Etiopathogenesis of Type 1 DM • Pathogenesis • DKA • Others
Etiopathogenesis of T 1 DM • Type I DM is a syndrome characterized by hyperglycemia and ketosis due to disturbed metabolism of carbohydrate, fat and protein resulting from insulinopenia • Type I DM is an autoimmune disorder triggered by some environmental factors develops in genetically susceptible individuals as a result of destruction of pancreatic b-cells
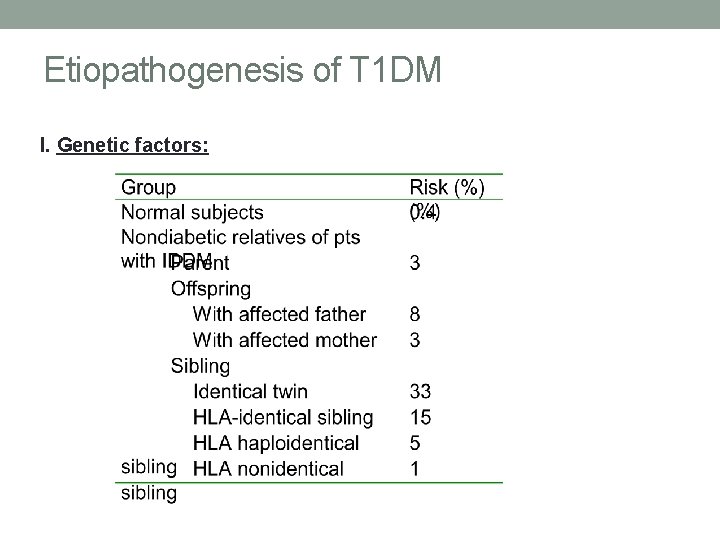
Etiopathogenesis of T 1 DM I. Genetic factors:
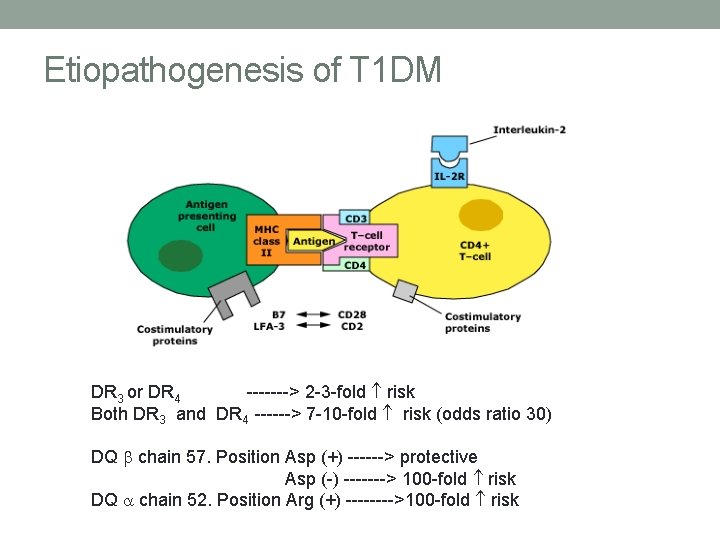
Etiopathogenesis of T 1 DM DR 3 or DR 4 -------> 2 -3 -fold risk Both DR 3 and DR 4 ------> 7 -10 -fold risk (odds ratio 30) DQ chain 57. Position Asp (+) ------> protective Asp (-) -------> 100 -fold risk DQ a chain 52. Position Arg (+) ---->100 -fold risk
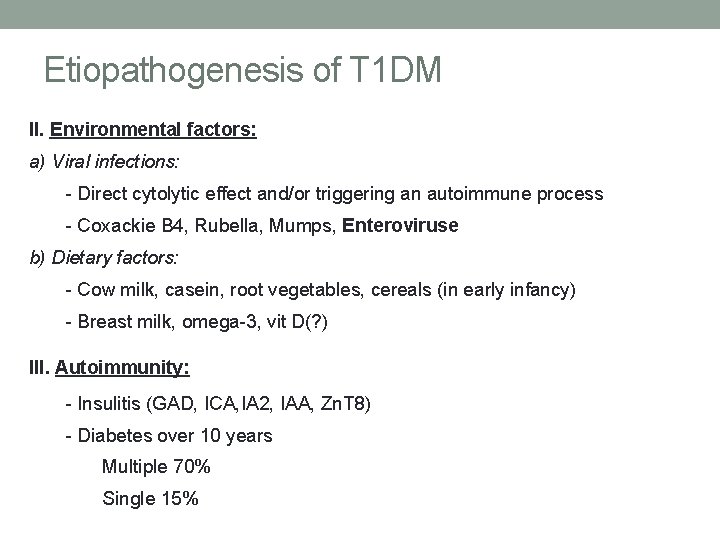
Etiopathogenesis of T 1 DM II. Environmental factors: a) Viral infections: - Direct cytolytic effect and/or triggering an autoimmune process - Coxackie B 4, Rubella, Mumps, Enteroviruse b) Dietary factors: - Cow milk, casein, root vegetables, cereals (in early infancy) - Breast milk, omega-3, vit D(? ) III. Autoimmunity: - Insulitis (GAD, ICA, IA 2, IAA, Zn. T 8) - Diabetes over 10 years Multiple 70% Single 15%
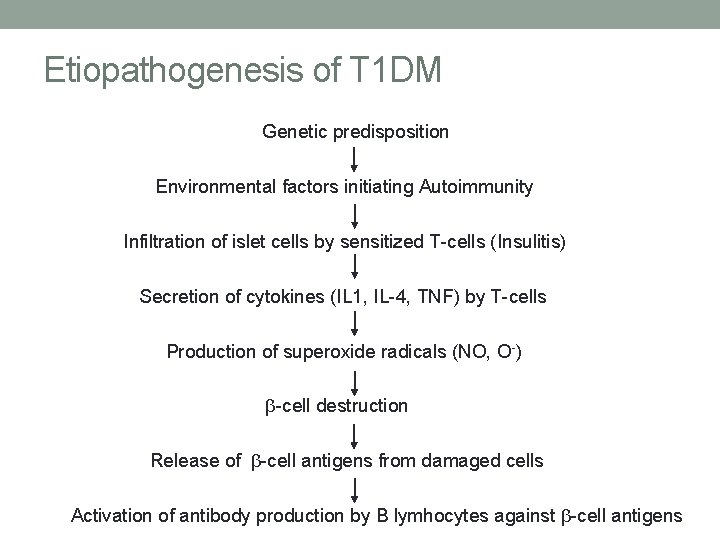
Etiopathogenesis of T 1 DM Genetic predisposition Environmental factors initiating Autoimmunity Infiltration of islet cells by sensitized T-cells (Insulitis) Secretion of cytokines (IL 1, IL-4, TNF) by T-cells Production of superoxide radicals (NO, O-) -cell destruction Release of -cell antigens from damaged cells Activation of antibody production by B lymhocytes against -cell antigens
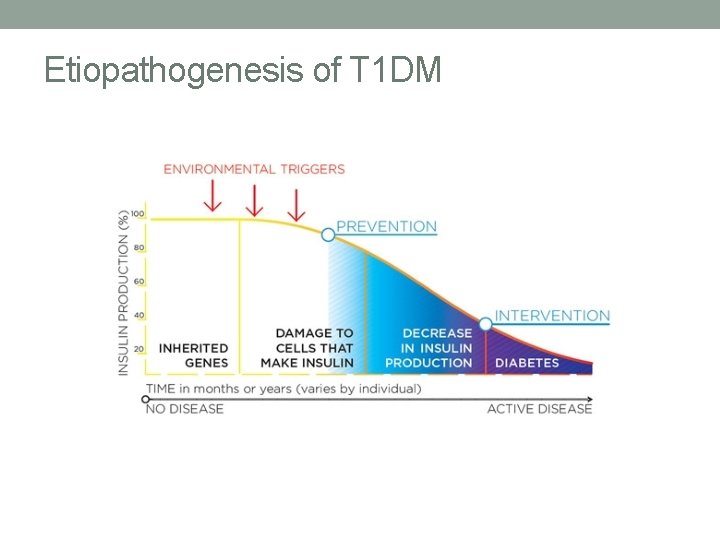
Etiopathogenesis of T 1 DM
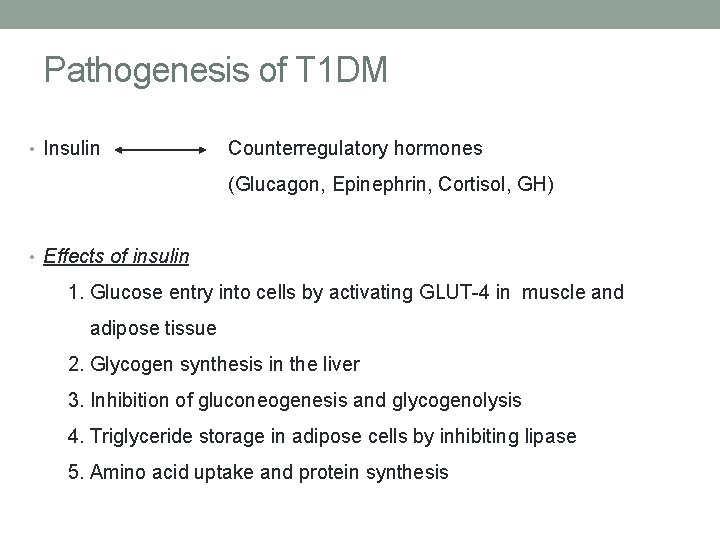
Pathogenesis of T 1 DM • Insulin Counterregulatory hormones (Glucagon, Epinephrin, Cortisol, GH) • Effects of insulin 1. Glucose entry into cells by activating GLUT-4 in muscle and adipose tissue 2. Glycogen synthesis in the liver 3. Inhibition of gluconeogenesis and glycogenolysis 4. Triglyceride storage in adipose cells by inhibiting lipase 5. Amino acid uptake and protein synthesis
Symptoms • Non-emergency: • Recent onset of enuresis • Vaginal candidiasis (prepubertal girls) • Chronic weight loss or failure to gain weight despite of polyphagia • Recurrent skin infections • Emergency: • Polyuria, polydipsia (moderate to severe dehydration) • Generalized weakness • Nausea, abdominal pain, vomiting (AGE, acute abdomen!!) • Heavy breathing, kussmaul respiration, acetone odeur • Dowsiness, coma

DIABETIC KETOACIDOSIS (DKA)
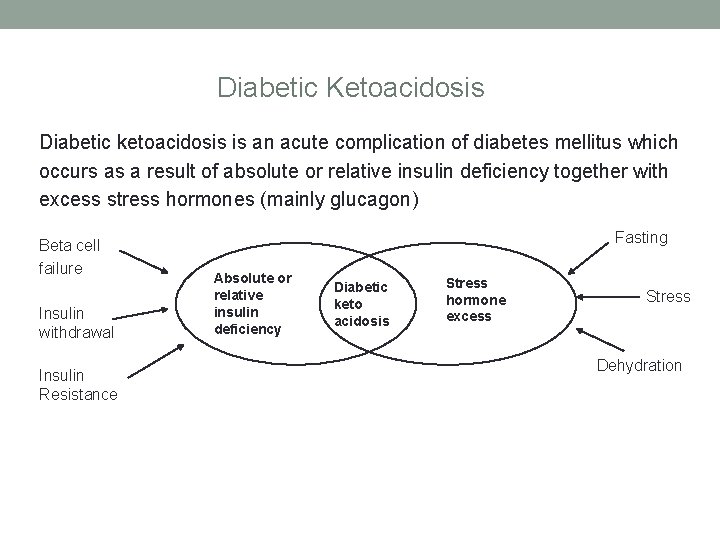
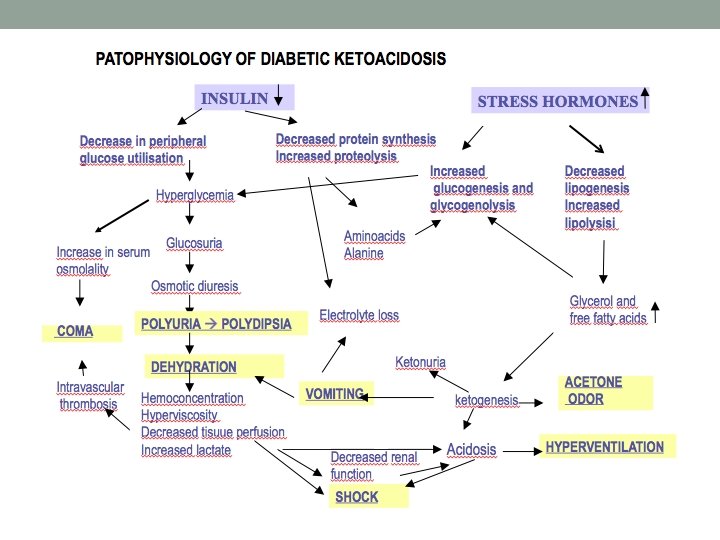
Diabetic Ketoacidosis Diabetic ketoacidosis is an acute complication of diabetes mellitus which occurs as a result of absolute or relative insulin deficiency together with excess stress hormones (mainly glucagon) Beta cell failure Insulin withdrawal Insulin Resistance Fasting Absolute or relative insulin deficiency Diabetic keto acidosis Stress hormone excess Stress Dehydration

DKA 1. Hyperglycemia BG > 200 mg/dl 2. Acidosis venous p. H <7. 3 HCO 3< 15 m. Eq/L 3. Ketonemia and or ketonuria in addition to classical signs and symptoms of diabetes Degree of acidosis: Mild DKA: Venous p. H: 7. 2 -7. 3, HCO 3: 10 -15 Moderate DKA: Venous p. H: 7. 1 -7. 2, HCO 3: 5 -10 Severe DKA: Venous p. H: <7. 1, HCO 3: < 5
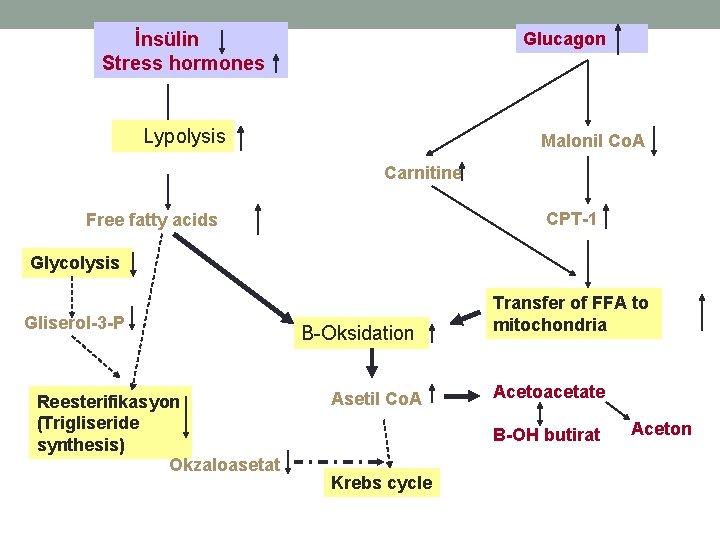
İnsülin Stress hormones Glucagon Lypolysis Malonil Co. A Carnitine CPT-1 Free fatty acids Glycolysis Gliserol-3 -P Reesterifikasyon (Trigliseride synthesis) Okzaloasetat B-Oksidation Asetil Co. A Transfer of FFA to mitochondria Acetoacetate B-OH butirat Krebs cycle Aceton

Pathophysiology of DKA I. Mechanism of acidosis: 1 - Ketoacids: -OH butyric acid, acetoacetic acid, aceton Triglycerides FFA 3 Free fatty acids + 3 H+ 4 ketone bodies + 3 H+ Normally, ratio of -OH butyric acid /acetoacetic acid is: 3: 1 In DKA: this ratio is > 8: 1 2 - Lactic acid: Hypovolemia Poor tissue perfusion Lactic acidosis Low erythrocyte 2, 3 di. P glycerate level Poor tissue oxygenation

Pathophysiology of DKA II. Fluid and electrolyte status: a- Fluid: Serum glucose >170 mg/dl (renal threshold) Glycosuria Osmotic diuresis (10 ml of water for each gr of glucose) Ongoing urinary and other fluid losses >intake= Dehydration b- Sodium: Total body Na is decreased in DKA due to osmotic diuresis and vomiting. Approximate loss is 6 -12 m. Eq/kg (Na low / normal) Pseudohyponatremia Corrected (real) serum Na: Na + 1. 6 x (glucose-100/100)

Pathophysiology of DKA II. Fluid and electrolyte status: a- Potassium Total body K is also depleted in DKA due to: - Acidosis (K moves out of the cell and excreted) - Dehydration (K moves out of muscle cells with. H 2 O - Intracellular P loss (to maintain electrical neutrality) - Vomiting -Approximate loss is 4 -6 m. Eq/kg (K low / normal / high) Serum K invariably drops down after the initiation of insulin treatment
Precipitating factors in DKA In known diabetics: A. Noncompliance with insulin injections (frequent in adolescents) B. Increased stress hormones: -Infections -Anesthesia, surgery -Trauma, burns -Emotional distresses Incidence of DKA episodes in known diabetics can be decreased by improvement in diabetic education
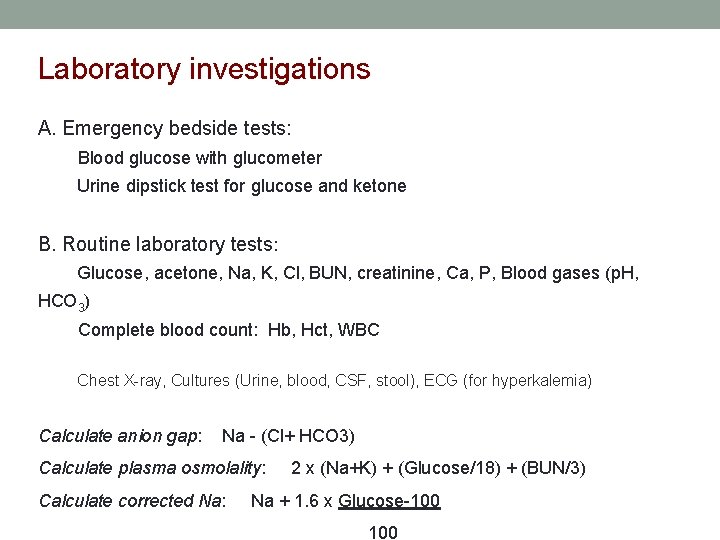
Laboratory investigations A. Emergency bedside tests: Blood glucose with glucometer Urine dipstick test for glucose and ketone B. Routine laboratory tests: Glucose, acetone, Na, K, Cl, BUN, creatinine, Ca, P, Blood gases (p. H, HCO 3) Complete blood count: Hb, Hct, WBC Chest X-ray, Cultures (Urine, blood, CSF, stool), ECG (for hyperkalemia) Calculate anion gap: Na - (Cl+ HCO 3) Calculate plasma osmolality: Calculate corrected Na: 2 x (Na+K) + (Glucose/18) + (BUN/3) Na + 1. 6 x Glucose-100
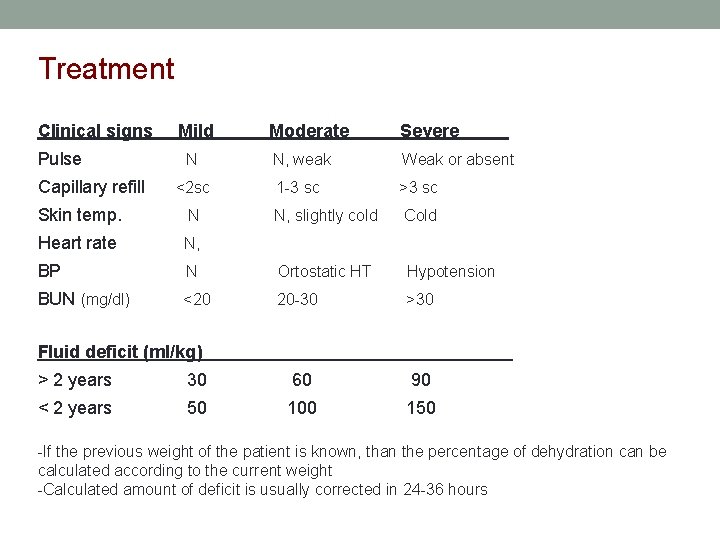
Treatment Clinical signs Pulse Capillary refill Mild Moderate Severe N N, weak Weak or absent <2 sc 1 -3 sc >3 sc N, slightly cold Cold Skin temp. N Heart rate N, BP N Ortostatic HT Hypotension BUN (mg/dl) <20 20 -30 >30 Fluid deficit (ml/kg) > 2 years 30 60 90 < 2 years 50 100 150 -If the previous weight of the patient is known, than the percentage of dehydration can be calculated according to the current weight -Calculated amount of deficit is usually corrected in 24 -36 hours
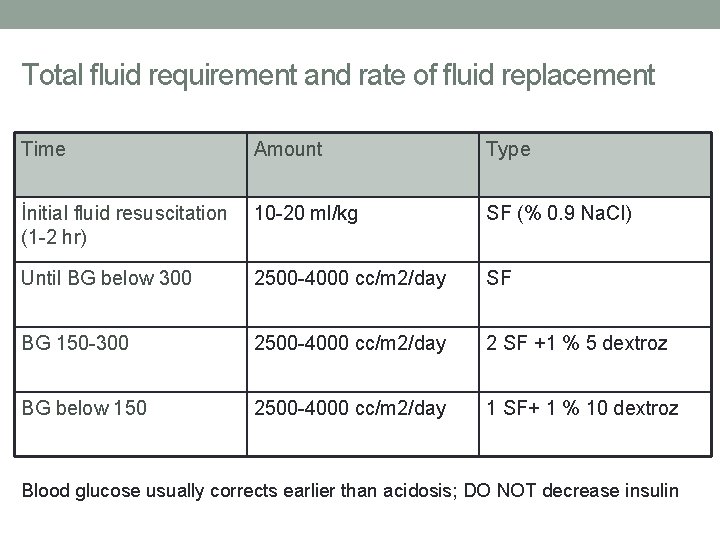
Total fluid requirement and rate of fluid replacement Time Amount Type İnitial fluid resuscitation (1 -2 hr) 10 -20 ml/kg SF (% 0. 9 Na. Cl) Until BG below 300 2500 -4000 cc/m 2/day SF BG 150 -300 2500 -4000 cc/m 2/day 2 SF +1 % 5 dextroz BG below 150 2500 -4000 cc/m 2/day 1 SF+ 1 % 10 dextroz Blood glucose usually corrects earlier than acidosis; DO NOT decrease insulin
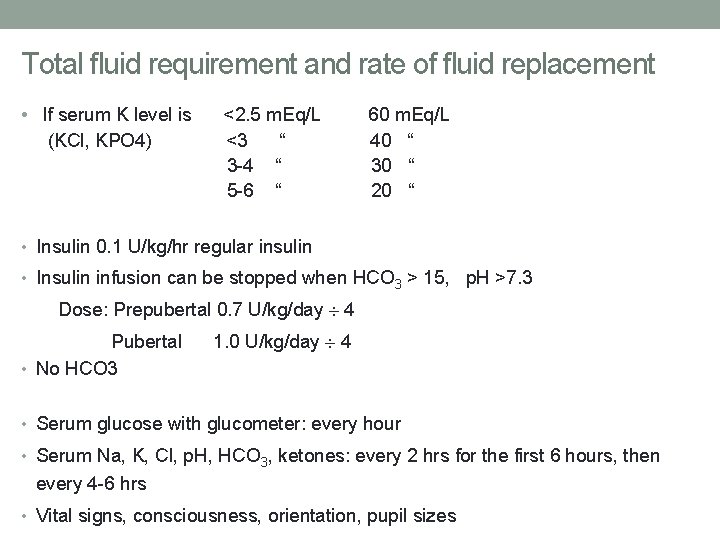
Total fluid requirement and rate of fluid replacement • If serum K level is (KCl, KPO 4) <2. 5 m. Eq/L <3 “ 3 -4 “ 5 -6 “ 60 m. Eq/L 40 “ 30 “ 20 “ • Insulin 0. 1 U/kg/hr regular insulin • Insulin infusion can be stopped when HCO 3 > 15, p. H >7. 3 Dose: Prepubertal 0. 7 U/kg/day ¸ 4 Pubertal • No HCO 3 1. 0 U/kg/day ¸ 4 • Serum glucose with glucometer: every hour • Serum Na, K, Cl, p. H, HCO 3, ketones: every 2 hrs for the first 6 hours, then every 4 -6 hrs • Vital signs, consciousness, orientation, pupil sizes

Complications of DKA I. Cerebral edema: Etiology: Accumulation of idiogenic osmoles Overhydration Risk factors: New onset DM Overhydration (>4000 cc/m 2/d) Negative Na trend and rapid fall in BG Symptoms: Headache, agitation, dysorientation Vomiting, bradicardia, hypertansion, apnea Ophtalmoplegia, pupil asymmetry, papilledema (late) Absent of light reflex, seizure Treatment: Elevate head IV mannitol 1 -2 gr/kg/dose or 3%Na. Cl Decrease IV fluid and intubate-hyperventilate II. Hypoglycemia:
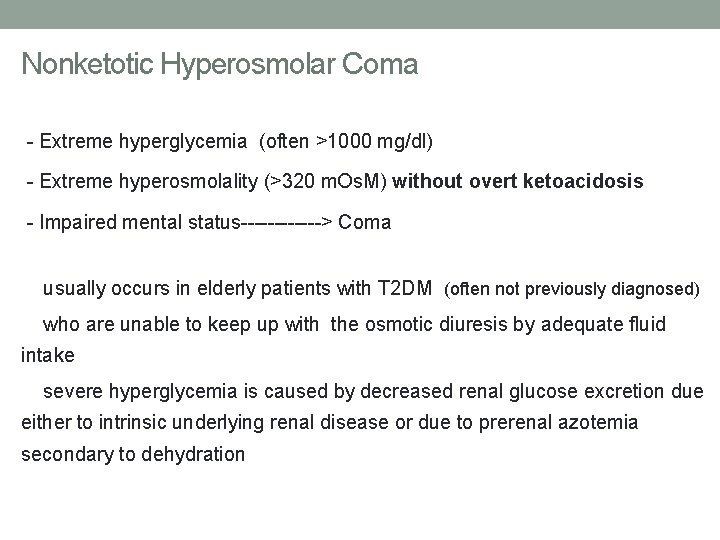
Nonketotic Hyperosmolar Coma - Extreme hyperglycemia (often >1000 mg/dl) - Extreme hyperosmolality (>320 m. Os. M) without overt ketoacidosis - Impaired mental status------> Coma usually occurs in elderly patients with T 2 DM (often not previously diagnosed) who are unable to keep up with the osmotic diuresis by adequate fluid intake severe hyperglycemia is caused by decreased renal glucose excretion due either to intrinsic underlying renal disease or due to prerenal azotemia secondary to dehydration
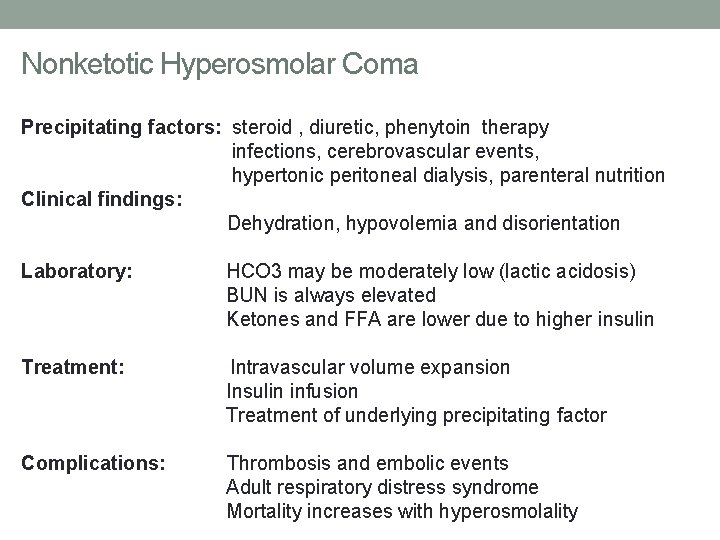
Nonketotic Hyperosmolar Coma Precipitating factors: steroid , diuretic, phenytoin therapy infections, cerebrovascular events, hypertonic peritoneal dialysis, parenteral nutrition Clinical findings: Dehydration, hypovolemia and disorientation Laboratory: HCO 3 may be moderately low (lactic acidosis) BUN is always elevated Ketones and FFA are lower due to higher insulin Treatment: Intravascular volume expansion Insulin infusion Treatment of underlying precipitating factor Complications: Thrombosis and embolic events Adult respiratory distress syndrome Mortality increases with hyperosmolality
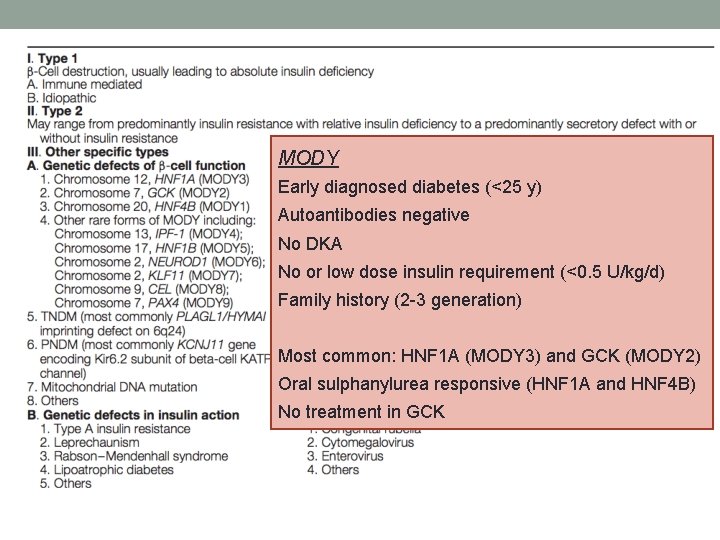
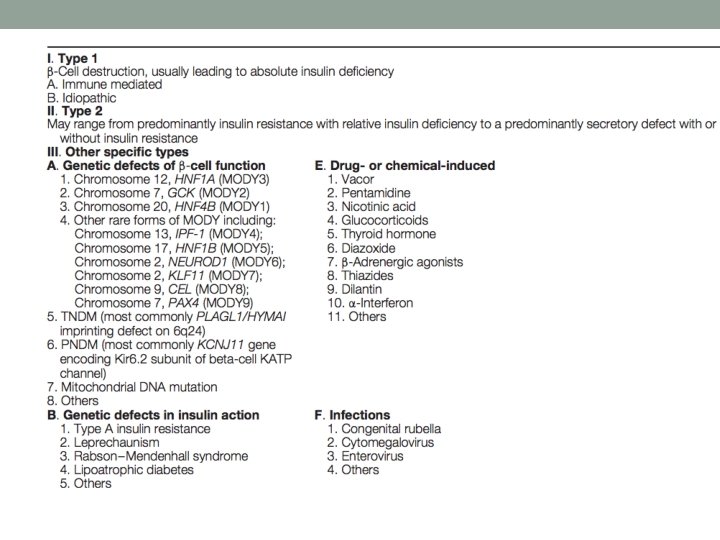
MODY Early diagnosed diabetes (<25 y) Autoantibodies negative No DKA No or low dose insulin requirement (<0. 5 U/kg/d) Family history (2 -3 generation) Most common: HNF 1 A (MODY 3) and GCK (MODY 2) Oral sulphanylurea responsive (HNF 1 A and HNF 4 B) No treatment in GCK
- Slides: 34