Diabetes In Canada Evaluation The DICE Study Impact
Diabetes In Canada Evaluation (The DICE Study): Impact on Family Practice Stewart B. Harris MD MPH FCFP FACPM Associate Professor Centre for Studies in Family Medicine Ian Mc. Whinney Chair of Family Medicine Studies Schulich School of Medicine and Dentistry University of Western Ontario London, Ontario
Overview • • • What is diabetes? Epidemiology of diabetes Revisiting the CDA guidelines How are FPs doing? Review of the DICE study findings
What Is Diabetes? Type 1 diabetes (5 -10%) • Body’s own immune system attacks the cells in the pancreas that produce insulin Type 2 diabetes (90 - 95%) The pancreas does not produce enough insulin and/or the bodies’ tissues do not respond properly to the actions of insulin • Caused by both genetic and environmental factors Gestational diabetes • Diabetes with first onset or recognition during pregnancy • Puts women at higher risk for type 2 DM later in life
What Diabetes is NOT • Diabetes is NOT “a touch of sugar” • It is a serious chronic disease that can lead to complications such as heart attack, stroke, blindness, amputation, kidney disease, sexual dysfunction, and nerve damage
The Complications of Diabetes
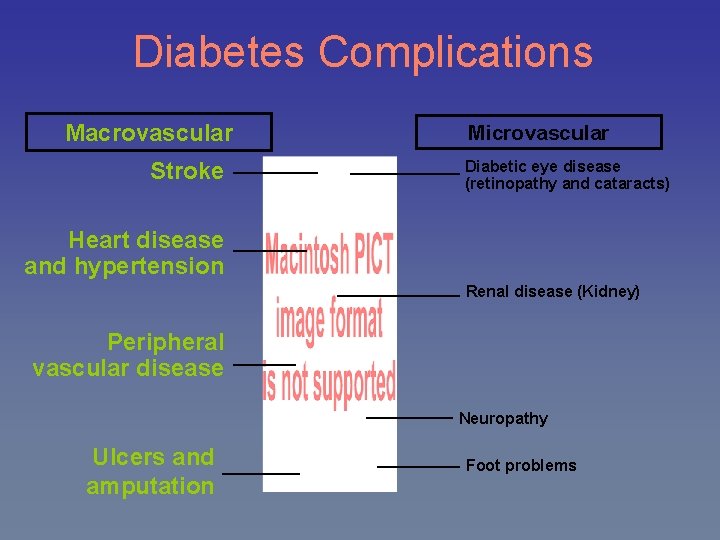
Diabetes Complications Macrovascular Stroke Microvascular Diabetic eye disease (retinopathy and cataracts) Heart disease and hypertension Renal disease (Kidney) Peripheral vascular disease Neuropathy Ulcers and amputation Foot problems
Diabetes = CVD Up to 80% of adults with diabetes will die of cardiovascular disease. Adapted from Barrett-Connor 2001.
Cardiovascular Disease • Diabetes is a major risk factor for heart disease and stroke • Acute MI (heart attack) occurs 15 to 20 years earlier in people with diabetes • 80% of people with diabetes will die from cardiovascular disease Diabetes in Ontario, An ICES Practice Atlas, 2002
Amputation • Diabetes is the leading cause of nontraumatic amputation • Increases the risk of amputation by 20 fold Diabetes in Ontario, An ICES Practice Atlas, 2002
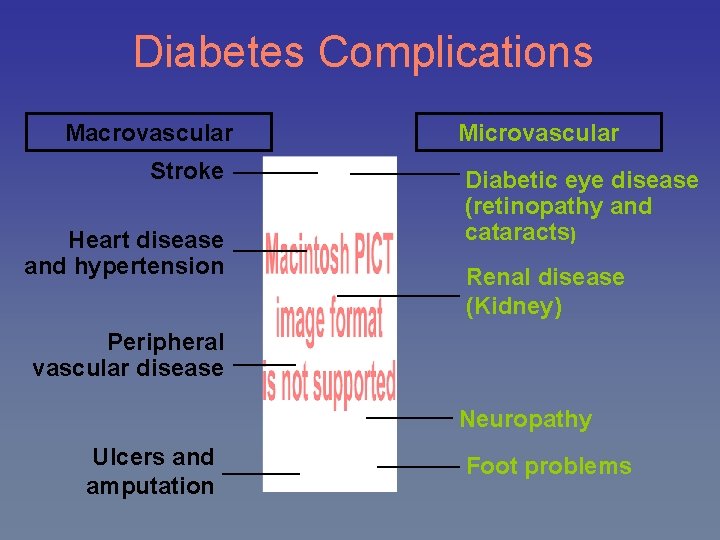
Diabetes Complications Macrovascular Stroke Heart disease and hypertension Microvascular Diabetic eye disease (retinopathy and cataracts) Renal disease (Kidney) Peripheral vascular disease Neuropathy Ulcers and amputation Foot problems
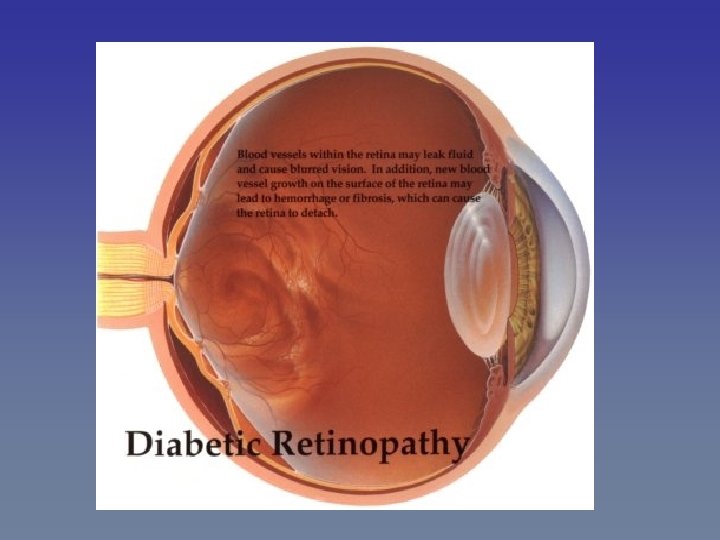
Retinopathy • Diabetes is the leading cause of adult-onset blindness • Prevalence of diabetic retinopathy: – 70% in people with type 1 diabetes – 40% with person with type 2 diabetes • Increased risk of macular edema, cataracts, glaucoma Diabetes in Ontario, An ICES Practice Atlas, 2002
Nephropathy • Diabetes is the leading cause of kidney failure (end-stage renal disease) • Increases the risk of developing ESRD by up to 13 -fold • Potent predictor of CVD Parchman ML, et al Medical Care 2002; 40(2): 137 -144
Diabetes Complications: Other Problems • • Skin infections Digestive problems Thyroid problems (hypothyroidism) Sexual dysfunction in men (50 -70% of all male diabetes patients suffer from erectile dysfunction) • Urinary tract and vaginal infections • Carpal tunnel syndrome CDA, 2003 www. diabetes. ca
The Scope of the Problem World-wide and Canada
The Worldwide Epidemic: Diabetes Trends www. who. int www. idf Zimmet P. et al Nature: 414, 13 Dec 2001
Why the Epidemic? • Physical Inactivity – 60% to 85% of adults are not active enough to maintain their health • Diet – Calorie dense; high fat • Aging population • Urbanization – Shift from an agricultural to an urban lifestyle means a decrease in physical activity
The Canadian Epidemic • The Canadian population is aging – Boomer and Echo generations • Immigration and ethnicity – High percentage (77%) of Canadian immigrants are from ethnic groups that are at high risk for the development of diabetes • Latino, Hispanic • South East Asian • African - Growth in Aboriginal populations
The Canadian Epidemic: Age Distribution of Canadians with Diabetes in 2000 & 2016 * Source: Statistics Canada
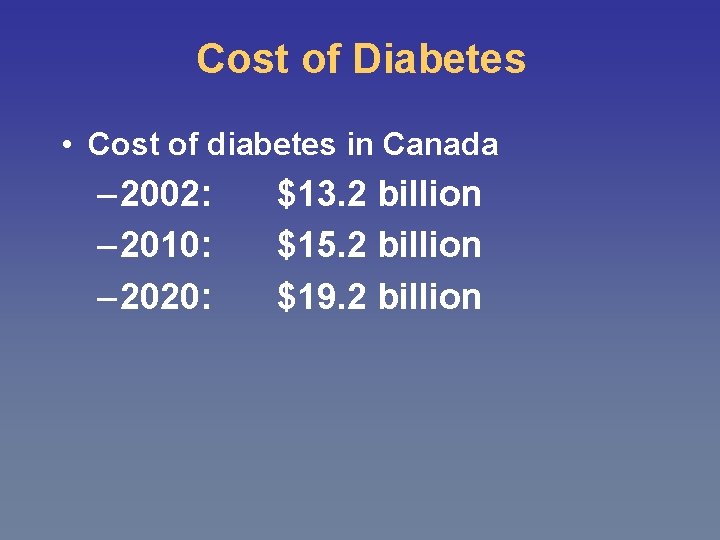
Cost of Diabetes • Cost of diabetes in Canada – 2002: – 2010: – 2020: $13. 2 billion $15. 2 billion $19. 2 billion
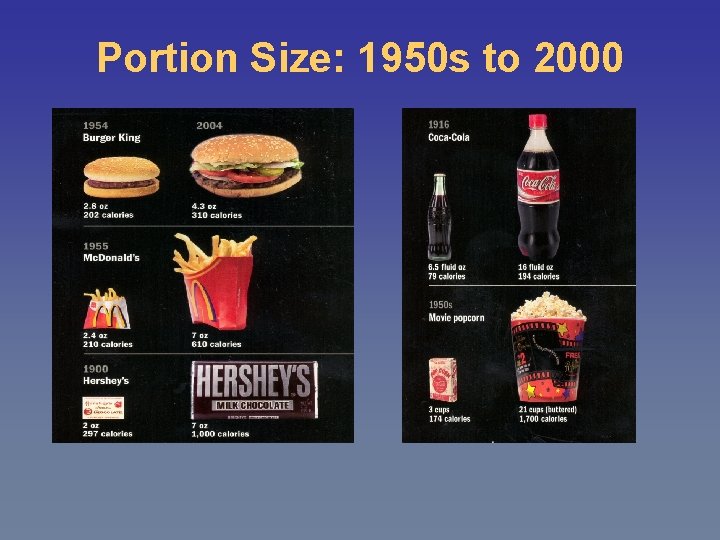
Portion Size: 1950 s to 2000
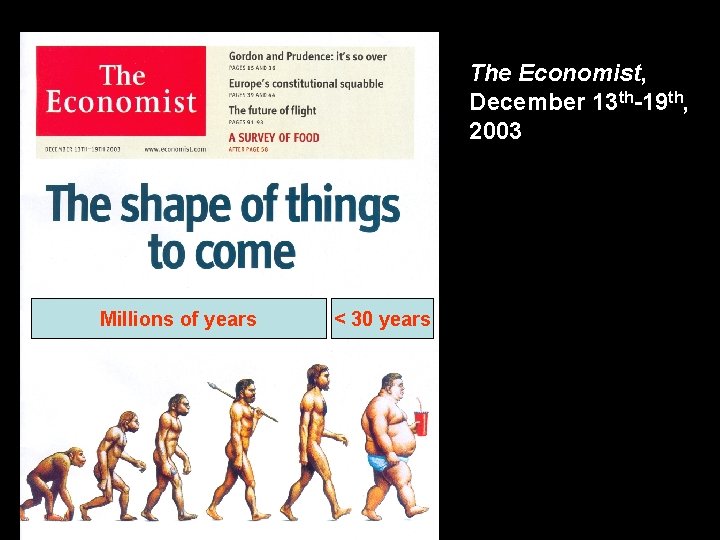
The Economist, December 13 th-19 th, 2003 Millions of years < 30 years
Revisiting the Guidelines Screening and Prevention Glycemic Management Targets Monitoring Treatment paradigm Macrovascular Complications BP and lipid targets
A Growing Divide Evidence Behaviour How can we facilitate translating science to better outcomes?
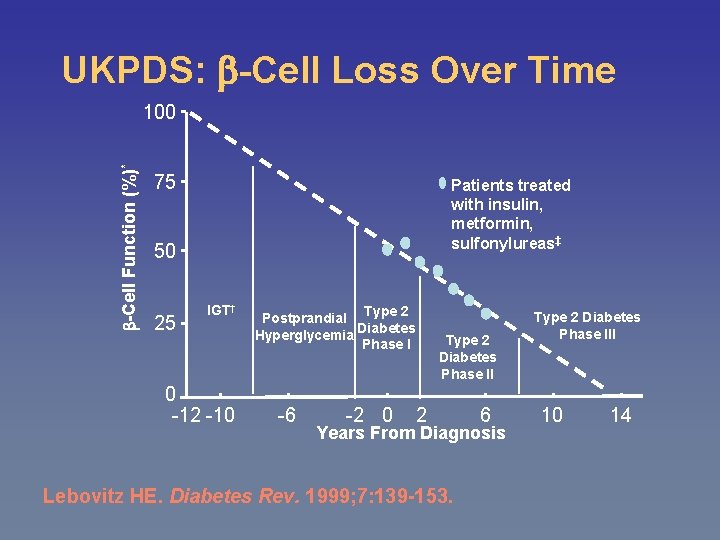
UKPDS: -Cell Loss Over Time -Cell Function (%)* 100 75 Patients treated with insulin, metformin, sulfonylureas‡ 50 25 IGT† 0 -12 -10 Type 2 Postprandial Diabetes Hyperglycemia Phase I -6 -2 0 Type 2 Diabetes Phase II 2 6 Years From Diagnosis Lebovitz HE. Diabetes Rev. 1999; 7: 139 -153. Type 2 Diabetes Phase III 10 14
Diabetes Management (It’s Not Just About Blood Glucose)
General Principles of Care • Multidisciplinary team approach • Care must be systematic – Use clinical flow charts – Institute diabetes mini clinics – Computer data bases assist with physician and patient recall • Sporadic reactive care is less effective in preventing complications
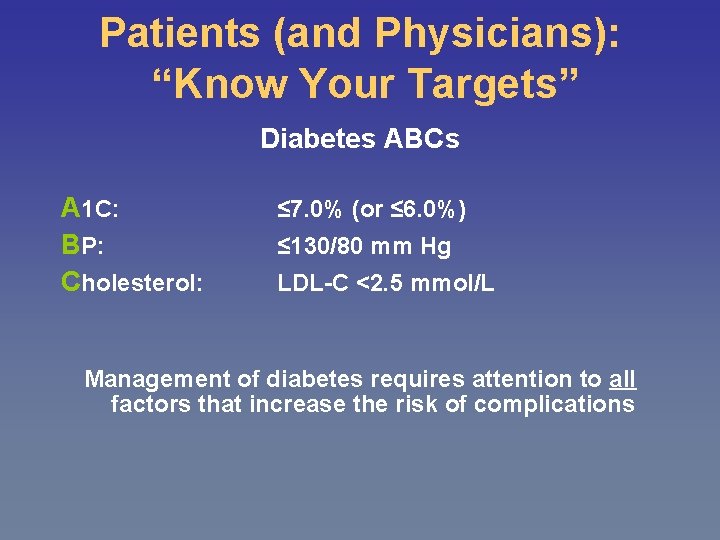
Patients (and Physicians): “Know Your Targets” Diabetes ABCs A 1 C: BP: Cholesterol: ≤ 7. 0% (or ≤ 6. 0%) ≤ 130/80 mm Hg LDL-C <2. 5 mmol/L Management of diabetes requires attention to all factors that increase the risk of complications
Glycemic Management
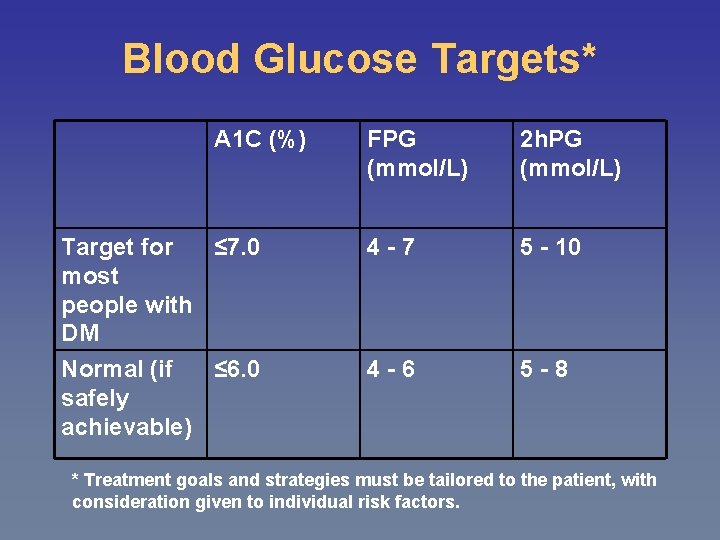
Blood Glucose Targets* A 1 C (%) Target for ≤ 7. 0 most people with DM Normal (if ≤ 6. 0 safely achievable) FPG (mmol/L) 2 h. PG (mmol/L) 4 -7 5 - 10 4 -6 5 -8 * Treatment goals and strategies must be tailored to the patient, with consideration given to individual risk factors.
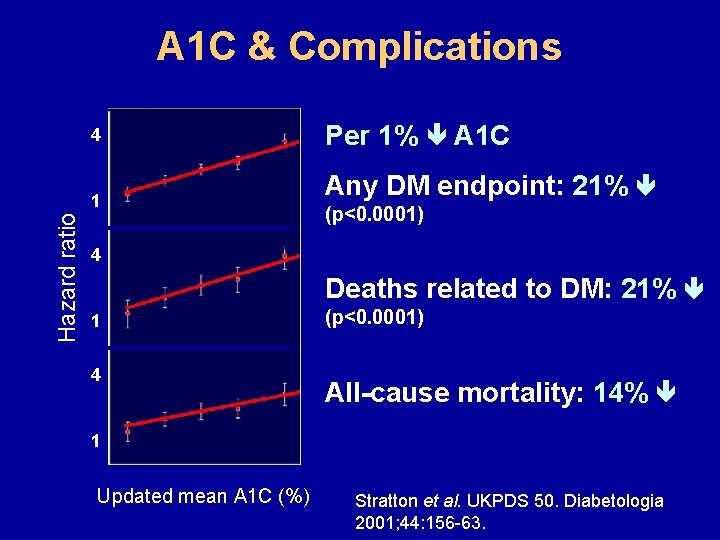
A 1 C & Complications Per 1% A 1 C 4 Any DM endpoint: 21% Hazard ratio 1 (p<0. 0001) 4 Deaths related to DM: 21% (p<0. 0001) 1 4 All-cause mortality: 14% (p<0. 0001) 1 5 6 7 8 9 10 Updated mean A 1 C (%) Stratton et al. UKPDS 50. Diabetologia 2001; 44: 156 -63.
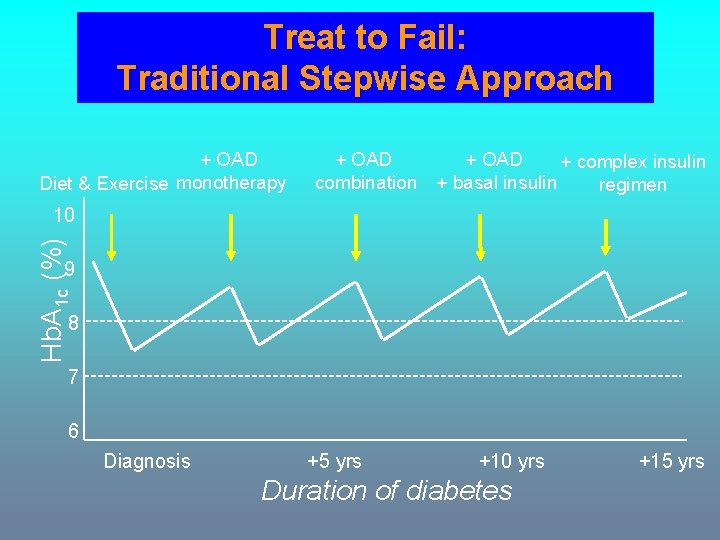
Treat to Fail: Traditional Stepwise Approach + OAD Diet & Exercise monotherapy + OAD combination + OAD + complex insulin + basal insulin regimen Hb. A 1 c (%) 10 9 8 7 6 Diagnosis +5 yrs +10 yrs Duration of diabetes +15 yrs
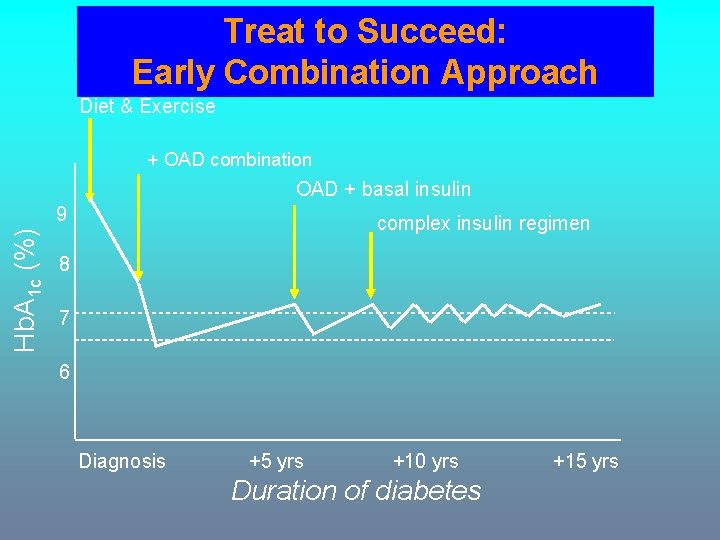
Treat to Succeed: Early Combination Approach Diet & Exercise + OAD combination OAD + basal insulin Hb. A 1 c (%) 9 complex insulin regimen 8 7 6 Diagnosis +5 yrs +10 yrs Duration of diabetes +15 yrs
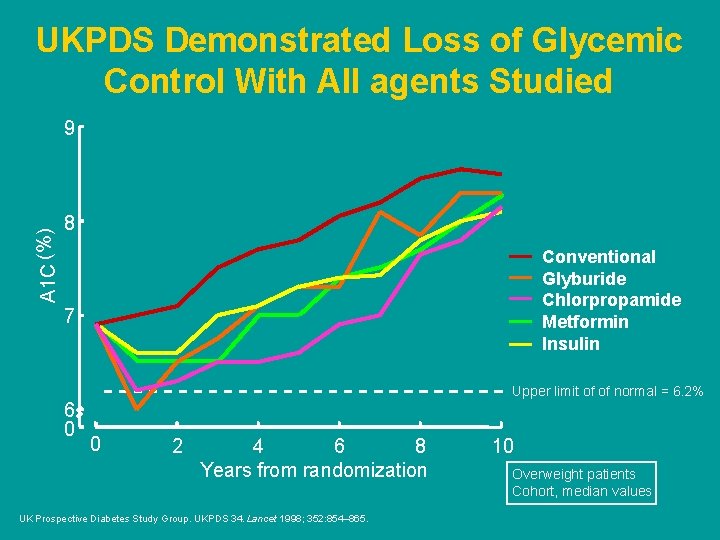
UKPDS Demonstrated Loss of Glycemic Control With All agents Studied A 1 C (%) 9 8 Conventional Glyburide Chlorpropamide Metformin Insulin 7 Upper limit of of normal = 6. 2% 6 0 0 2 4 6 8 Years from randomization UK Prospective Diabetes Study Group. UKPDS 34. Lancet 1998; 352: 854– 865. 10 Overweight patients Cohort, median values
Treatment Paradigm • Target euglycemia as early as possible (within 6 -12 months) • Tailor an individual regimen for each patient • Consider initial combination therapy, especially with marked hyperglycemia (A 1 C >9%) • Early and appropriate use of insulin
Polypharmacy A reality in modern diabetes management
Diabetes Medications In order to reach A 1 C, BP and lipid targets, people with diabetes typically require many medications: • To lower blood glucose: 1 -3 pills and/or insulin • To lower cholesterol: 1 or 2 pills • To lower blood pressure: 2 or 3 pills • For general vascular protection: aspirin Adherence to complex drug regimens can be a challenge for patients.
A solution to help improve adherence…
The Pill Burger
Who is Providing DM Care? Hux JE et al. Diabetes in Ontario, an ICES Practice Atlas, 2003
DICE: Diabetes in Canada Evaluation
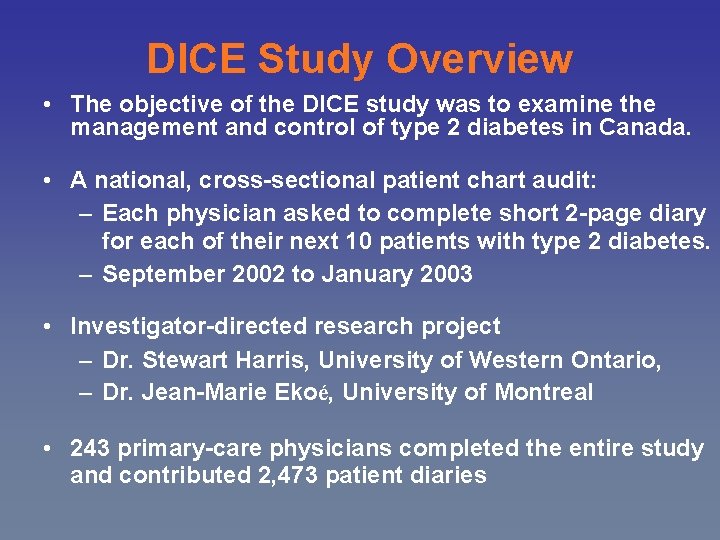
DICE Study Overview • The objective of the DICE study was to examine the management and control of type 2 diabetes in Canada. • A national, cross-sectional patient chart audit: – Each physician asked to complete short 2 -page diary for each of their next 10 patients with type 2 diabetes. – September 2002 to January 2003 • Investigator-directed research project – Dr. Stewart Harris, University of Western Ontario, – Dr. Jean-Marie Ekoé, University of Montreal • 243 primary-care physicians completed the entire study and contributed 2, 473 patient diaries
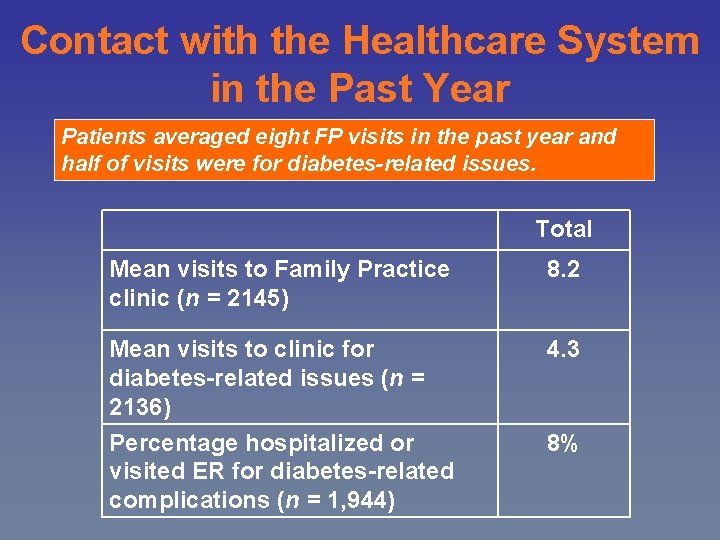
Contact with the Healthcare System in the Past Year Patients averaged eight FP visits in the past year and half of visits were for diabetes-related issues. Total Mean visits to Family Practice clinic (n = 2145) 8. 2 Mean visits to clinic for diabetes-related issues (n = 2136) 4. 3 Percentage hospitalized or visited ER for diabetes-related complications (n = 1, 944) 8%
Glycemic Control in Canada One in two type 2 diabetes patients in Canada are not at target (< 7%). Mean A 1 C = 7. 3% Most recent A 1 C test results (n = 2, 337) Uncontrolled A 1 c 49% Controlled A 1 c 51%
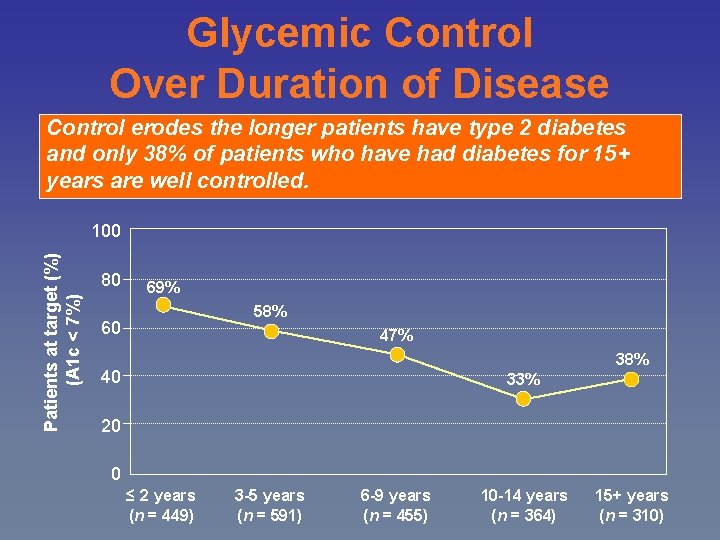
Glycemic Control Over Duration of Disease Control erodes the longer patients have type 2 diabetes and only 38% of patients who have had diabetes for 15+ years are well controlled. Patients at target (%) (A 1 c < 7%) 100 80 69% 58% 60 47% 38% 40 33% 20 0 ≤ 2 years (n = 449) 3 -5 years (n = 591) 6 -9 years (n = 455) 10 -14 years (n = 364) 15+ years (n = 310)
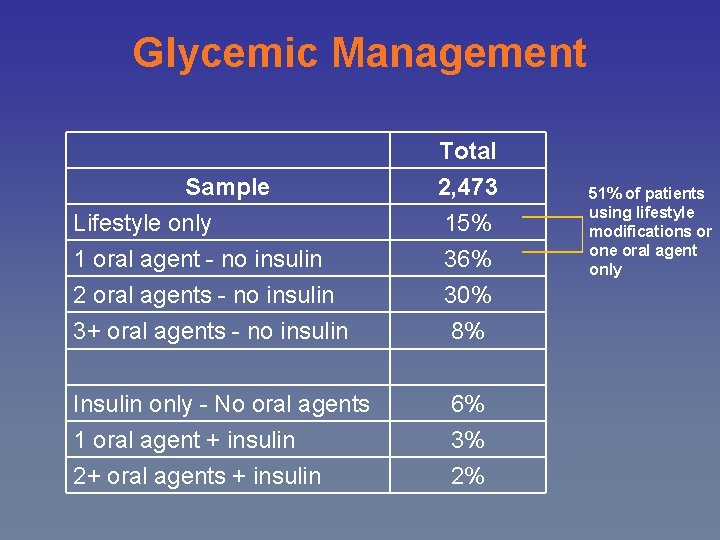
Glycemic Management Sample Total 2, 473 Lifestyle only 1 oral agent - no insulin 15% 36% 2 oral agents - no insulin 3+ oral agents - no insulin 30% 8% Insulin only - No oral agents 1 oral agent + insulin 2+ oral agents + insulin 6% 3% 2% 51% of patients using lifestyle modifications or one oral agent only
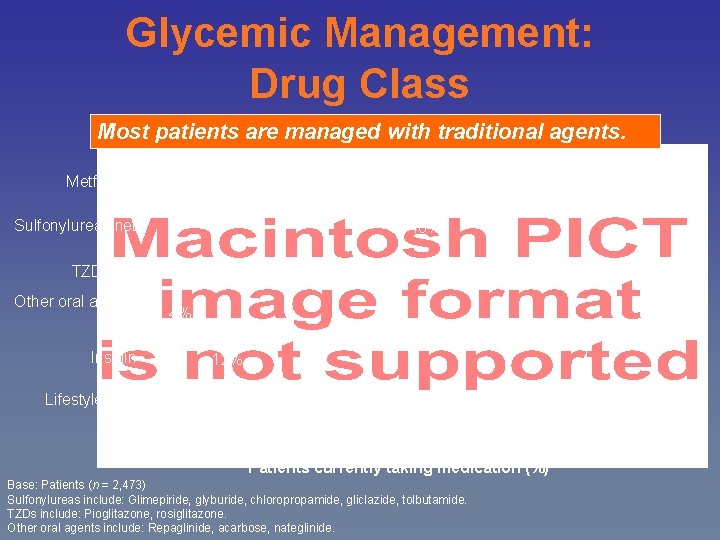
Glycemic Management: Drug Class Most patients are managed with traditional agents. Metformin 61% Sulfonylureas net 48% 15% TZDs net Other oral agents net Insulin Lifestyle only 4% 12% 15% Patients currently taking medication (%) Base: Patients (n = 2, 473) Sulfonylureas include: Glimepiride, glyburide, chloropropamide, gliclazide, tolbutamide. TZDs include: Pioglitazone, rosiglitazone. Other oral agents include: Repaglinide, acarbose, nateglinide.
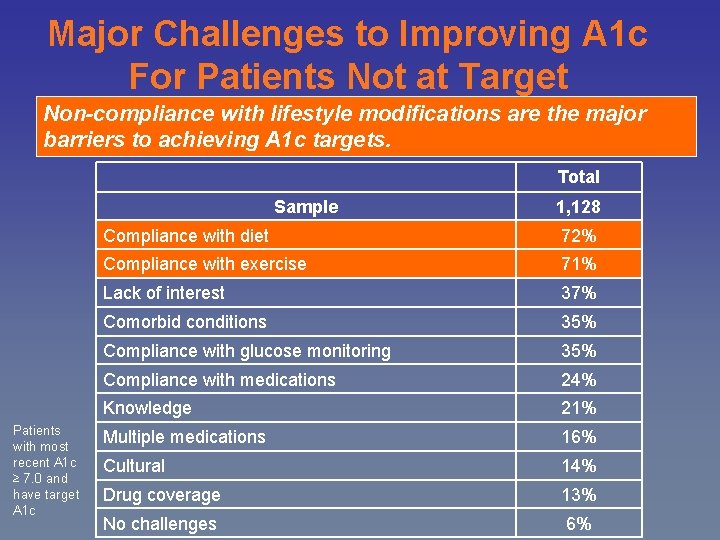
Major Challenges to Improving A 1 c For Patients Not at Target Non-compliance with lifestyle modifications are the major barriers to achieving A 1 c targets. Total Sample Patients with most recent A 1 c ≥ 7. 0 and have target A 1 c 1, 128 Compliance with diet 72% Compliance with exercise 71% Lack of interest 37% Comorbid conditions 35% Compliance with glucose monitoring 35% Compliance with medications 24% Knowledge 21% Multiple medications 16% Cultural 14% Drug coverage 13% No challenges 6%
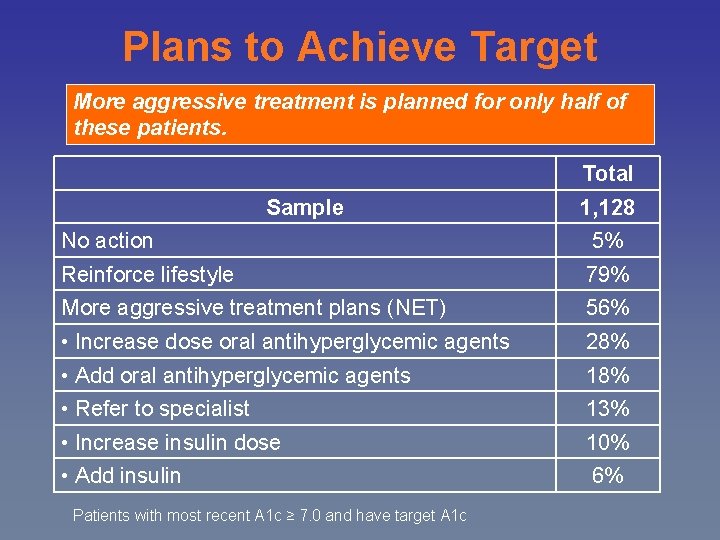
Plans to Achieve Target More aggressive treatment is planned for only half of these patients. Total Sample 1, 128 No action 5% Reinforce lifestyle 79% More aggressive treatment plans (NET) 56% • Increase dose oral antihyperglycemic agents 28% • Add oral antihyperglycemic agents 18% • Refer to specialist 13% • Increase insulin dose 10% • Add insulin 6% Patients with most recent A 1 c ≥ 7. 0 and have target A 1 c
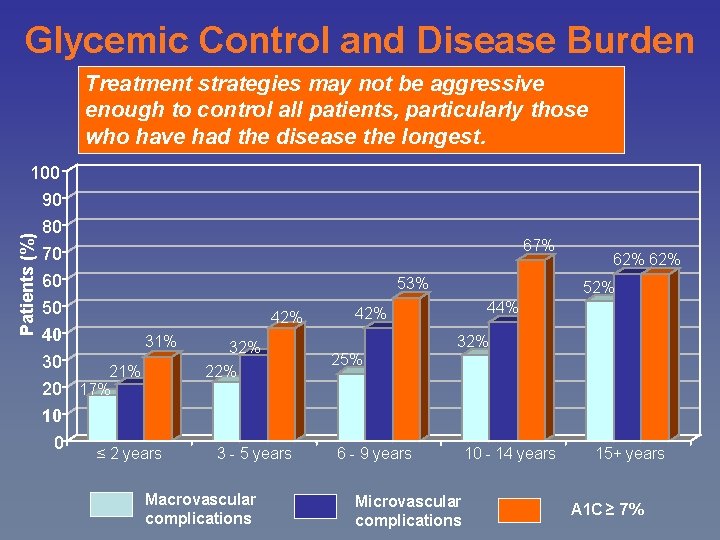
Glycemic Control and Disease Burden Treatment strategies may not be aggressive enough to control all patients, particularly those who have had the disease the longest. Patients (%) 100 90 80 70 60 50 40 31% 30 21% 20 17% 10 0 ≤ 2 years 67% 53% 42% 32% 22% 3 - 5 years Macrovascular complications 62% 52% 44% 42% 32% 25% 6 - 9 years Microvascular complications 10 - 14 years 15+ years A 1 C ≥ 7%
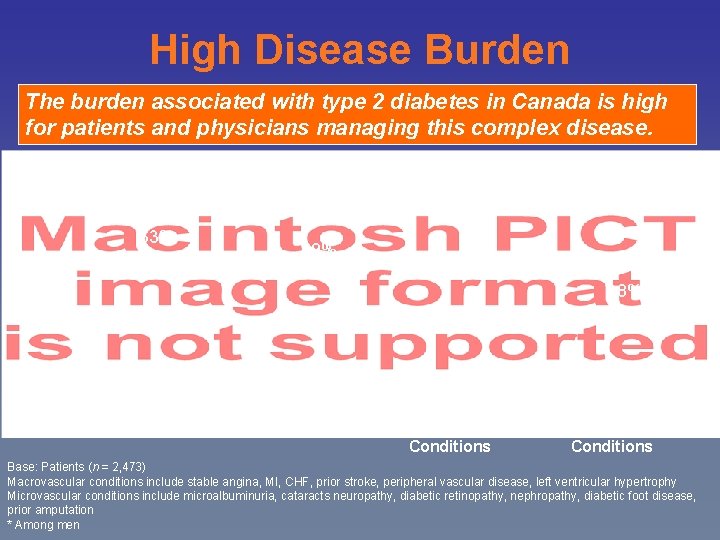
High Disease Burden The burden associated with type 2 diabetes in Canada is high for patients and physicians managing this complex disease. 63% 59% 38% 28% Hypertension Dyslipidemia Macrovascular Conditions Microvascular Conditions Base: Patients (n = 2, 473) Macrovascular conditions include stable angina, MI, CHF, prior stroke, peripheral vascular disease, left ventricular hypertrophy Microvascular conditions include microalbuminuria, cataracts neuropathy, diabetic retinopathy, nephropathy, diabetic foot disease, prior amputation * Among men
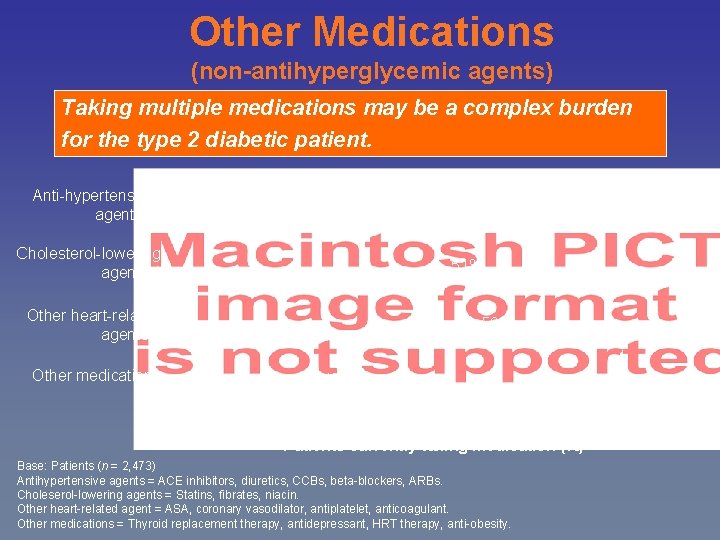
Other Medications (non-antihyperglycemic agents) Taking multiple medications may be a complex burden for the type 2 diabetic patient. Anti-hypertensive agents** 73% Cholesterol-lowering agents** 51% Other heart-related agents** Other medications 56% 24% Patients currently taking medication (%) Base: Patients (n = 2, 473) Antihypertensive agents = ACE inhibitors, diuretics, CCBs, beta-blockers, ARBs. Choleserol-lowering agents = Statins, fibrates, niacin. Other heart-related agent = ASA, coronary vasodilator, antiplatelet, anticoagulant. Other medications = Thyroid replacement therapy, antidepressant, HRT therapy, anti-obesity.
DICE Summary • In Canada, 1 in 2 patients with type 2 patients are not at target, suggesting that current treatment approaches in family practice are not intensive enough. • Type 2 diabetes is a complex disease with a high disease burden even within the first 2 years of diagnosis. • DICE suggests that with duration of diabetes, glycemic control erodes and morbidity increases among Canadian patients. • Physicians are cognizant of Clinical Practice Guideline glycemic targets, but this knowledge does not necessarily translate into action. • To help delay or even prevent complications earlier aggressive treatment is needed for type 2 diabetes patients in Canada.
- Slides: 55