Diabetes and Learning Disability Dr Andrew Lee YH
Diabetes and Learning Disability Dr Andrew Lee Y&H PHE Centre Lead for Learning Disabilities Andrew. lee@phe. gov. uk
Health profile of people with learning disabilities • In 2011, there were ~1. 2 million persons with learning disabilities in England • 905, 000 were adults (aged over 18 years) • 530, 000 were men, 375, 000 were women • ~170, 000 were children on school registers (2. 5%) • Considerably more people with learning disabilities in poorer households This Photo by Unknown Author is licensed under CC BY
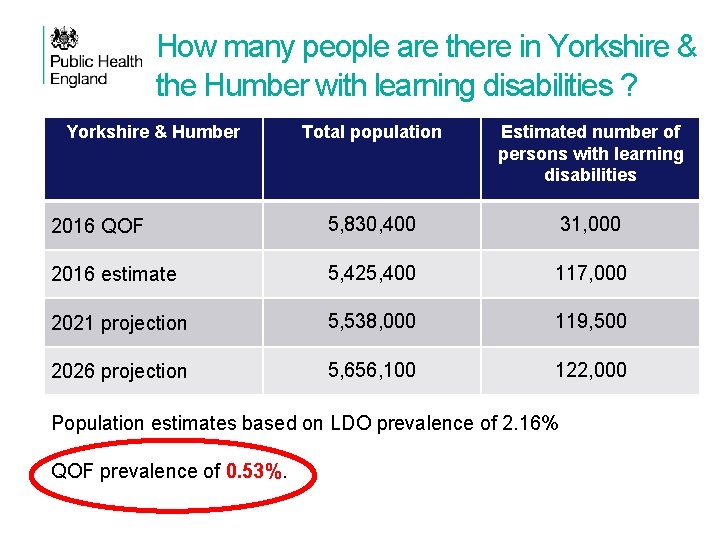
How many people are there in Yorkshire & the Humber with learning disabilities ? Yorkshire & Humber Total population Estimated number of persons with learning disabilities 2016 QOF 5, 830, 400 31, 000 2016 estimate 5, 425, 400 117, 000 2021 projection 5, 538, 000 119, 500 2026 projection 5, 656, 100 122, 000 Population estimates based on LDO prevalence of 2. 16% QOF prevalence of 0. 53%.
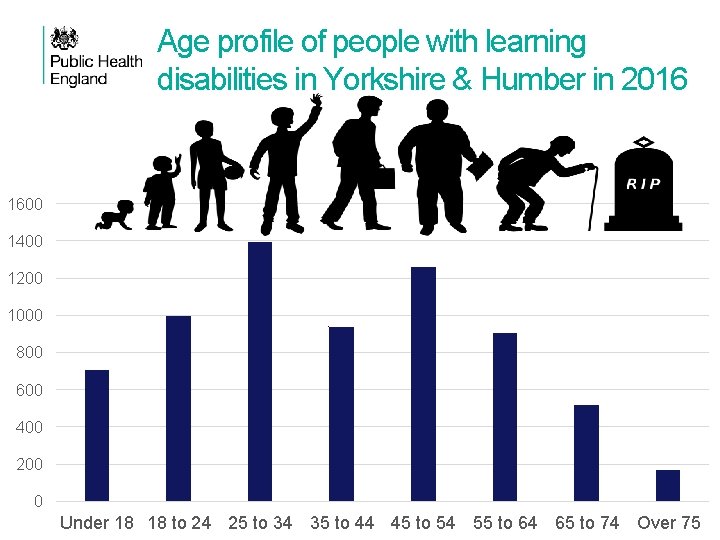
Age profile of people with learning disabilities in Yorkshire & Humber in 2016 1600 1400 1200 1000 800 600 400 200 0 Under 18 18 to 24 25 to 34 35 to 44 45 to 54 55 to 64 65 to 74 Over 75
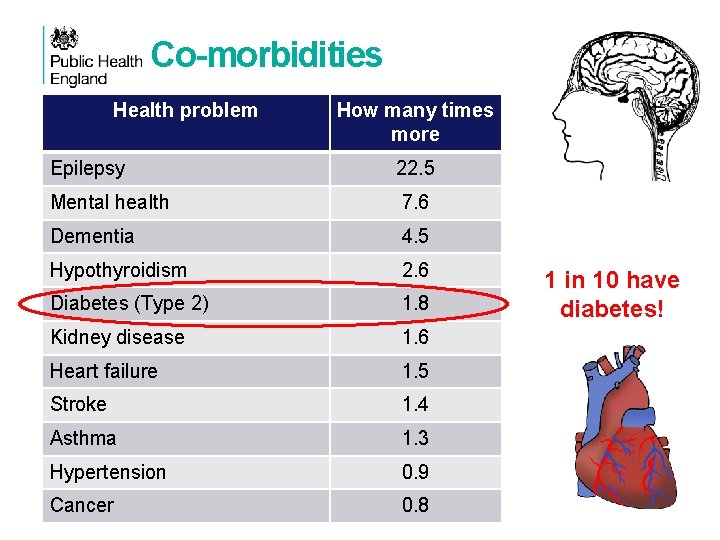
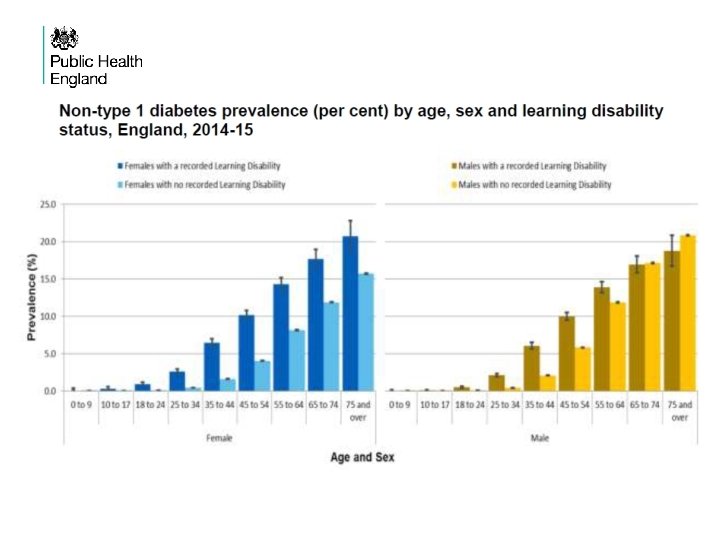
Co-morbidities Health problem How many times more Epilepsy 22. 5 Mental health 7. 6 Dementia 4. 5 Hypothyroidism 2. 6 Diabetes (Type 2) 1. 8 Kidney disease 1. 6 Heart failure 1. 5 Stroke 1. 4 Asthma 1. 3 Hypertension 0. 9 Cancer 0. 8 1 in 10 have diabetes!
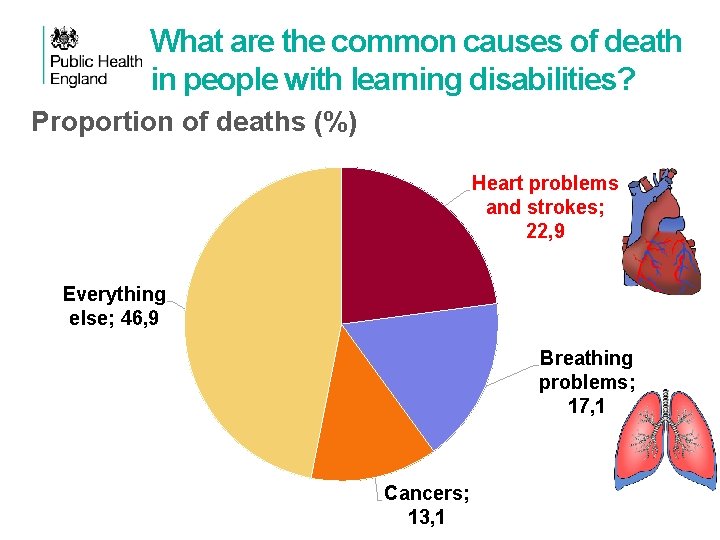
What are the common causes of death in people with learning disabilities? Proportion of deaths (%) Heart problems and strokes; 22, 9 Everything else; 46, 9 Breathing problems; 17, 1 Cancers; 13, 1
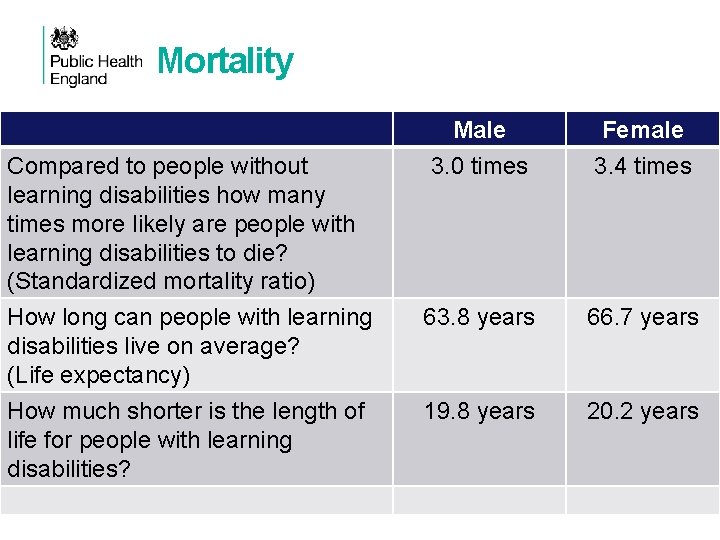
Mortality Compared to people without learning disabilities how many times more likely are people with learning disabilities to die? (Standardized mortality ratio) How long can people with learning disabilities live on average? (Life expectancy) How much shorter is the length of life for people with learning disabilities? Male 3. 0 times Female 3. 4 times 63. 8 years 66. 7 years 19. 8 years 20. 2 years
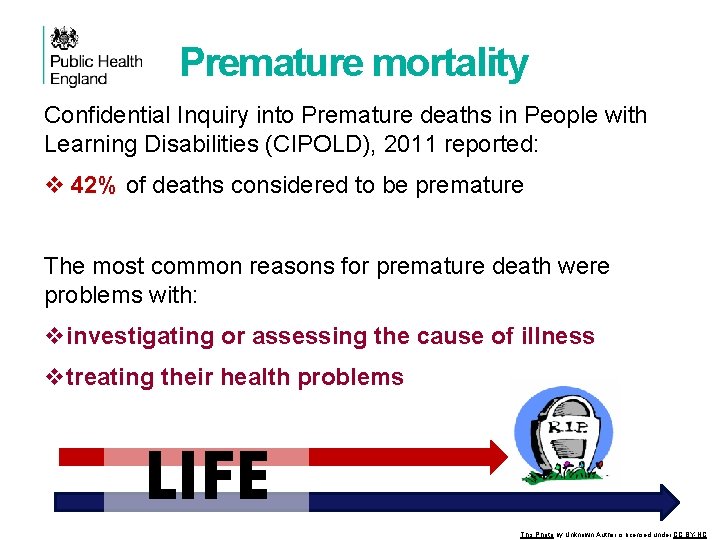
Premature mortality Confidential Inquiry into Premature deaths in People with Learning Disabilities (CIPOLD), 2011 reported: v 42% of deaths considered to be premature The most common reasons for premature death were problems with: vinvestigating or assessing the cause of illness vtreating their health problems LIFE This Photo by Unknown Author is licensed under CC BY-NC
Premature mortality BMA(2014) reported: Excess morbidity and premature mortality predominantly result from a failure to adequately diagnose, treat and prevent comorbid physical health conditions in people with a learning disability. In the worst cases, people receive less than optimal medical care and unnecessarily have unmet health needs. Research by Mencap (2012) found cases of DNAR orders being inappropriately applied to people with LD
Contributing factors q Lack of awareness of their health needs amongst health care staff. q Lack of effective advocacy for people with multiple conditions and vulnerabilities. q Lack of priority given in the NHS generally q Lack of coordination of care across and between different disease pathways and service providers. q Problems with identifying needs q Difficulty providing appropriate care in response to changing needs. TRANSITIONS ARE PROBLEMATIC Source: CIPOLD (2011)
Contributing factors q Low take-up for national screening programmes q Diagnostic overshadowing q Delays or problems with diagnosis or treatment q Communication problems during the consultation. q Lack of time to conduct an adequate consultation. q Patient inhibitions because of previous negative encounters SOURCE: CIPOLD & Mc. Carthy M. Exercising choice and control–women with learning disabilities and contraception. British Journal of Learning Disabilities. 2010 Dec 1; 38(4): 293 -302.
Contributing factors q Lack of reasonable adjustments to help people to access healthcare services. - Inflexible organisational policies, procedures and practices - E. g. many deaf people or those with a hearing impairment were forced to make contact with their GP using a method that was not the best for them - 90% of GP surgeries in Wales did not offer suitable alternatives for making appointments.
Equality Act 2010 When we’re making decisions, the Equality Act 2010 gives us a duty to take into account the need to: • eliminate discrimination, harassment and victimisation • advance equality of opportunity • foster good relations between different parts of the community This covers, age, disability, gender reassignment, marital or civil partnership status, pregnancy and motherhood, race (including ethnic or national origin, colour and nationality), religion or belief (including lack of belief), sex and sexual orientation.
What are reasonable adjustments? Reasonable adjustments are changes or additions to existing services designed to make them more accessible and effective for disabled people. Their aim is to ensure that disabled people are not excluded from services, and can achieve the same outcomes as those who are not disabled. Three things to consider when making reasonable adjustments: v Does the diabetes service have all the components it needs to ensure accessibility to and effectiveness for Pw. LD? (ACCESSIBLE) v Are there systems in place to ensure individuals are assessed and the appropriate adjustments are made to meet their personal needs? (MEETS NEEDS) v Do the people in the service have the right knowledge and skills? (STAFF TRAINED) 15
Learning Disabilities Register ü Get them on your GP Learning Disabilities Register. You can’t make reasonable adjustments if you haven’t identified them. ü Flag it on your GP systems and use it to alert and remind practice staff of the need to make adjustments. ü Don’t forget the carers, who often ignore their own health needs. They’re entitled to flu jabs too!
Diabetes and Learning disabilities: Reasonable adjustments needed along diabetes pathway
People with learning disabilities (Pw. LD) at higher risk of developing Type 2 diabetes • More sedentary lifestyle, low levels of exercise • Consuming high fat diets • Being prescribed high levels of antipsychotic medications which can contribute to obesity This Photo by Unknown Author is licensed under CC BY-SA (Source: Mac. Rae et al, 2015; Walwyn et al, 2015 and Mc. Villy et al, 2014; Taggart and Cousins, 2014).
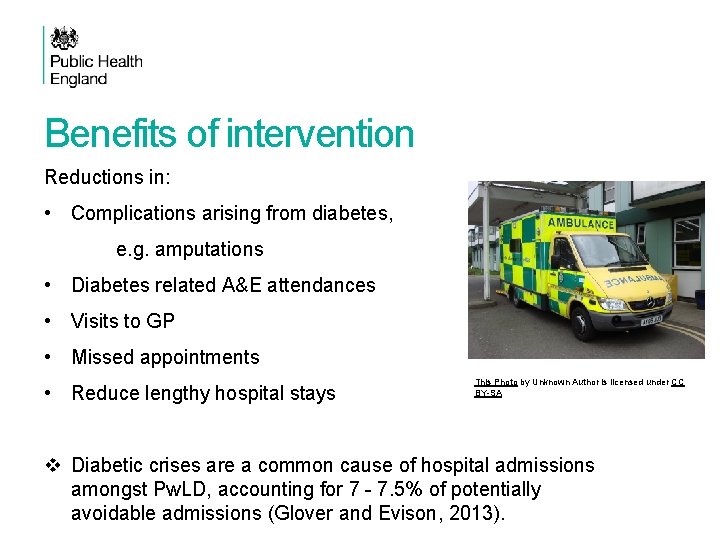
Benefits of intervention Reductions in: • Complications arising from diabetes, e. g. amputations • Diabetes related A&E attendances • Visits to GP • Missed appointments • Reduce lengthy hospital stays This Photo by Unknown Author is licensed under CC BY-SA v Diabetic crises are a common cause of hospital admissions amongst Pw. LD, accounting for 7 - 7. 5% of potentially avoidable admissions (Glover and Evison, 2013).
Where Reasonable adjustments are particularly essential ü Tests and investigations ü Structured support programmes to support health lifestyles, and structured education ü Weight management programmes ü Supported self-management of diabetes ü Personalised care planning
Identification of Diabetes Mellitus • Annual Health Checks • Adapted Diabetes Prevention Programme (where available) or other local lifestyle change programmes with reasonable adjustments • Where obesity is a significant problem, a specific weight loss programme is indicated, rather than a more generic lifestyle programme. • Individuals, who decline support in lifestyle change or weight loss should continue to be offered it and it is important to review capacity, explore reasons for refusal and provide reasonable adjustments if required.
ANNUAL HEALTH CHECKS Not to be confused with NHS Health Checks £ 140 for each patient aged 14 or over who received a compliant health check Series of questions that cover a range of issues from sex, disease screening to vulnerability. Linked to Health Action Plans Important tool for detecting issues RCGP has a useful toolkit on how to do it 25
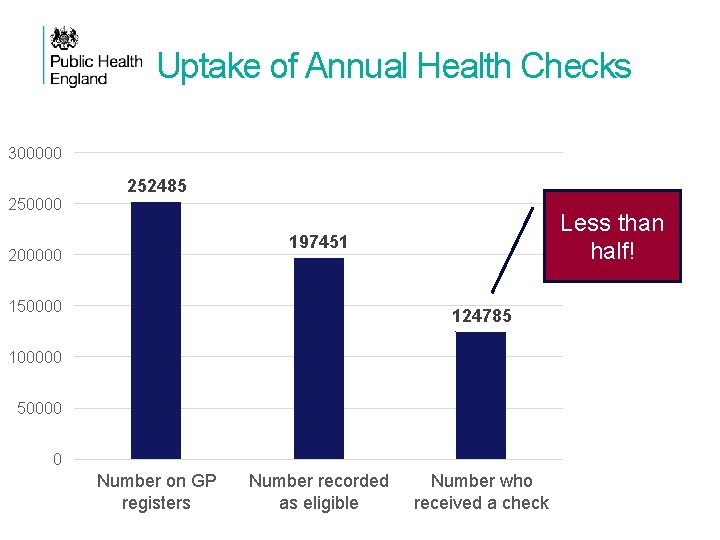
Uptake of Annual Health Checks 300000 252485 Less than half! 197451 200000 150000 124785 100000 50000 0 Number on GP registers Number recorded as eligible Number who received a check
Annual Health Checks: Opportunity for health promotion (Unhealthy) Lifestyle behaviours common: • Lack of physical activity • Poor diets • Alcohol, Tobacco and Drug use • Sex
Annual Health Checks Dental health Eye checks Hearing Feet Screening tests Flu jabs
Detect longer term health problems • • • Epilepsy Mental health Dementia Thyroid problems Diabetes Heart disease & strokes Dysphagia Asthma / respiratory problems Mobility
Responding to the initial diagnosis • Clinicians should check the person’s understanding of diabetes and be aware of their mood in response to diagnosis. • An initial assessment meeting can be facilitated by a learning disability health professional (e. g. a Learning Disability Nurse). • Some parts of the initial assessment (e. g. referral for diabetic retinopathy screening) could be delivered better at a later appointment. • It may be necessary for the initial assessment for diabetes management that Pw. LD are offered a phased series of appointments. • Part of the initial assessment is a requirement for a psychological assessment; which could be enhanced by an appropriately trained practitioner, able to make reasonable adjustments and has access to learning disability expert professionals.
Tests and investigations Two key features for reasonable adjustments: v Use of accessible material ensures good understanding of procedure v Always involving carers where possible. Pw. LD have higher rates of physical and mental health problems, problematic health behaviours, plus the stress of illness. Can aggravate glycaemic control and necessitates more frequent monitoring of blood glucose and urine or blood ketones. Where multimorbidity occurs, conflict between the recommendations for different diseases may occur. Need shared decision making with the individual and their supporter/carer to make decisions which patients find most appropriate to them
Issues with procedures They may be very fearful of medical procedures and examination! ü Familiarise them with procedures and clinical settings in advance. ü Use dolls, etc… to demonstrate the procedure ü Have you got topical anaesthetics for painful procedures? ü Are there any videos you can show them? https: //www. youtube. com/watch? v=c 4 g. VGmllu 7 c
Structured support • DESMOND structured education programme recommended as routine. • Has been adapted for adults with a learning disability. Can be delivered in a community setting, over 6 -weeks, with 1 session per week, each ~2. 5 hours, to Pw. LD and their carers. • DESMOND-ID programme had an additional education session aimed at family/paid carers to support their understanding about Type 2 diabetes and their specific role in supporting the Pw. LD. • Initial results suggest that such a multi-session education programme can be acceptable and feasible to deliver. • Important for commissioners to work with other providers of structured education in making the necessary reasonable adaptions to meet the needs of Pw. LD.
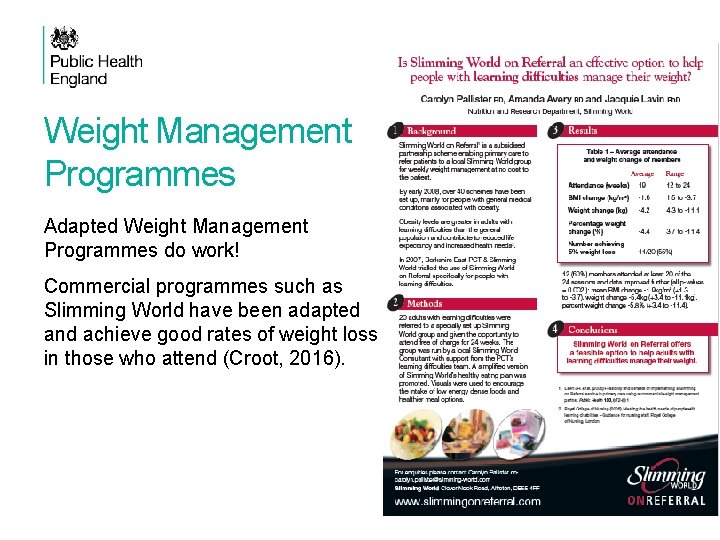
Weight Management Programmes Adapted Weight Management Programmes do work! Commercial programmes such as Slimming World have been adapted and achieve good rates of weight loss in those who attend (Croot, 2016).
Supported self-management • With support, many Pw. LD can set goals for self-management and participate in discussions about how to achieve them. • To achieve self-caring, education has a role, beginning from diagnosis to ongoing care. • Family members, advocates or paid support staff can make significant contributions the effectiveness of treatment by being part of: - Care planning and implementation - Identification of areas of risk, contributing to risk management plans. - Support staff need training in supporting self-management in diabetes • Should be given adequate and accessible information to increase opportunity to make informed decisions. • Mental Capacity Act training required for staff
Type 1 Diabetes Mellitus Low literacy and comprehension levels can make it difficult to learn new skills such as: • monitoring blood glucose levels, • injecting insulin or • learning how to use a new insulin device. Use of colour coded blood glucose monitors and structured education material for Pw. LD helpful.
Type 2 Diabetes Mellitus • The OK Diabetes study (Walwyn et al, 2015; House et al, 2016) developed a well supported self-management plan involving professional support via DSNs. The following elements needed before a supported selfmanagement plan is devised: ü An individual’s daily routine and lifestyle including current diet, social/work activity routines, food shopping and food preparation, ü Current self-reported health and self-management, identifying all supporters and helpers and who the key supporter is and their role in the life of the person with diabetes. • Goal setting should be realistic and done in collaboration with the Pw. LD aiming to involve the person in any lifestyle changes • Support should be given to goals suggested by the Pw. LD with diabetes that are specific, simple and achievable given the person’s current routines and social support (Walwyn et al, 2015; House et al, 2016).
Person centred care planning • For everyone with diabetes there should be an annual care plan review. • The management of diabetes for Pw. LD should be reflected in the Health Check Action Plan (HCAP) which is an outcome of the AHC. • The HCAP enables Pw. LD gain control and own their health needs and together with their GP plan how to meet these needs. • The HCAP should detail how the individual’s diabetes will be managed. - Might involve referral to DSNs who will together with the individual agree on goals and actions to be set out in the Diabetes Care Plan. - Care planning appointment with the Diabetes team should discuss results of the diabetes annual check • Pw. LDs and their carers may require more support from DSNs, Practice Nurses, GP and Community Learning Disability Teams. • Address mental health needs of a person with diabetes.
Accessible Information Standard (2016) Requirement! Make sure the information we give is accessible and understandable. Use EASY READ leaflets Use pictorial communication aids like social stories
Improving communication Medical information is often confusing for the patient/carer ü Provide easy read if possible ü Write it down ü Use pictures, large print and simpler words ü Let them audio record the consultation ü Allow in their carer to help them remember things
Appointments Remember they often have multiple health appointments to attend… ü Help them to plan appointments in advance if possible ü Be flexible with providing them appointments Do they need more time with the GP? ü Book a double appointment ü Book the last slot of the clinic session
Other Reasonable Adjustments Their needs may be very specific. ü If they need reasonable adjustments can they make arrangements with someone nominated in the practice for this (e. g. senior receptionist or practice manager in advance) They may be unsettled in the waiting room (claustrophobic, too much stimulation/noise, boring, etc…) ü Have them wait outside (e. g. in the car) & make an arrangement with the receptionist to call them in? ü Get the first appointment or end of the day when it is quieter? ü Arrange a home visit in advance?
Parents & Carers • They are not the enemy but valuable allies! • Remember that being a carer is extremely demanding and exhausting, and many may be ‘on the edge’ • They also know the Pw. LD well, what’s normal, what’s not, how they communicate, how they express pain etc… Many of them do have the patient’s best interest at heart. • At the end of the day health professionals may only see the ‘challenging’ patient once, but the parent/carer has to deal with it all the time…
Other considerations They are vulnerable adults to exploitation, abuse, domestic violence and assault. Lack of ‘problem-solving skills Lack insight into dangerous/risky situations Older Pw. LD may no longer have family carers to look out for them. Issues around mental capacity Coordination of care – Who’s taking responsibility? It is important to maintain consistency of care teams
Features of successful programmes Successful programmes adapted to meet the needs of Pw. LD are seen to have addressed the following: - Provision of adequate and accessible information to enable full participation - Accommodating views of those with a learning disability - Family/carer involvement also supporting their understanding of diabetes - Short sessions with Pw. LD and their carers - Programme rolled out over longer periods in community settings - Realistic goal setting
What this means for Commissioners q Know your population q Increase uptake of Health Checks q Avoid unnecessary hospital admissions q Reduce lengthy hospital stay q Support healthy lifestyle q Supporting structured education and self-management
Diabetes UK recommendations 1. Make information accessible 2. Provide training for staff 3. Address social barriers 4. Involve supporters 5. Plan for and make reasonable adjustments
Resources NHS England (2017): Rightcare pathway: Diabetes - Reasonable adjustments for people with a learning disability who have diabetes. https: //www. england. nhs. uk/rightcare/wpcontent/uploads/sites/40/2017/11/rightcare-pathway-diabetes-reasonableadjustments-learning-disability-2. pdf Diabetes UK: How to make reasonable adjustments to diabetes care for adults with a learning disability https: //www. diabetes. org. uk/resources-s 3/2018 -02/Diabetes%20 UK%20%20 How%20 to%20 make%20 reasonable%20 adjustments%20 to%20 diabetes %20 care%20 for%20 adults%20 with%20 a%20 learning%20 disability. pdf
Patient quotes
Understanding of food choices ‘I can eat fruit but can’t eat crisps – it’s difficult to not eat the things the doctor said not to’ ‘I don’t know what to eat or how to control it. I wasn’t given a diet sheet’ ‘Dieticians and sheets don’t always work – if you don’t know what moderation is then you can’t do it’ This Photo by Unknown Author is licensed under CC BY-SA This Photo by Unknown Author is licensed under CC BY-NC-ND
Management of diabetes ‘I've always found the most difficult thing is managing diabetes with someone who can’t communicate as easily as your average person. How can X say whether she feels ok or not. We rely on lots of blood tests – and that leads to very sore fingers!’ ‘X functions best in a structured regime so he has a written daily routine which he, and any support staff, refer to. This sets out timing and dosages for insulin injections and times when to take blood tests’. ‘I forget to take my medication’
Access to information ‘I can’t read the letters that they give me – especially the complicated words’ ‘My support worker reads my letters’ ‘Big print or helping read through it would help’ ‘Sometimes they assume you know something or can read it when you can’t
Referrals and appointments ‘I don’t like waiting hours to get a blood test’ ‘For seeing the consultant ask ahead for the first appointment so you are straight in is my only suggestion - get to know 1 consultant well who is sympathetic to the extra needs, make these known in writing’. Tips for doctors: ‘Talk to you and not the support worker – they can seem rude’ This Photo by Unknown Author is licensed under CC BY-NC-ND
Inpatient issues ‘It can be daunting or overwhelming in hospital’ ‘It is good if they let you choose which room to go into – I don’t like all the rooms’ ‘I don’t like being crowded round by lots of different people – I worry about what is being said’ ‘I struggle getting my daughter to cope with the clinics as she associates hospitals with her admission for diagnosis which was very traumatic’
Multi-professional working ‘Diabetes professionals may have the expertise about the condition but are unlikely to have had much training in learning disability, and can therefore give complicated instructions’. ‘The second tip is to build a small expert team around your child. Try to minimise the number of different consultants, diabetes nurses as getting to know how your child’s diabetes affects them, particularly if they find communication difficult, requires familiarity over a period of time’.
Spread the message and raise awareness with your staff and colleagues

- Slides: 57