Diabetes An Overview Maria Carr Learning Outcomes On
Diabetes An Overview Maria Carr
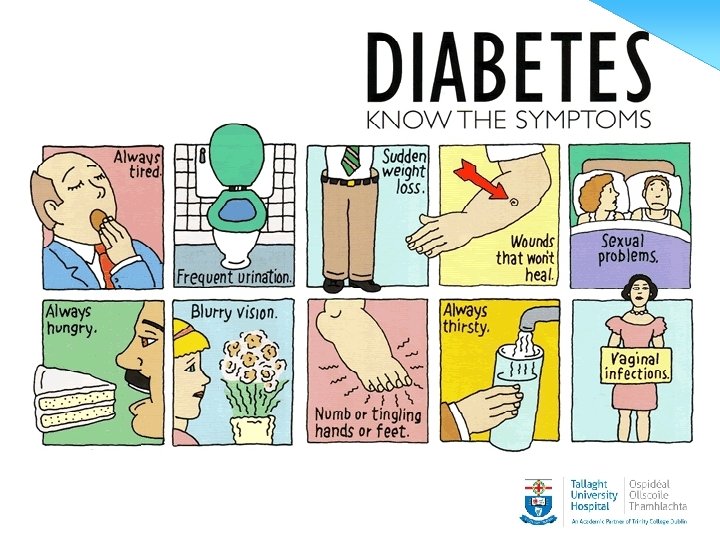
Learning Outcomes On completing this masterclass, the nurse will have an enhanced knowledge of the following • Diagnosis and Classification of diabetes • The treatment and management of type 1 diabetes • The treatment and management of type 2 diabetes • The screening for and prevention of the complications of diabetes
The diagnosis and classification of Diabetes
Classification • • • Type 1 Type 2 Type 1. 5/LADA and MODY I. G. T. /I. F. G. Secondary Gestational

What is the difference between type 1 and type 2 diabetes
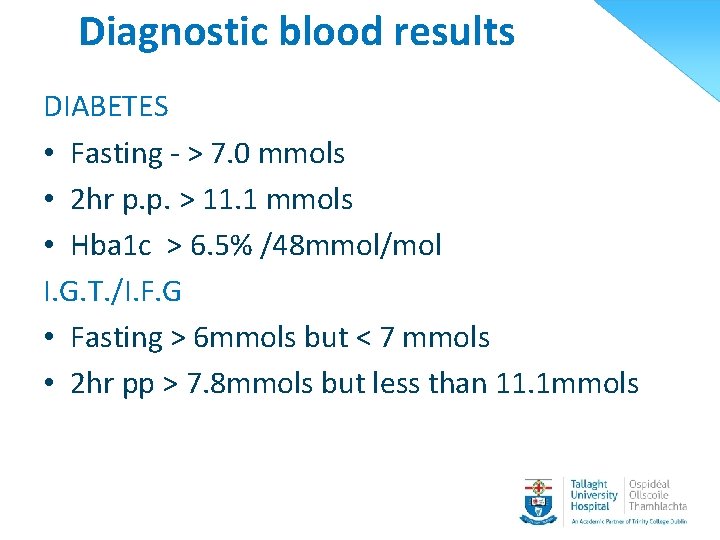
Diagnostic blood results DIABETES • Fasting - > 7. 0 mmols • 2 hr p. p. > 11. 1 mmols • Hba 1 c > 6. 5% /48 mmol/mol I. G. T. /I. F. G • Fasting > 6 mmols but < 7 mmols • 2 hr pp > 7. 8 mmols but less than 11. 1 mmols
Monitoring diabetes
The treatment and management of type 2 diabetes
Type 2 Diabetes • • • Onset typically over the age 40 yrs Genetic predisposition Associated with obesity Gradually onset [on average 7 -12 yrs] Insulin resistance /insulin insufficiency
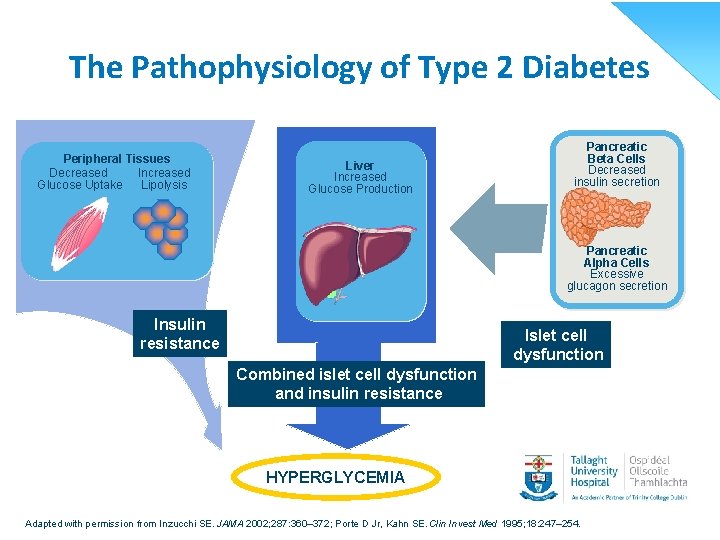
The Pathophysiology of Type 2 Diabetes Peripheral Tissues Decreased Increased Glucose Uptake Lipolysis Liver Increased Glucose Production Pancreatic Beta Cells Decreased insulin secretion Pancreatic Alpha Cells Excessive glucagon secretion Insulin resistance Islet cell dysfunction Combined islet cell dysfunction and insulin resistance HYPERGLYCEMIA Adapted with permission from Inzucchi SE. JAMA 2002; 287: 360– 372; Porte D Jr, Kahn SE. Clin Invest Med 1995; 18: 247– 254.
Weight reduction

Portion Size for Adults
![Exercise • 30 minutes daily [at least three times a week] • 45 min Exercise • 30 minutes daily [at least three times a week] • 45 min](http://slidetodoc.com/presentation_image_h/34e454d25a5cc6e4b1afe60f1e4258df/image-14.jpg)
Exercise • 30 minutes daily [at least three times a week] • 45 min to one hour - if weight loss is needed • At a pace that requires effort
Treatment of Type 2 • Healthy lifestyle and O. H. A • Healthy lifestyle, OHA and GLP- 1 • Healthy lifestyle O. H. A. and insulin • Healthy lifestyle and insulin
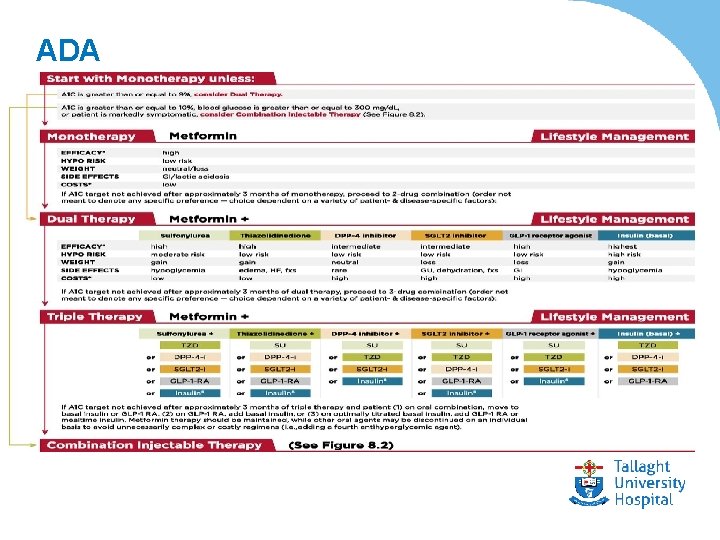
ADA
Drug treatment for patients with type 2 diabetes • • Metformin Sulphonyureas Prandial glucose regulators – novonorm Glitazones GLP 1 DDP 4 inhibitors SGLT 2
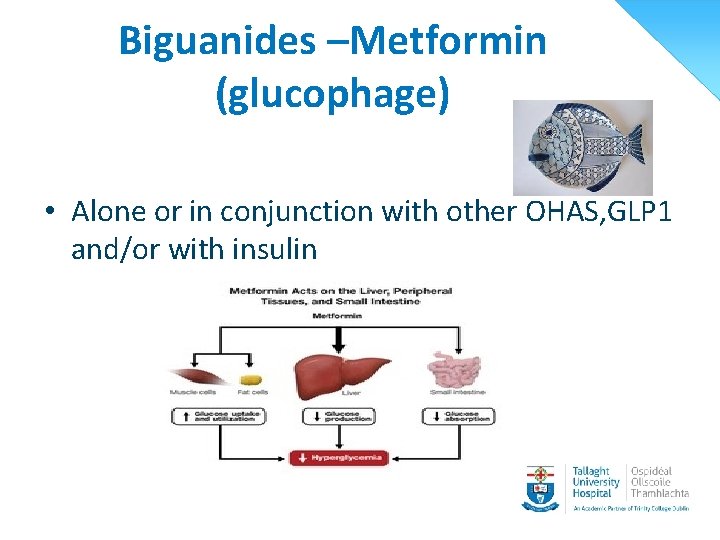
Biguanides –Metformin (glucophage) • Alone or in conjunction with other OHAS, GLP 1 and/or with insulin
Metformin • Main side effect Use with caution in those with renal impairment
![Sulphonylureas • Release insulin from beta cells [improves insulin secretion] • Given alone or Sulphonylureas • Release insulin from beta cells [improves insulin secretion] • Given alone or](http://slidetodoc.com/presentation_image_h/34e454d25a5cc6e4b1afe60f1e4258df/image-20.jpg)
Sulphonylureas • Release insulin from beta cells [improves insulin secretion] • Given alone or in conjunction with other OHA • Side effect -
![Sulphonyureas • Gliclazide mr 30 -120 mg [diaglyc, diamicron mr, zycron mr] • Glipizide Sulphonyureas • Gliclazide mr 30 -120 mg [diaglyc, diamicron mr, zycron mr] • Glipizide](http://slidetodoc.com/presentation_image_h/34e454d25a5cc6e4b1afe60f1e4258df/image-21.jpg)
Sulphonyureas • Gliclazide mr 30 -120 mg [diaglyc, diamicron mr, zycron mr] • Glipizide 5 mg[glibenese] • Glibenclamide Daonil 5 mg • Glimepiride 1 mg-4 mg [amaryl]
Glitazones -Actos • Insulin action enhancer • Used as a second line in conjunction with another OHA • Contraindicated in severe renal impairment
GLP 1 • Incretin mimic • Used in combination with Glucophage and/or sulphonylurea • Side effects
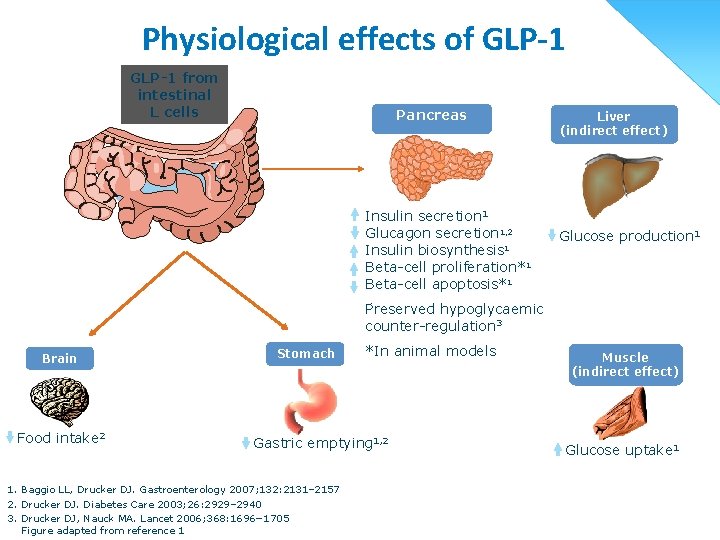
Physiological effects of GLP-1 from intestinal L cells Pancreas Insulin secretion 1 Glucagon secretion 1, 2 Insulin biosynthesis 1 Beta-cell proliferation*1 Beta-cell apoptosis*1 Liver (indirect effect) Glucose production 1 Preserved hypoglycaemic counter-regulation 3 Brain Food intake 2 Stomach *In animal models Gastric emptying 1, 2 1. Baggio LL, Drucker DJ. Gastroenterology 2007; 132: 2131– 2157 2. Drucker DJ. Diabetes Care 2003; 26: 2929– 2940 3. Drucker DJ, Nauck MA. Lancet 2006; 368: 1696− 1705 Figure adapted from reference 1 Muscle (indirect effect) Glucose uptake 1

GLP -1 • Exenatide (Bydureon/Byetta) e. GFR<30 • Liraglutide (Victoza) e. GFR <30 • Dulaglutide (Trulicity) e. GFR < 30
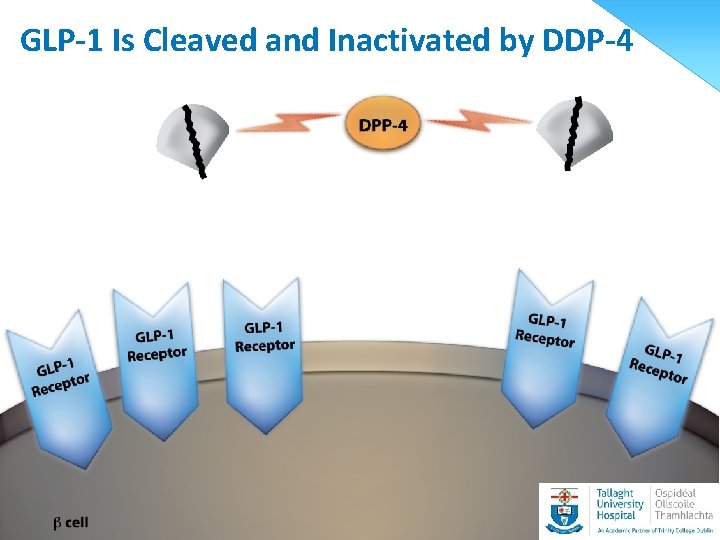
GLP-1 Is Cleaved and Inactivated by DDP-4
![DDP inhibitors • Linagliptin [Trajenta] 5 mg /no dose adjustment • Saxaglitin [Onglyza] e. DDP inhibitors • Linagliptin [Trajenta] 5 mg /no dose adjustment • Saxaglitin [Onglyza] e.](http://slidetodoc.com/presentation_image_h/34e454d25a5cc6e4b1afe60f1e4258df/image-27.jpg)
DDP inhibitors • Linagliptin [Trajenta] 5 mg /no dose adjustment • Saxaglitin [Onglyza] e. GFR< 50 /2. 5 mg OD • Sitagliptin [Januvia] e. GFR 30 -50 /50 mg OD • Vildaglipton [Galvus] e. GFR< 50 /50 mg OD
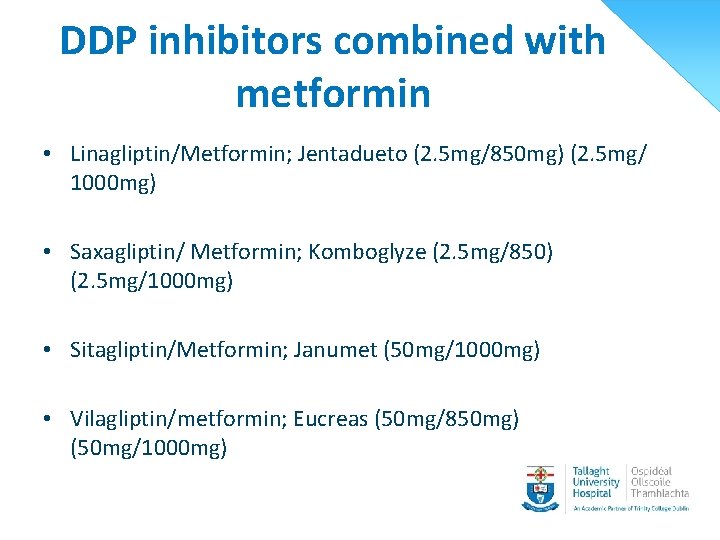
DDP inhibitors combined with metformin • Linagliptin/Metformin; Jentadueto (2. 5 mg/850 mg) (2. 5 mg/ 1000 mg) • Saxagliptin/ Metformin; Komboglyze (2. 5 mg/850) (2. 5 mg/1000 mg) • Sitagliptin/Metformin; Janumet (50 mg/1000 mg) • Vilagliptin/metformin; Eucreas (50 mg/850 mg) (50 mg/1000 mg)
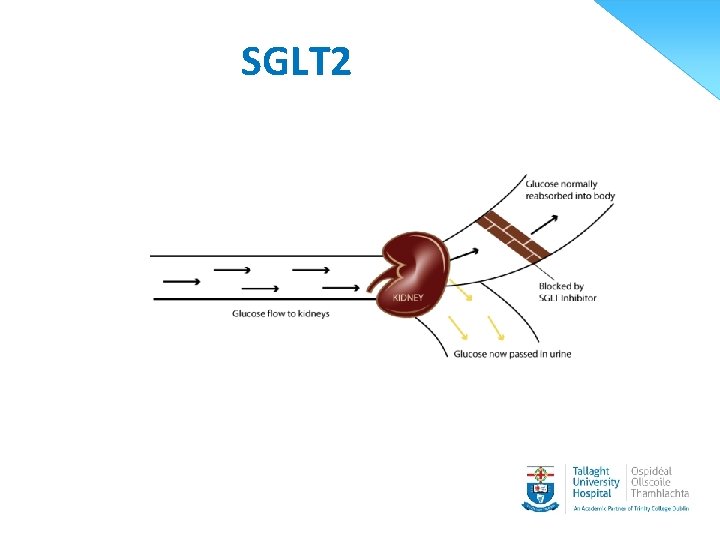
SGLT 2 29
SGLT 2 • No hypos • Reduce weight • Reduce blood pressure But……… Genitourinary infections Polyuria
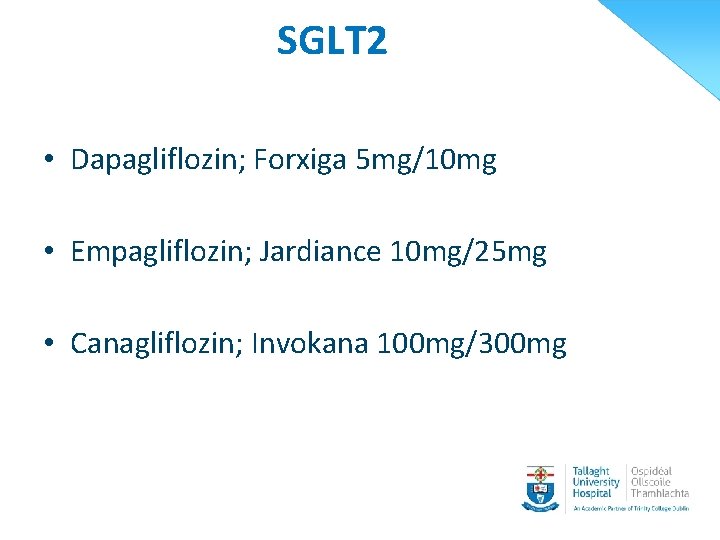
SGLT 2 • Dapagliflozin; Forxiga 5 mg/10 mg • Empagliflozin; Jardiance 10 mg/25 mg • Canagliflozin; Invokana 100 mg/300 mg
Insulin therapy in type 2 diabetes • OHAS and long acting analogues • Biphasic insulin usually given pre breakfast and pre evening meal • Basal/ bolus
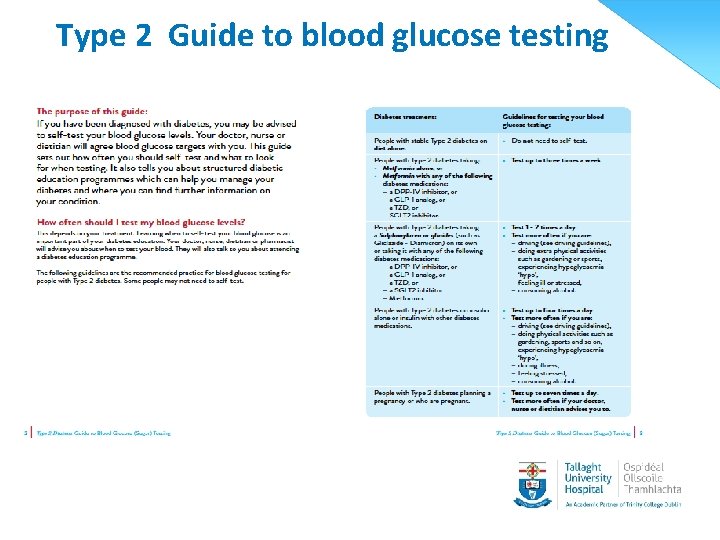
Type 2 Guide to blood glucose testing • •
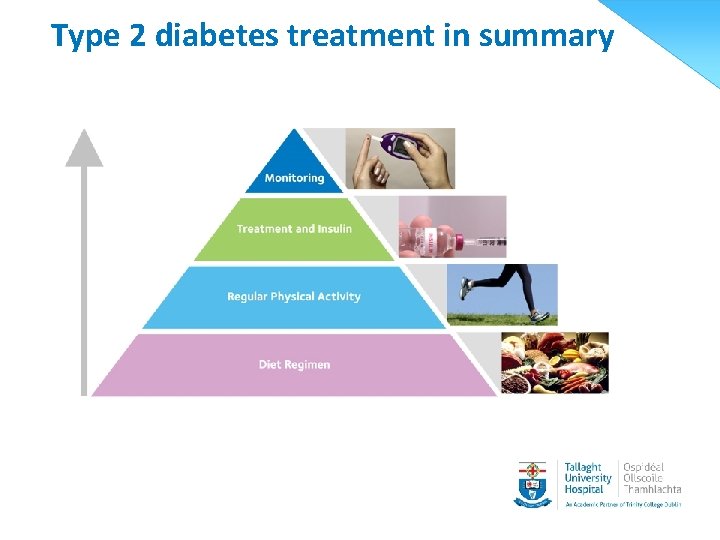
Type 2 diabetes treatment in summary
The treatment and management of type 1 diabetes
Type 1 Diabetes • • • Onset usually < 40 yrs Typically normal weight or slim No endogenous insulin Onset dramatic Family history less common • Insulin is needed to sustain life
Treatment of type 1 diabetes • Healthy lifestyle • Healthy eating • Carbohydrate counting/Carbohydrate awareness • Exercise • Monitoring • Insulin [needed to sustain life]
Insulin therapy
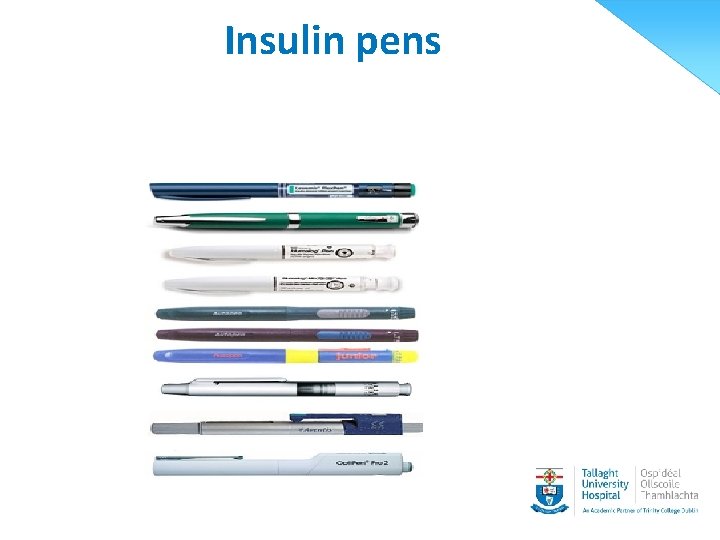
Insulin pens
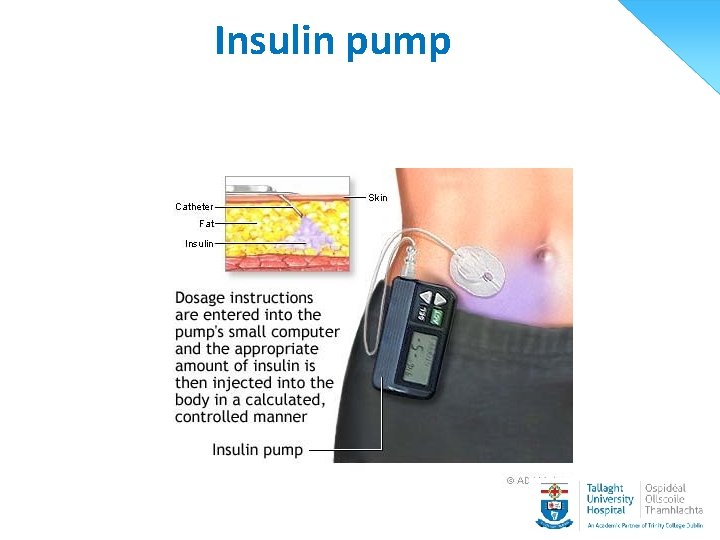
Insulin pump
Types of insulin • Rapid acting analogues - Novorapid, Humalog Apidra • Short acting – Humlin S, Insuman rapid • Long acting analogues - Lantus, Toujeo, Levemir, Tresbia, • Intermediate – Insulatard, Humlin 1, Insuman basal • Biphasic insulin Insuman comb, Humlog mix 25/50, Novomix 30
Common insulin regime • Basal/ bolus • Biphasic insulin bd • Insulin pump/Rapid acting
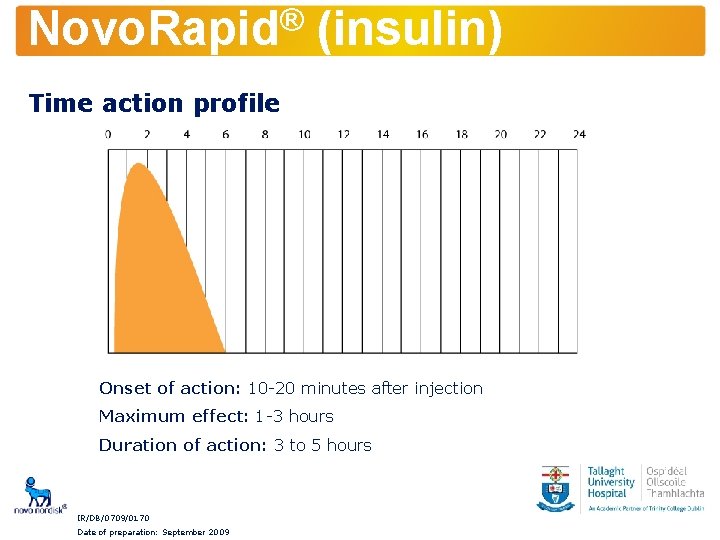
® Novo. Rapid (insulin) Time action profile Onset of action: 10 -20 minutes after injection Maximum effect: 1 -3 hours Duration of action: 3 to 5 hours IR/DB/0709/0170 Date of preparation: September 2009
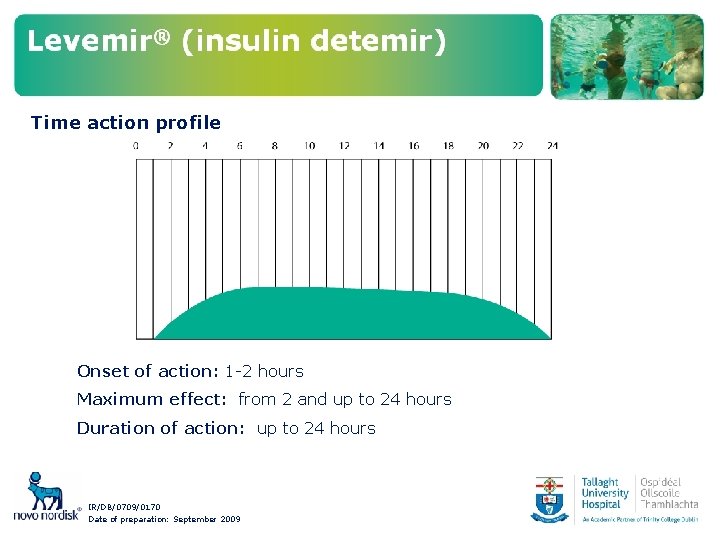
Time action profile Onset of action: 1 -2 hours Maximum effect: from 2 and up to 24 hours Duration of action: up to 24 hours IR/DB/0709/0170 Date of preparation: September 2009

Tresbia
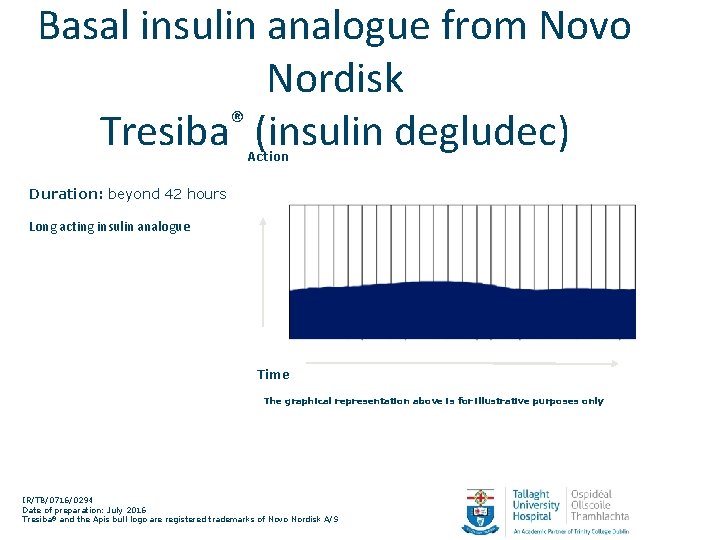
Basal insulin analogue from Novo Nordisk ® Tresiba (insulin degludec) Action Duration: beyond 42 hours Long acting insulin analogue Time The graphical representation above is for illustrative purposes only IR/TB/0716/0294 Date of preparation: July 2016 Tresiba® and the Apis bull logo are registered trademarks of Novo Nordisk A/S Tresiba® Summary of Product Characteristics
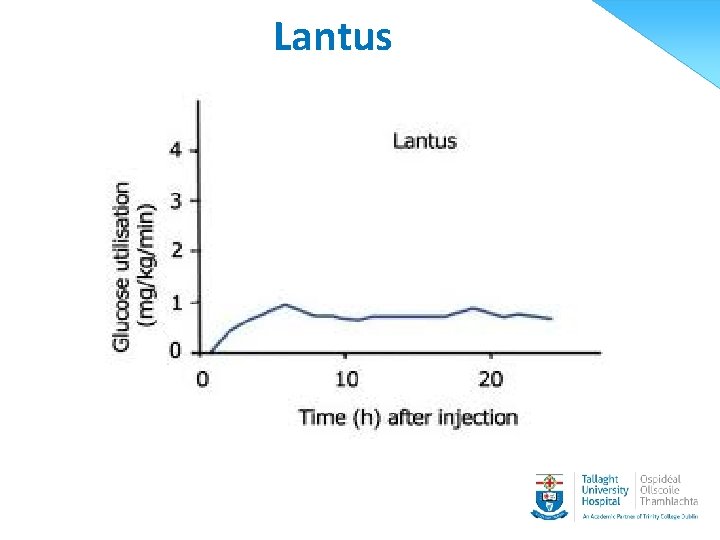
Lantus
Toujeo (Glargine U 300) • • • Specific pen High concentration Third of volume Once daily Same duration of action as lantus (same drug)
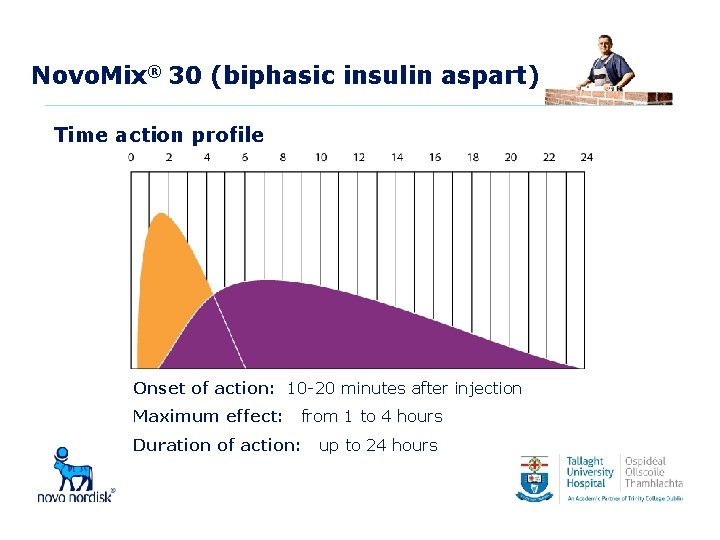
Novo. Mix® 30 (biphasic insulin aspart) Time action profile Onset of action: 10 -20 minutes after injection Maximum effect: from 1 to 4 hours Duration of action: up to 24 hours

Autocover™ designed for safety • Novo. Fine® Autocover™ is a technology-based single use needle • Automatic shield initially covers the needle • Retracts during insulin deposition • Following insulin injection, locks into place covering the needle once again • Prevents any accidental needle puncture wounds and needle reuse.

Injection sites


Overused injection sites
The complications of diabetes
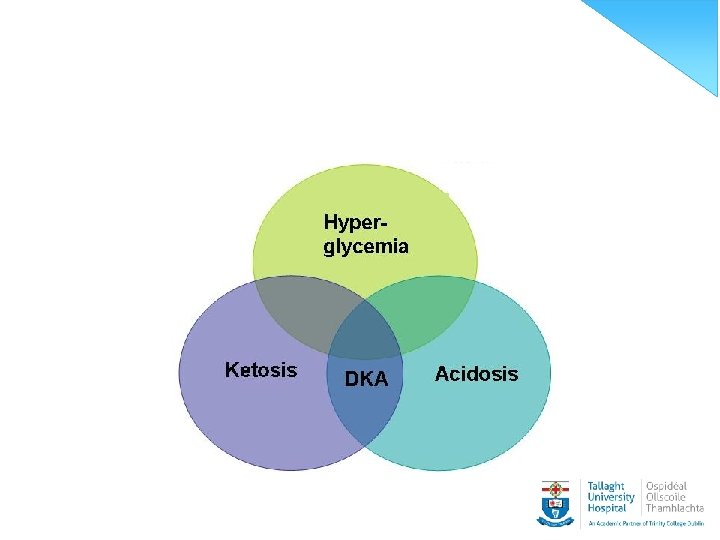
Acute complications of Diabetes • Hypoglycaemia • Hyperglycaemia a. Diabetic Ketone acidosis b. Hyperglycaemic Hyperosmoler State
Hypoglycaemia POSSIBLE CAUSES • Food • Exercise • Alcohol • OHA/Insulin
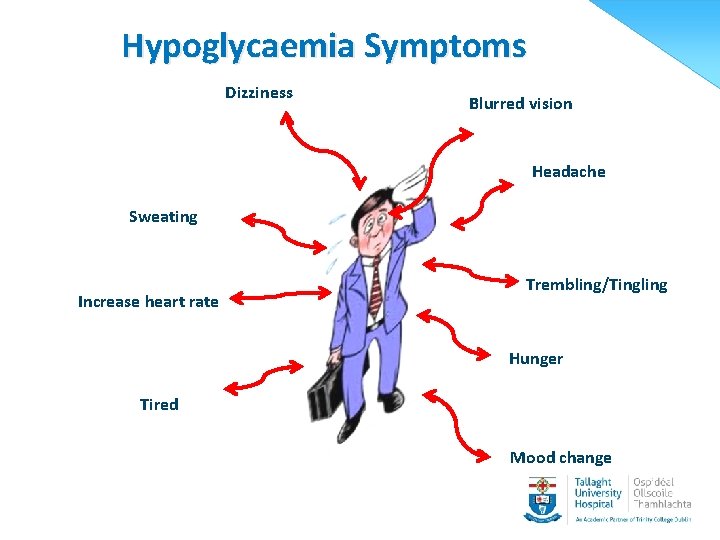
Hypoglycaemia Symptoms Dizziness Blurred vision Headache Sweating Increase heart rate Trembling/Tingling Hunger Tired Mood change
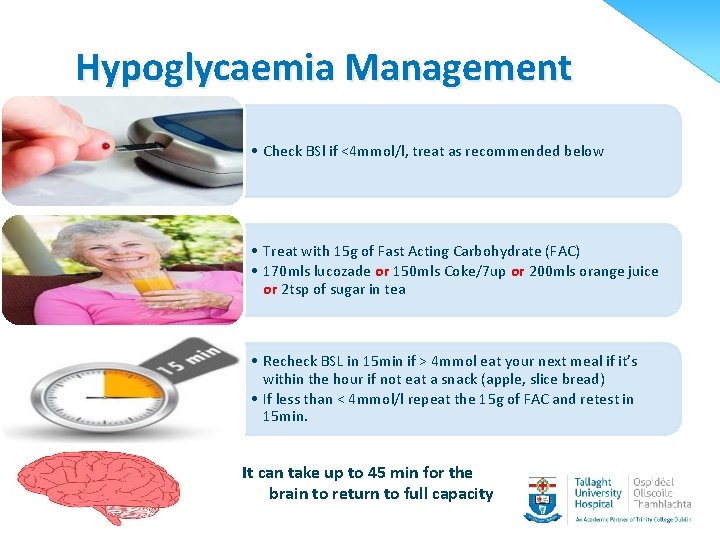
Hypoglycaemia Management • Check BSl if <4 mmol/l, treat as recommended below • Treat with 15 g of Fast Acting Carbohydrate (FAC) • 170 mls lucozade or 150 mls Coke/7 up or 200 mls orange juice or 2 tsp of sugar in tea • Recheck BSL in 15 min if > 4 mmol eat your next meal if it’s within the hour if not eat a snack (apple, slice bread) • If less than < 4 mmol/l repeat the 15 g of FAC and retest in 15 min. It can take up to 45 min for the brain to return to full capacity
![Hypoglycaemia [contd] Signs and symtoms of moderate hypo • Disorientation • Mood change • Hypoglycaemia [contd] Signs and symtoms of moderate hypo • Disorientation • Mood change •](http://slidetodoc.com/presentation_image_h/34e454d25a5cc6e4b1afe60f1e4258df/image-59.jpg)
Hypoglycaemia [contd] Signs and symtoms of moderate hypo • Disorientation • Mood change • Can be mistaken for been drunk. • SEVERE HYPO loss of consciousness
![Hypoglycaemia [contd] Treatment of a severe hypo • Care of unconscious patient • IVI Hypoglycaemia [contd] Treatment of a severe hypo • Care of unconscious patient • IVI](http://slidetodoc.com/presentation_image_h/34e454d25a5cc6e4b1afe60f1e4258df/image-60.jpg)
Hypoglycaemia [contd] Treatment of a severe hypo • Care of unconscious patient • IVI dextrose in hospital situation • Glucagons Hypo kits
Hyperglycaemia • Possible reason for high blood sugar level • Diabetes Ketone Acidosis • Hyperglycaemic Hyperosmolar State • Symptoms • Treatment • Sick day rules
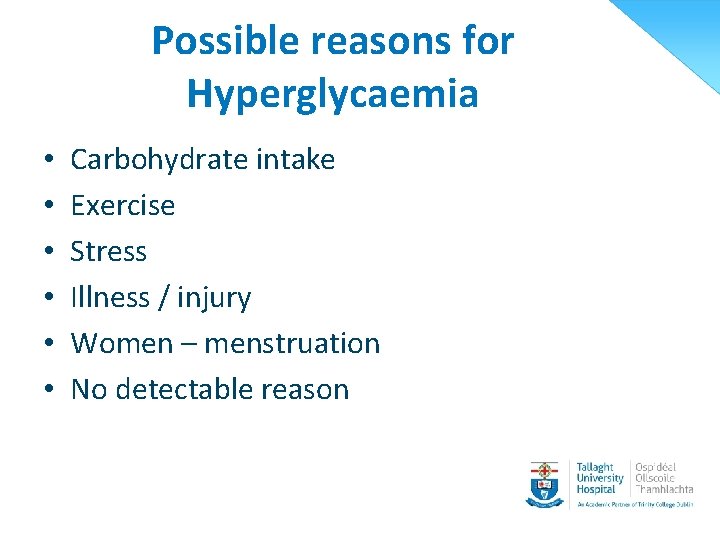
Possible reasons for Hyperglycaemia • • • Carbohydrate intake Exercise Stress Illness / injury Women – menstruation No detectable reason
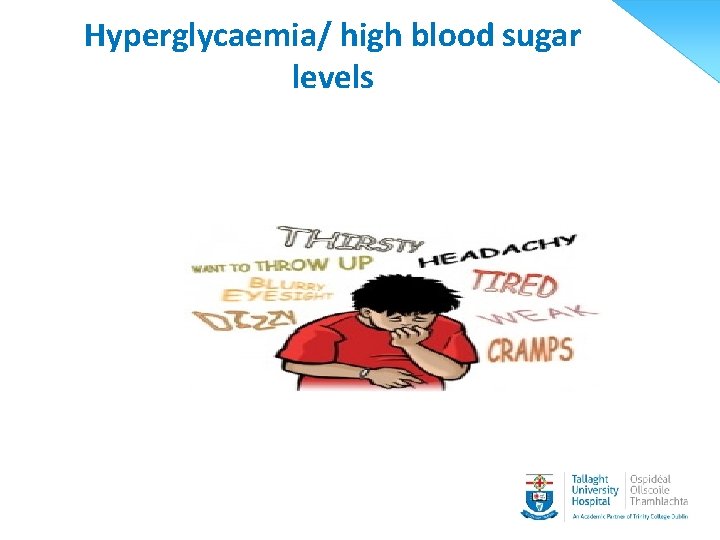
Hyperglycaemia/ high blood sugar levels
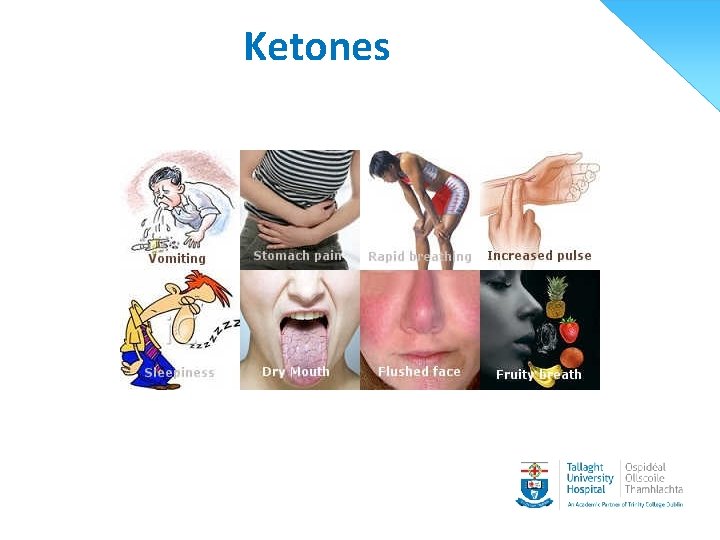
Ketones
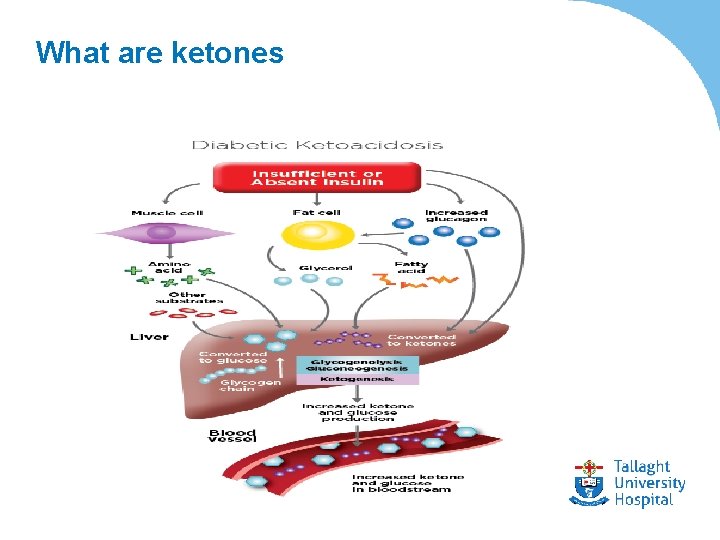
What are ketones
Sick day rules • • • Test blood sugars more frequently Drink plenty of fluids Eat regular food if able [or replacement food] Get plenty of rest Strong possibility diabetes medication will need to be increased
![Sick days rules [contd] When to seek assistance • Persistent high blood sugars • Sick days rules [contd] When to seek assistance • Persistent high blood sugars •](http://slidetodoc.com/presentation_image_h/34e454d25a5cc6e4b1afe60f1e4258df/image-68.jpg)
Sick days rules [contd] When to seek assistance • Persistent high blood sugars • Vomiting or diarrhoea more than once • Only tolerating fluids for more than 24 hrs • Not fully better within 3 days • Infection/injury etc. • The presents of KETONES (Type 1 Diabetes)
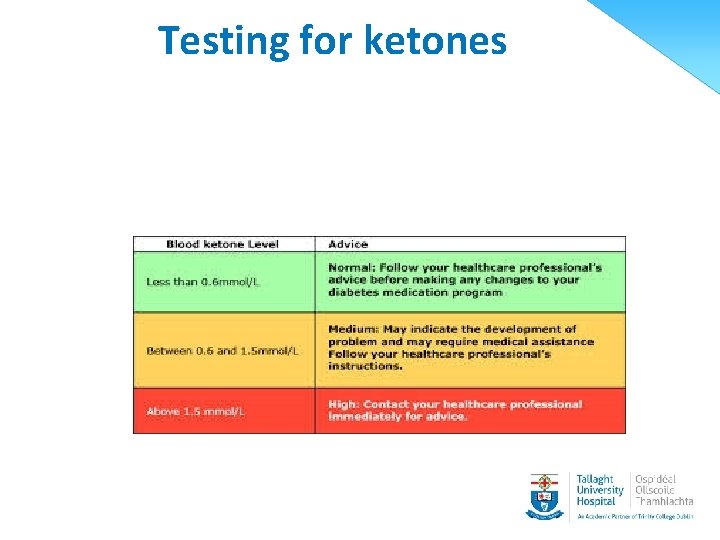
Testing for ketones
Treatment for ketones
Treatment of DKA

Hyperglycaemic Hyperosmolar State (HHS) • Decrease in plasma insulin leading to increase plasma sugar • BUT there is enough insulin to prevent lipolysis • Increased osmotic diuresis
HHS • • • Rare New onset Incurrent illness History hyperglycaemic symptoms by weeks Dehydration Confusion /seizures
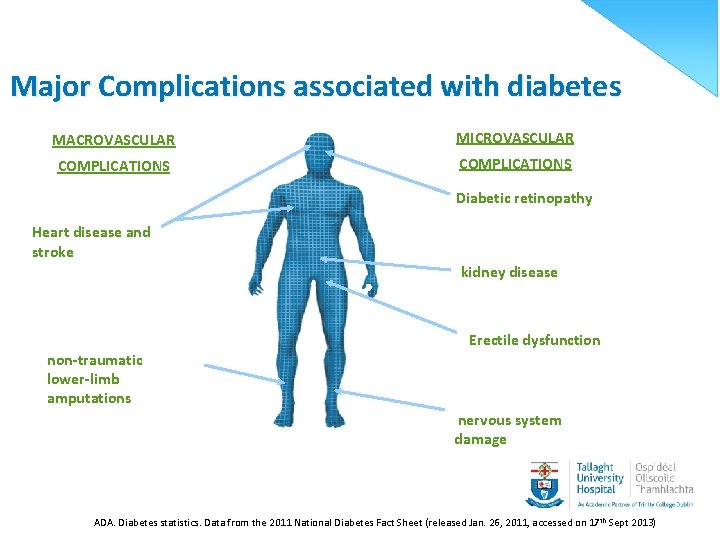
Major Complications associated with diabetes MACROVASCULAR MICROVASCULAR COMPLICATIONS Diabetic retinopathy Heart disease and stroke kidney disease non-traumatic lower-limb amputations Erectile dysfunction nervous system damage ADA. Diabetes statistics. Data from the 2011 National Diabetes Fact Sheet (released Jan. 26, 2011, accessed on 17 th Sept 2013)
Chronic complications of Diabetes OUR GOAL – to prevent complication where possible • Glycaemic control – within normal levels • Blood pressure control 130/70 • Lipid control • Screening
Diabetes Support Team Ophthalmologist G. P. Doctor Nurse Dietician Podiatrist
Thank you
- Slides: 77