Devolution Health Creation Greater Manchester Health Social Care




- Slides: 21
Devolution Health Creation: Greater Manchester Health & Social Care Partnership Warren Heppolette, Executive Lead – Strategy and System Development

INRODUCTION Greater Manchester Health and Social Care Partnership BACKGROUND 1. GM HISTORY 2. HEALTH DEVOLUTION PRINCPLES & OBJECTIVES 3. TRANSFORMATION THEMES 4. GOVERNANCE 5. SYSTEM ARCHITECTURE
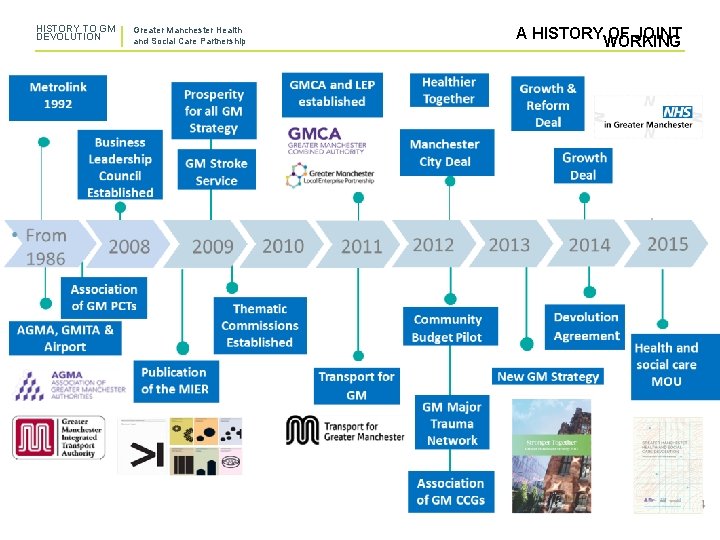
HISTORY TO GM DEVOLUTION Greater Manchester Health and Social Care Partnership BACKGROUND • • A longstanding history of local government collaboration in GM dating back to 1986 and leading major developments (Metrolink, Manchester Airport Group etc). GM, therefore, at the forefront of English Devolution for a number of years A significant history of collaboration in the GM NHS (Making it Better, Hyper Acute Stroke, Major Trauma developments) Manchester Independent Economic Review confirming the relationship between health and GM’s economic potential in 2009 The Community Budget pilot from 2011 -12 began to bring these elements together and inform principles and objectives of comprehensive public service reform. The 2014 devolution agreement significantly extended the responsibilities of the GM Combined Authority and established the role of the GM Mayor The same agreement invited consideration of the potential for health and social care devolution An Memorandum of Understanding was signed in February 2015 to establish a delegated arrangement between NHS England GM which was enacted from April 2016 following agreement of: Ø A 5 year strategy for clinical and financial sustainability – “Taking Charge” Ø An Accountability Agreement – containing the commitments to the NHS Constitution Ø A Delegation Agreement – Confirming the delegations from NHSE to the GM
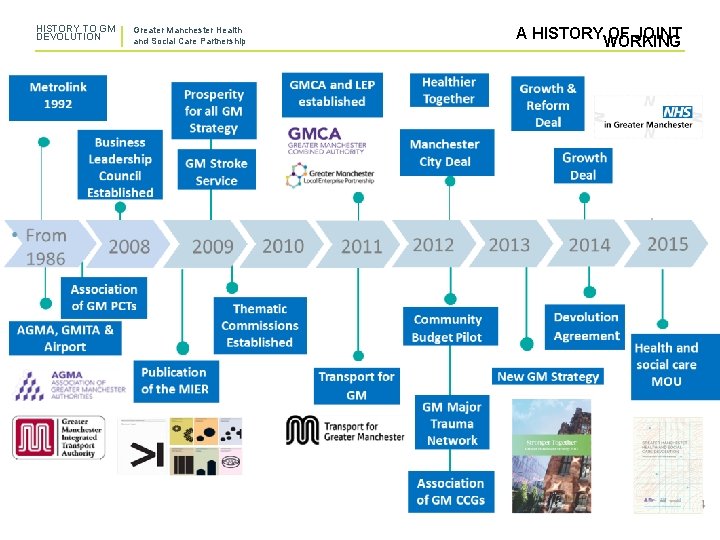
HISTORY TO GM DEVOLUTION Greater Manchester Health and Social Care Partnership A HISTORYWORKING OF JOINT
PRINCIPLES & OBJECTIVES Greater Manchester Health and Social Care Partnership HEALTH DEVOLUTION PRINCIPLES • GM will still remain part of the National (EXTRACT) • • • Health Service and social care system, uphold the national standards Decisions will be focussed on the interests and outcomes of patients and people in Greater Manchester, and organisations will collaborate to prioritise those interests; In creating new models of inclusive governance and decision-making, GM commissioners, providers, patients, carers and partners will shape the future of GM together Commissioning for health and social care will be undertaken at a GM level where the GM place-based approach is optimum for its residents, rather than at a regional or national level A principle of subsidiarity will apply within GM, ensuring that decisions are made at the most appropriate level • • Decision making will be underpinned by transparency and the open sharing of information There will continue to be clear accountability arrangements for services and public expenditure The delivery of shared outcomes will drive changes to organisational form where necessary We commit to the production, during 2015/16, of a comprehensive GM Strategic Sustainability Plan for health and social care. We will aim to address any funding inequalities for the benefit of all residents in GM; A radical approach will be taken to optimising the use of NHS and social care estates
PRINCIPLES & OBJECTIVES Greater Manchester Health and Social Care Partnership HEALTH DEVOLUTION OBJECTIVES • • • To improve the health and wellbeing of all of the residents of Greater Manchester (GM) from early age to the elderly, recognising that this will only be achieved with a focus on prevention of ill health and the promotion of wellbeing. We want to move from having some of the worst health outcomes to having some of the best; To close the health inequalities gap within GM and between GM and the rest of the UK faster; To deliver effective integrated health and social care across GM; • • • To deliver effective integrated health and social care across GM; To continue to redress the balance of care to move it closer to home where possible; To strengthen the focus on wellbeing, including greater focus on prevention and public health; To contribute to growth and to connect people to growth, e. g. supporting employment and early years services; and To forge a partnership between the NHS, social care, universities and science and knowledge industries for the benefit of the population.
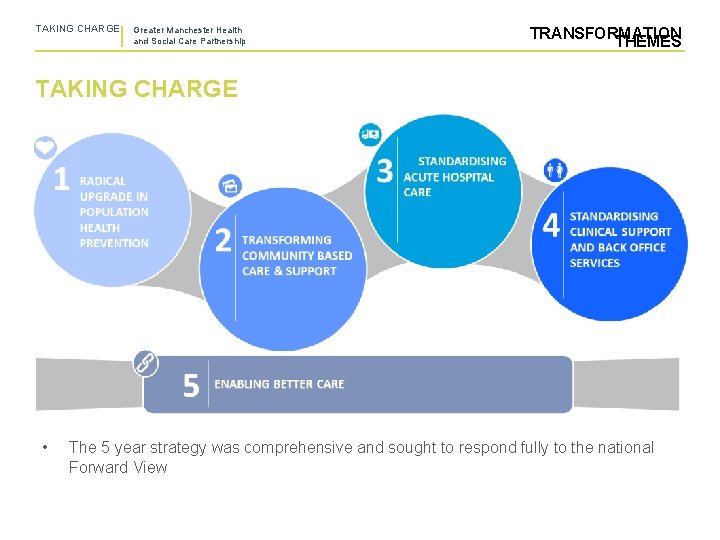
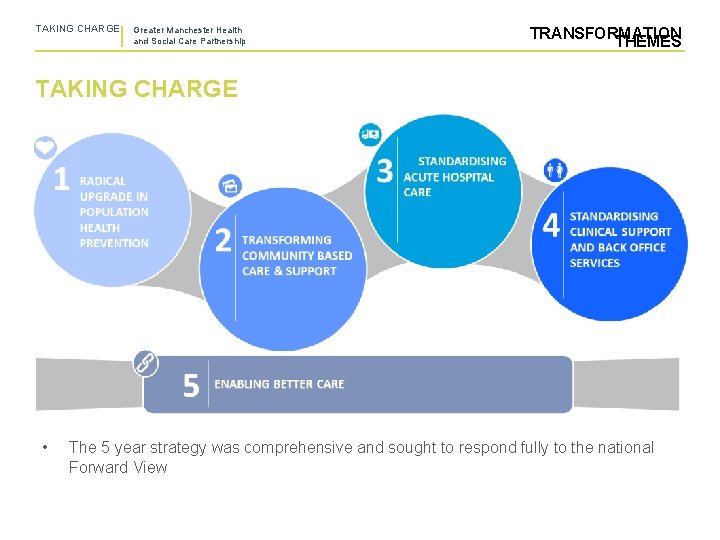
TAKING CHARGE Greater Manchester Health and Social Care Partnership TRANSFORMATION THEMES TAKING CHARGE • The 5 year strategy was comprehensive and sought to respond fully to the national Forward View
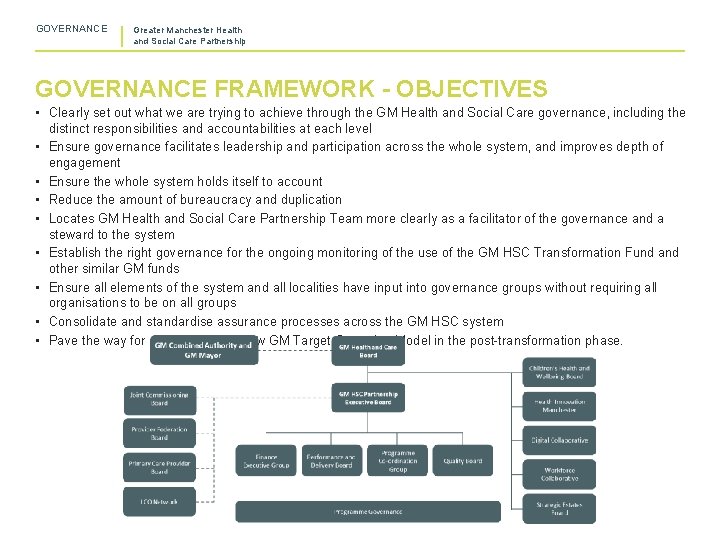
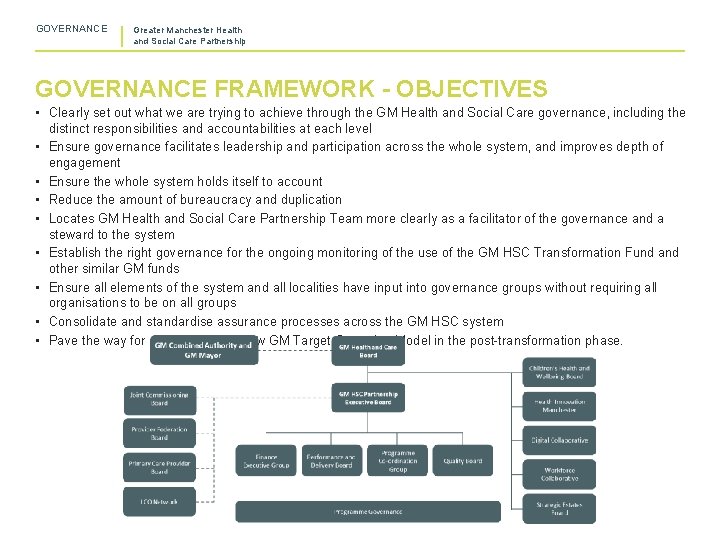
GOVERNANCE Greater Manchester Health and Social Care Partnership GOVERNANCE FRAMEWORK - OBJECTIVES • Clearly set out what we are trying to achieve through the GM Health and Social Care governance, including the distinct responsibilities and accountabilities at each level • Ensure governance facilitates leadership and participation across the whole system, and improves depth of engagement • Ensure the whole system holds itself to account • Reduce the amount of bureaucracy and duplication • Locates GM Health and Social Care Partnership Team more clearly as a facilitator of the governance and a steward to the system • Establish the right governance for the ongoing monitoring of the use of the GM HSC Transformation Fund and other similar GM funds • Ensure all elements of the system and all localities have input into governance groups without requiring all organisations to be on all groups • Consolidate and standardise assurance processes across the GM HSC system • Pave the way for development of new GM Target Operating Model in the post-transformation phase.
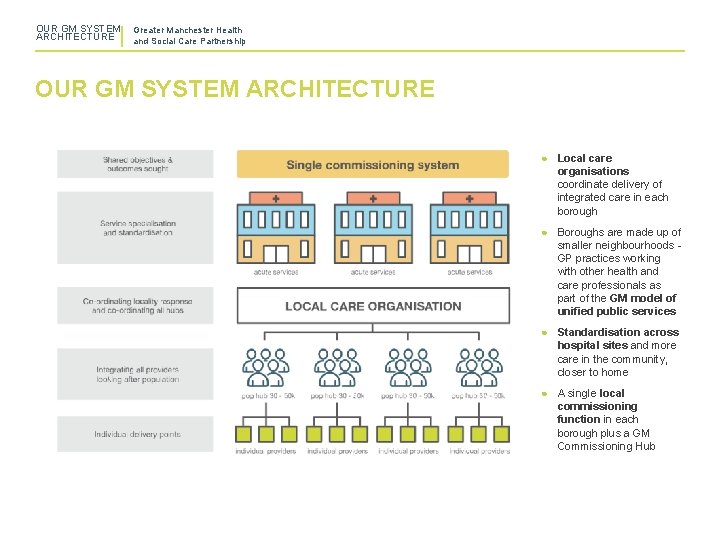
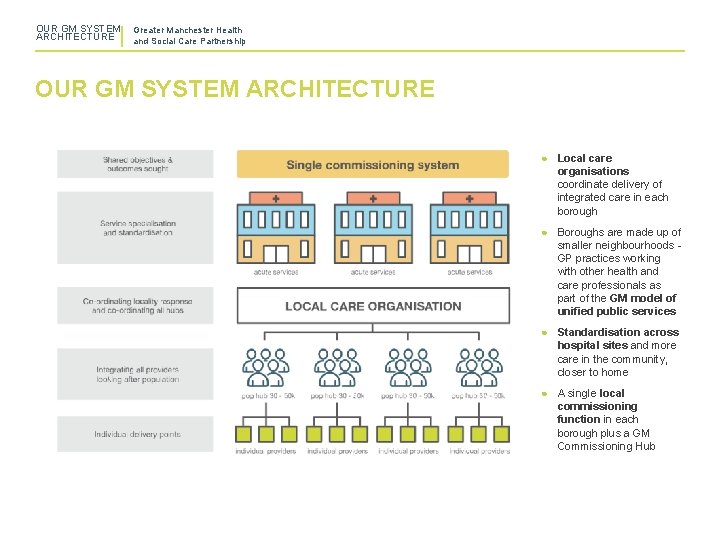
OUR GM SYSTEM ARCHITECTURE Greater Manchester Health and Social Care Partnership OUR GM SYSTEM ARCHITECTURE ● Local care organisations coordinate delivery of integrated care in each borough ● Boroughs are made up of smaller neighbourhoods GP practices working with other health and care professionals as part of the GM model of unified public services ● Standardisation across hospital sites and more care in the community, closer to home ● A single local commissioning function in each borough plus a GM Commissioning Hub
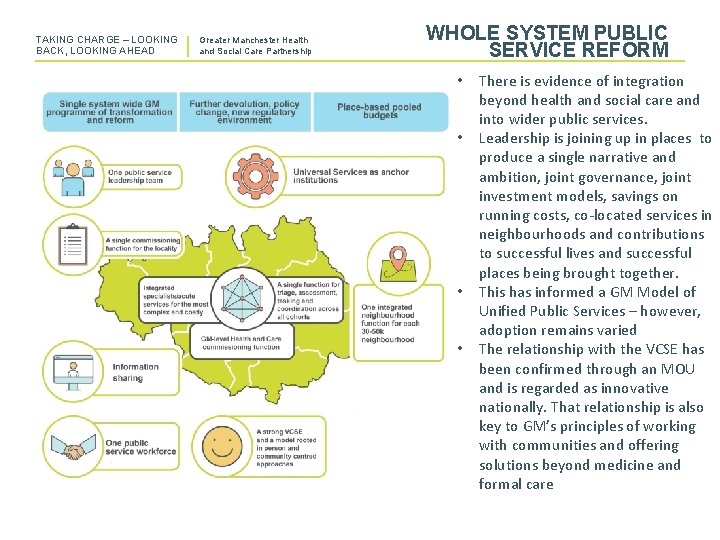
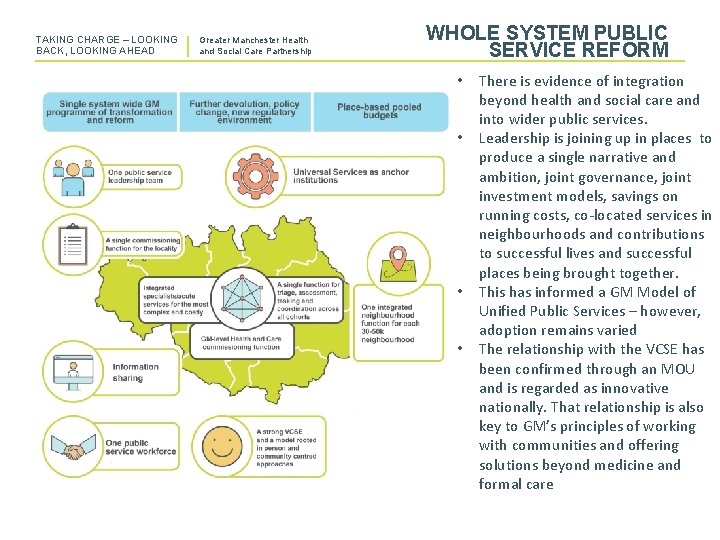
TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership WHOLE SYSTEM PUBLIC SERVICE REFORM • • 10 There is evidence of integration beyond health and social care and into wider public services. Leadership is joining up in places to produce a single narrative and ambition, joint governance, joint investment models, savings on running costs, co-located services in neighbourhoods and contributions to successful lives and successful places being brought together. This has informed a GM Model of Unified Public Services – however, adoption remains varied The relationship with the VCSE has been confirmed through an MOU and is regarded as innovative nationally. That relationship is also key to GM’s principles of working with communities and offering solutions beyond medicine and formal care
EFFECTS TO DATE Greater Manchester Health and Social Care Partnership ACHIEVEMENTS & CHALLENGES 1. EVALUATION FRAMEWORK 2. ACHIEVEMENTS TO DATE 3. PERSISTENT CHALLENGES
TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership EVALUATION THE EVALUATION • PROGRAMME… We should recognise that the lessons from GM as a first 5 year programme will need to wait to some degree, for the formal evaluation. This process is underway and brings together: Ø Ø Ø A series of longitudinal evaluations of the GM Strategic Plan examining a number of key themes – with a focus on the 10 localities within GM The locality evaluations will cover a three year period in the first instance. This time period may be extended so that we capture some of the longer-term outcomes – for example, in population health Evaluations will be both formative and summative in nature. Whilst the evaluation is in progress, the evaluators will be expected to capture examples of best practice that have the potential to be scaled across GM – to inform the ongoing transformation programme. The evaluation programme will cover both locality and GM-level and will have quantitative and qualitative elements to enable evaluation of “how transformation plans were designed and implemented, what effects they have for whom, how and why” There are likely to be a range of evaluators within the programme – given the scale and complexity of GM. Effective co-ordination will be needed. HOWEVER, AHEAD OF THAT PROCESS… • There are measurable effects which give us an indication of where we are making progress and where we are not • This is part of ongoing monitoring against those indicators the range of programmes and approaches were targeted to affect
TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership BUILDING A SUSTAINABLE HEALTH & CARE SYSTEM SOME ACHIEVEMENTS… • • • We have narrowed the gap to the rest of England in respect of smoking. Two years into our Making Smoking History programme we are on track to reach our target, with smoking prevalence falling twice as fast as the national average, to a record low of 16. 2%. This means there are roughly 46, 500 fewer smokers in Greater Manchester now than there were in 2016; School readiness - we have now closed the gap on the England average from 4. 8% to 3. 5%: our aim is to match it by 2021; We have significantly improved cancer survival rates so that they now almost reach the national average in Greater Manchester; Our Working Well Early Help assists people at risk of falling out of employment, or who are newly unemployed, because of their health. In its first six months the Working Well Early Help service helped 349 people and of those 73% were given support and 27% were provided with advice. 20, 000 people have been helped back towards work via the broader Working Well programme since 2014. We are on track to achieve our target of 75% of people being active or fairly active by 2025. We have started to see rates of physical activity rise, narrowing the gap between GM and England (by 1. 2 percentage points). We expect this improvement to accelerate as Greater Manchester Moving: The Plan for Physical Activity and Sport 2017– 21 is implemented. Through a concerted system-wide improvement in the safety of maternity services, an average of an extra 23 babies are being born alive and well each year in Greater
TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership BUILDING A SUSTAINABLE HEALTH & CARE SYSTEM SOME MORE… • • An additional 250 smoke free babies were born in the first year of our programme to reduce smoking during pregnancy. We have reduced the proportion of new mothers who smoke from 12. 8% to 11. 7% - closing our gap with the England average rate from 1. 8% to 0. 8%. The number of people admitted to hospital for alcohol-related conditions in GM has dropped to close to the national average. During 2016/17, there were 679 admissions per 100, 000 of our population compared to 636 for England as a whole – a gap of 43, down from 60 in 2015/16; 100% of GM’s residents can get routine or pre-booked appointments with their GP practice seven days a week (up from 47% in 2016); Over 96% of Greater Manchester GP practices are rated good or outstanding by the Care Quality Commission (CQC) - above the national average; Our GP Excellence academy, partnering with the RCGP, is supporting the improvement of practices and PCNs. The proportion of care home beds and domiciliary care agencies in GM rated good or outstanding by the CQC has improved: this rose from 47% and 63% respectively in 2016 to 66% and 85% in 2019; We have ended each of the three full years of health devolution with a financial surplus– this has supported the national NHS financial position.

TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership BUILDING A SUSTAINABLE HEALTH & CARE SYSTEM KEY CHALLENGES… • We have not secured reliable delivery of NHS Constitutional Standards – The GM system hasn't managed to reduce the overall demand on urgent care which is reflected in the 4 hour target performance and rising pressure on front line services • We still have too much variation in progress of localities in reducing demand for acute services • There is insufficient workforce capacity in some key areas • There also variation in the development and maturity of Local Care Organisations, a key part of our overall system architecture • The absence of a stable long term financial settlement for social care remains a source of significant pressure across the system

KEY LEARNIJNG Greater Manchester Health and Social Care Partnership LEARNING & REFLECTIONS 1. REFLECTIONS ON GOVERNANCE 2. REFLECTIONS ON IMPROVEMENT APPROACHES 3. THE PARALLELS WITH ICSs 4. LOOKING FORWARD
TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership KEY LEARNING GOVERNANCE PLANNING & ASSURANCE… ü Clear Governance, understood by all partners, enabling decisions to be taken at scale – eg Joint Commissioning Board ü Track record in managing transformation funding deployment, utilising a tested cost benefit methodology ü Track record in delivering system control total through early reporting and collaboration ü GM coordination of planning responses, including activity and finance. ü Contract deals managed within GM without recourse to national support or arbitration ü GM undertakes CCG assurance and regulation, on behalf of NHS England, through a place-based approach ü GM Performance & Delivery Group manages system level exceptions on a monthly basis HOWEVER… • The ‘regulatory’ delegation has only applied to NHS commissioners (CCGs) and not to providers • There is a reflection that statutory regulatory functions cannot easily be part of a Partnership
TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership KEY LEARNING IMPROVEMENT & TRANSFORMATION… ü ü ü ü ü Single agreed neighbourhood model of care, deployed by localities in a way that reflects local circumstances Increased flexibility emerging over the use of resources and stronger tie in to other public services, such as employment support, housing strategies Business Intelligence tool (Tableau) deployed across GM for comparison of primary, social care and NHS performance indicators Establishment of Health Innovation Manchester to pull innovations through from discovery to develop at scale across all 10 localities Support for peer learning – eg Commissioning Review, LCO network Peer-led improvement – eg care homes quality Improvement Collaboratives – pressure ulcers Distributed leadership in GM for key improvement priorities, eg Cancer, Elective Care, Urgent & Emergency Care Agreement of standards at GM level, with clear governance for locality oversight (eg discharge standards led by UECB & overseen by locality UECBs) Transformation projects at GM where this adds value over local work (eg Clinical Assessment Service for Urgent Care, reduction in acute mental health out of area placements) HOWEVER… • • Progress against the agreed model is varied and takes time and trust to build • Choosing the right things to do at the right level is a constant challenge There is a strong sense that we have too many priorities and are spreading the focus of our collective work too thinly • Consequently, genuine ownership of the GM project isn’t as deeply shared as it needs to be

TAKING CHARGE – LOOKING BACK, LOOKING AHEAD Greater Manchester Health and Social Care Partnership ICS PARALLELS NATIONAL INTENTIONS FOR ICSs DRAW MUCH FROM GM’s EXPERIENCE… It is important to avoid seeing GM health devolution as an isolated experiment and recognise the similarities NHSEI envisage for mature ICSs. Two roles envisaged for ICSs: 1. System transformation – deliver a co-ordinated programme of transformational change, to secure the long-term sustainability of the system, ensure local delivery of the LTP and delivery of plans agreed collectively for the population. 2. Management of system performance – together ICS partners work to improve operational performance of the system, and hold each other to account; supported by appropriate governance However, it is also important to recognise the relative narrowness of ICSs in comparison to GM - a whole public service Partnership within a devolved city region. The route to complementary contributions to health creation across the whole of local government, police, fire, economic development, education, skills and housing is being progressed in GM.
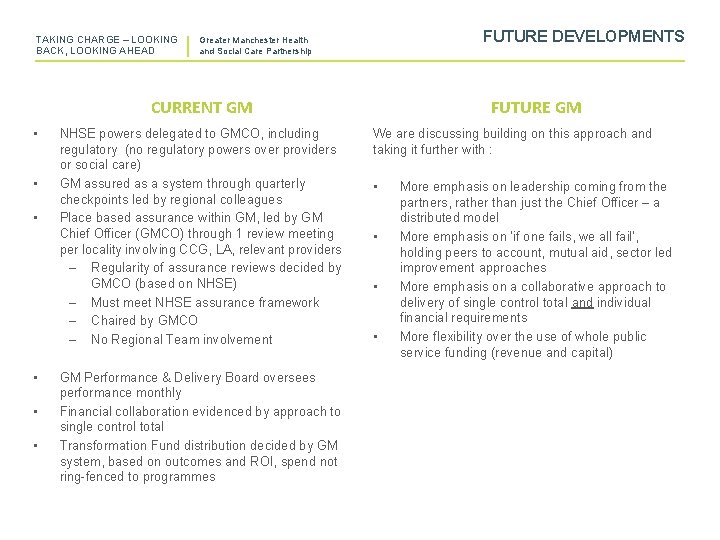
TAKING CHARGE – LOOKING BACK, LOOKING AHEAD FUTURE DEVELOPMENTS Greater Manchester Health and Social Care Partnership CURRENT GM • • • NHSE powers delegated to GMCO, including regulatory (no regulatory powers over providers or social care) GM assured as a system through quarterly checkpoints led by regional colleagues Place based assurance within GM, led by GM Chief Officer (GMCO) through 1 review meeting per locality involving CCG, LA, relevant providers – Regularity of assurance reviews decided by GMCO (based on NHSE) – Must meet NHSE assurance framework – Chaired by GMCO – No Regional Team involvement GM Performance & Delivery Board oversees performance monthly Financial collaboration evidenced by approach to single control total Transformation Fund distribution decided by GM system, based on outcomes and ROI, spend not ring-fenced to programmes FUTURE GM We are discussing building on this approach and taking it further with : • • More emphasis on leadership coming from the partners, rather than just the Chief Officer – a distributed model More emphasis on ‘if one fails, we all fail’, holding peers to account, mutual aid, sector led improvement approaches More emphasis on a collaborative approach to delivery of single control total and individual financial requirements More flexibility over the use of whole public service funding (revenue and capital)
Greater Manchester Health and Social Care Partnership Contact us If you have any queries about these guidelines, contact the GMHSC communications team: gm. hsccomms@nhs. net www. gmhsc. org. uk @GM_HSC
 Greater manchester health and social care partnership
Greater manchester health and social care partnership Integral manchester encoding
Integral manchester encoding Strategic planning workshop greater manchester
Strategic planning workshop greater manchester Greater manchester good employment charter
Greater manchester good employment charter Greater manchester ageing hub
Greater manchester ageing hub Catholic social teaching care for god's creation
Catholic social teaching care for god's creation Health and social care values unit 2
Health and social care values unit 2 Is balkanization devolution
Is balkanization devolution Ethnocultural devolution examples
Ethnocultural devolution examples Democratization definition ap human geography
Democratization definition ap human geography Devolution aphg
Devolution aphg Devolution ap gov
Devolution ap gov Cornwall devolution deal
Cornwall devolution deal Health and social component 3
Health and social component 3 Primary secondary tertiary care nursing
Primary secondary tertiary care nursing Step into care
Step into care Health and social care level 3 unit 6
Health and social care level 3 unit 6 Unit 2 health and social care
Unit 2 health and social care Health and social care unit 2
Health and social care unit 2 Unit 14 health and social care example
Unit 14 health and social care example Wholly nutritious btec business
Wholly nutritious btec business Ocr health and social care level 2
Ocr health and social care level 2