Development of the gonads The indifferent gonads Genital

- Slides: 69
Development of the gonads
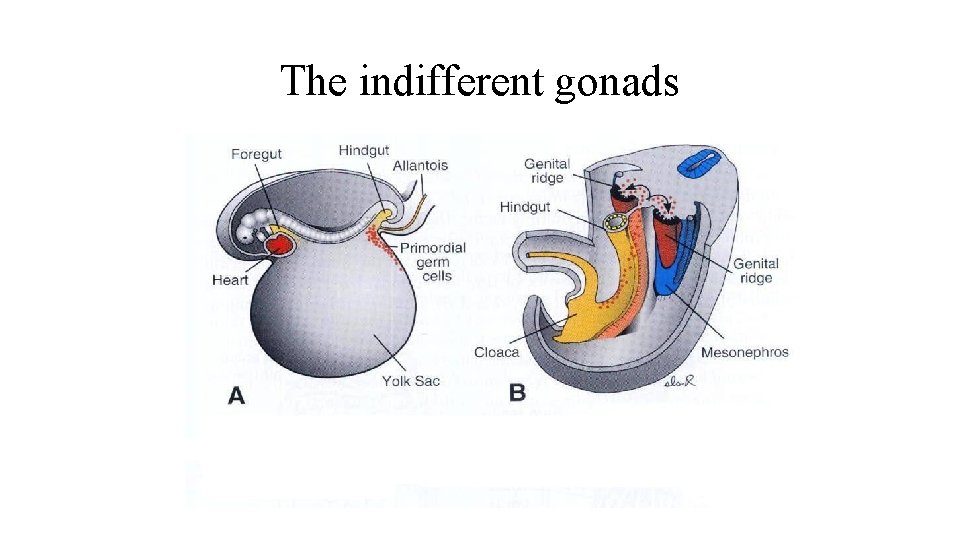
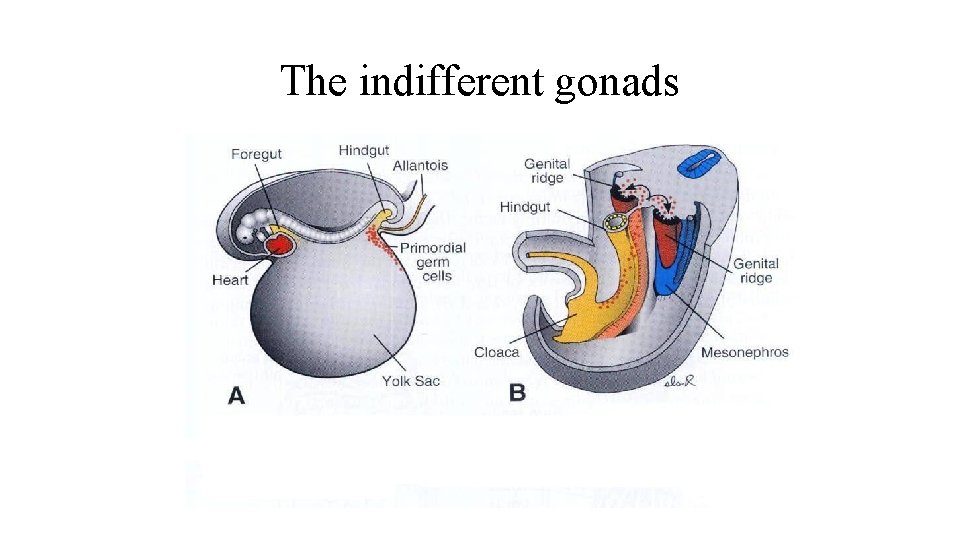
The indifferent gonads
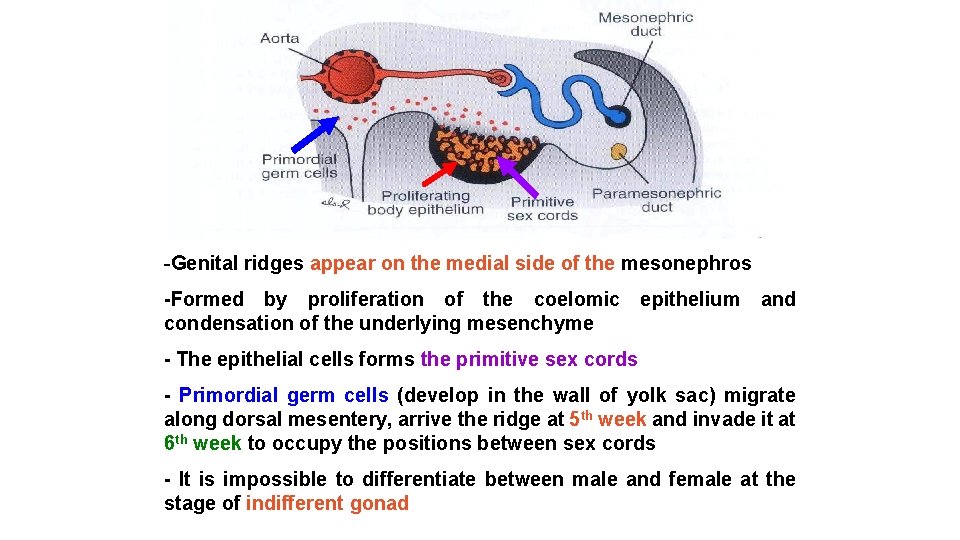
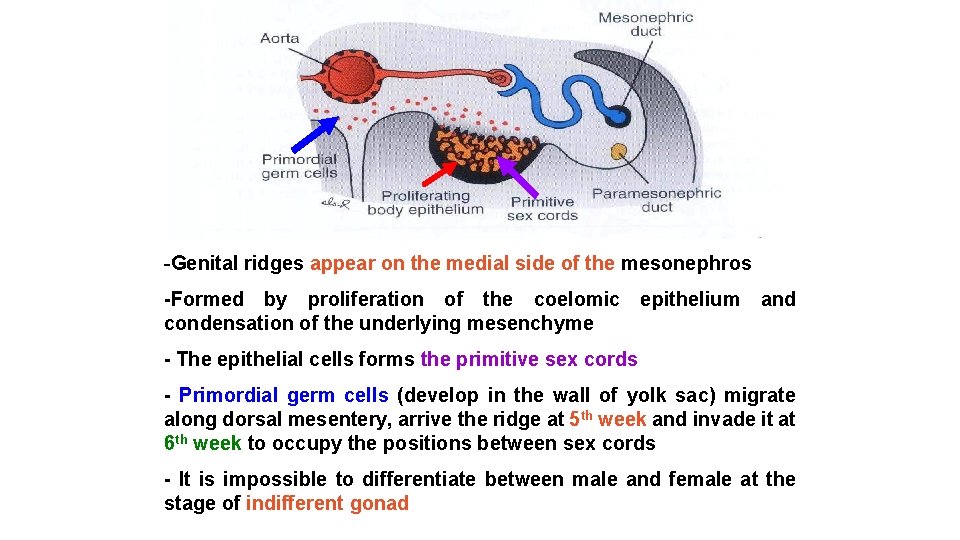
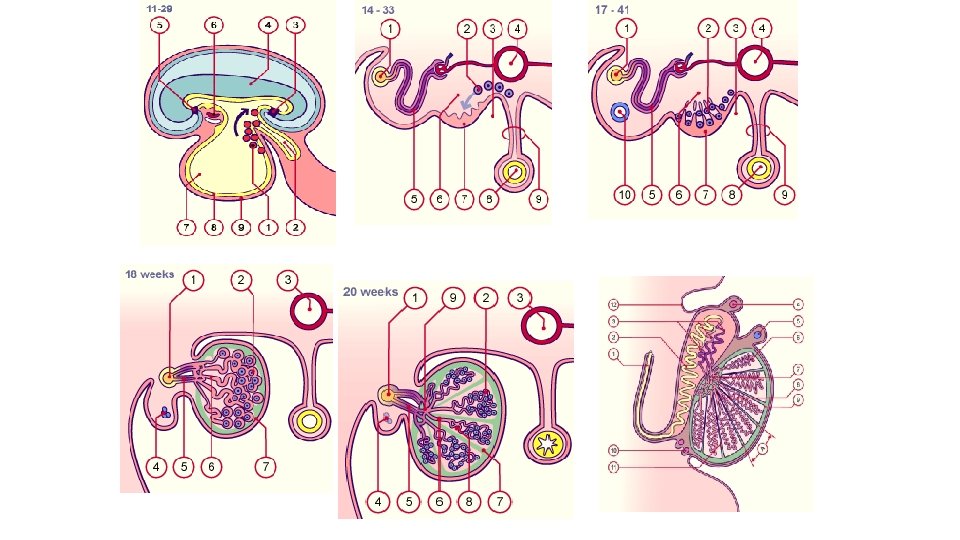
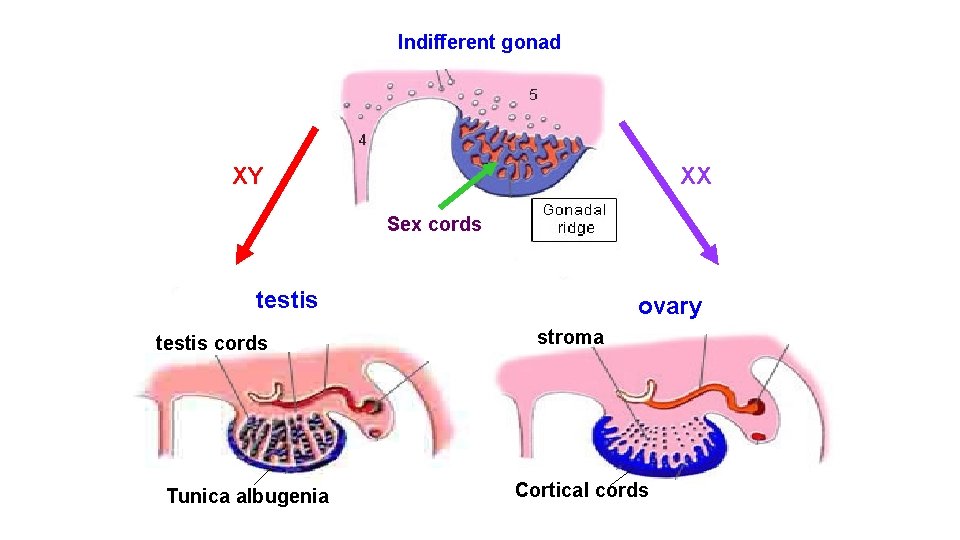
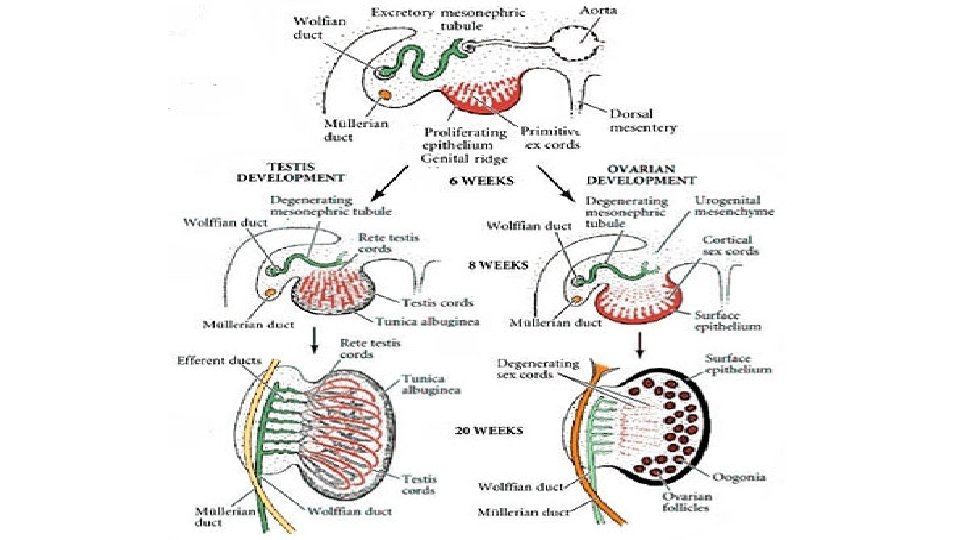
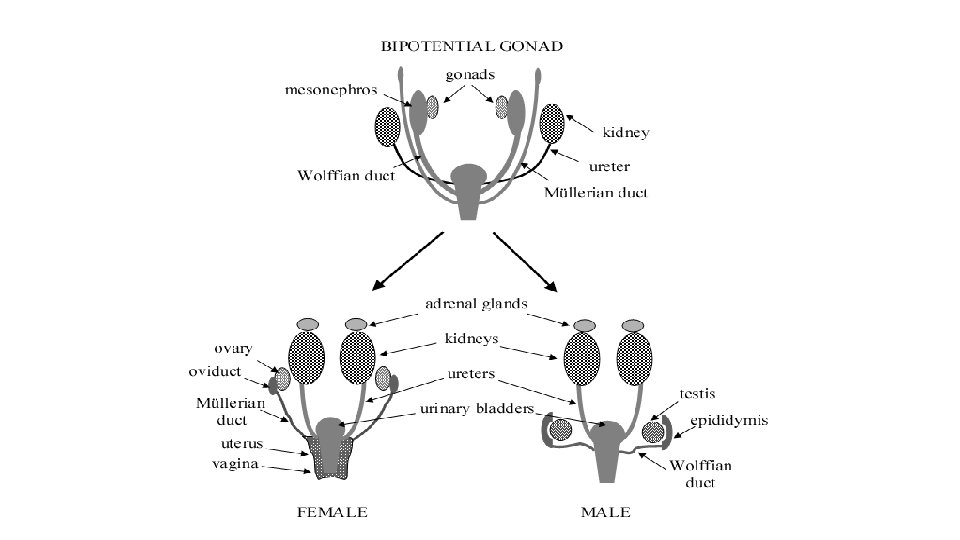
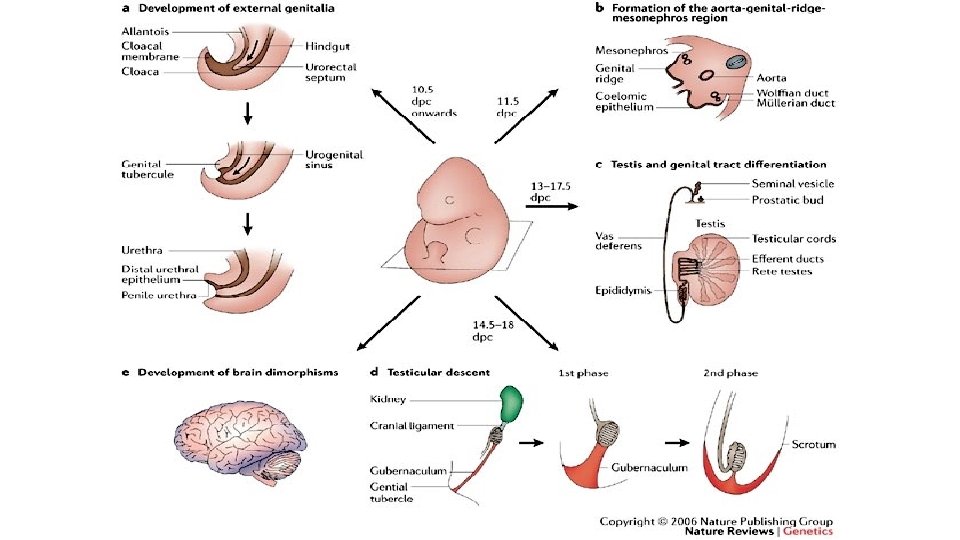
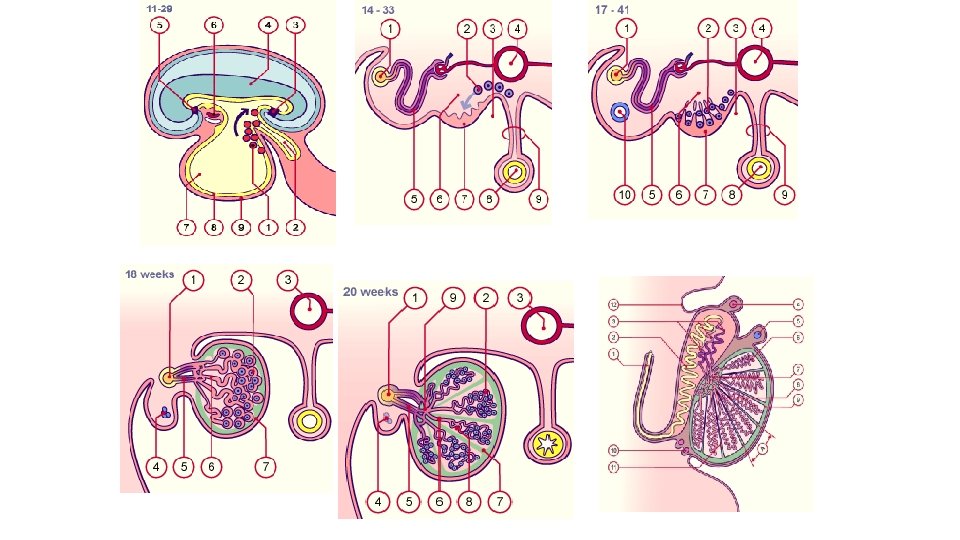
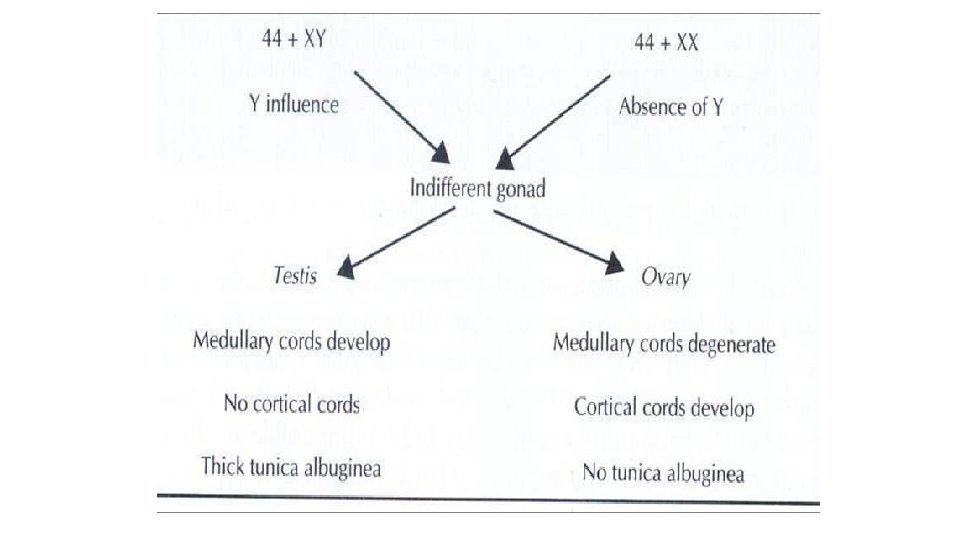
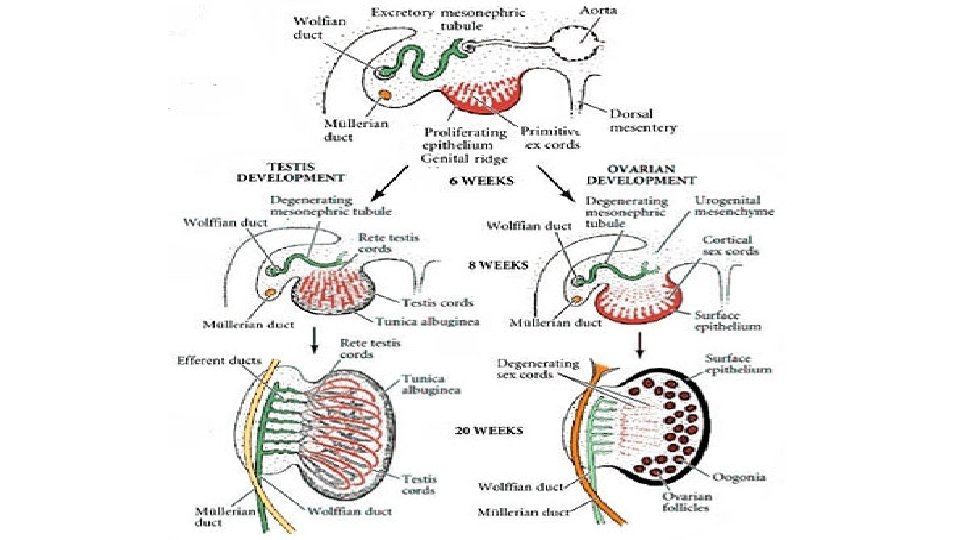
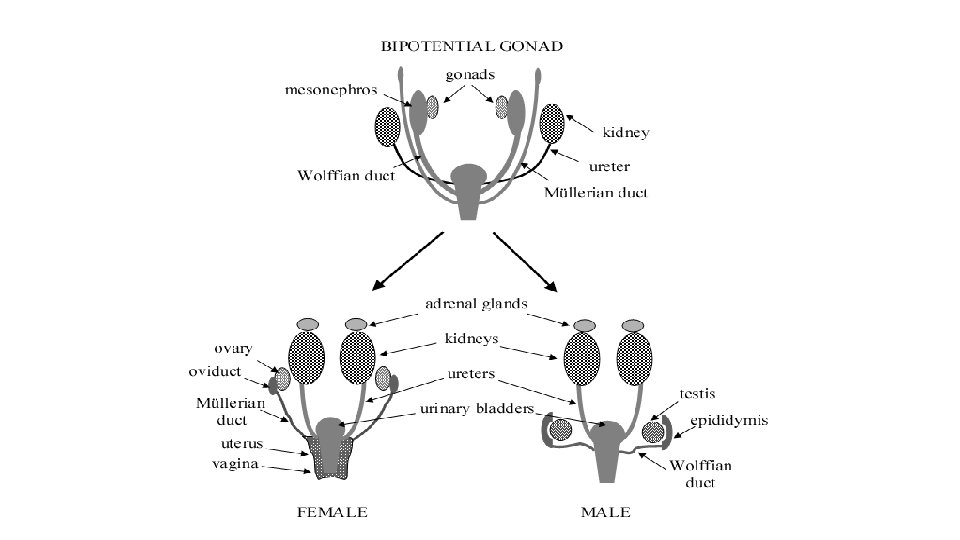
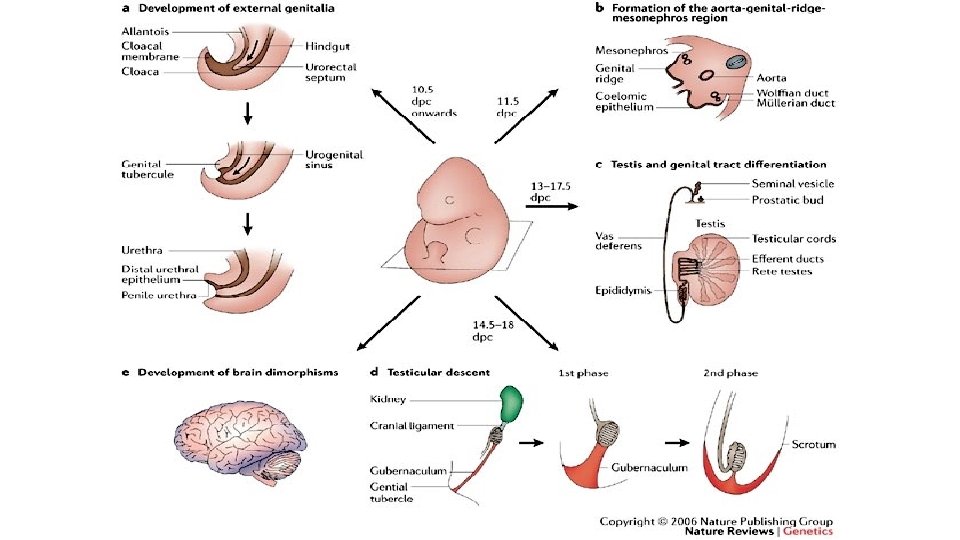
-Genital ridges appear on the medial side of the mesonephros -Formed by proliferation of the coelomic condensation of the underlying mesenchyme epithelium and - The epithelial cells forms the primitive sex cords - Primordial germ cells (develop in the wall of yolk sac) migrate along dorsal mesentery, arrive the ridge at 5 th week and invade it at 6 th week to occupy the positions between sex cords - It is impossible to differentiate between male and female at the stage of indifferent gonad
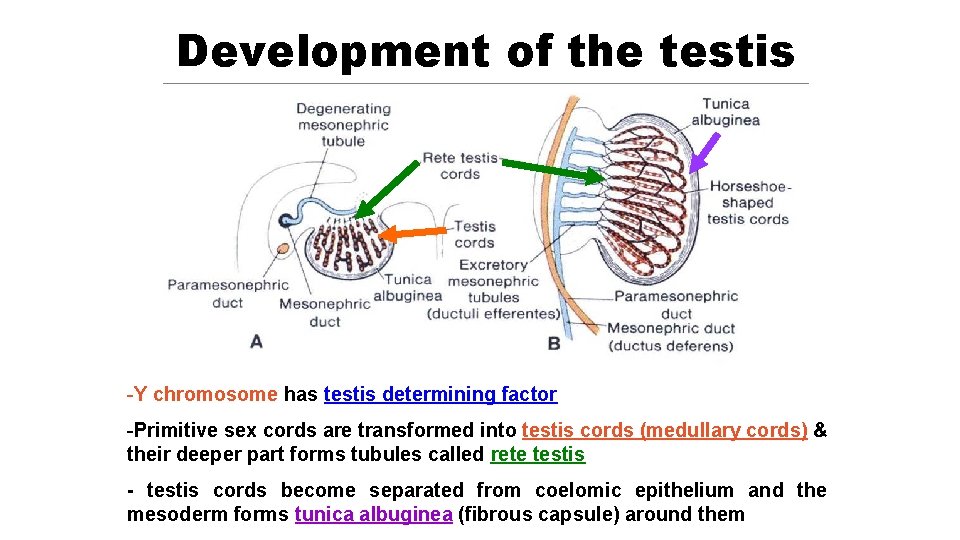
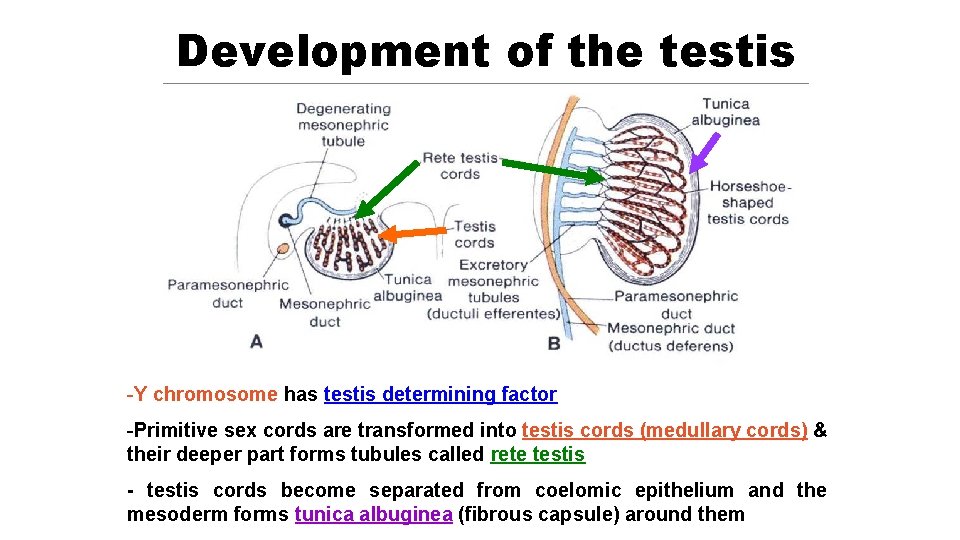
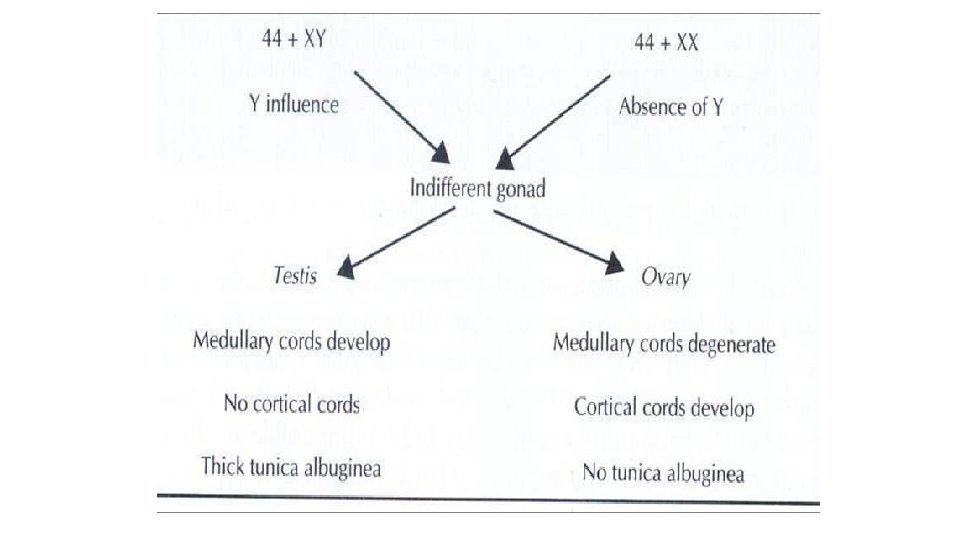
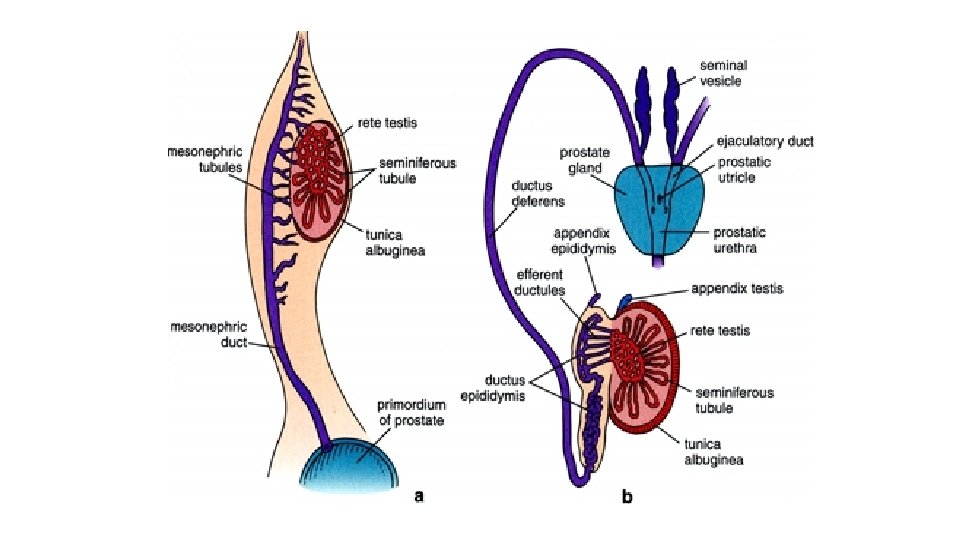
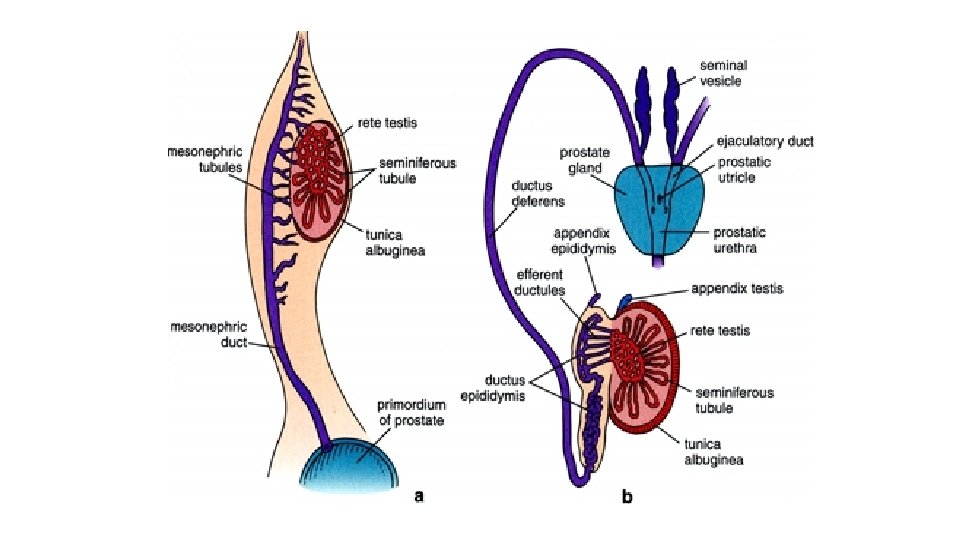
Development of the testis -Y chromosome has testis determining factor -Primitive sex cords are transformed into testis cords (medullary cords) & their deeper part forms tubules called rete testis - testis cords become separated from coelomic epithelium and the mesoderm forms tunica albuginea (fibrous capsule) around them
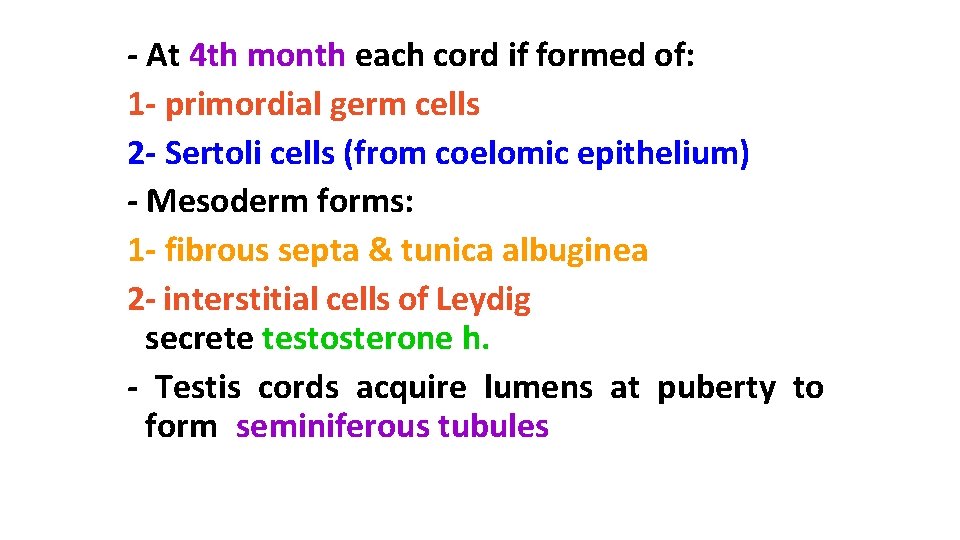
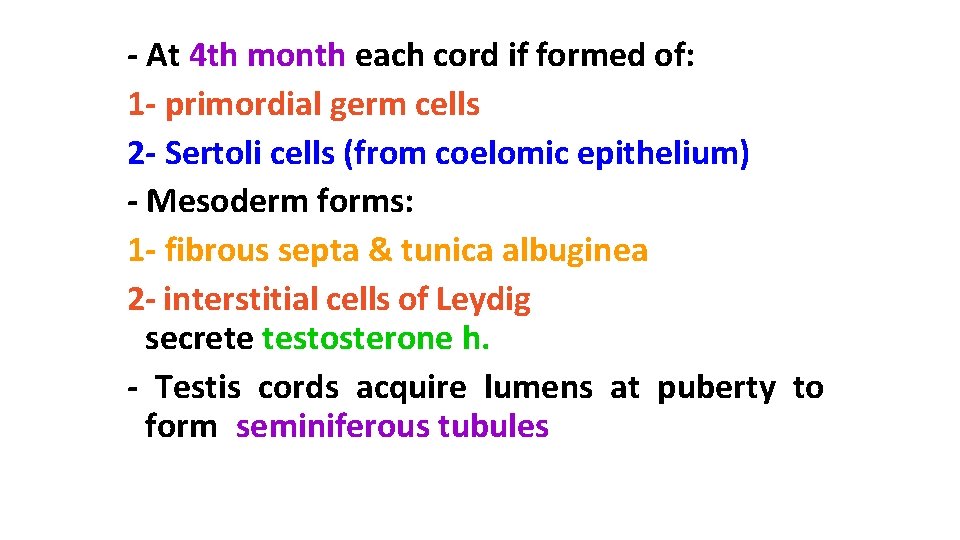
- At 4 th month each cord if formed of: 1 - primordial germ cells 2 - Sertoli cells (from coelomic epithelium) - Mesoderm forms: 1 - fibrous septa & tunica albuginea 2 - interstitial cells of Leydig secrete testosterone h. - Testis cords acquire lumens at puberty to form seminiferous tubules
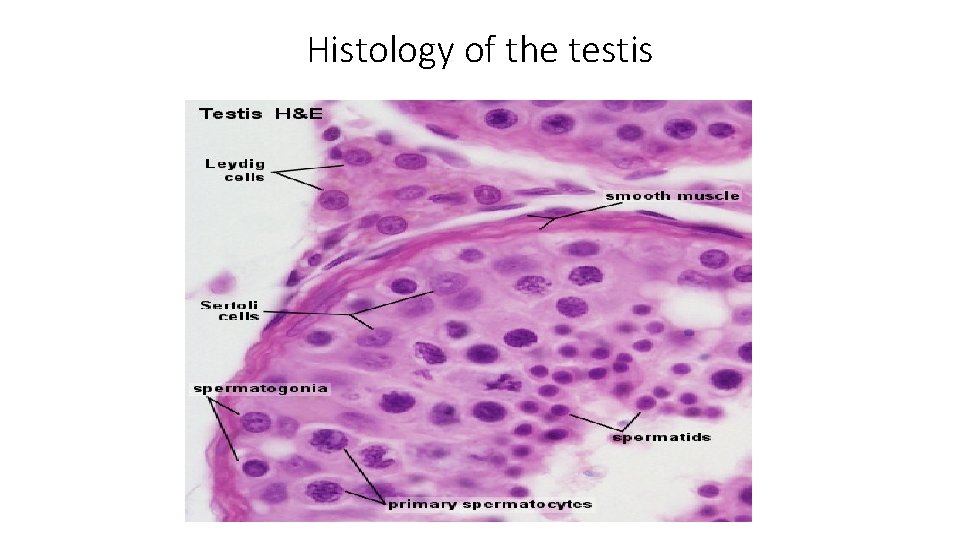
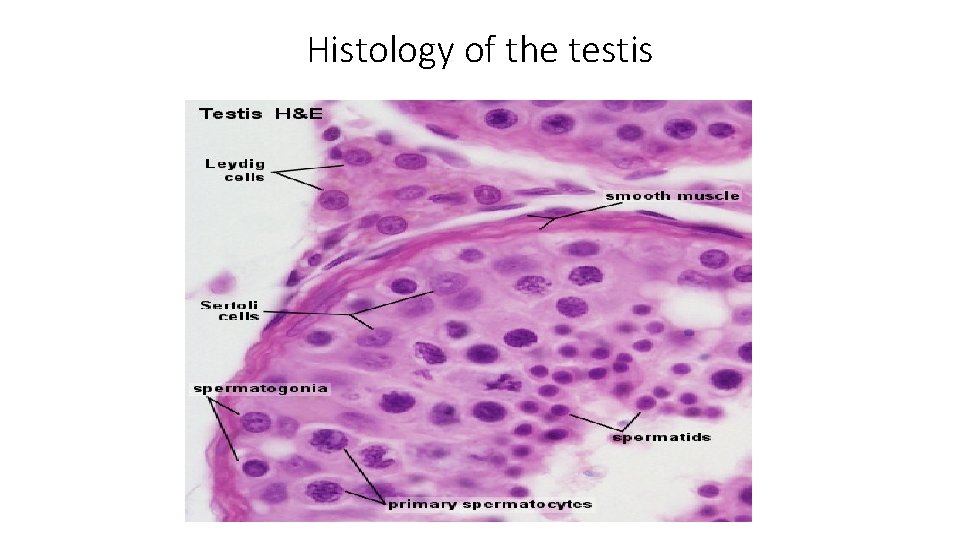
Histology of the testis
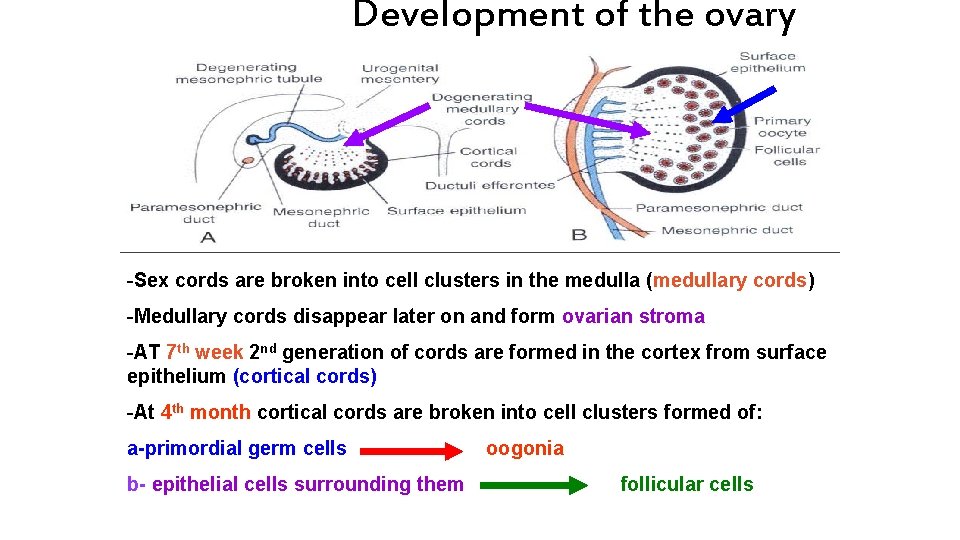
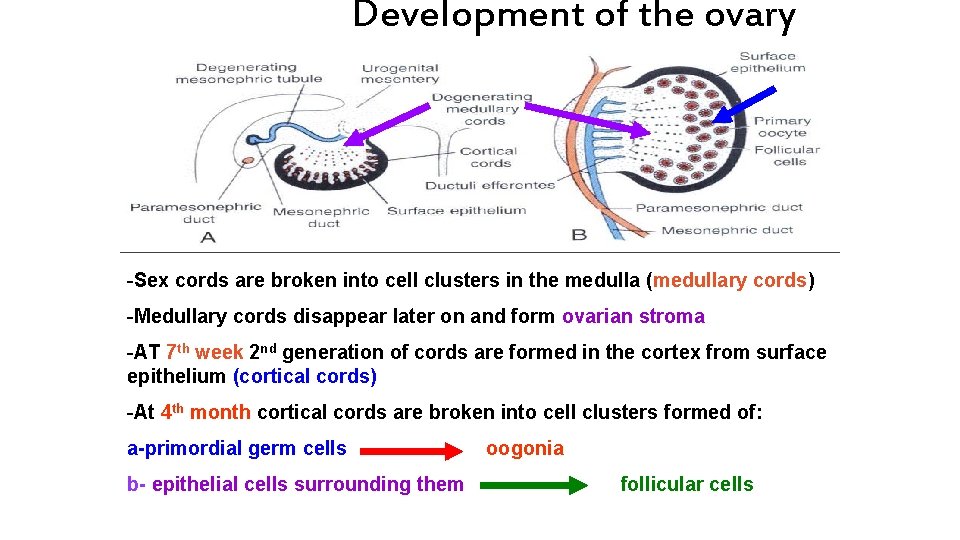
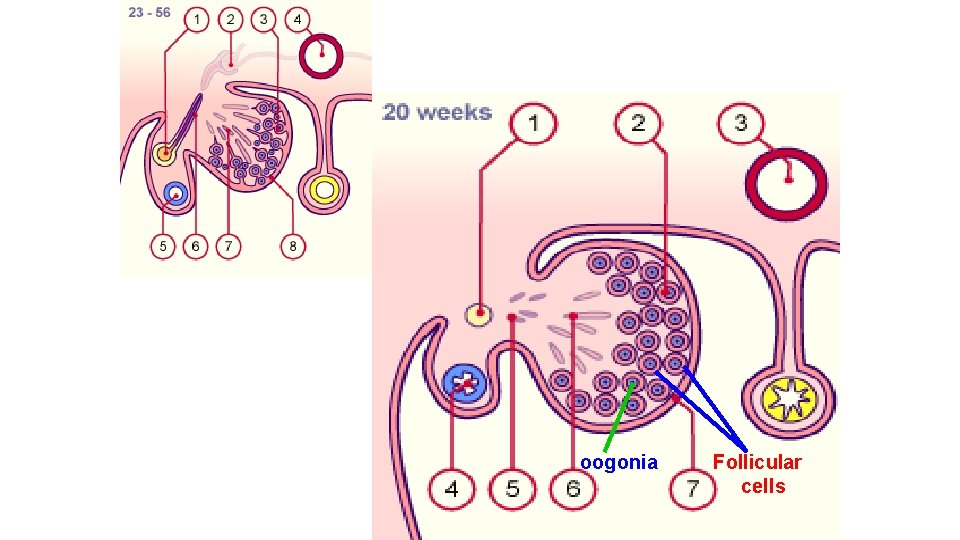
Development of the ovary -Sex cords are broken into cell clusters in the medulla (medullary cords) -Medullary cords disappear later on and form ovarian stroma -AT 7 th week 2 nd generation of cords are formed in the cortex from surface epithelium (cortical cords) -At 4 th month cortical cords are broken into cell clusters formed of: a-primordial germ cells b- epithelial cells surrounding them oogonia follicular cells
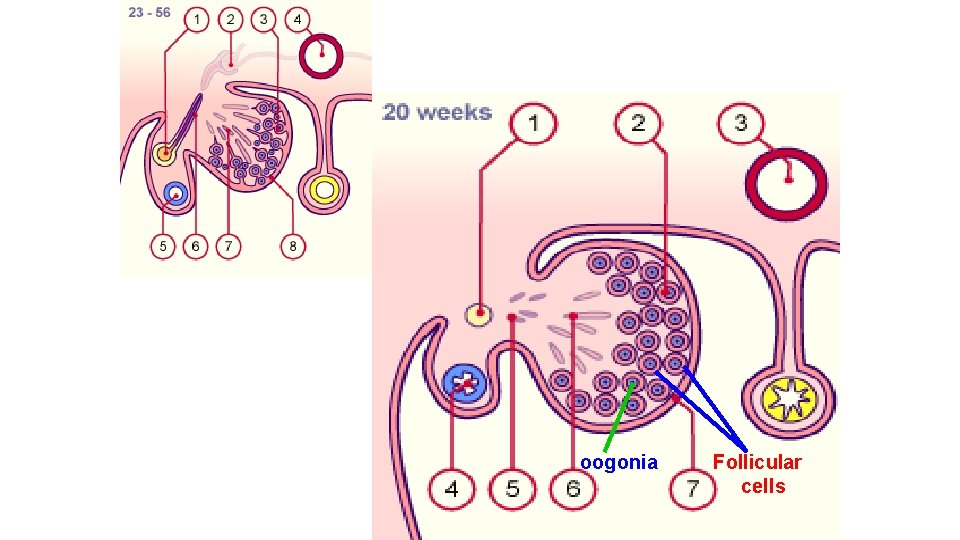
oogonia Follicular cells
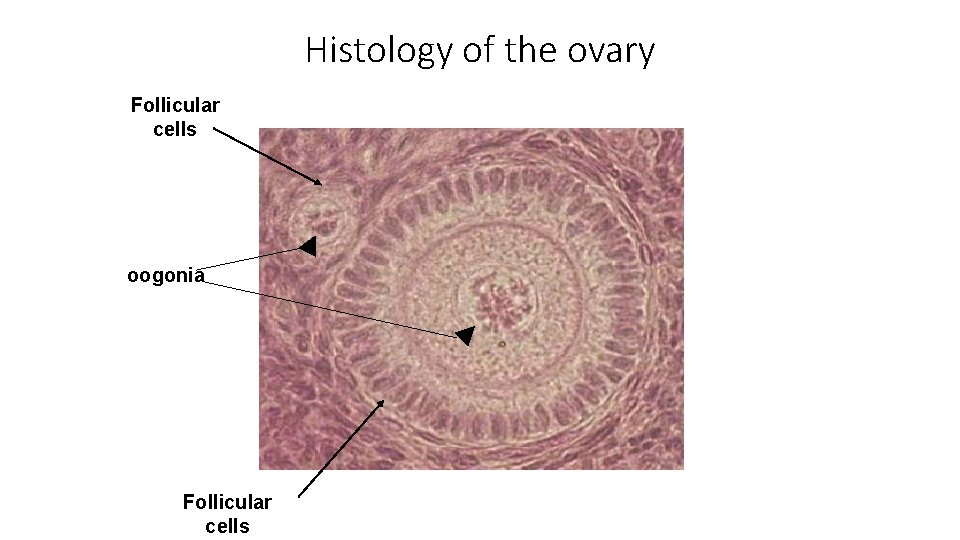
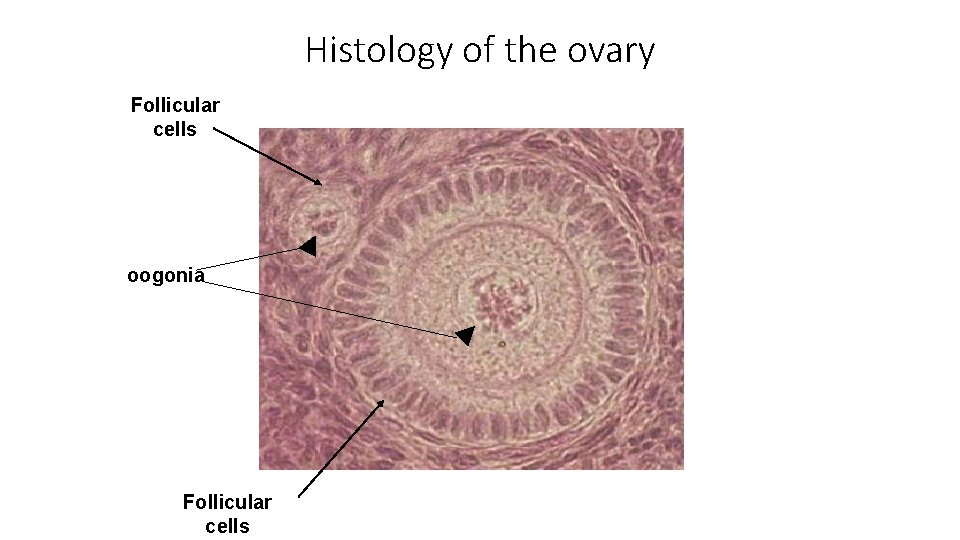
Histology of the ovary Follicular cells oogonia Follicular cells
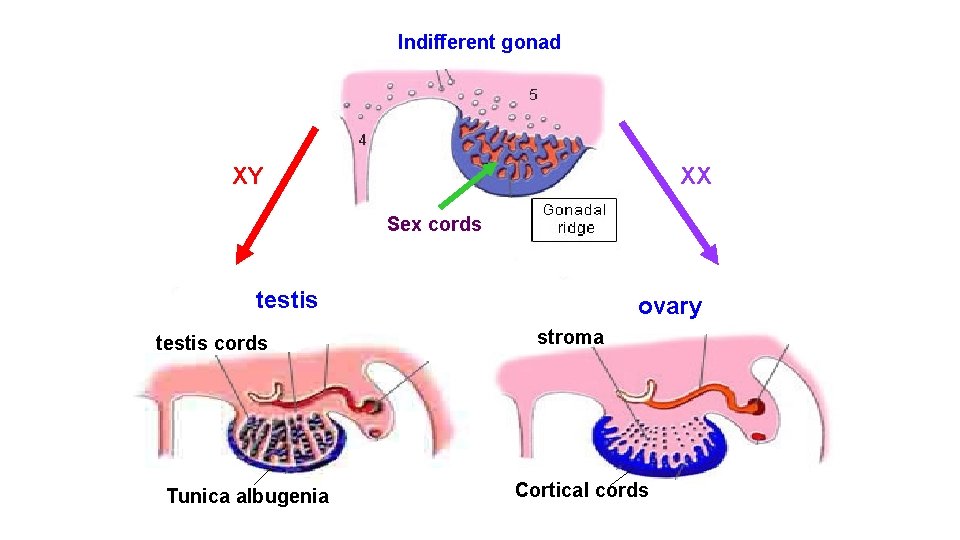
Indifferent gonad XY XX Sex cords testis cords Tunica albugenia ovary stroma Cortical cords
Development of the genital ducts
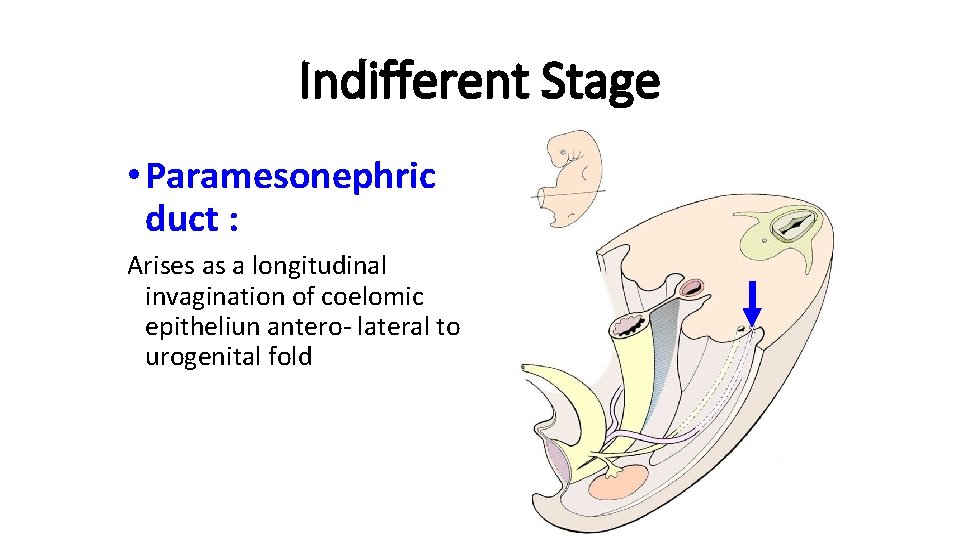
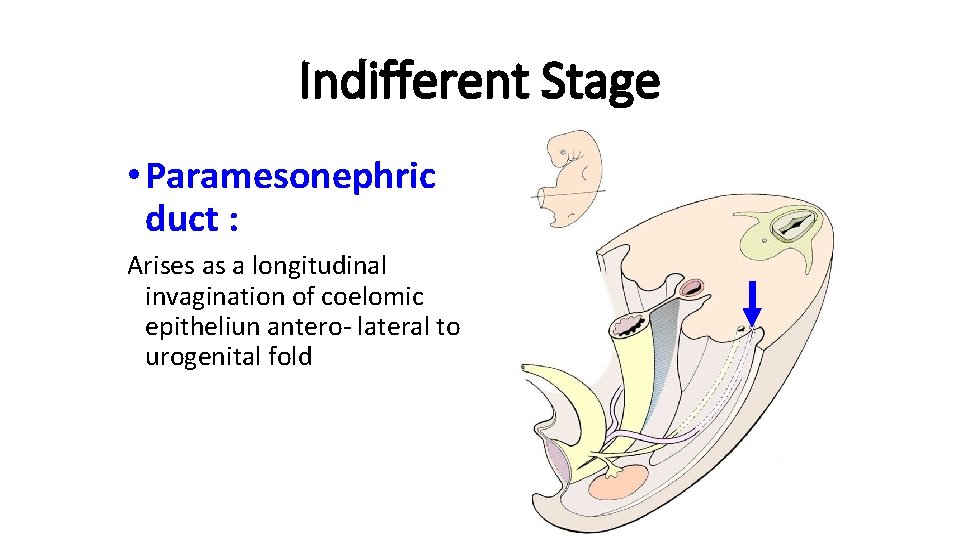
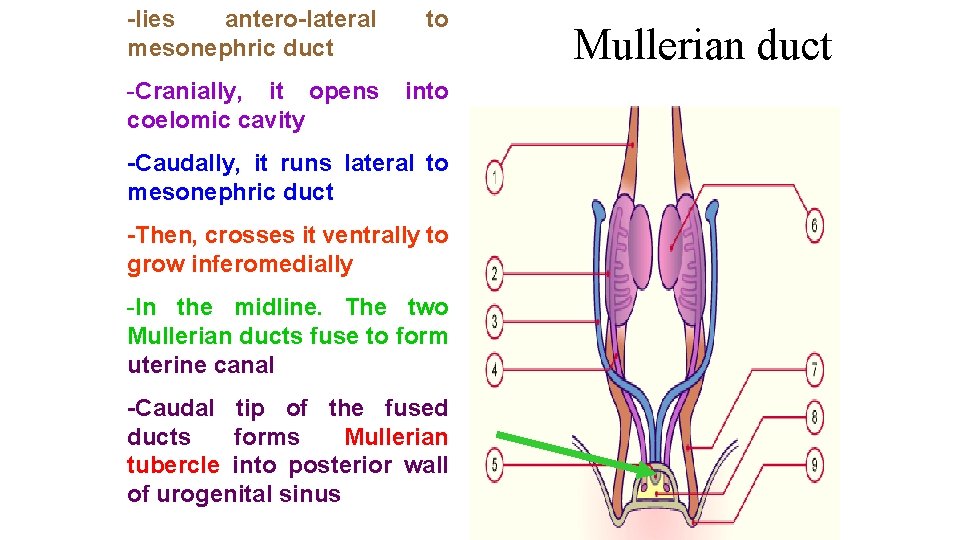
Indifferent Stage • Paramesonephric duct : Arises as a longitudinal invagination of coelomic epitheliun antero- lateral to urogenital fold
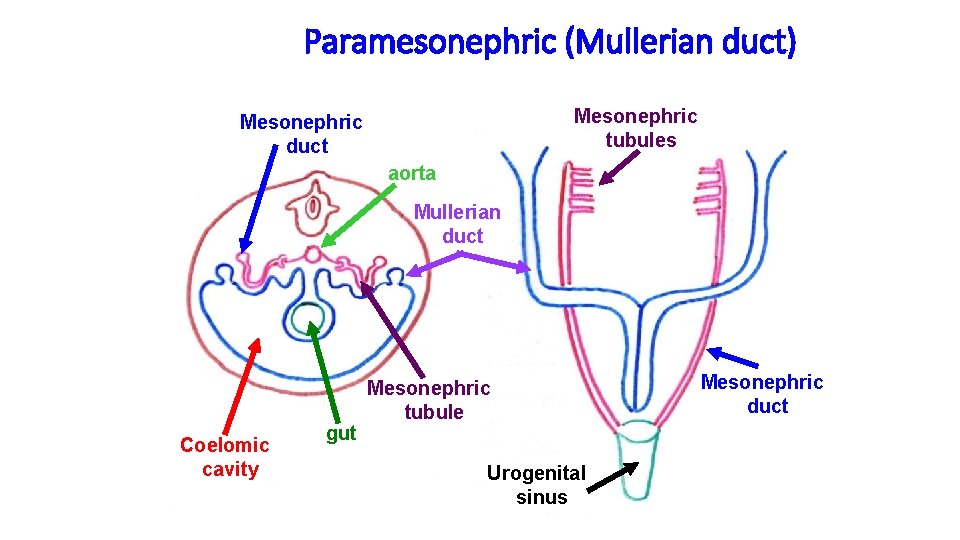
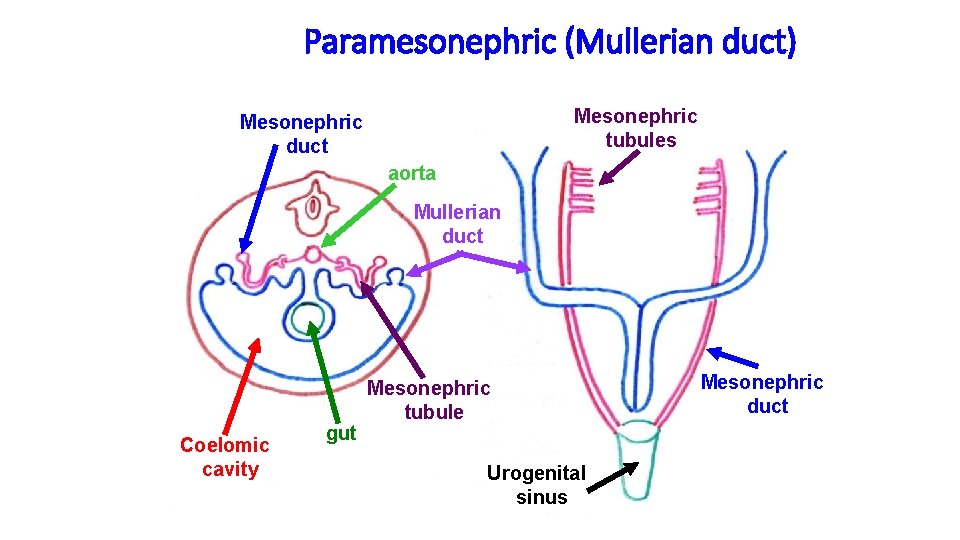
Paramesonephric (Mullerian duct) Mesonephric tubules Mesonephric duct aorta Mullerian duct Coelomic cavity gut Mesonephric tubule Urogenital sinus Mesonephric duct
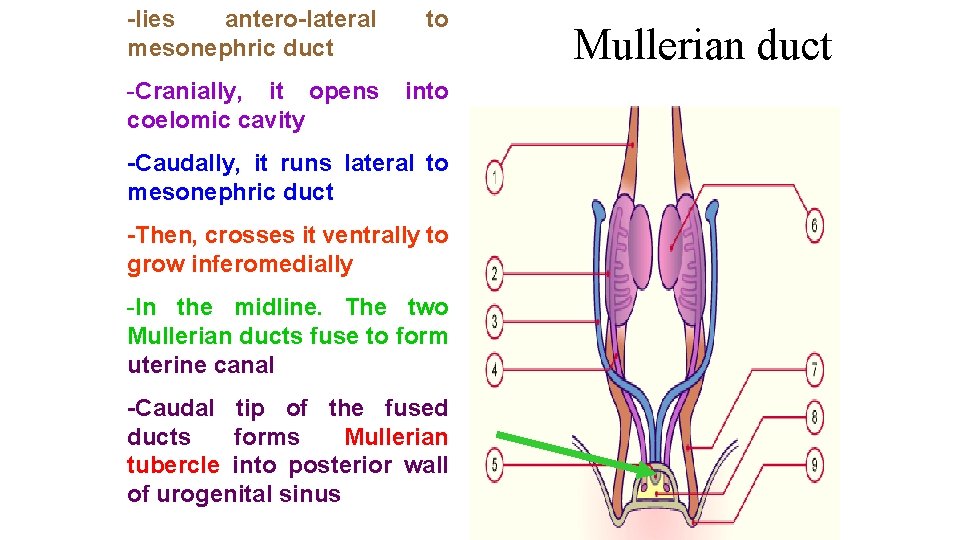
-lies antero-lateral mesonephric duct to -Cranially, it opens coelomic cavity into -Caudally, it runs lateral to mesonephric duct -Then, crosses it ventrally to grow inferomedially -In the midline. The two Mullerian ducts fuse to form uterine canal -Caudal tip of the fused ducts forms Mullerian tubercle into posterior wall of urogenital sinus Mullerian duct
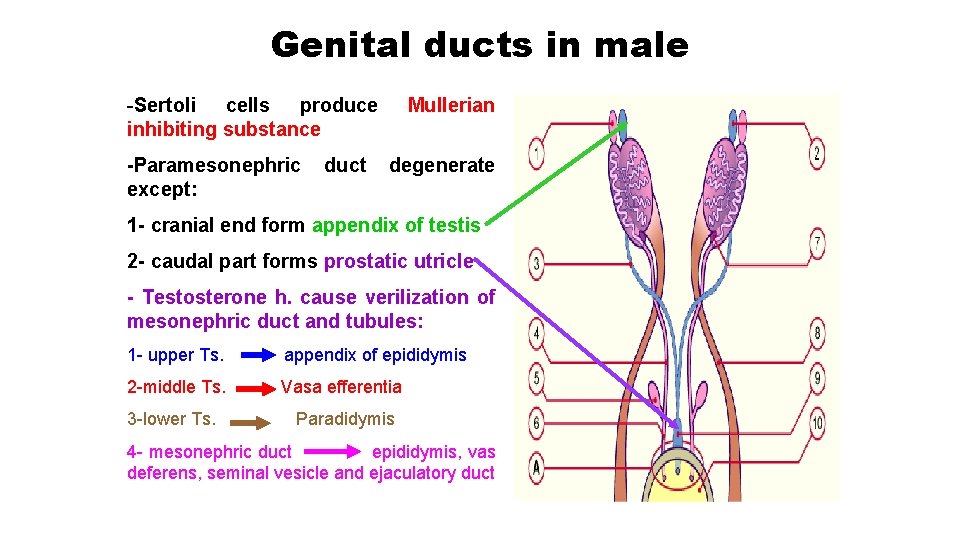
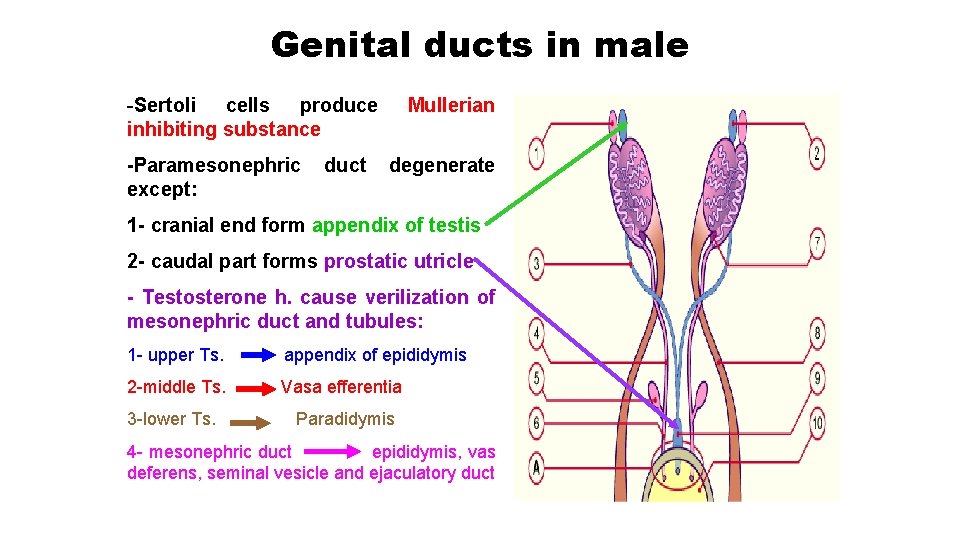
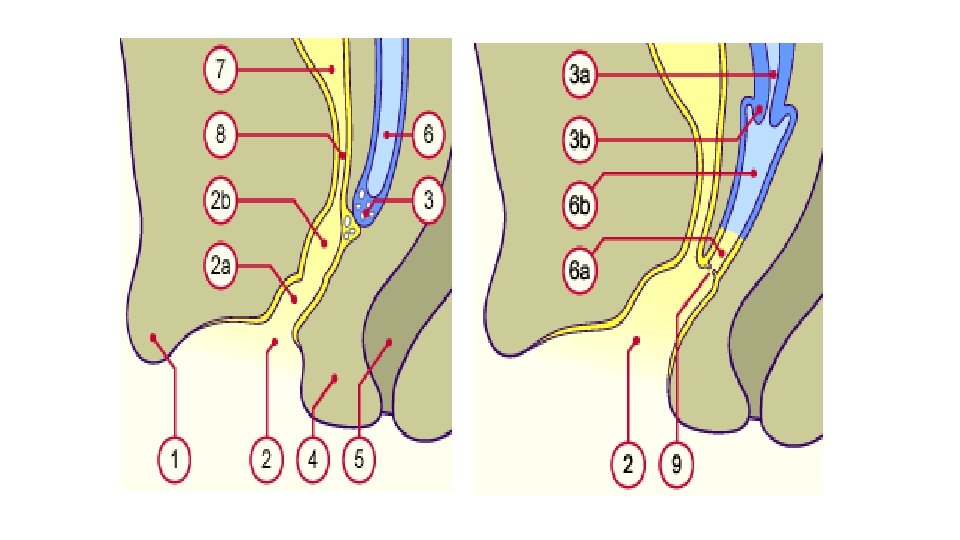
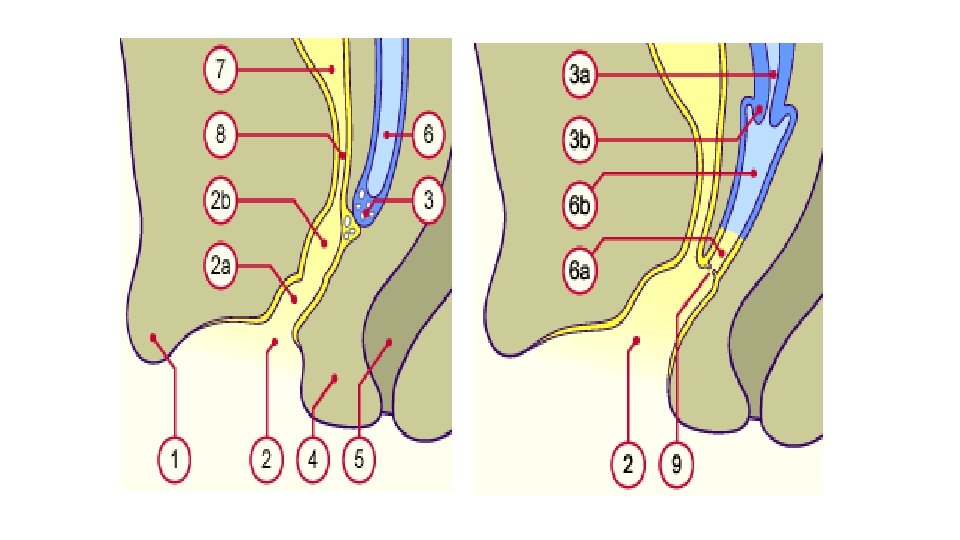
Genital ducts in male -Sertoli cells produce inhibiting substance -Paramesonephric except: duct Mullerian degenerate 1 - cranial end form appendix of testis 2 - caudal part forms prostatic utricle - Testosterone h. cause verilization of mesonephric duct and tubules: 1 - upper Ts. appendix of epididymis 2 -middle Ts. Vasa efferentia 3 -lower Ts. Paradidymis 4 - mesonephric duct epididymis, vas deferens, seminal vesicle and ejaculatory duct
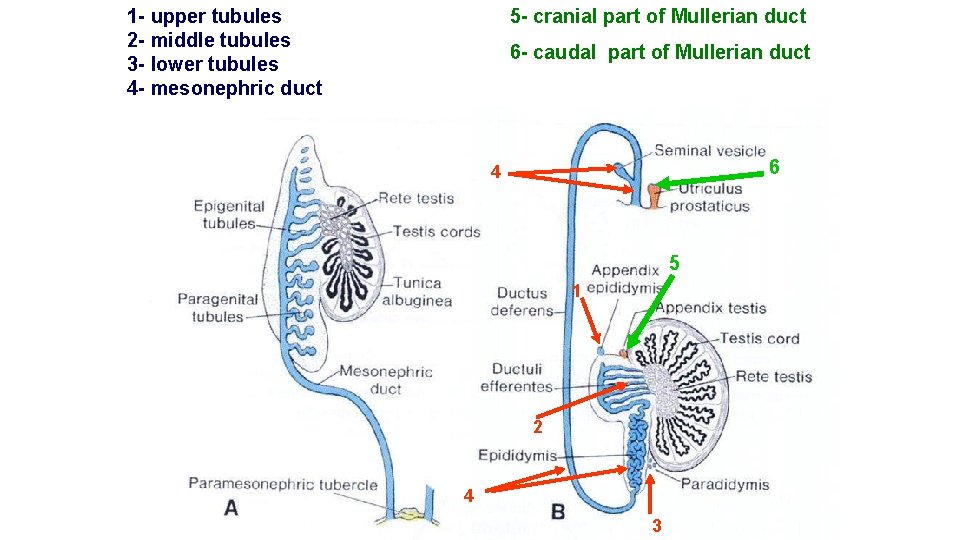
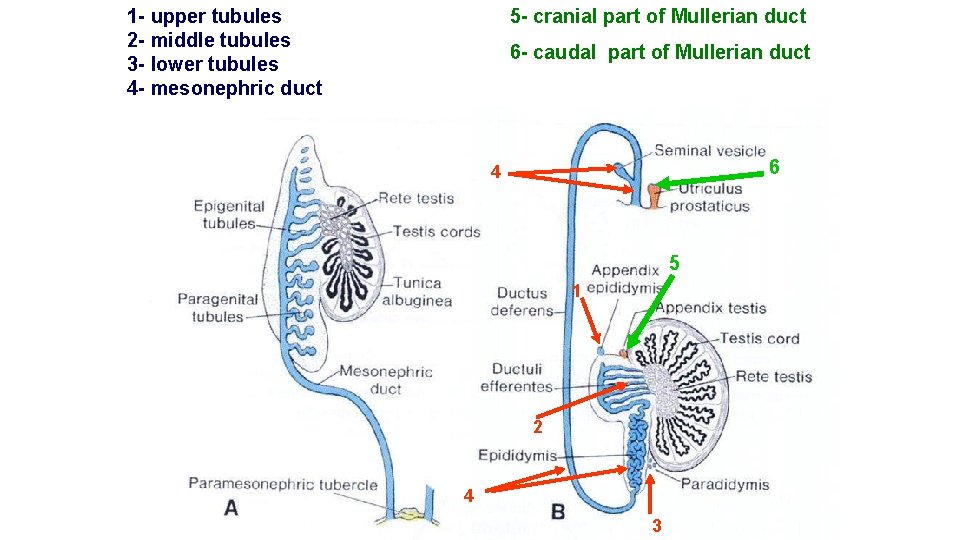
1 - upper tubules 2 - middle tubules 3 - lower tubules 4 - mesonephric duct 5 - cranial part of Mullerian duct 6 - caudal part of Mullerian duct 6 4 5 1 2 4 3
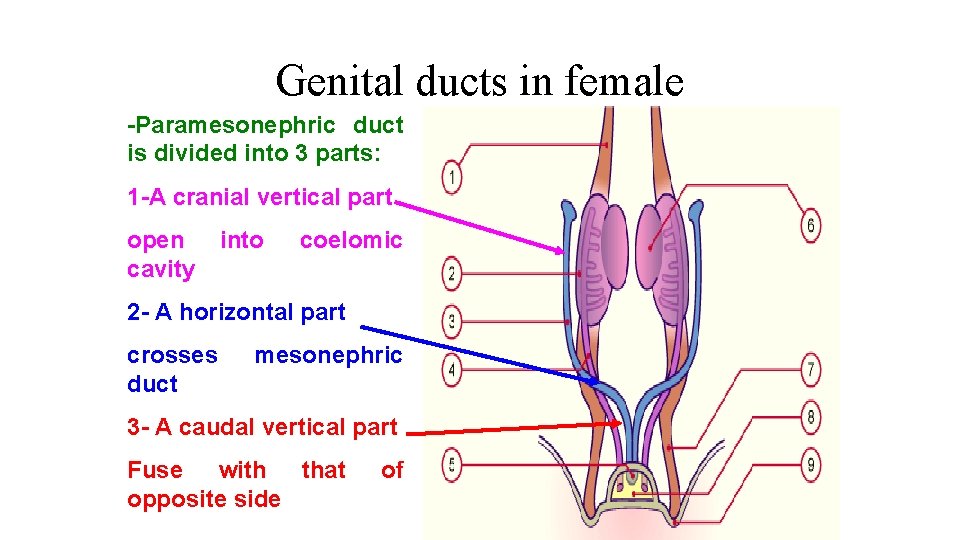
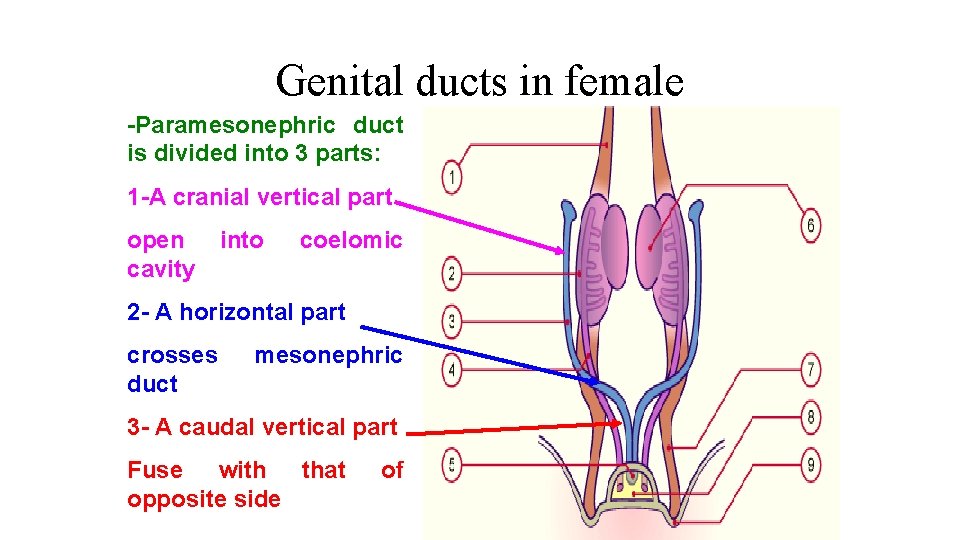
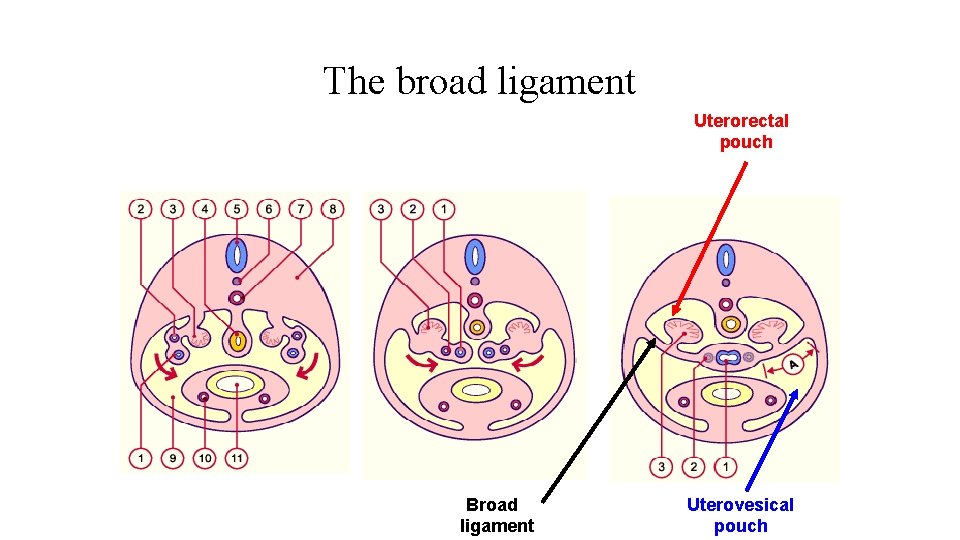
Genital ducts in female -Paramesonephric duct is divided into 3 parts: 1 -A cranial vertical part open cavity into coelomic 2 - A horizontal part crosses duct mesonephric 3 - A caudal vertical part Fuse with that opposite side of
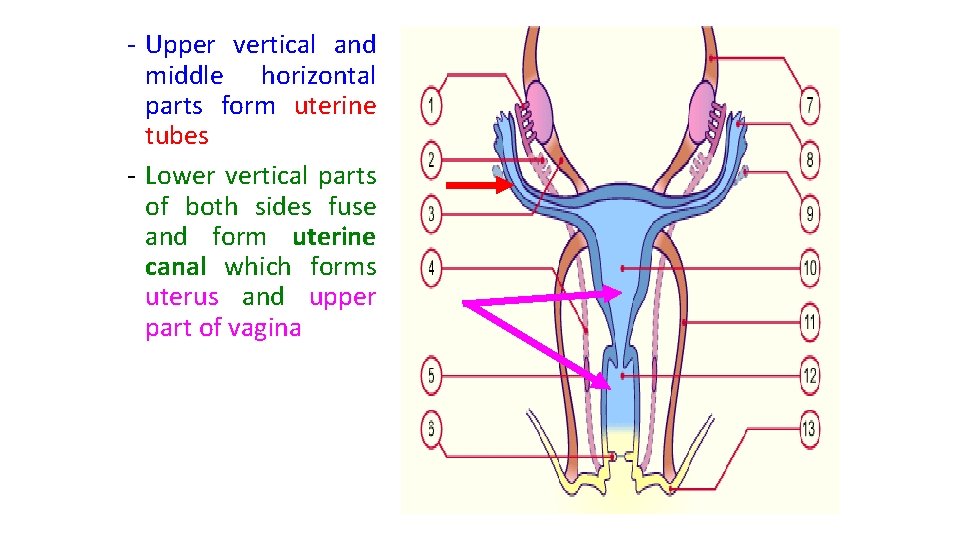
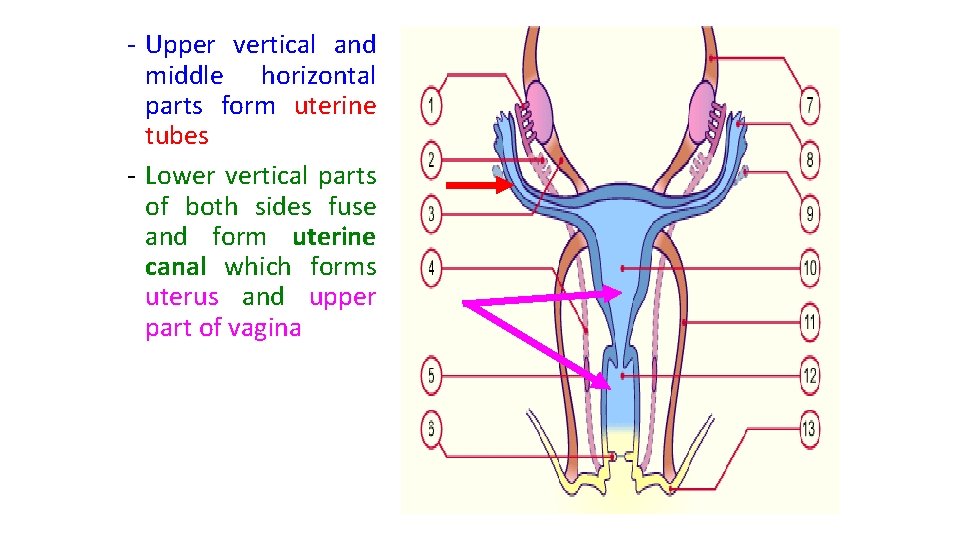
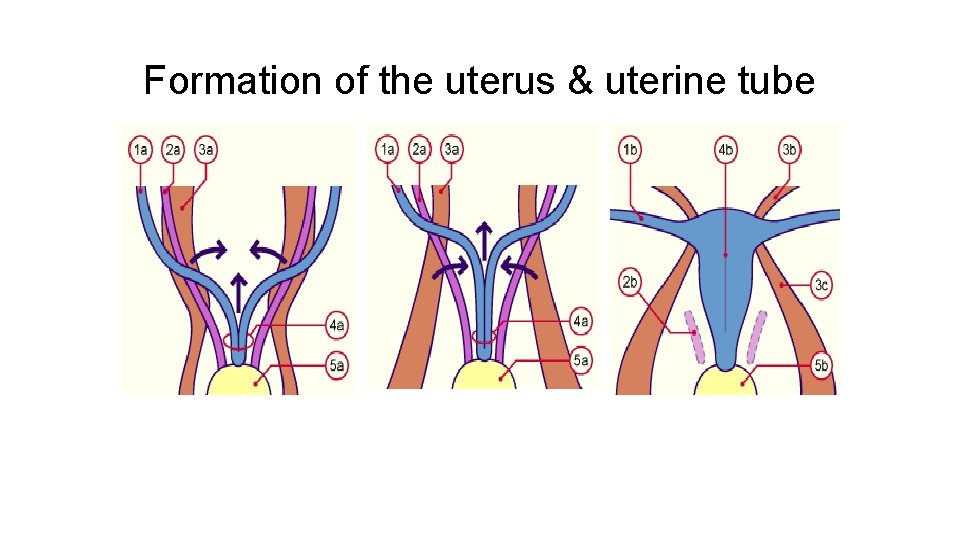
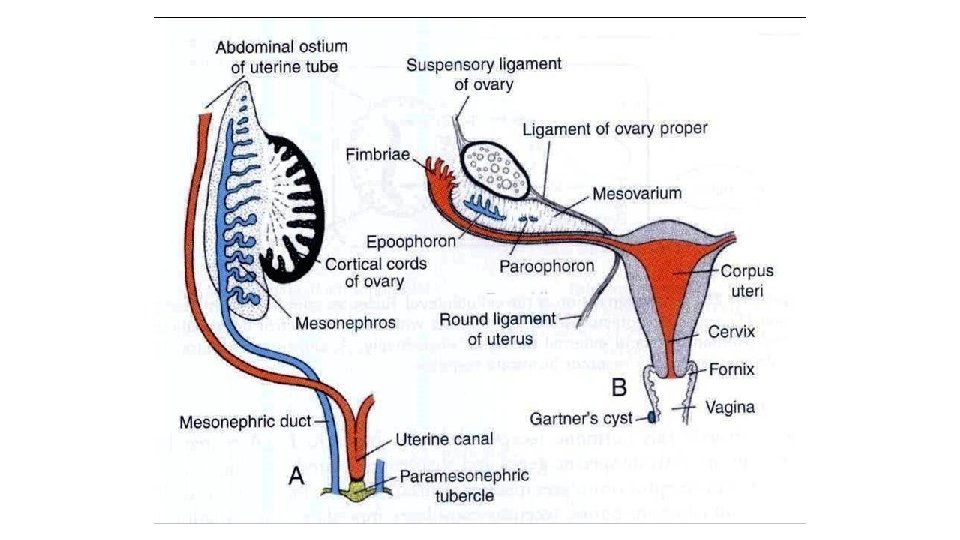
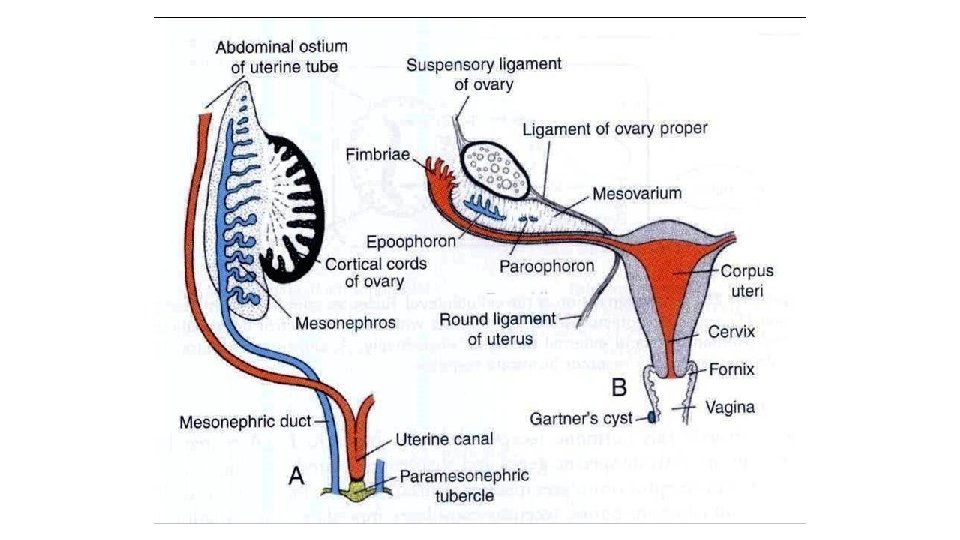
- Upper vertical and middle horizontal parts form uterine tubes - Lower vertical parts of both sides fuse and form uterine canal which forms uterus and upper part of vagina
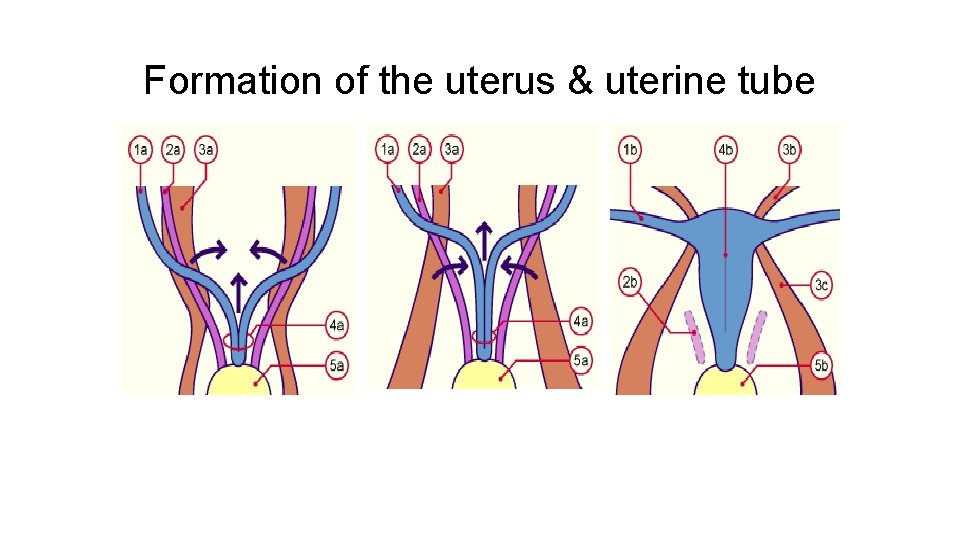
Formation of the uterus & uterine tube
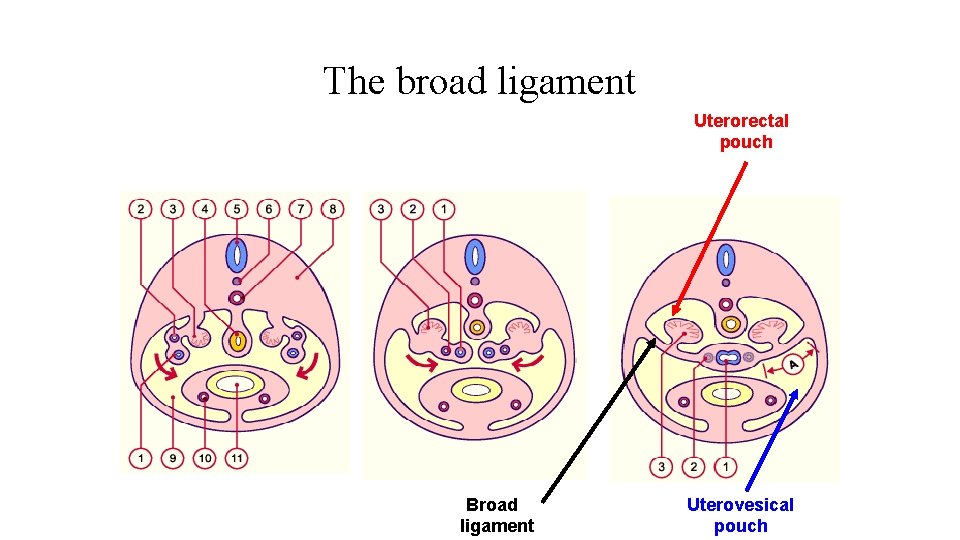
The broad ligament Uterorectal pouch Broad ligament Uterovesical pouch
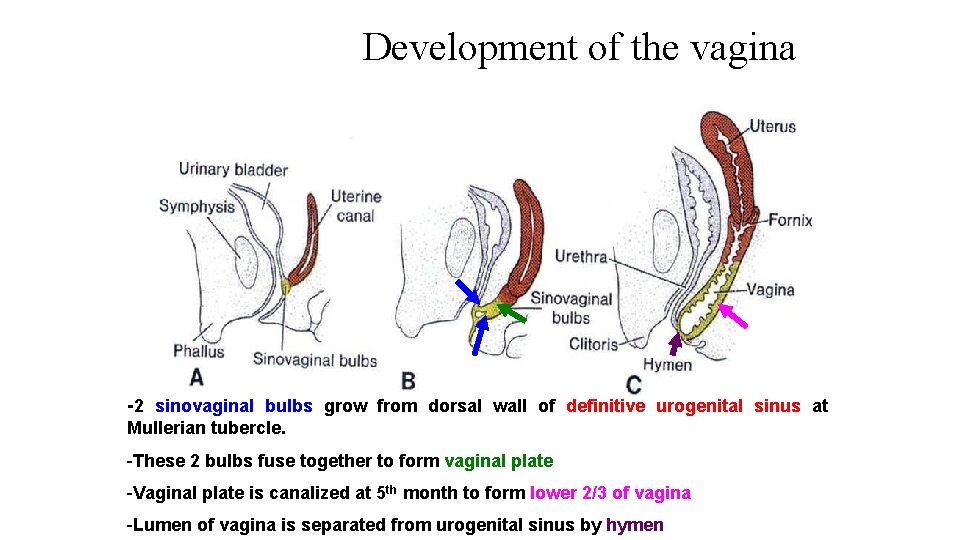
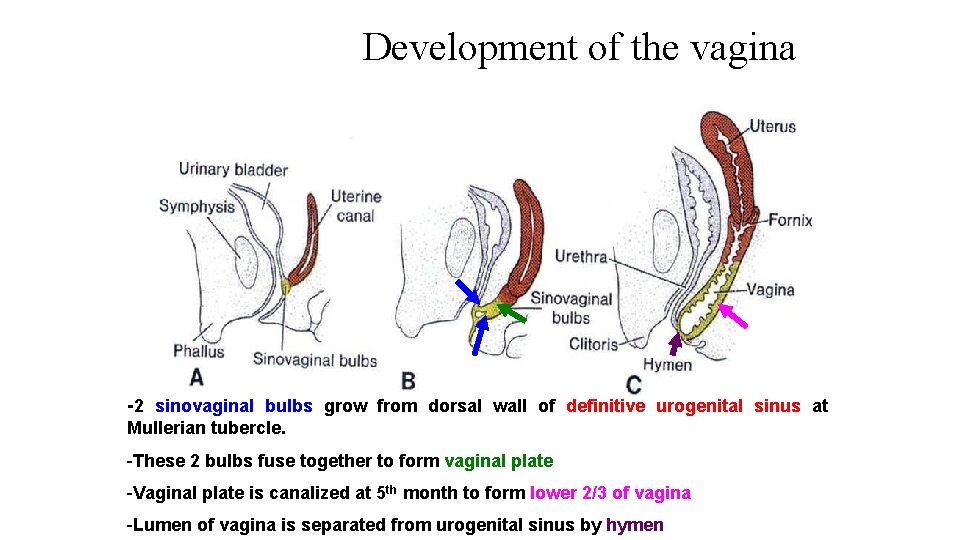
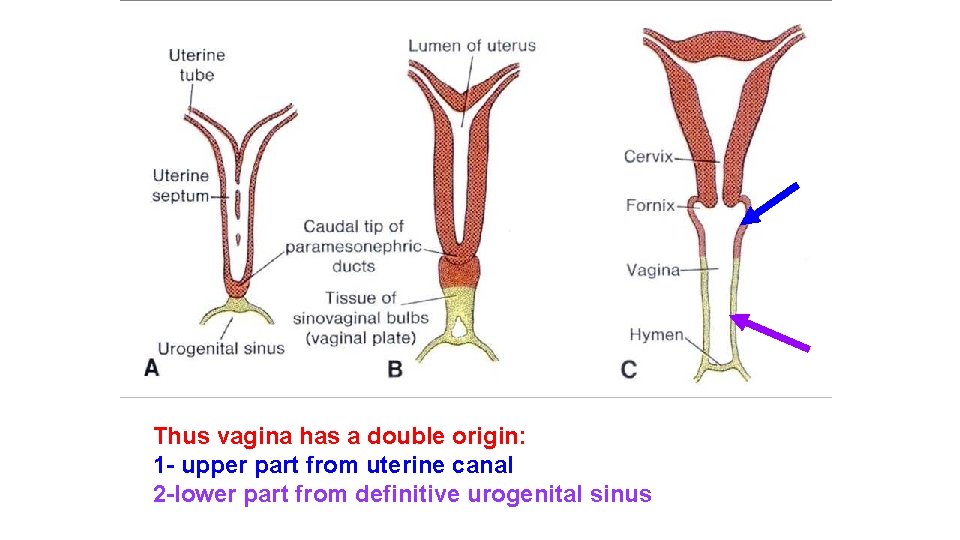
Development of the vagina -2 sinovaginal bulbs grow from dorsal wall of definitive urogenital sinus at Mullerian tubercle. -These 2 bulbs fuse together to form vaginal plate -Vaginal plate is canalized at 5 th month to form lower 2/3 of vagina -Lumen of vagina is separated from urogenital sinus by hymen
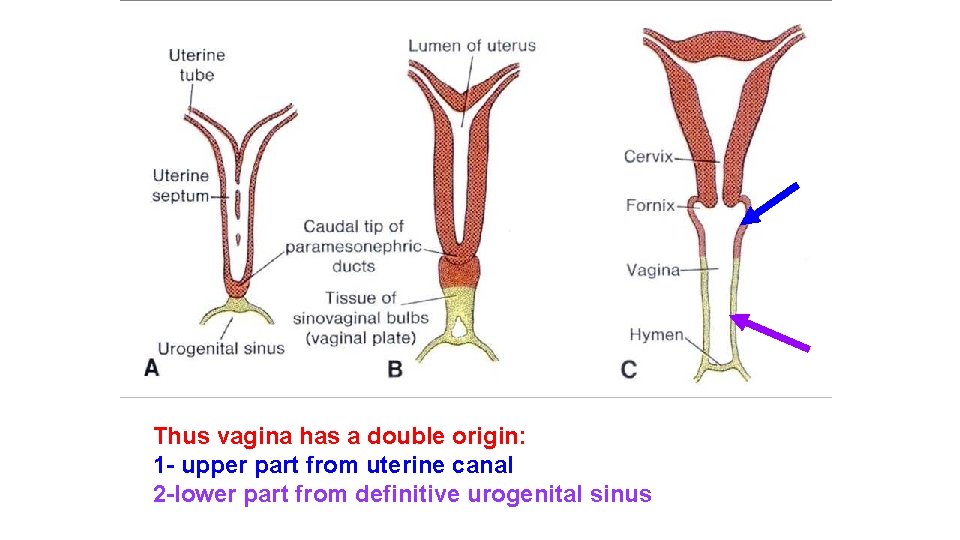
Thus vagina has a double origin: 1 - upper part from uterine canal 2 -lower part from definitive urogenital sinus
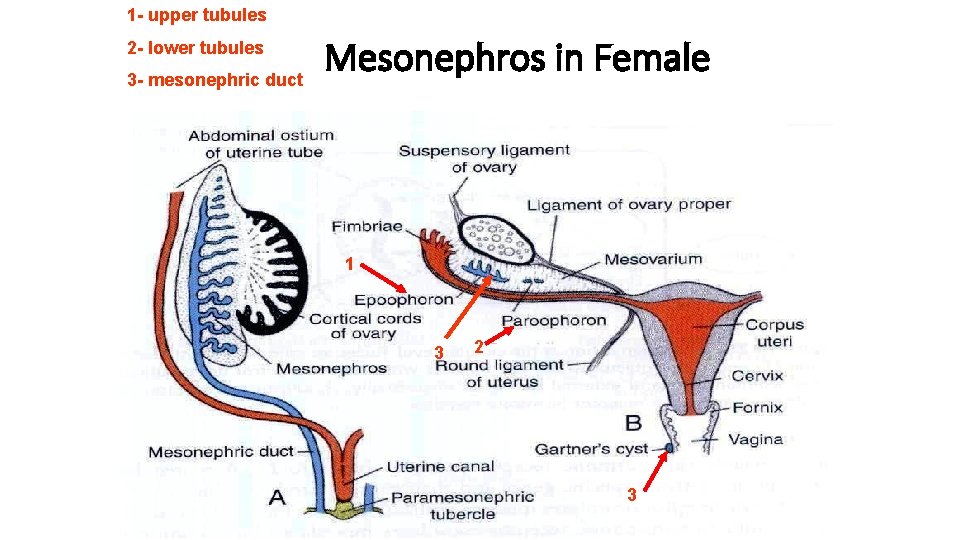
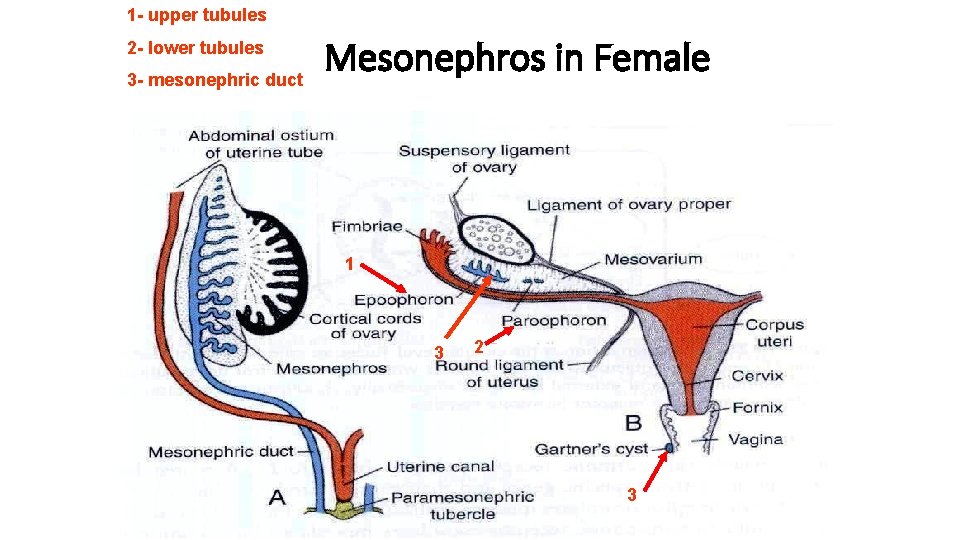
1 - upper tubules 2 - lower tubules 3 - mesonephric duct Mesonephros in Female 1 3 2 3
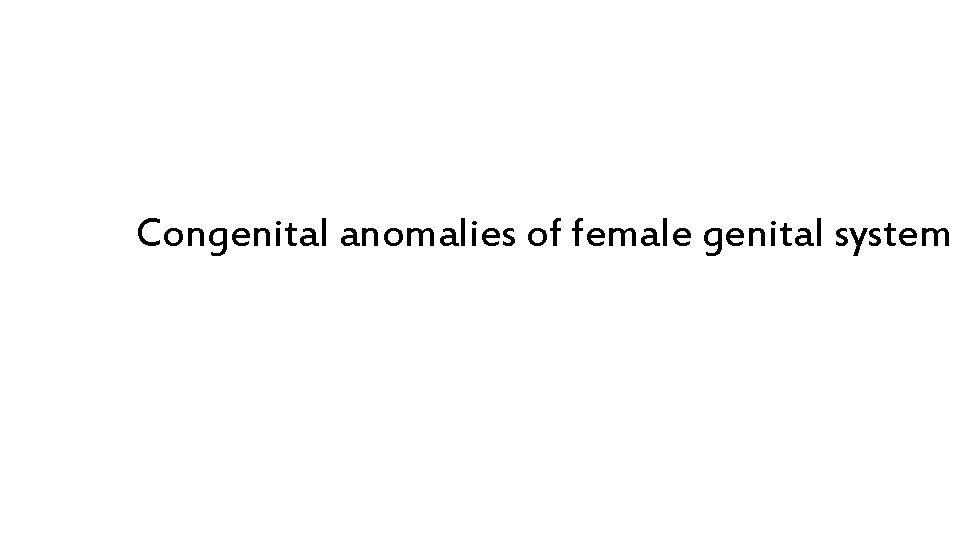
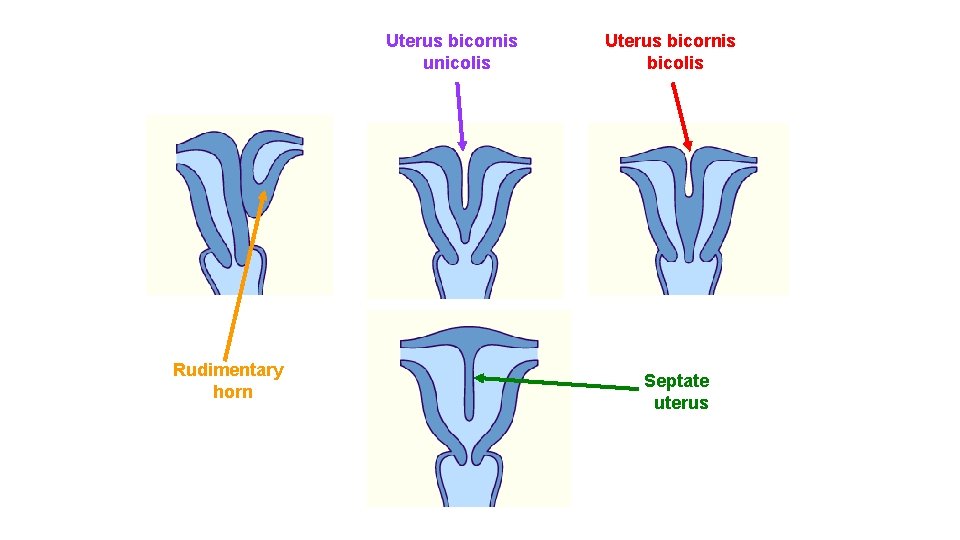
Congenital anomalies of female genital system
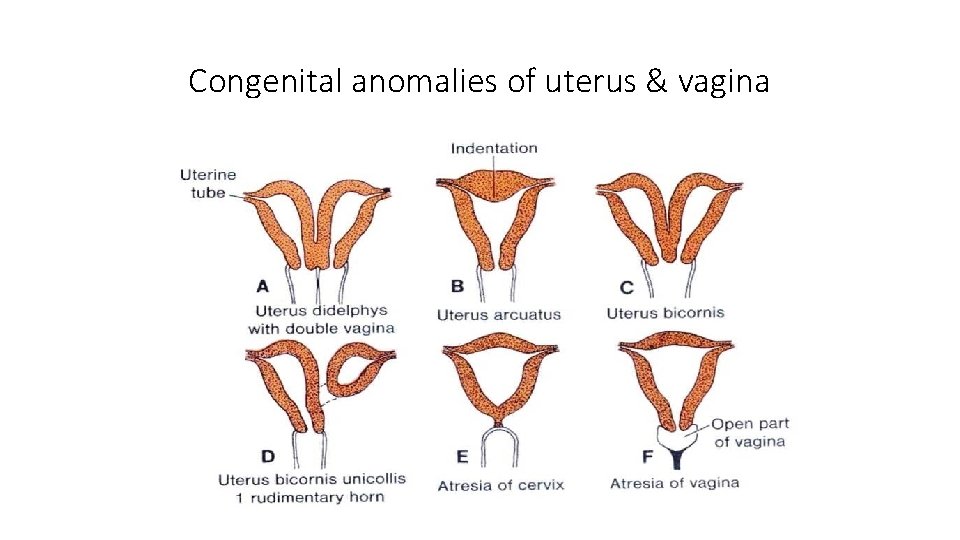
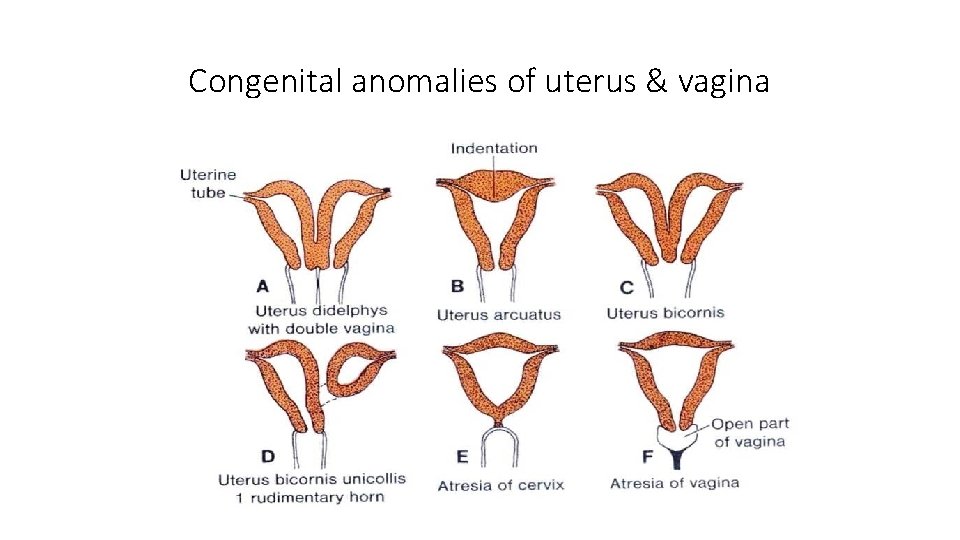
Congenital anomalies of uterus & vagina
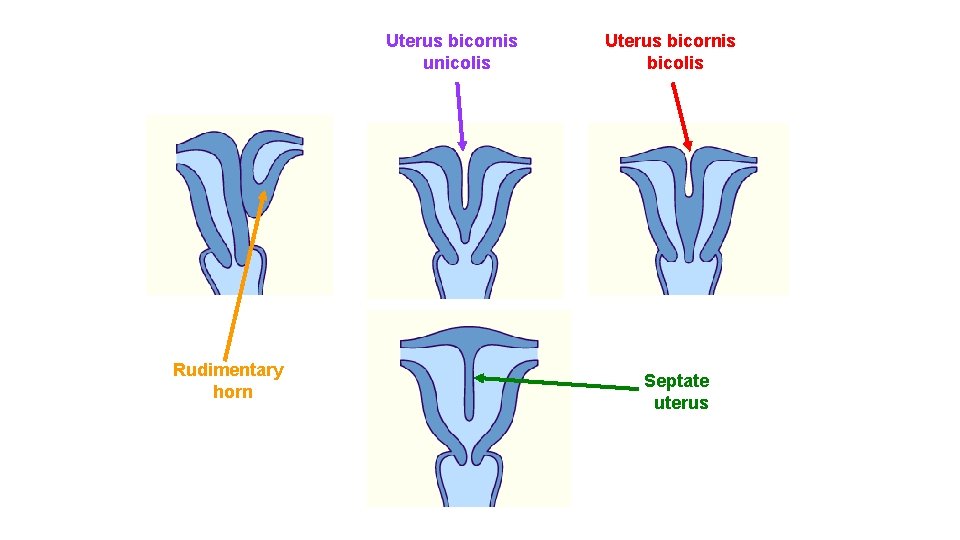
Uterus bicornis unicolis Rudimentary horn Uterus bicornis bicolis Septate uterus
Descent of the gonads
testis Descent of the
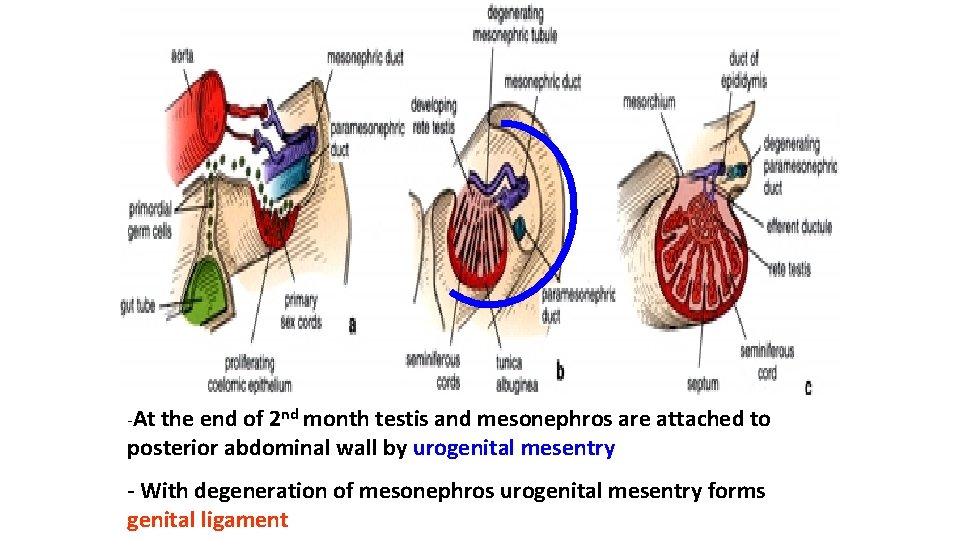
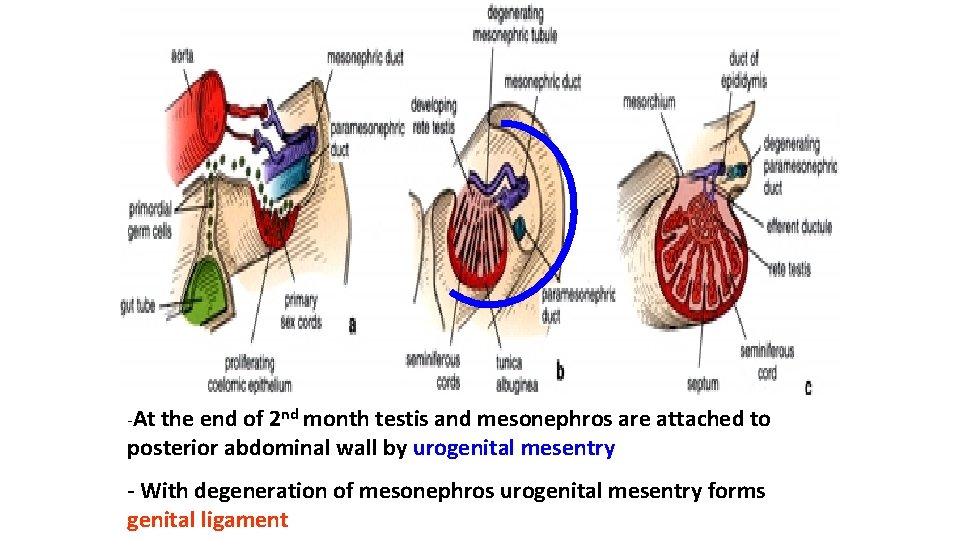
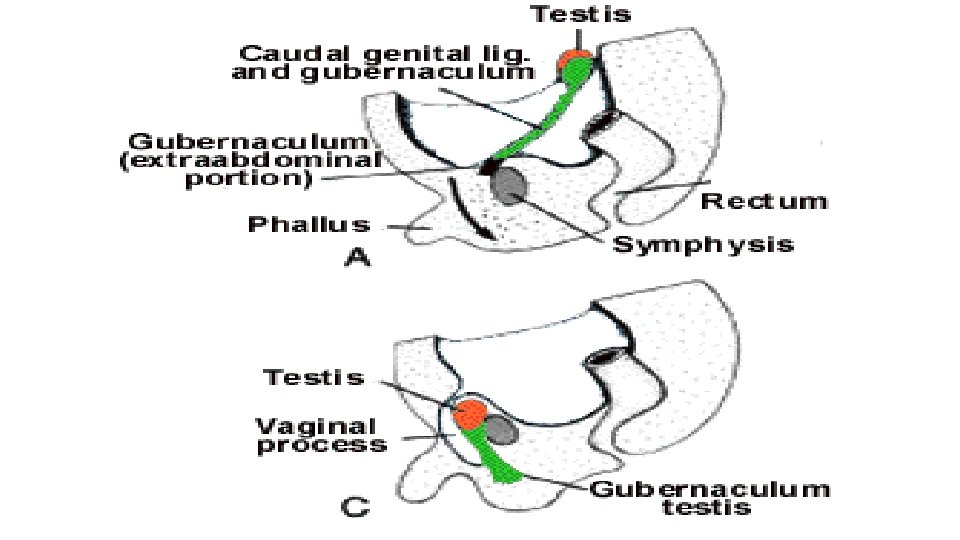
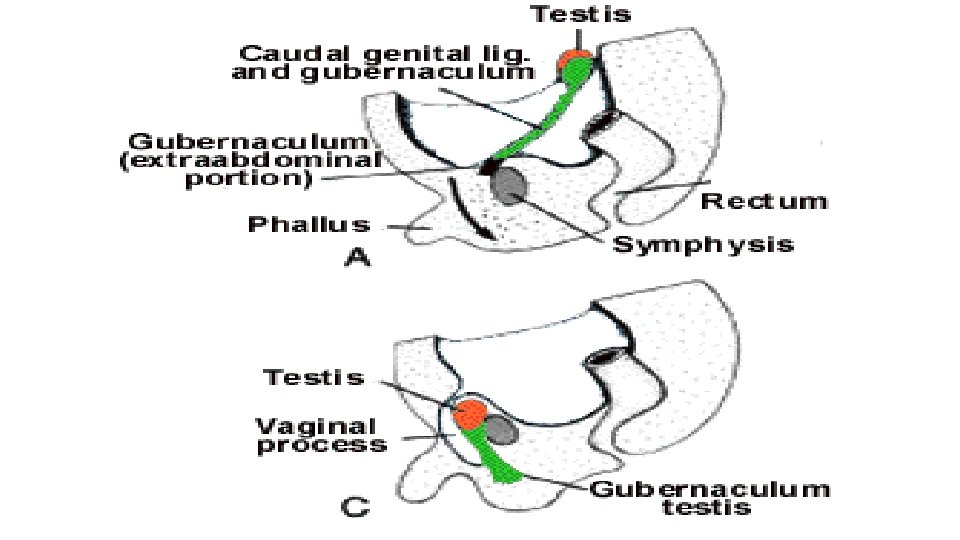
-At the end of 2 nd month testis and mesonephros are attached to posterior abdominal wall by urogenital mesentry - With degeneration of mesonephros urogenital mesentry forms genital ligament
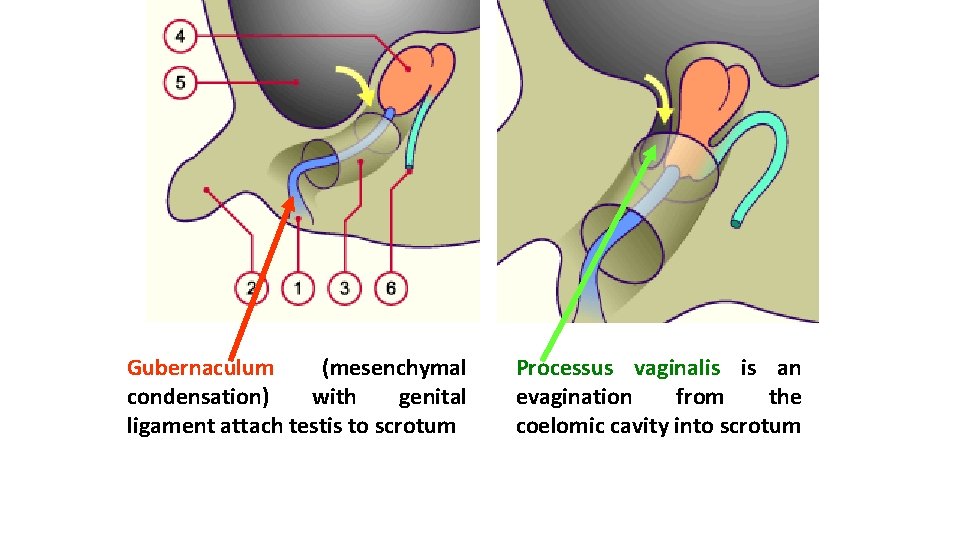
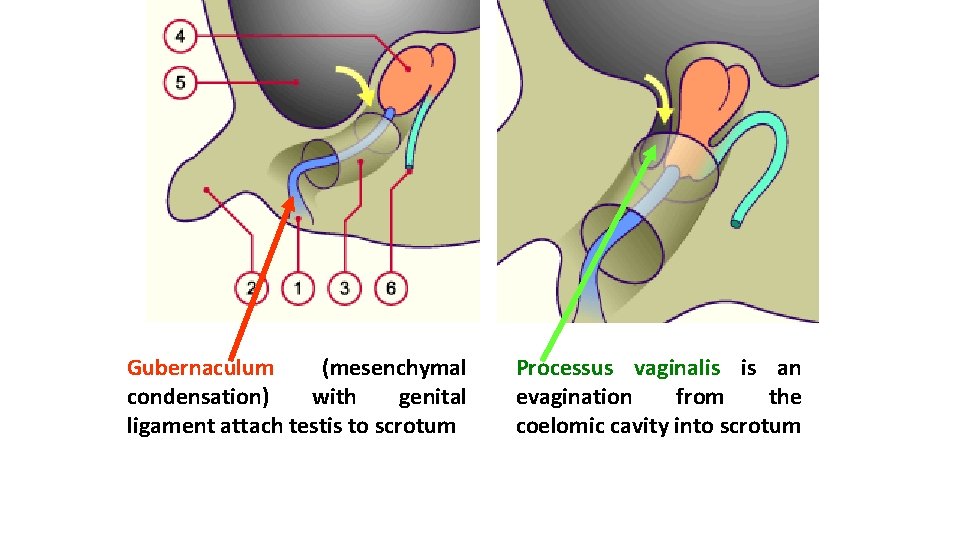
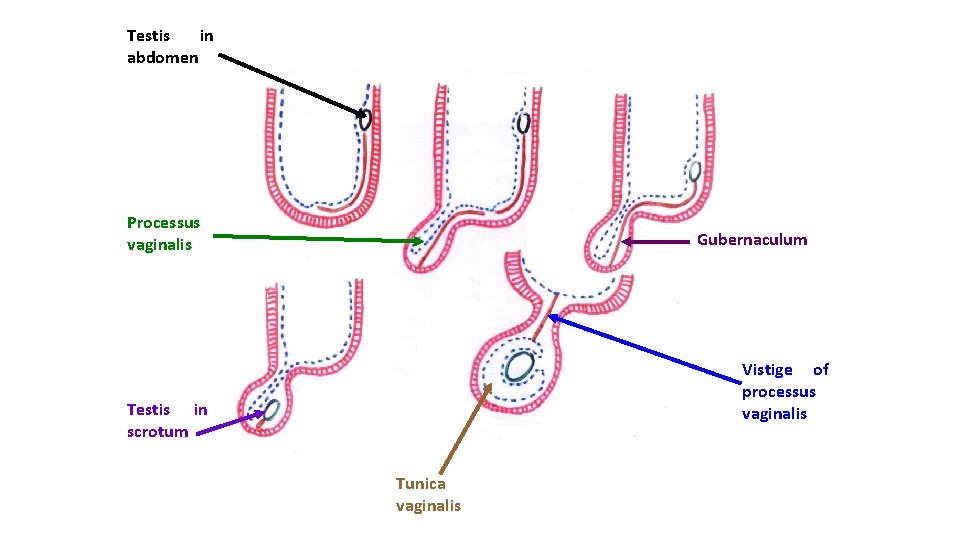
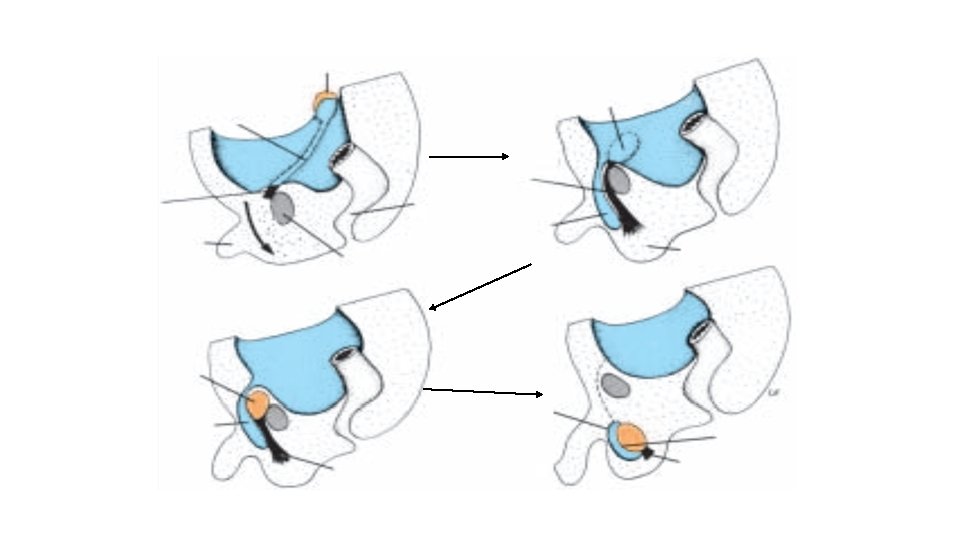
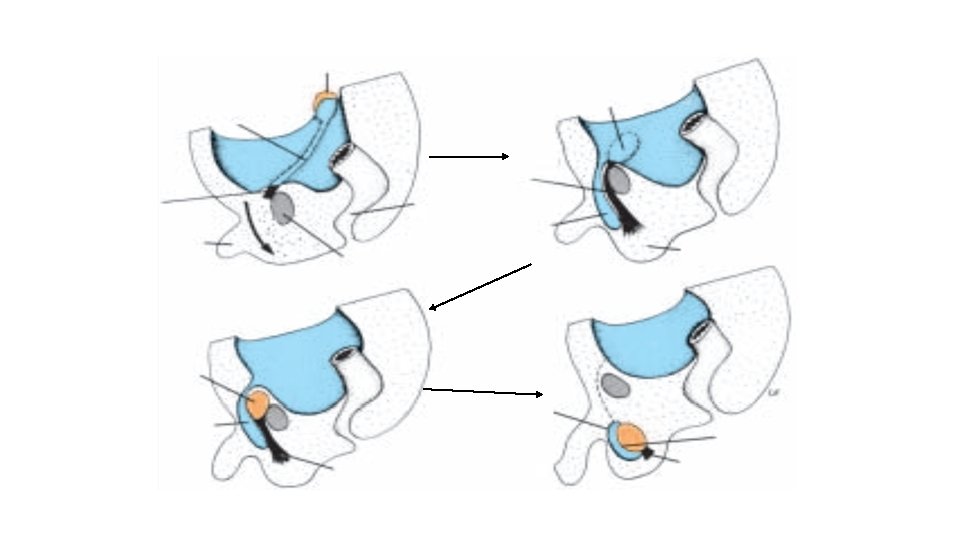
Gubernaculum (mesenchymal condensation) with genital ligament attach testis to scrotum Processus vaginalis is an evagination from the coelomic cavity into scrotum
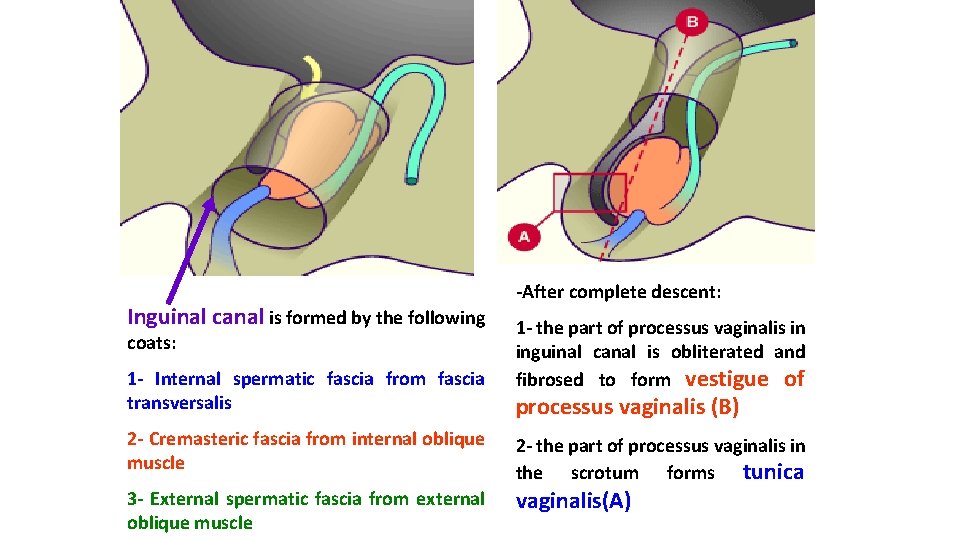
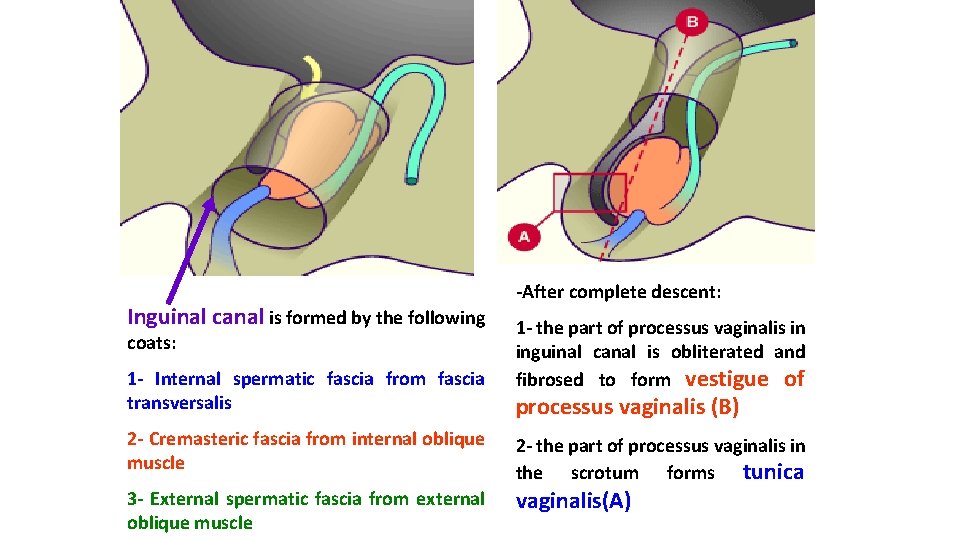
Inguinal canal is formed by the following coats: 1 - Internal spermatic fascia from fascia transversalis 2 - Cremasteric fascia from internal oblique muscle 3 - External spermatic fascia from external oblique muscle -After complete descent: 1 - the part of processus vaginalis in inguinal canal is obliterated and fibrosed to form vestigue of processus vaginalis (B) 2 - the part of processus vaginalis in the scrotum forms tunica vaginalis(A)
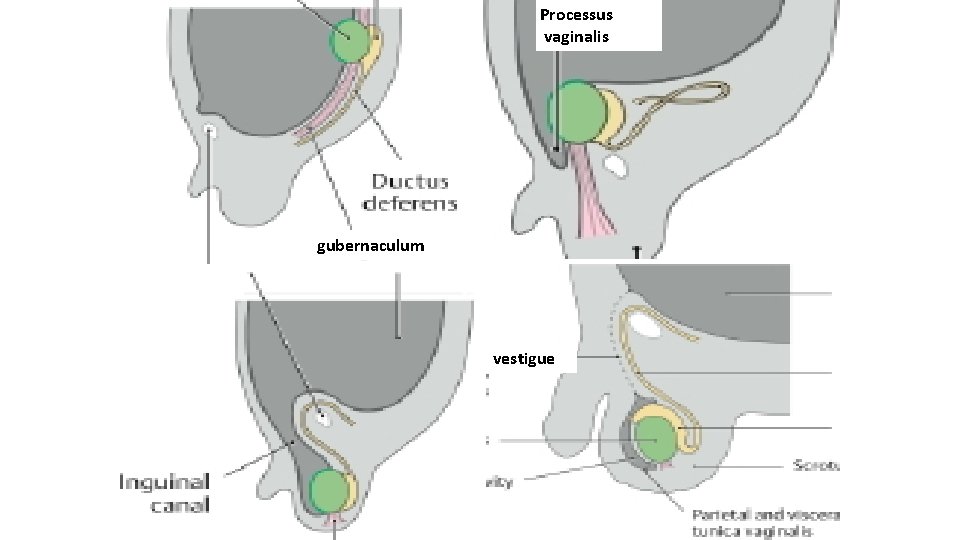
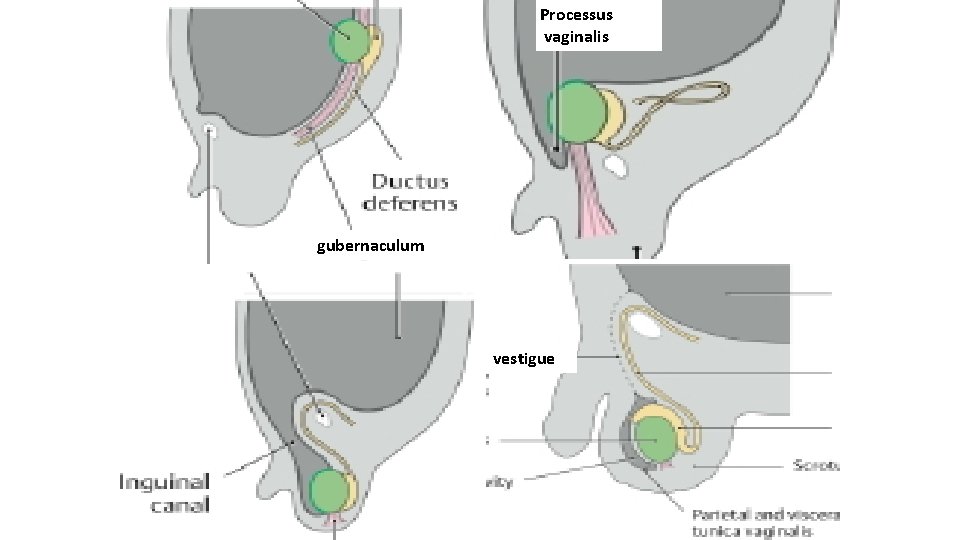
Processus vaginalis gubernaculum vestigue
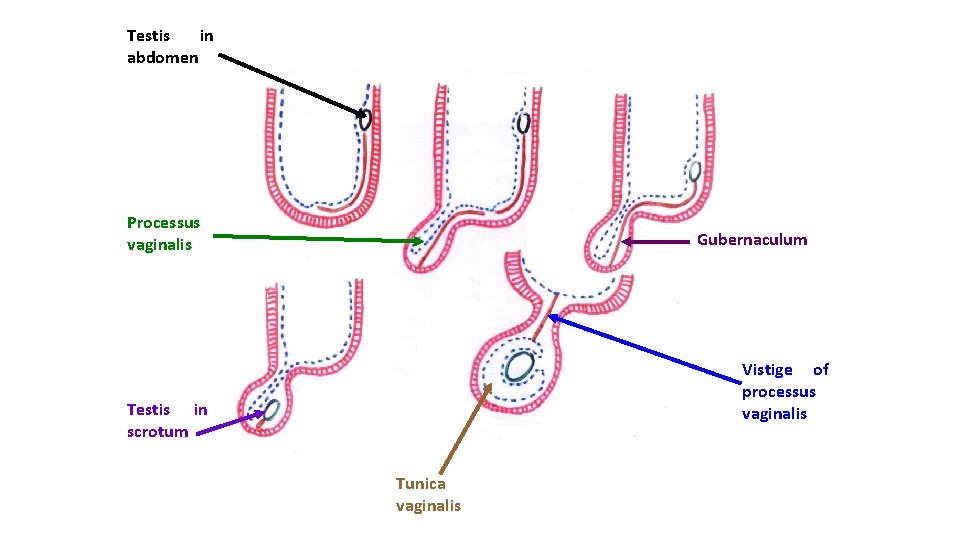
Testis in abdomen Processus vaginalis Gubernaculum Vistige of processus vaginalis Testis in scrotum Tunica vaginalis
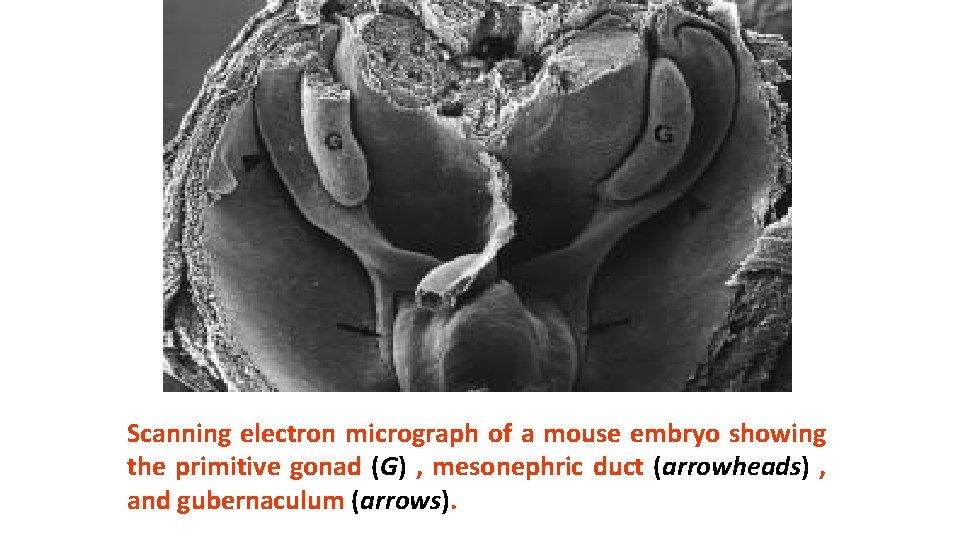
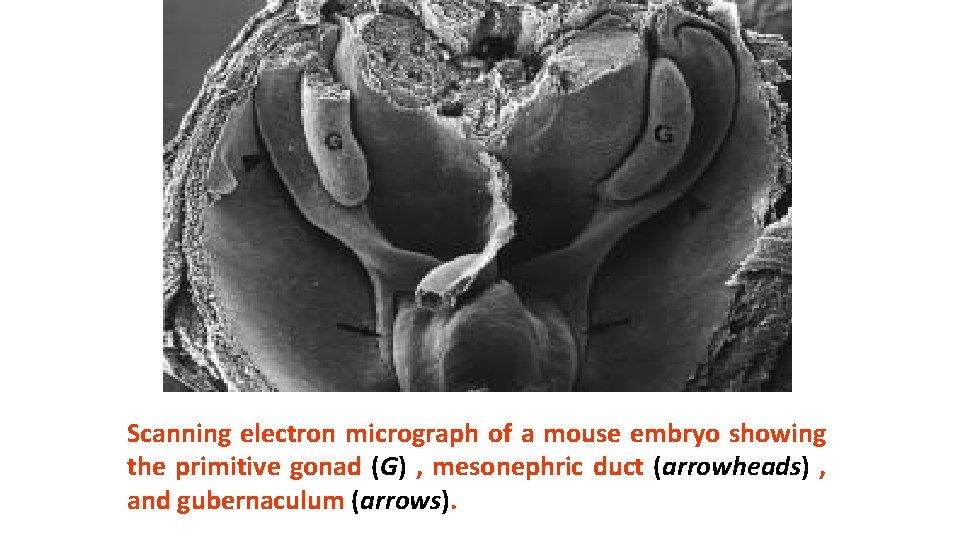
Scanning electron micrograph of a mouse embryo showing the primitive gonad (G) , mesonephric duct (arrowheads) , and gubernaculum (arrows).
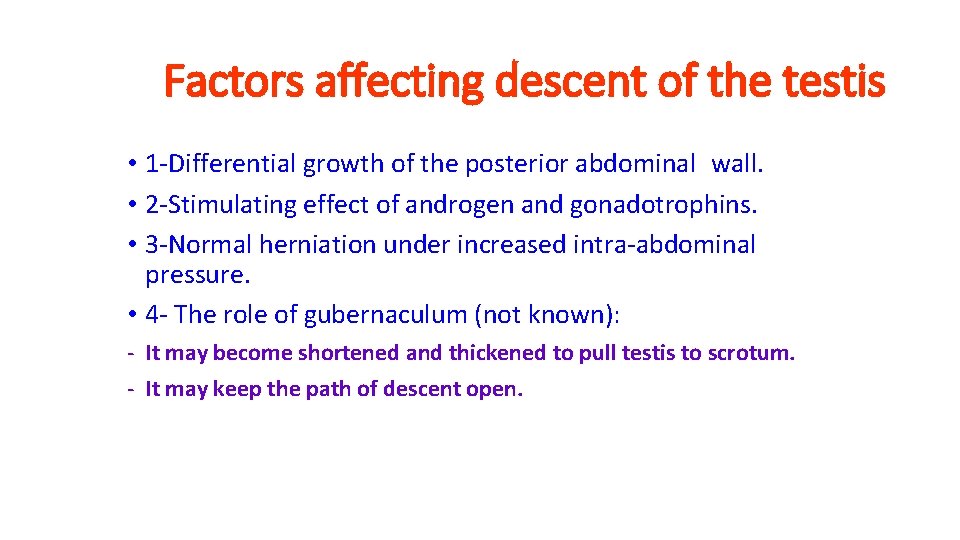
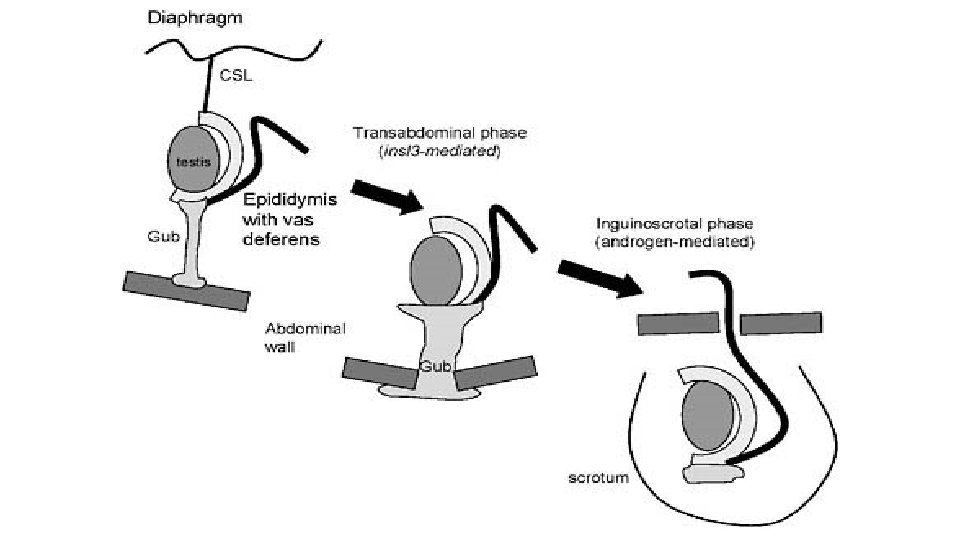
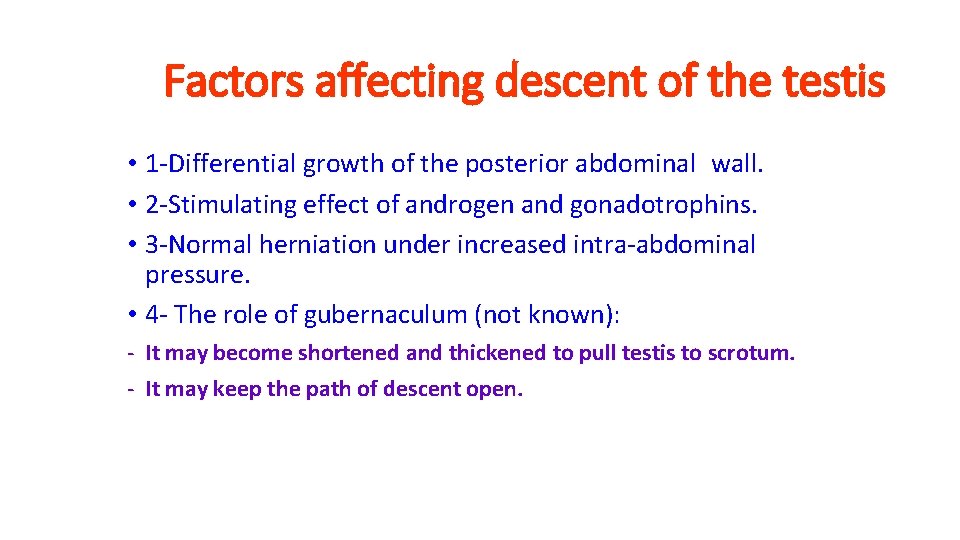
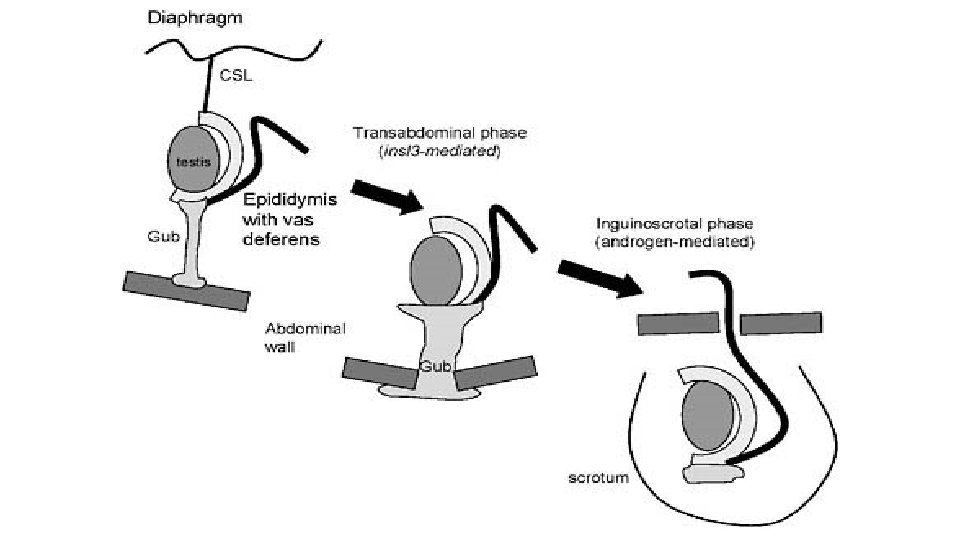
Factors affecting descent of the testis • 1 -Differential growth of the posterior abdominal wall. • 2 -Stimulating effect of androgen and gonadotrophins. • 3 -Normal herniation under increased intra-abdominal pressure. • 4 - The role of gubernaculum (not known): - It may become shortened and thickened to pull testis to scrotum. - It may keep the path of descent open.
Descent of the ovary
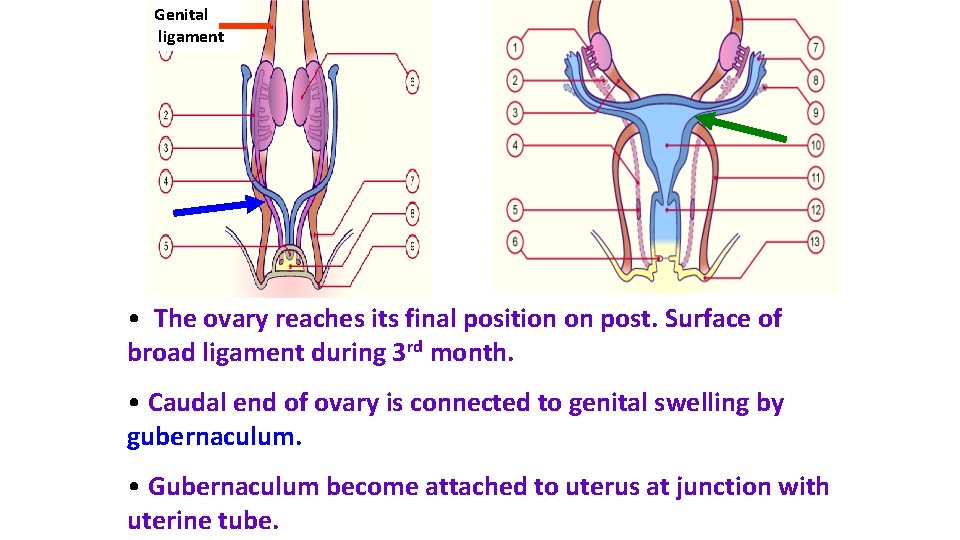
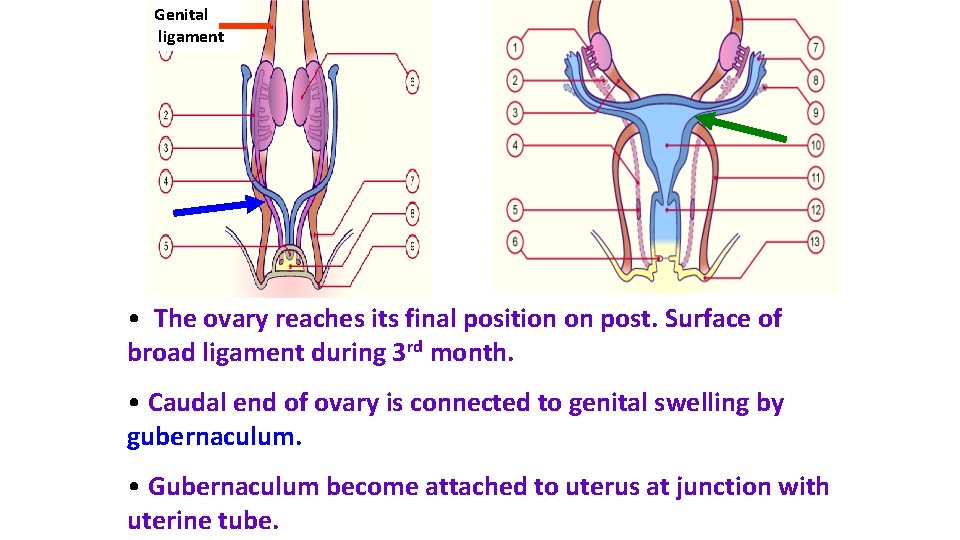
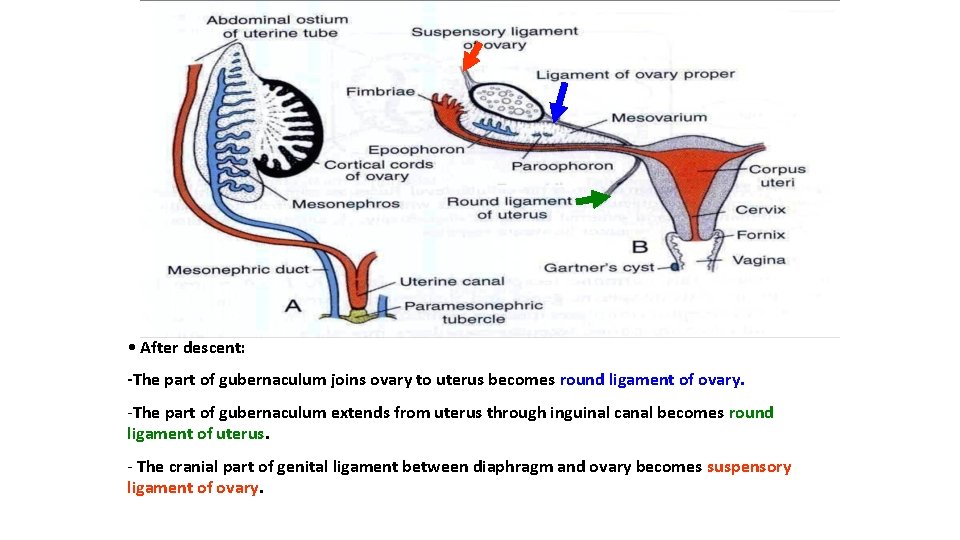
Genital ligament • The ovary reaches its final position on post. Surface of broad ligament during 3 rd month. • Caudal end of ovary is connected to genital swelling by gubernaculum. • Gubernaculum become attached to uterus at junction with uterine tube.
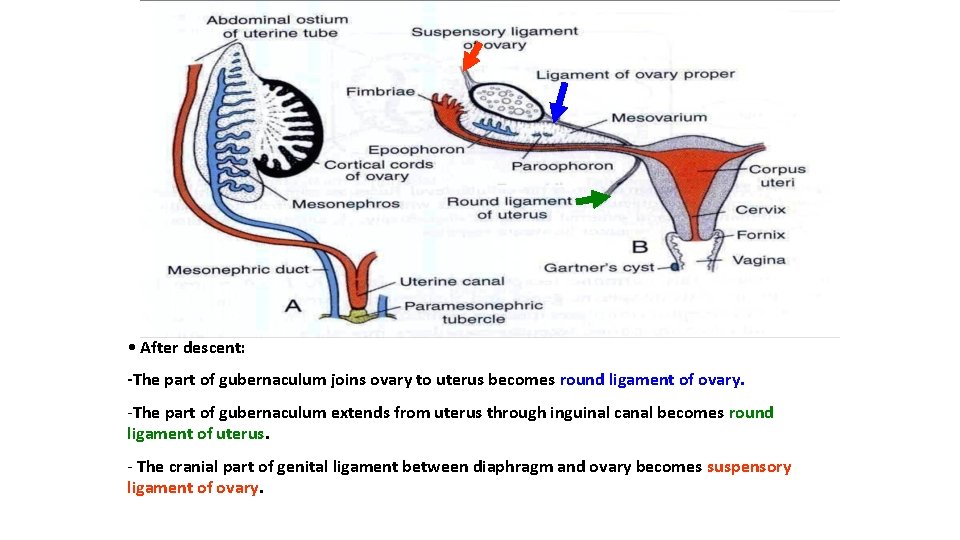
• After descent: -The part of gubernaculum joins ovary to uterus becomes round ligament of ovary. -The part of gubernaculum extends from uterus through inguinal canal becomes round ligament of uterus. - The cranial part of genital ligament between diaphragm and ovary becomes suspensory ligament of ovary.
Congenital anomalies of male genital system
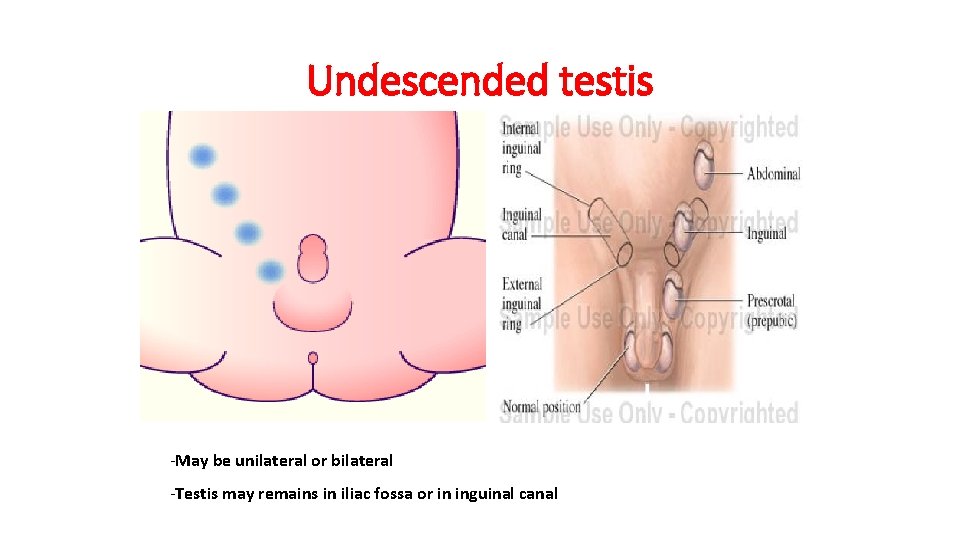
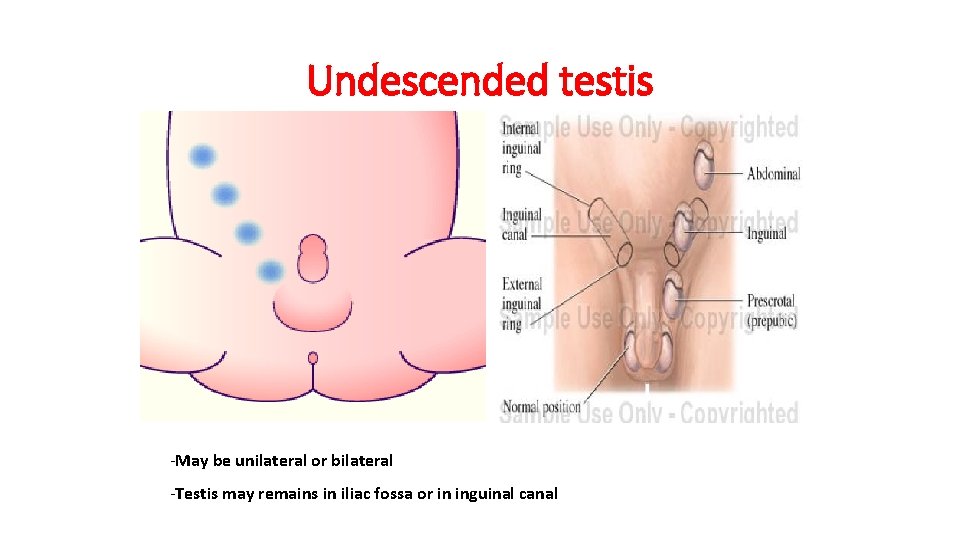
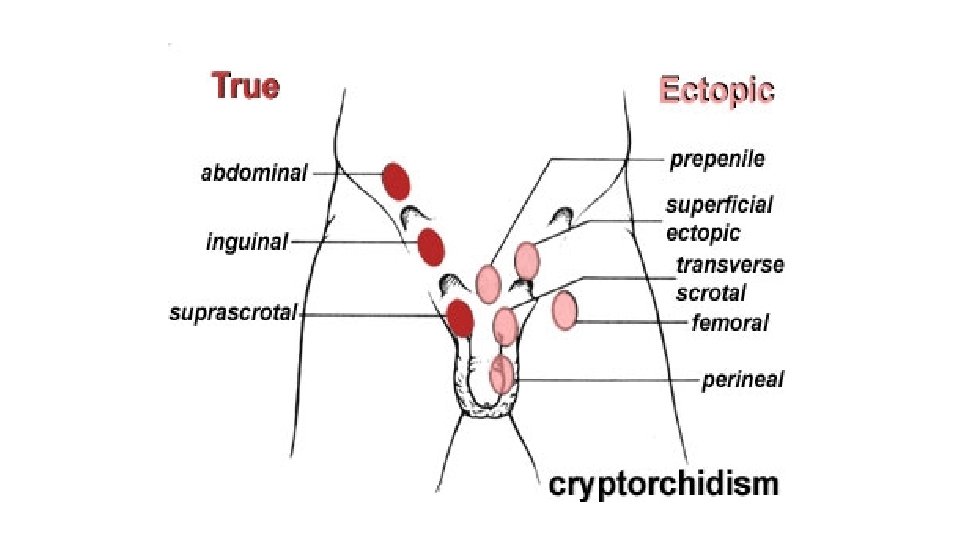
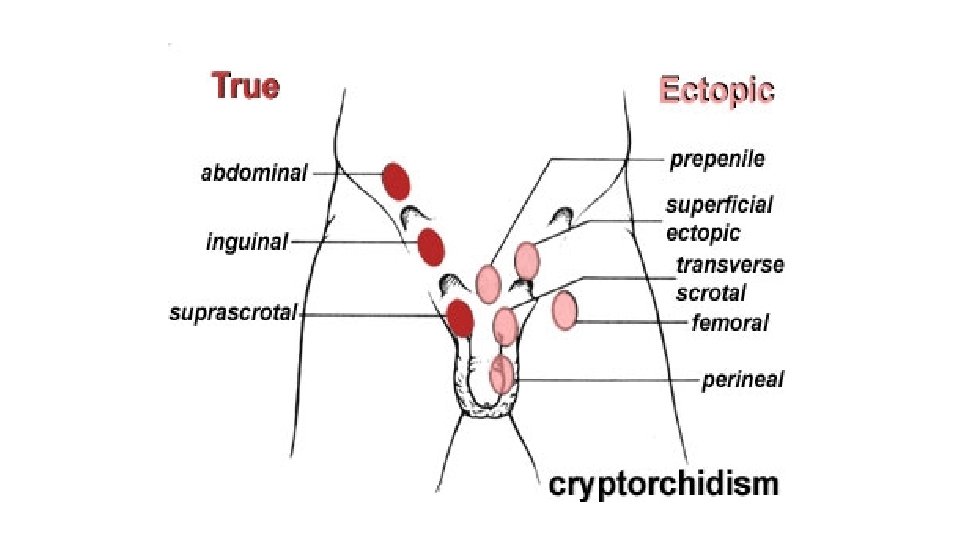
Undescended testis -May be unilateral or bilateral -Testis may remains in iliac fossa or in inguinal canal
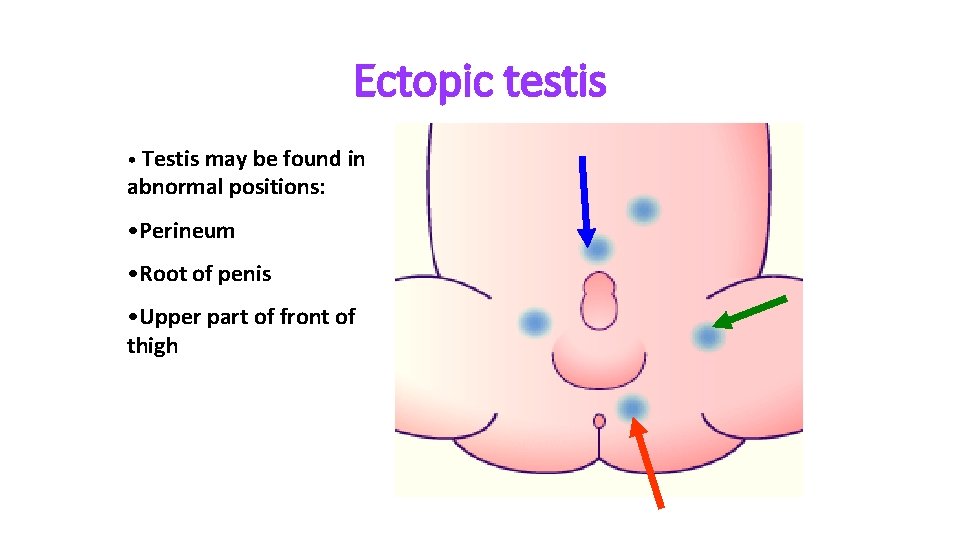
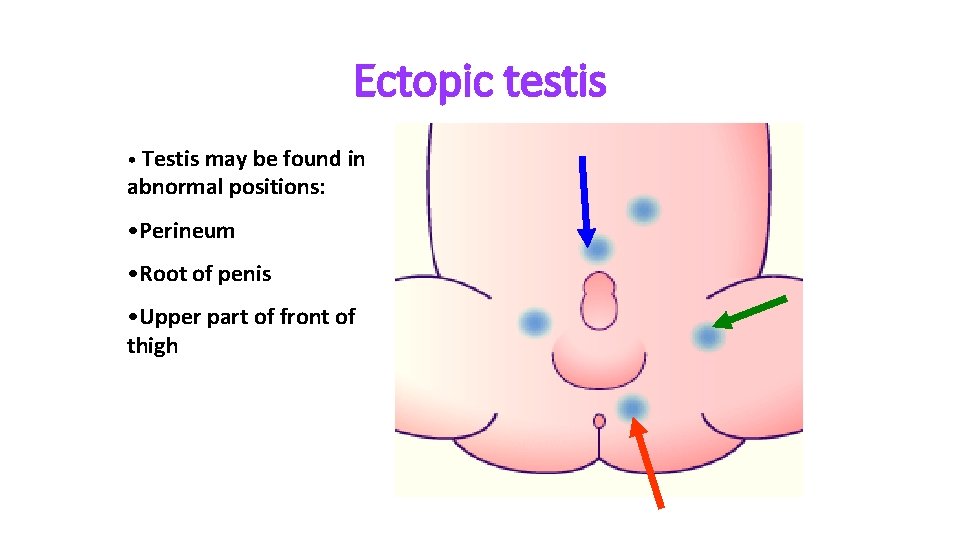
Ectopic testis • Testis may be found in abnormal positions: • Perineum • Root of penis • Upper part of front of thigh
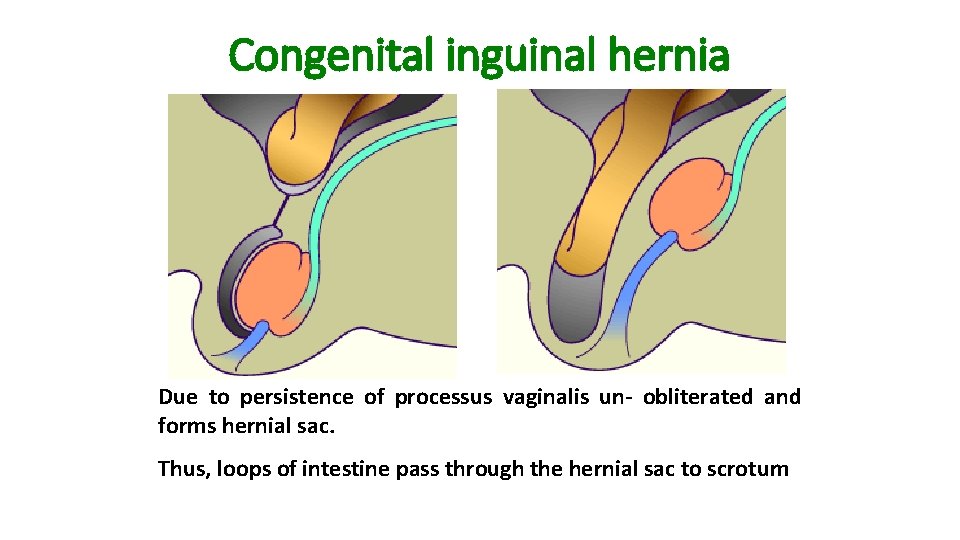
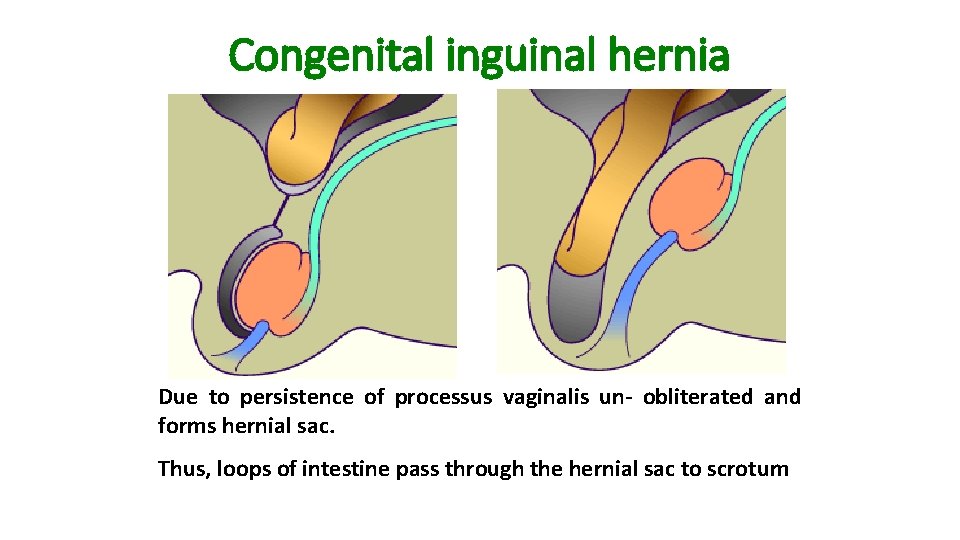
Congenital inguinal hernia Due to persistence of processus vaginalis un- obliterated and forms hernial sac. Thus, loops of intestine pass through the hernial sac to scrotum
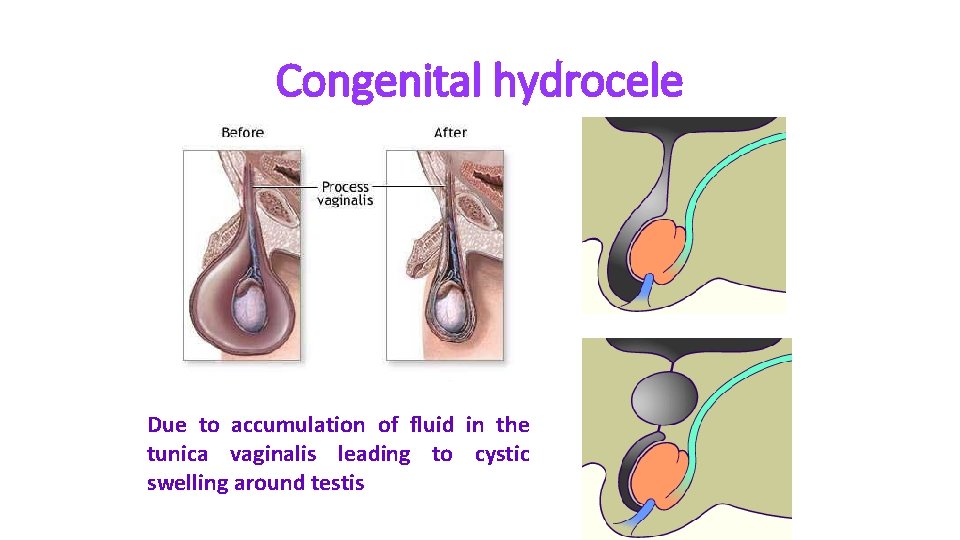
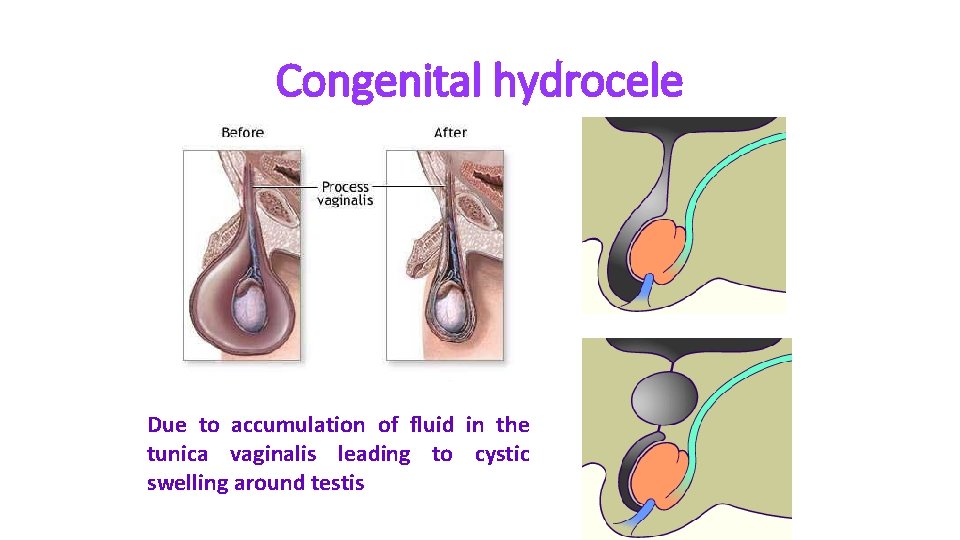
Congenital hydrocele Due to accumulation of fluid in the tunica vaginalis leading to cystic swelling around testis
Development of the external genitalia
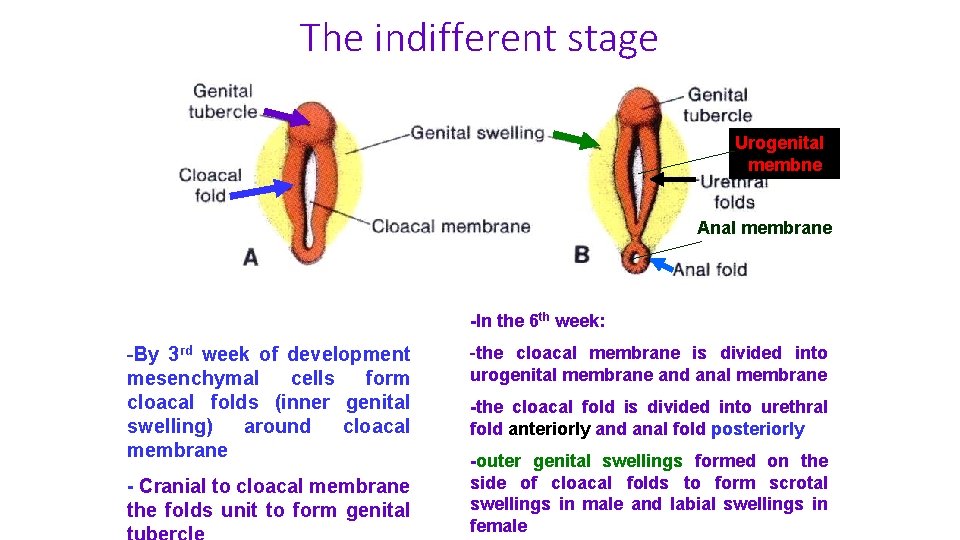
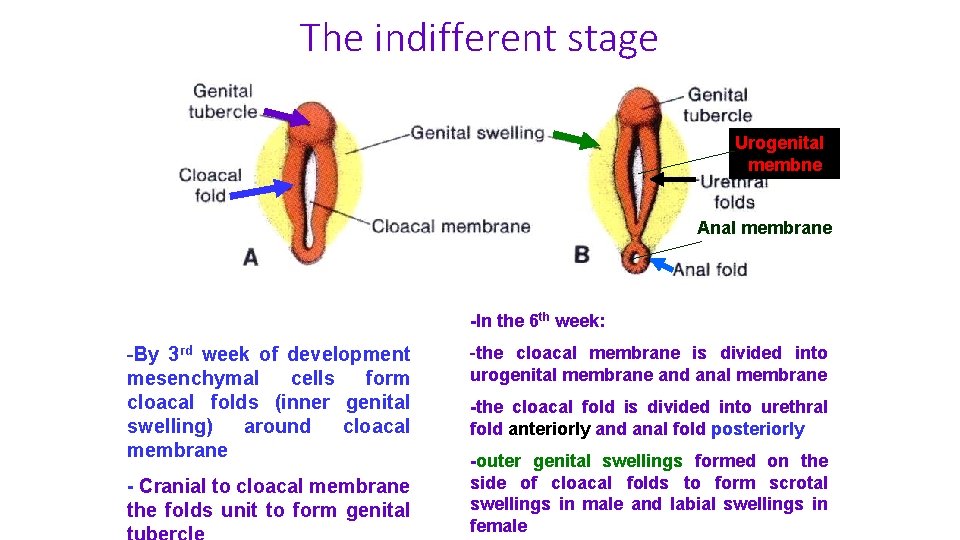
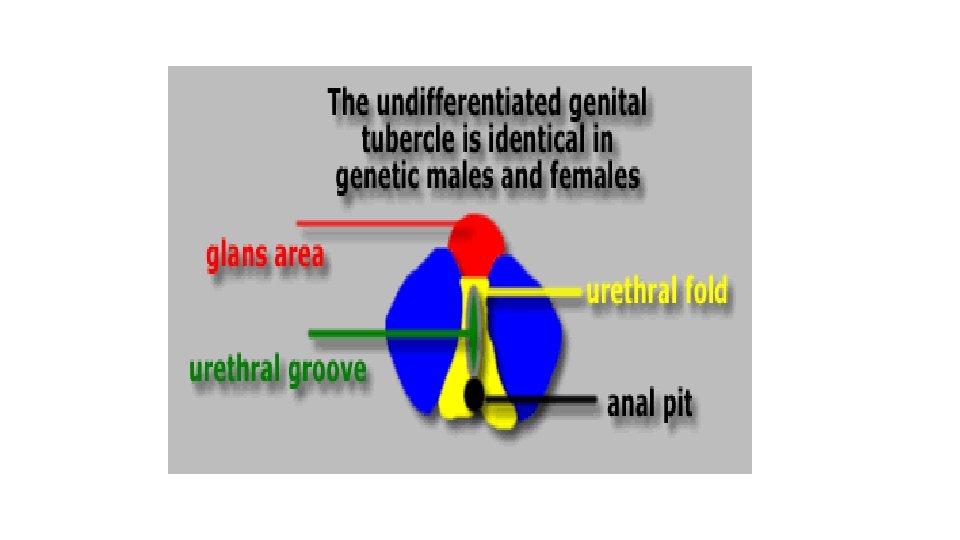
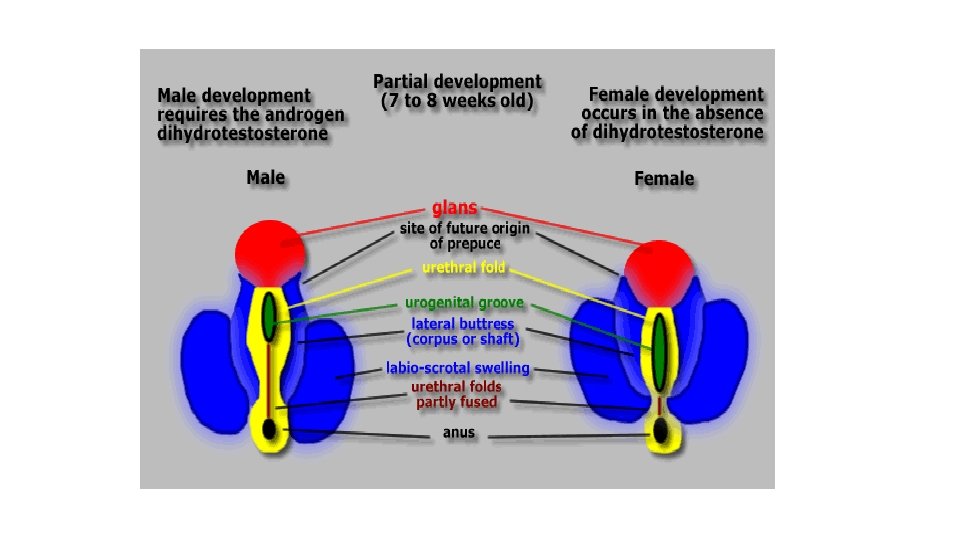
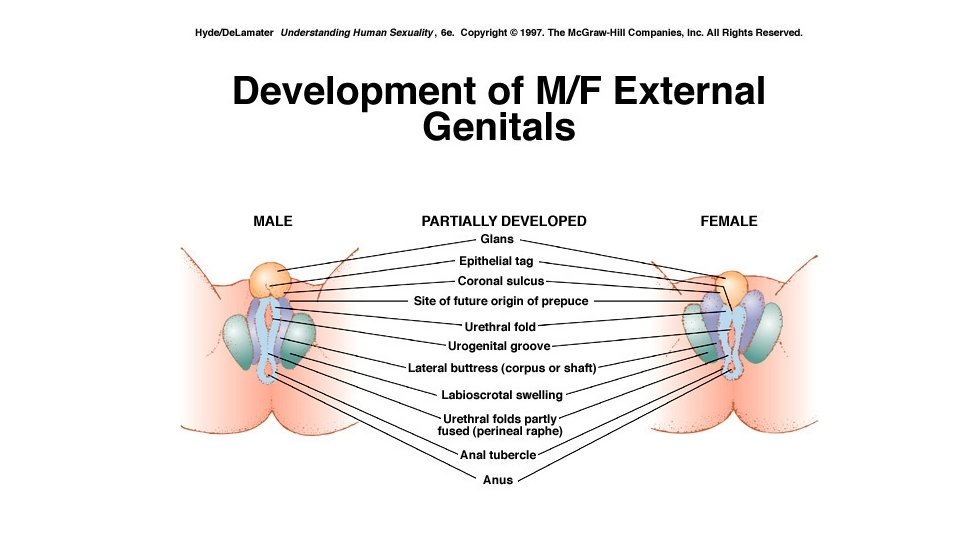
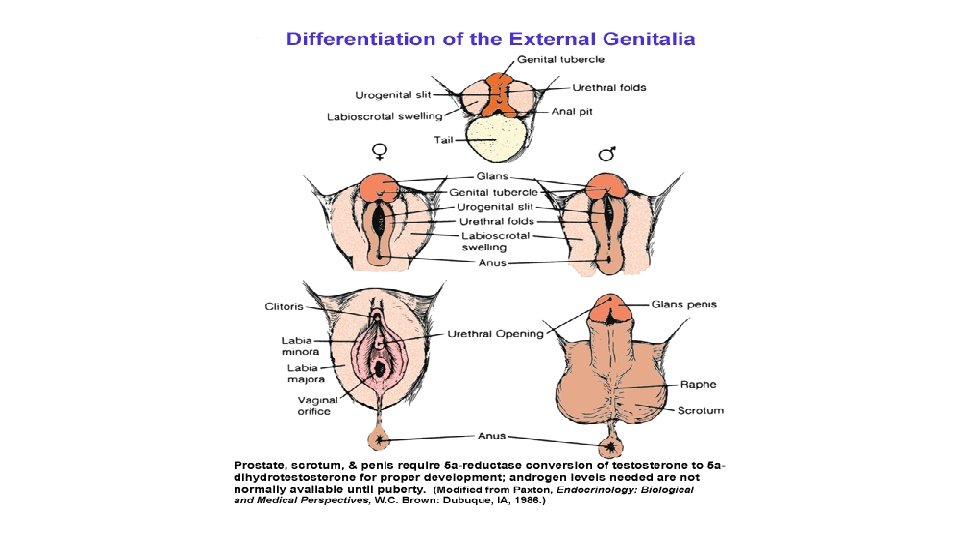
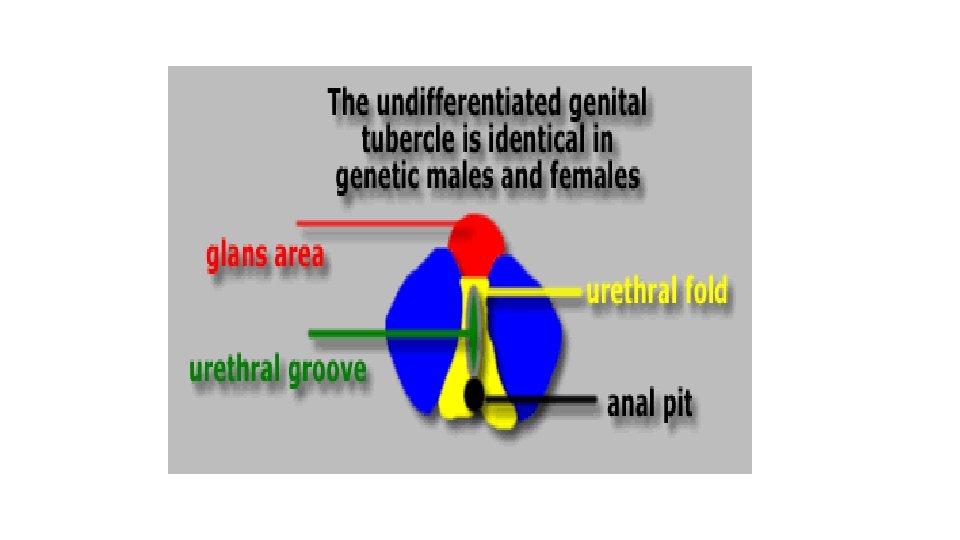
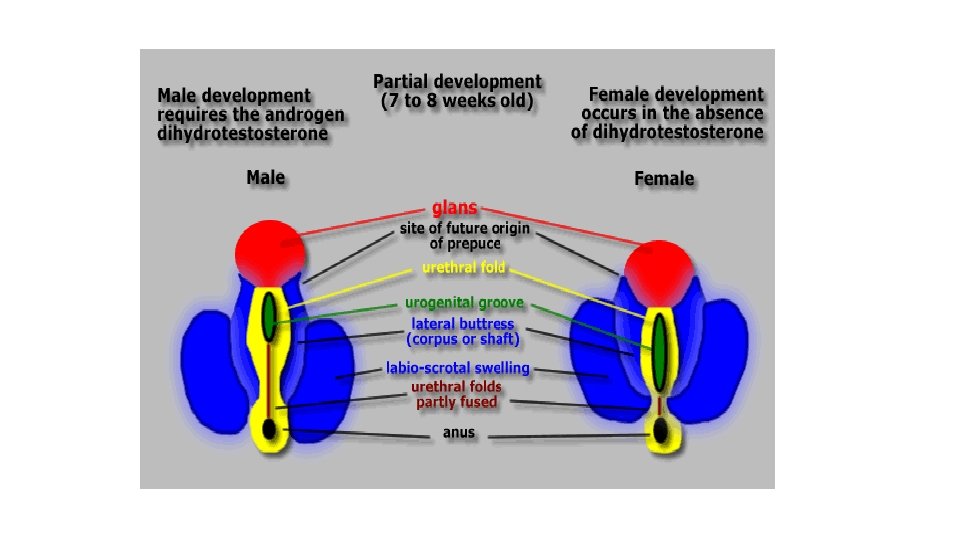
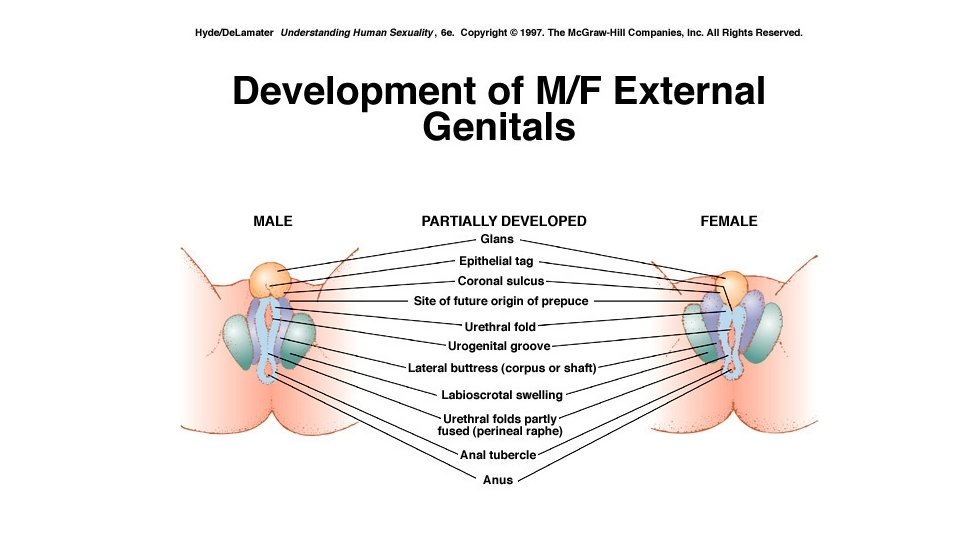
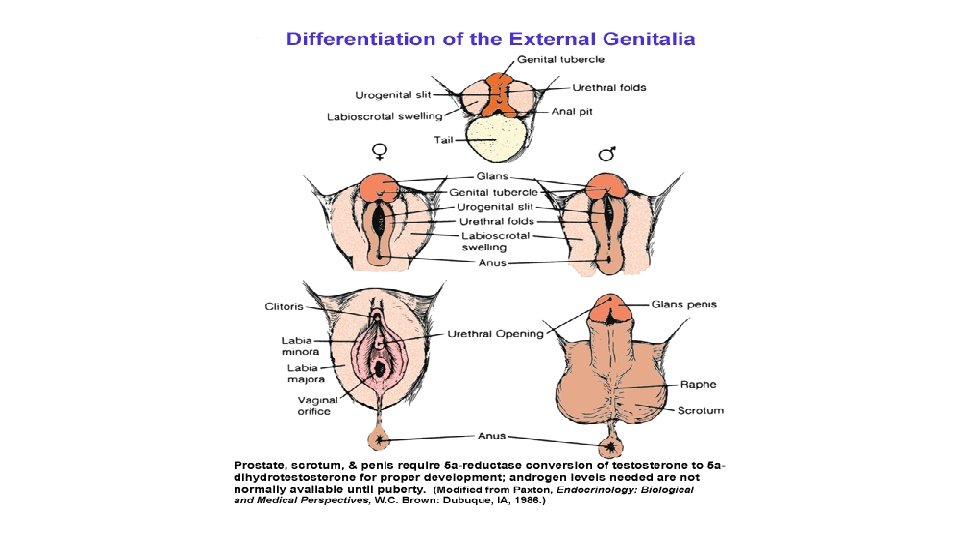
The indifferent stage Urogenital membne Anal membrane -In the 6 th week: -By 3 rd week of development mesenchymal cells form cloacal folds (inner genital swelling) around cloacal membrane - Cranial to cloacal membrane the folds unit to form genital -the cloacal membrane is divided into urogenital membrane and anal membrane -the cloacal fold is divided into urethral fold anteriorly and anal fold posteriorly -outer genital swellings formed on the side of cloacal folds to form scrotal swellings in male and labial swellings in female
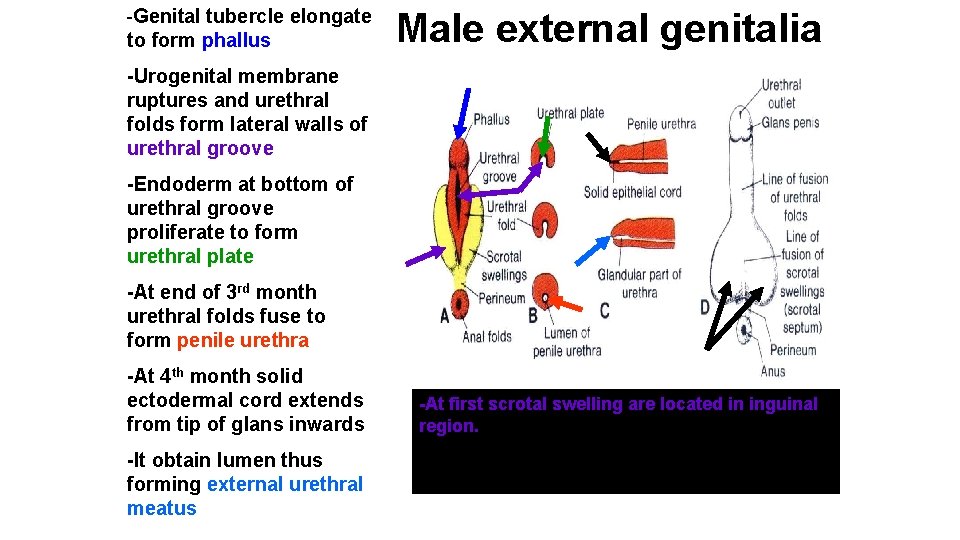
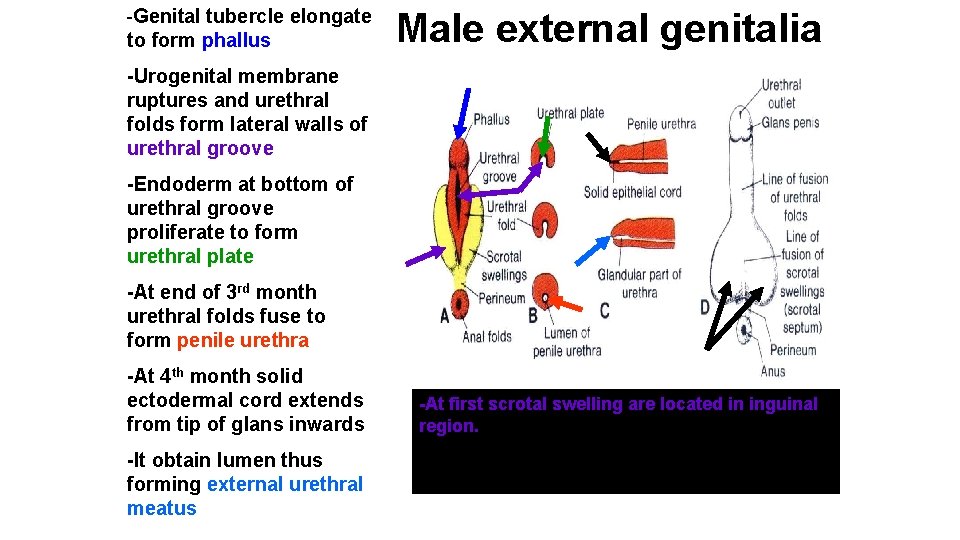
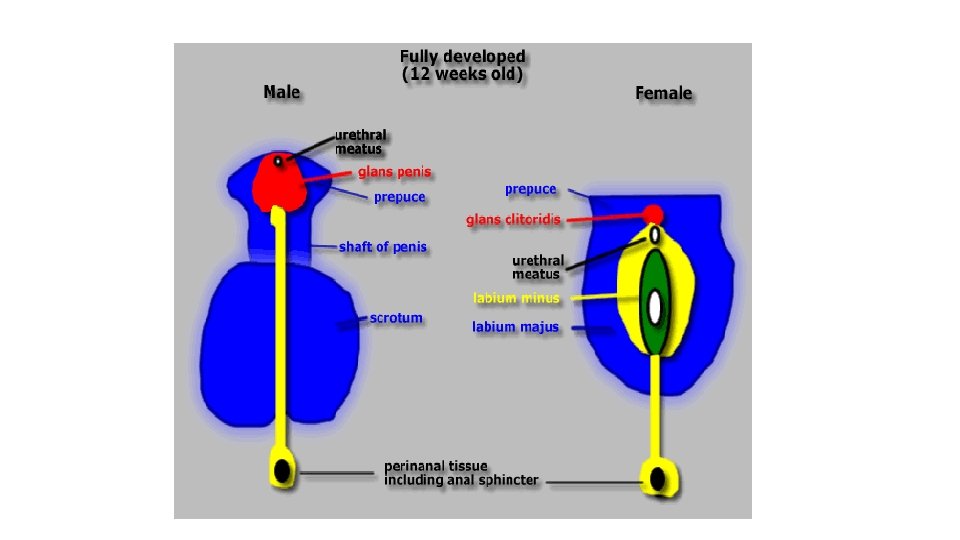
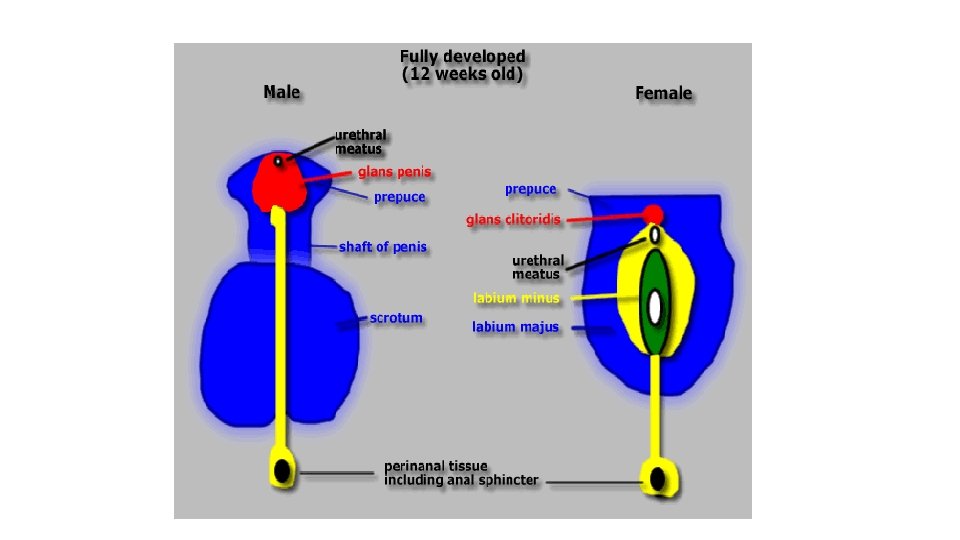
-Genital tubercle elongate to form phallus Male external genitalia -Urogenital membrane ruptures and urethral folds form lateral walls of urethral groove -Endoderm at bottom of urethral groove proliferate to form urethral plate -At end of 3 rd month urethral folds fuse to form penile urethra -At 4 th month solid ectodermal cord extends from tip of glans inwards -It obtain lumen thus forming external urethral meatus -At first scrotal swelling are located in inguinal region. -Then they move caudally and each swelling forms half of scrotum
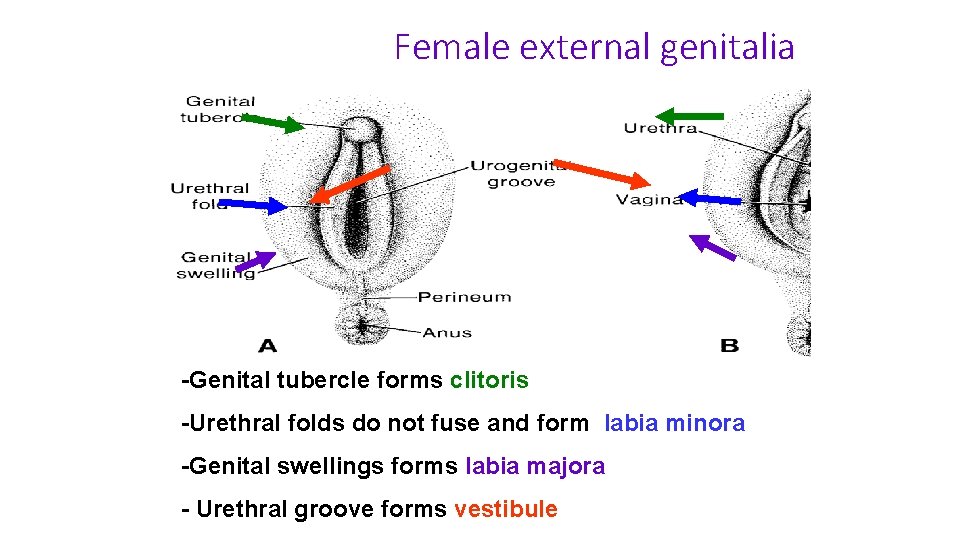
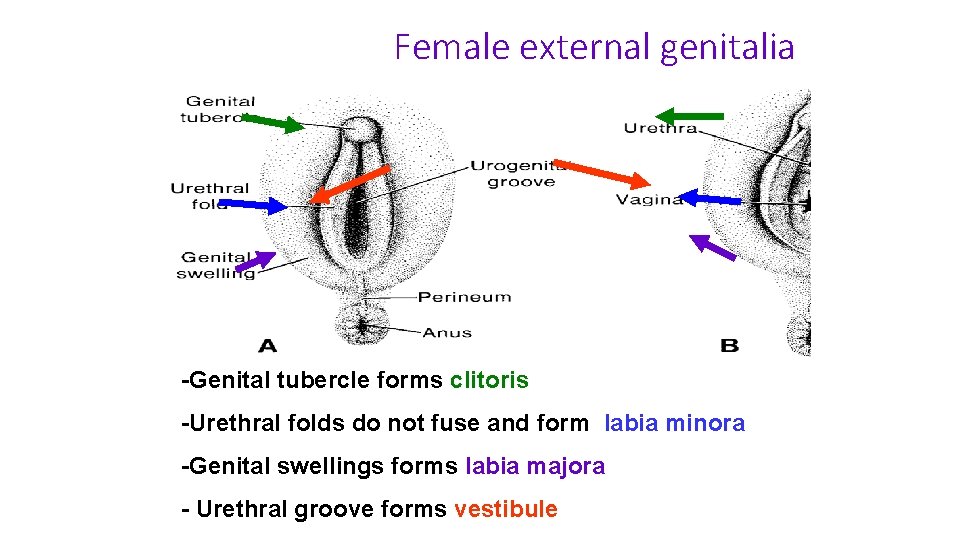
Female external genitalia -Genital tubercle forms clitoris -Urethral folds do not fuse and form labia minora -Genital swellings forms labia majora - Urethral groove forms vestibule
Congenital anomalies of the male urethra
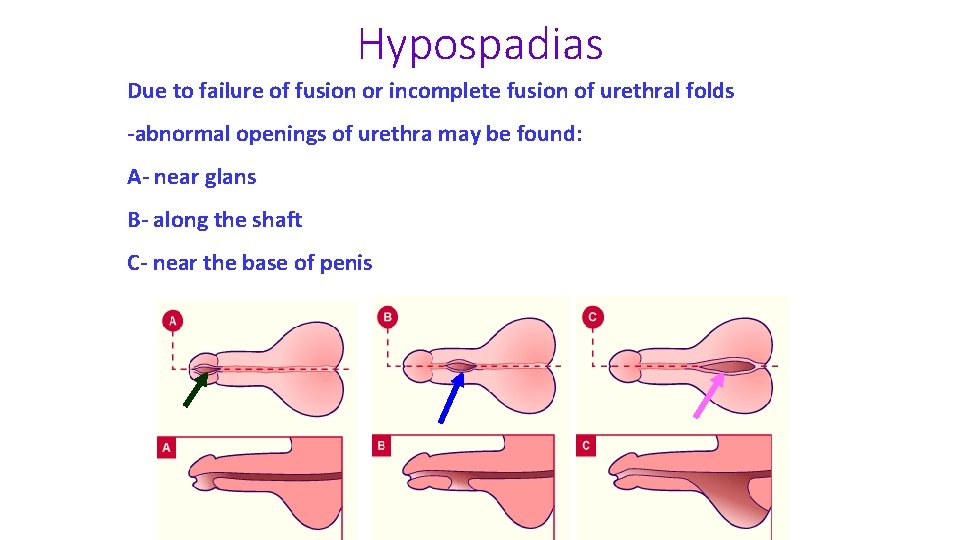
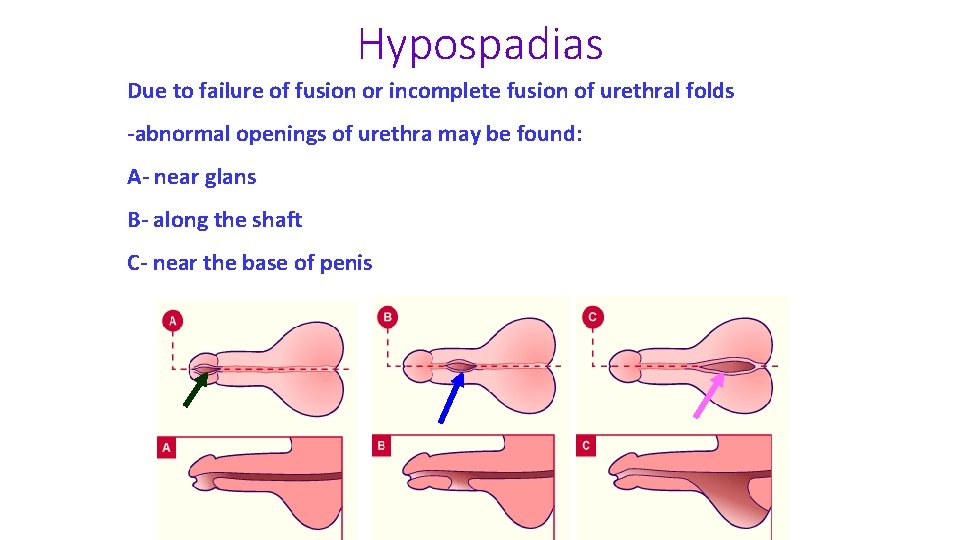
Hypospadias Due to failure of fusion or incomplete fusion of urethral folds -abnormal openings of urethra may be found: A- near glans B- along the shaft C- near the base of penis
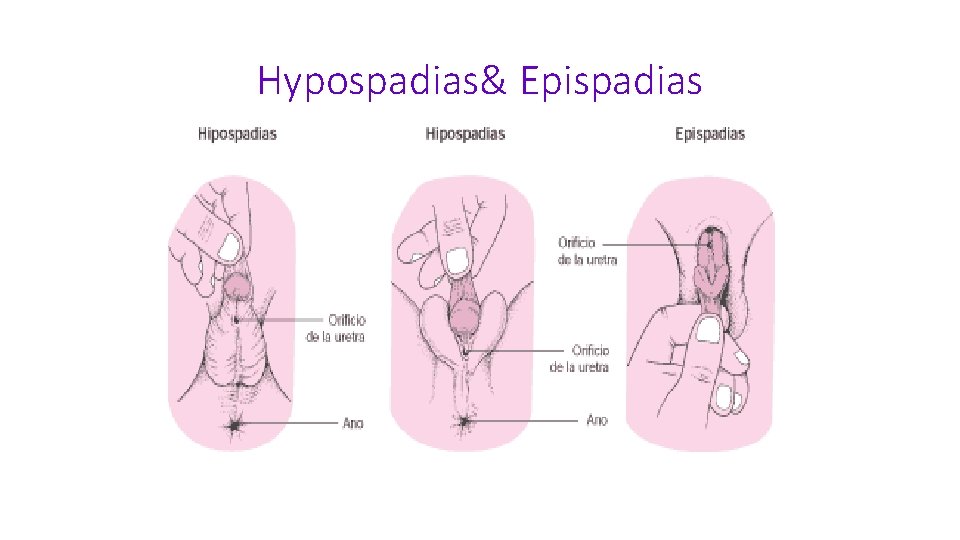
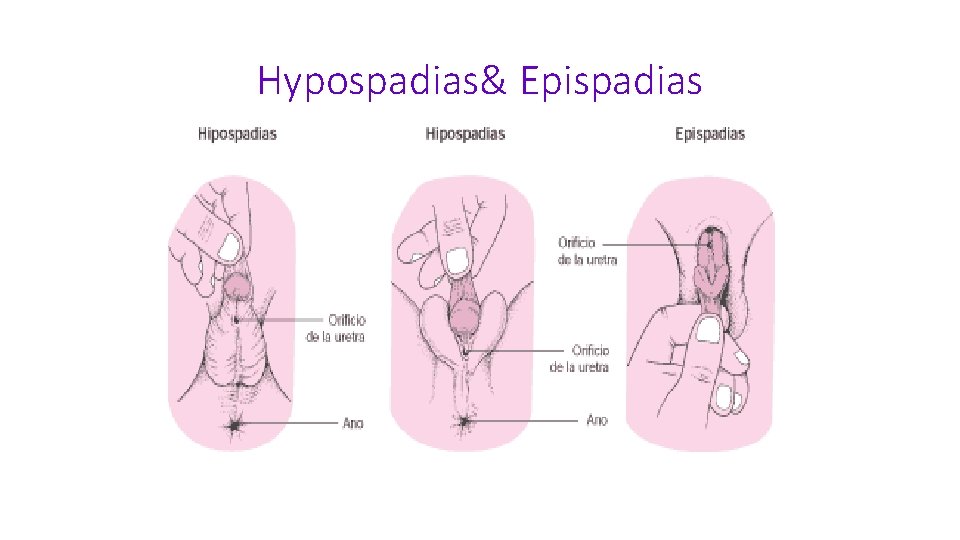
Hypospadias& Epispadias
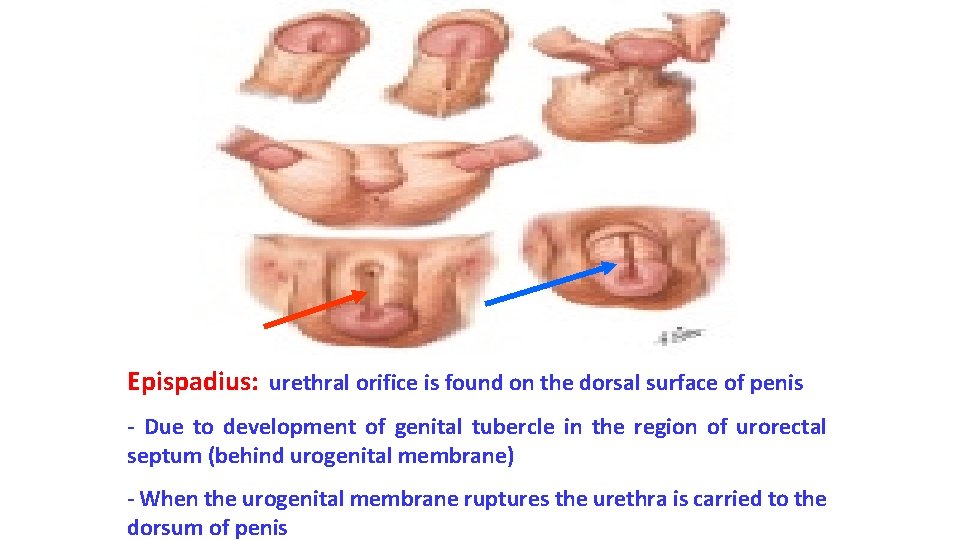
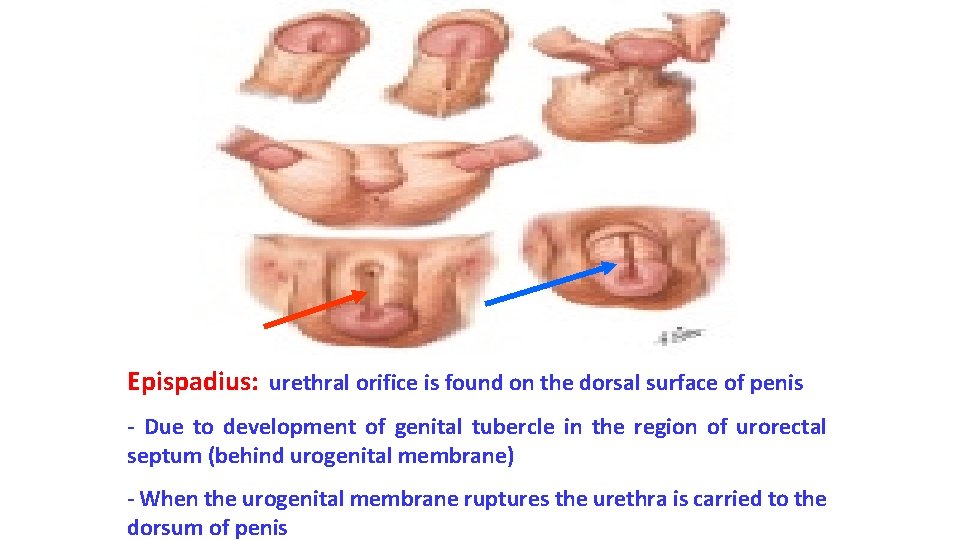
Epispadius: urethral orifice is found on the dorsal surface of penis - Due to development of genital tubercle in the region of urorectal septum (behind urogenital membrane) - When the urogenital membrane ruptures the urethra is carried to the dorsum of penis

Thank you