Development of Respiratory System 5 processes share in

- Slides: 49
Development of Respiratory System
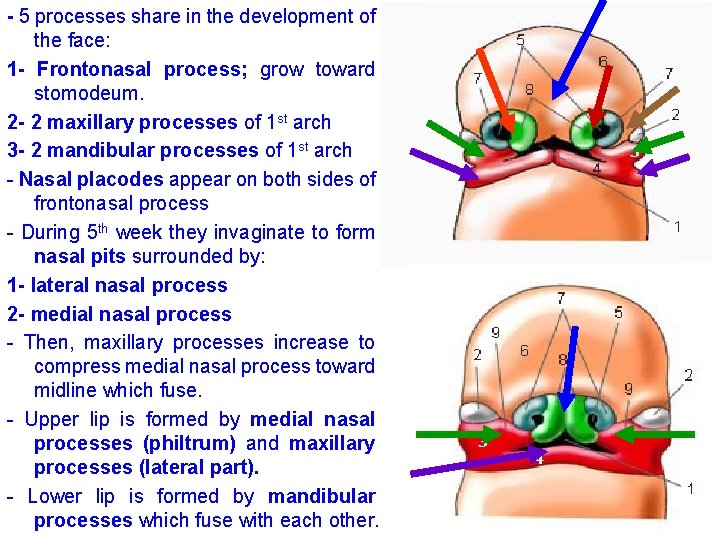
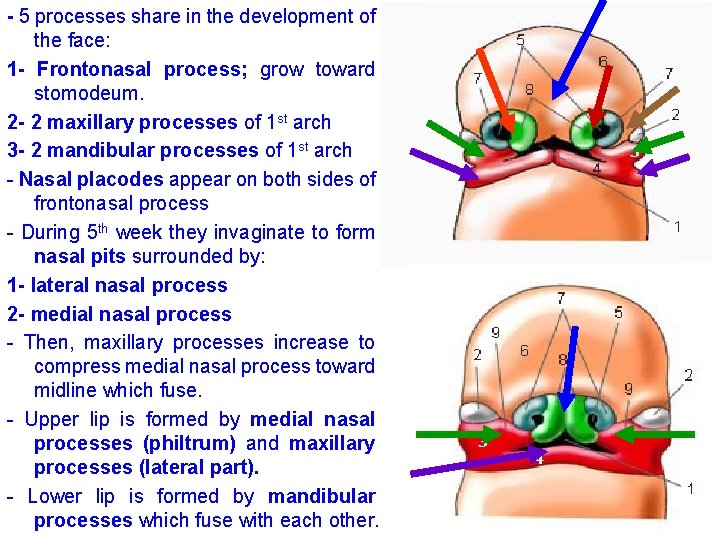
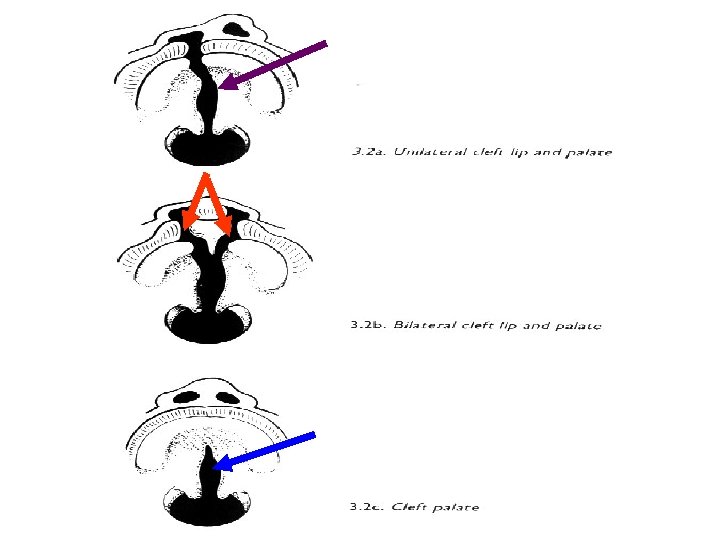
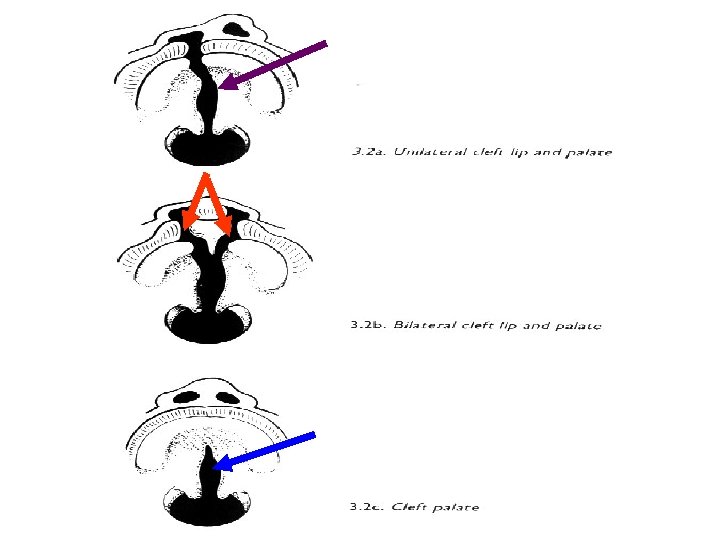
- 5 processes share in the development of the face: 1 - Frontonasal process; grow toward stomodeum. 2 - 2 maxillary processes of 1 st arch 3 - 2 mandibular processes of 1 st arch - Nasal placodes appear on both sides of frontonasal process - During 5 th week they invaginate to form nasal pits surrounded by: 1 - lateral nasal process 2 - medial nasal process - Then, maxillary processes increase to compress medial nasal process toward midline which fuse. - Upper lip is formed by medial nasal processes (philtrum) and maxillary processes (lateral part). - Lower lip is formed by mandibular processes which fuse with each other.
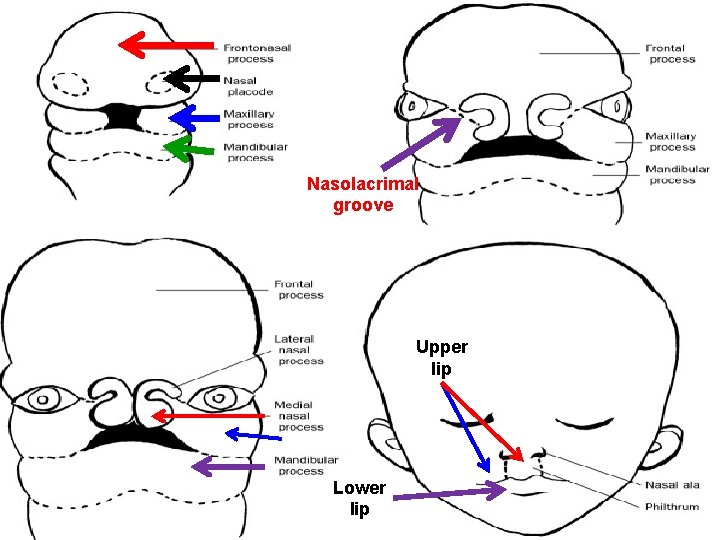
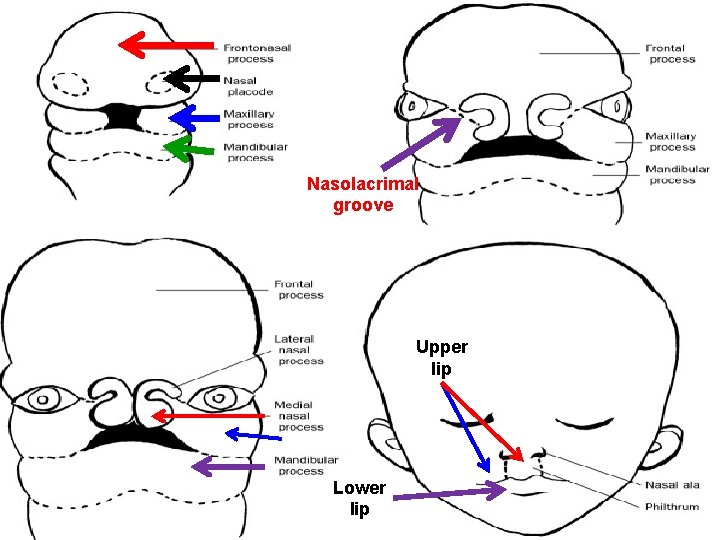
Nasolacrimal groove Upper lip Lower lip
- Maxillary and lateral nasal processes are separated by nasolacrimal groove. - The ectoderm in the floor of groove forms a solid ectodermal cord. - The ectodermal cord detaches from the surface ectoderm, then the two processes fuse with each other. - Then, canalization occurs in the cord to form nasolacrimal duct and its upper part dilate to form the lacrimal sac. - Maxillary processes enlarge to form cheeks and maxilla.
Nose develops from: 1 - frontonasal process forms bridge 2 - fused medial nasal processes forms crest and tip 3 - lateral nasal process forms alae
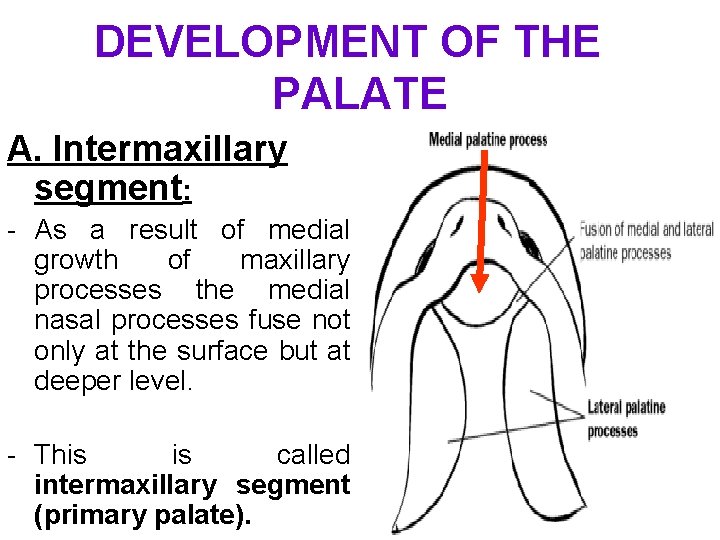
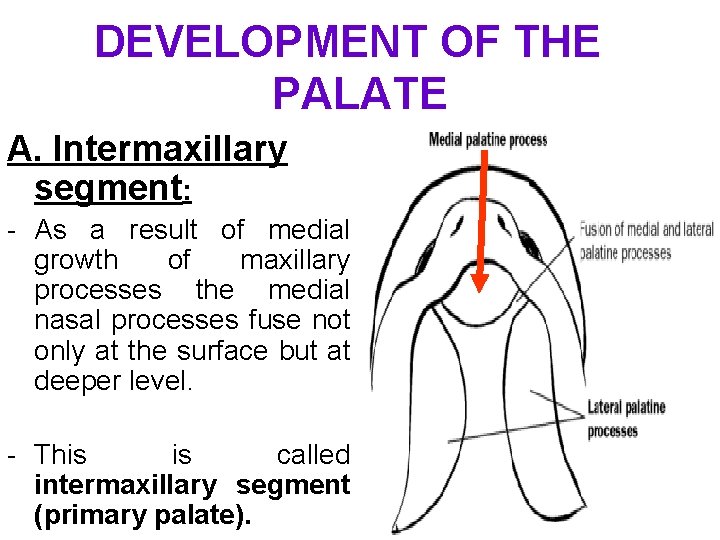
DEVELOPMENT OF THE PALATE A. Intermaxillary segment: - As a result of medial growth of maxillary processes the medial nasal processes fuse not only at the surface but at deeper level. - This is called intermaxillary segment (primary palate).
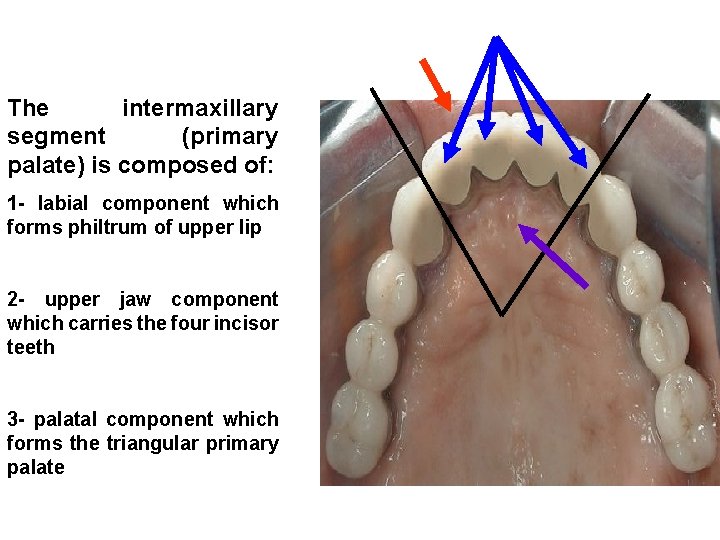
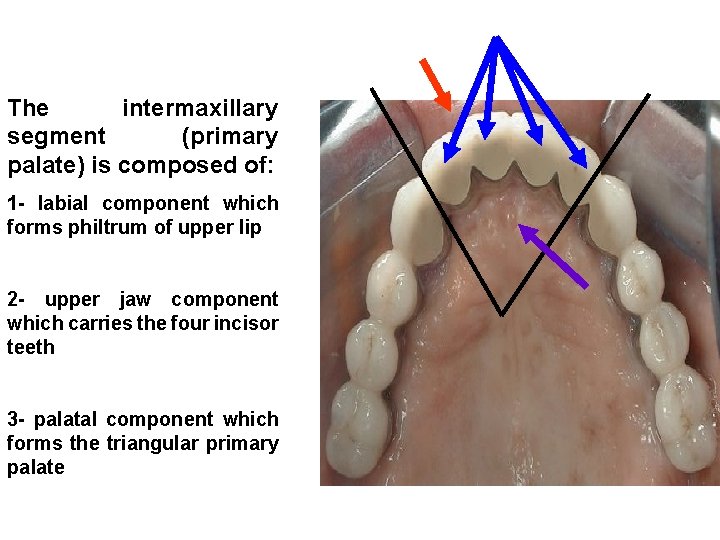
The intermaxillary segment (primary palate) is composed of: 1 - labial component which forms philtrum of upper lip 2 - upper jaw component which carries the four incisor teeth 3 - palatal component which forms the triangular primary palate
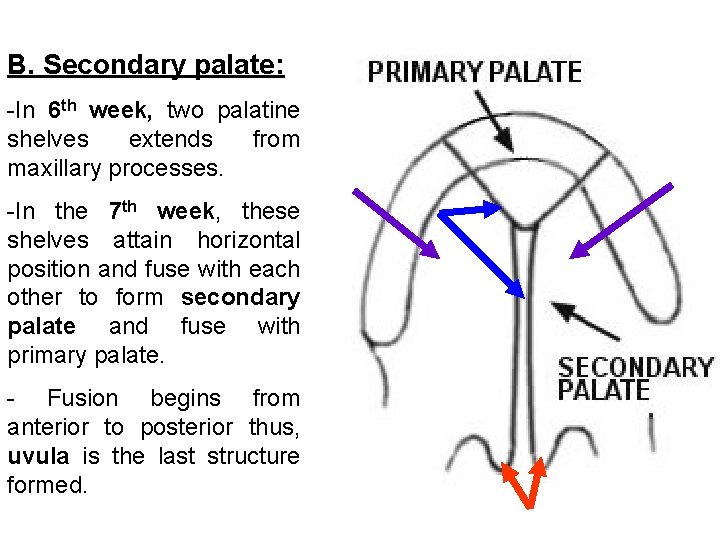
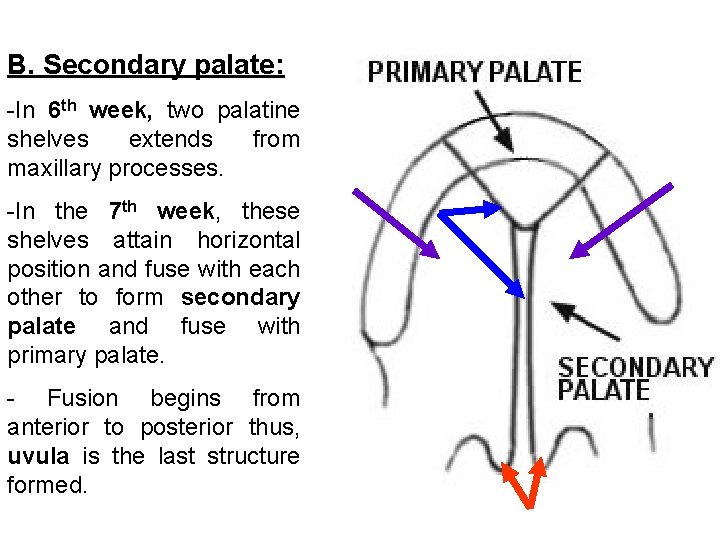
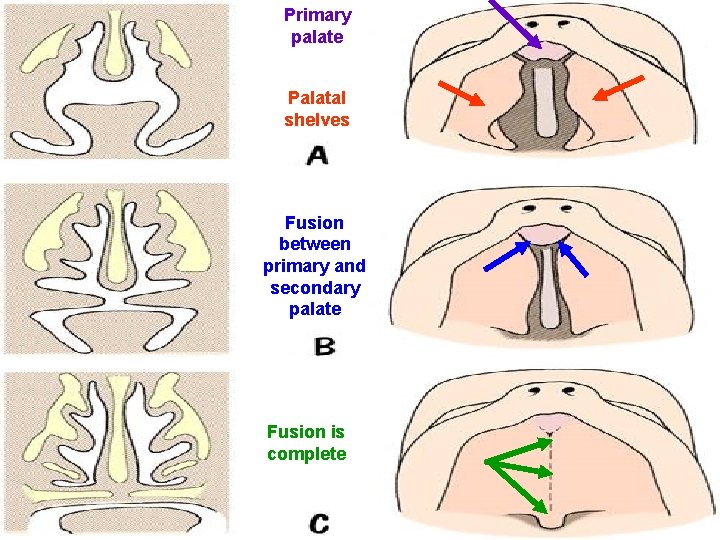
B. Secondary palate: -In 6 th week, two palatine shelves extends from maxillary processes. -In the 7 th week, these shelves attain horizontal position and fuse with each other to form secondary palate and fuse with primary palate. - Fusion begins from anterior to posterior thus, uvula is the last structure formed.
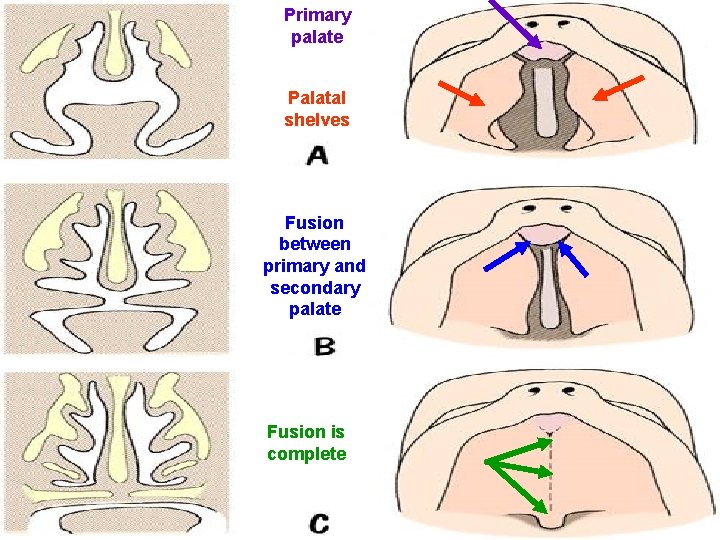
Primary palate Palatal shelves Fusion between primary and secondary palate Fusion is complete
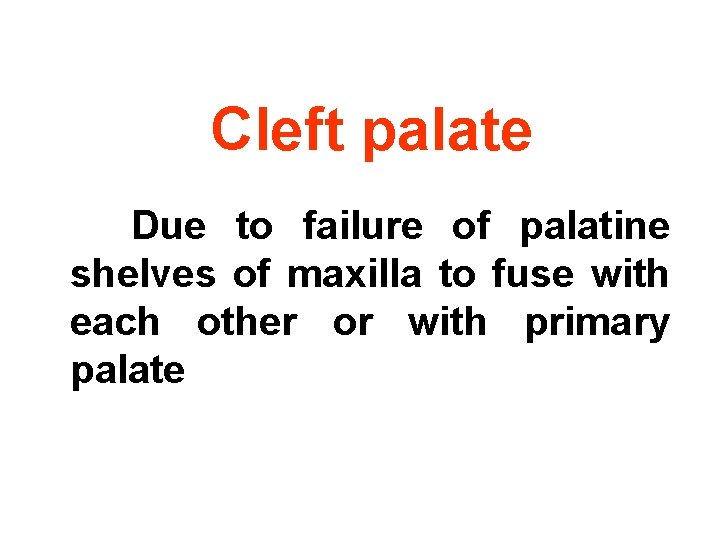
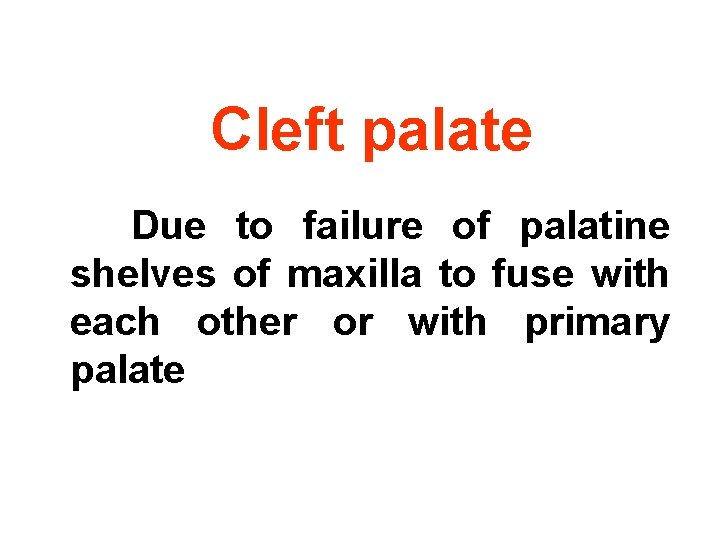
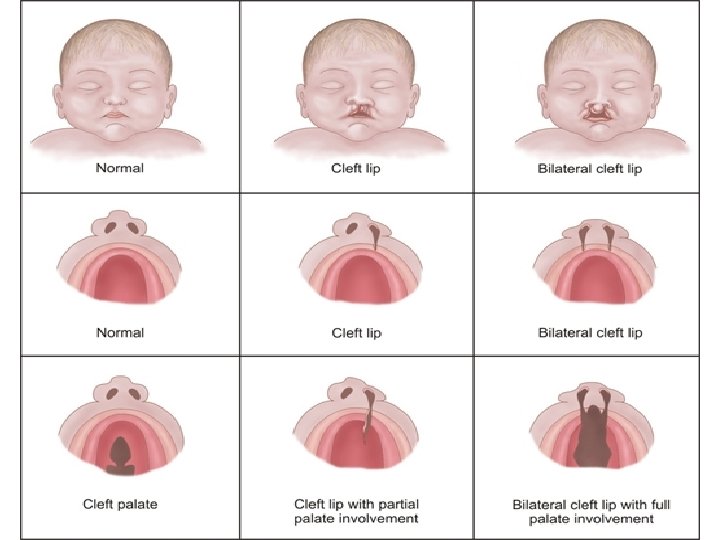
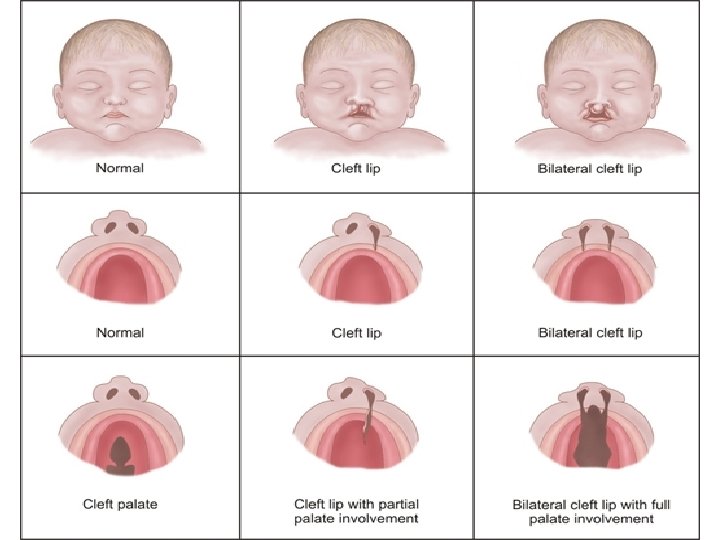
Cleft palate Due to failure of palatine shelves of maxilla to fuse with each other or with primary palate
• During 5 th week, the mesoderm on each side of the pharynx shows an anteroposterior segmentation into 6 segments called pharyngeal arches.
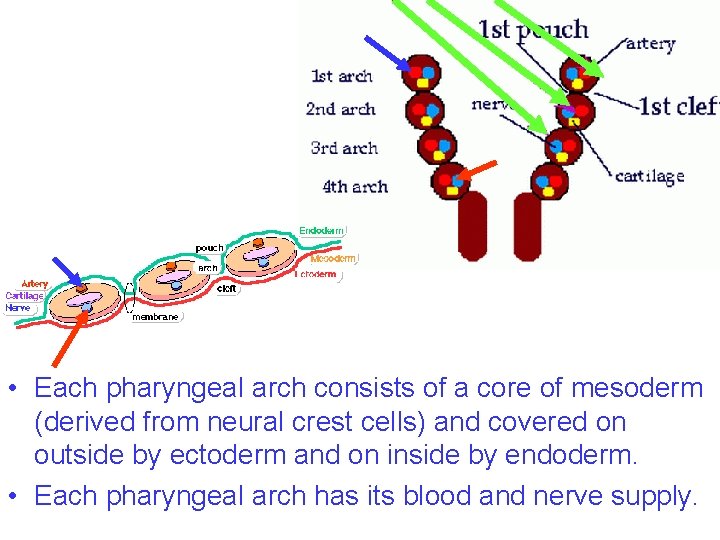
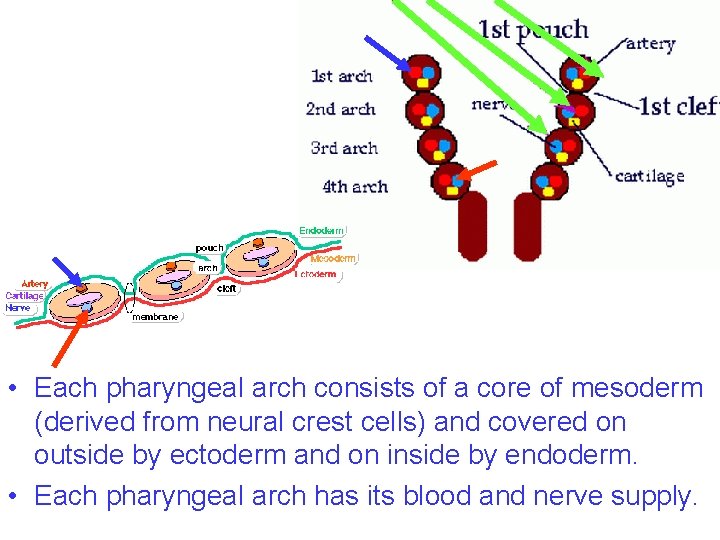
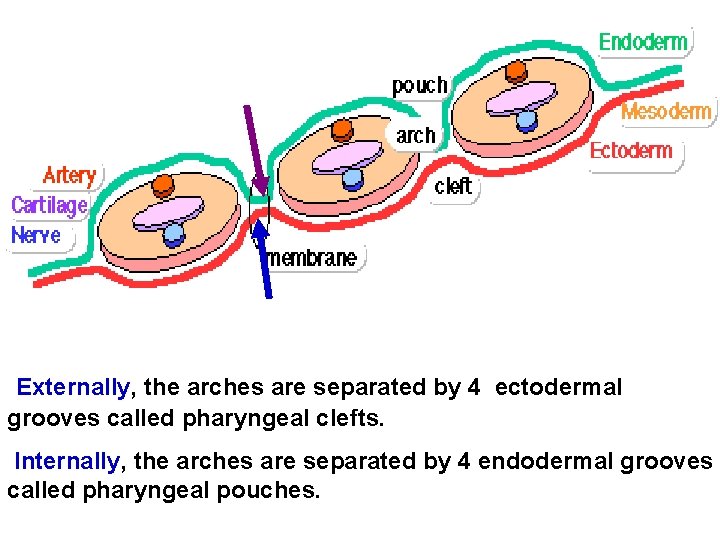
• Each pharyngeal arch consists of a core of mesoderm (derived from neural crest cells) and covered on outside by ectoderm and on inside by endoderm. • Each pharyngeal arch has its blood and nerve supply.
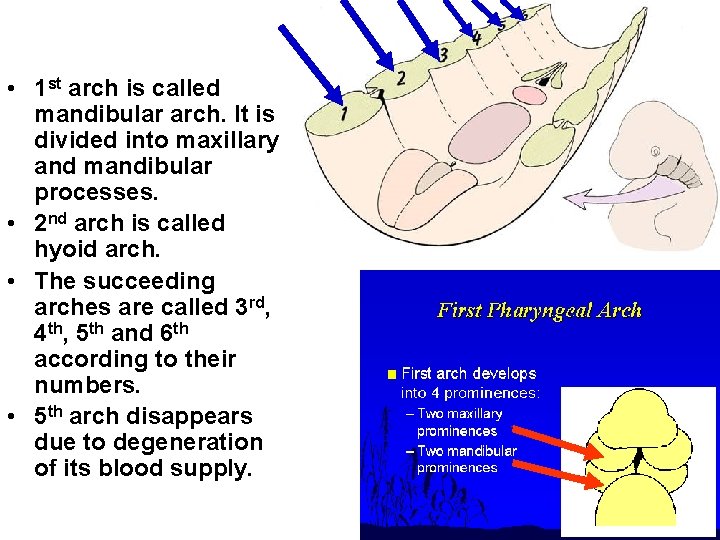
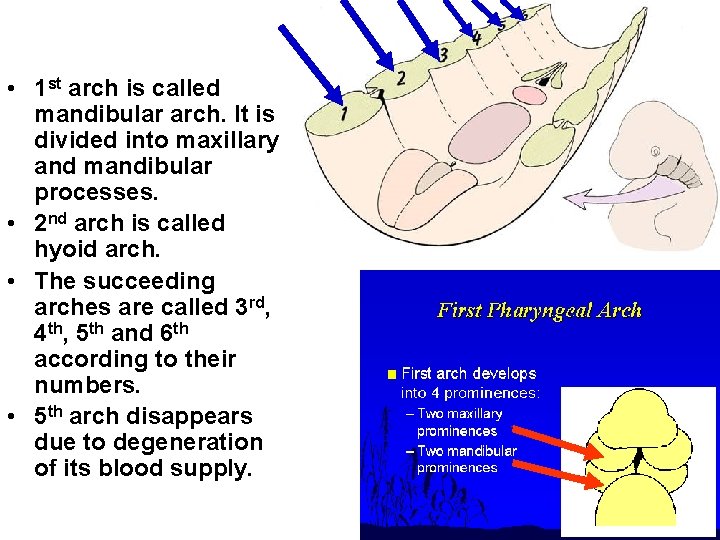
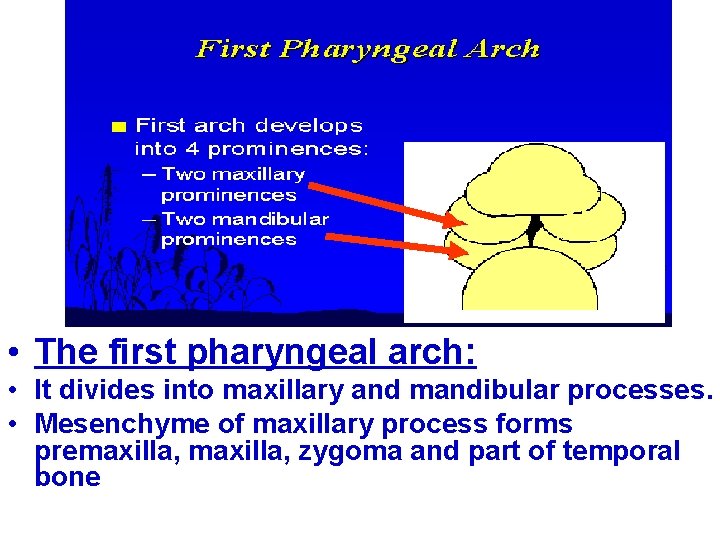
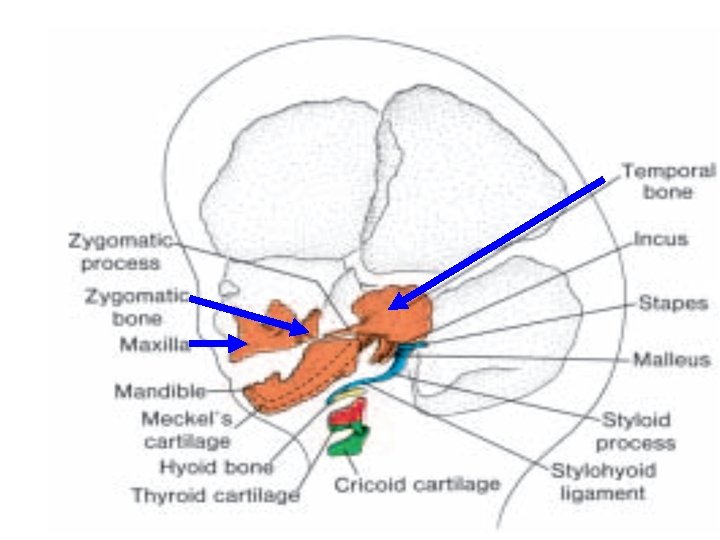
• 1 st arch is called mandibular arch. It is divided into maxillary and mandibular processes. • 2 nd arch is called hyoid arch. • The succeeding arches are called 3 rd, 4 th, 5 th and 6 th according to their numbers. • 5 th arch disappears due to degeneration of its blood supply.
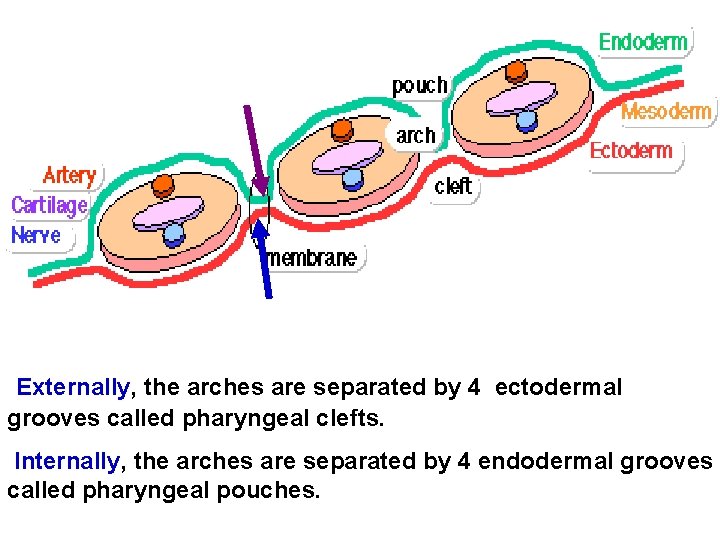
Externally, the arches are separated by 4 ectodermal grooves called pharyngeal clefts. Internally, the arches are separated by 4 endodermal grooves called pharyngeal pouches.
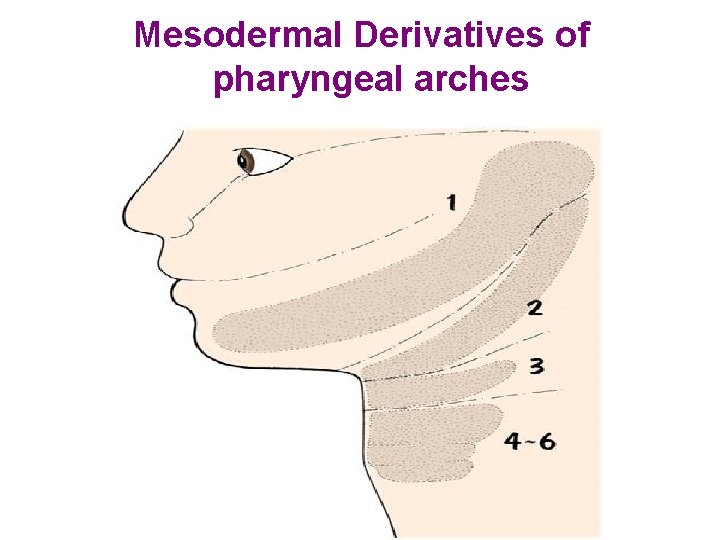
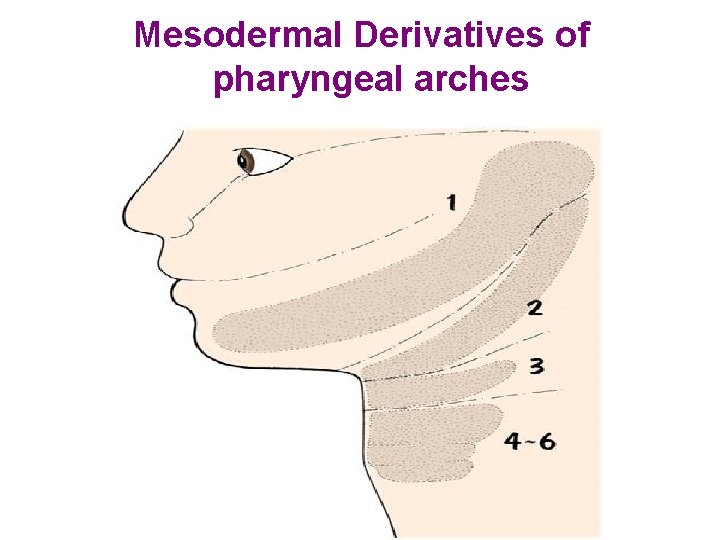
Mesodermal Derivatives of pharyngeal arches
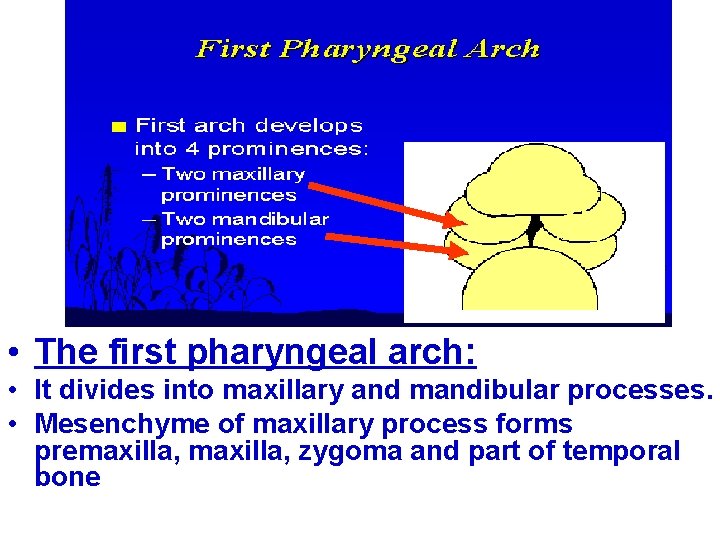
• The first pharyngeal arch: • It divides into maxillary and mandibular processes. • Mesenchyme of maxillary process forms premaxilla, zygoma and part of temporal bone
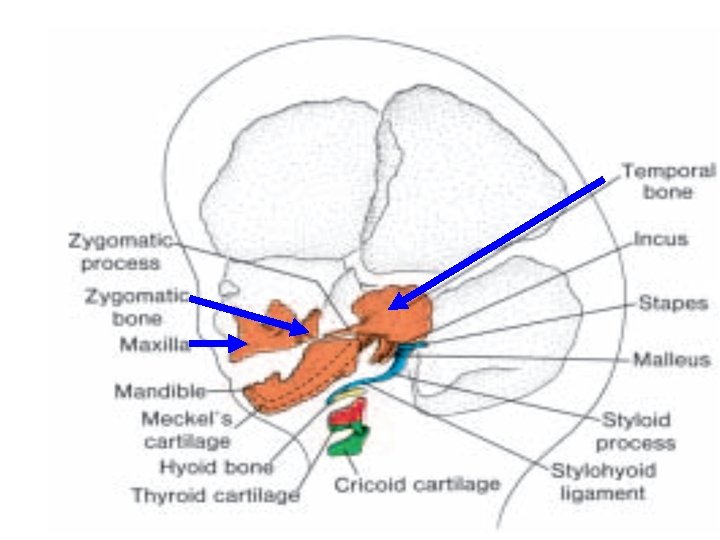
• The muscle derivatives of 1 st arch are: 1. 2. 3. 4. 5. Muscles of mastication Anterior belly of digastric Mylohyoid Tensor palati Tensor tympani The nerve of 1 st arch is mandibular nerve The artery is 1 st aortic arch which disappears except a small portion forming maxilllary artery.
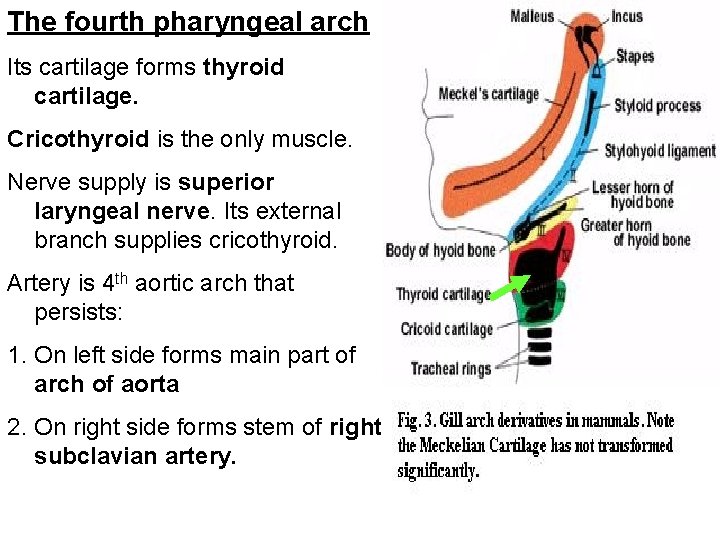
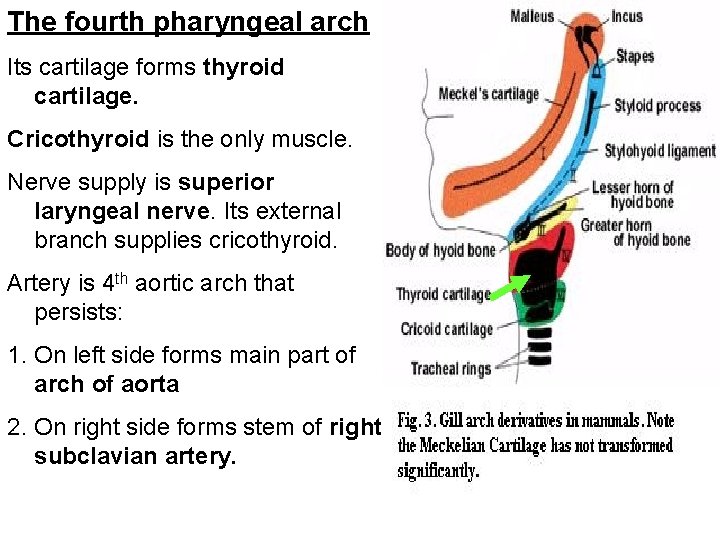
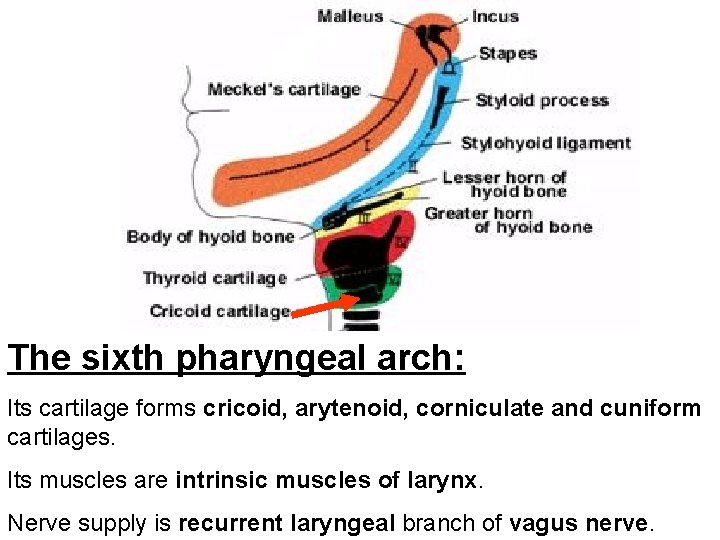
The fourth pharyngeal arch Its cartilage forms thyroid cartilage. Cricothyroid is the only muscle. Nerve supply is superior laryngeal nerve. Its external branch supplies cricothyroid. Artery is 4 th aortic arch that persists: 1. On left side forms main part of arch of aorta 2. On right side forms stem of right subclavian artery.
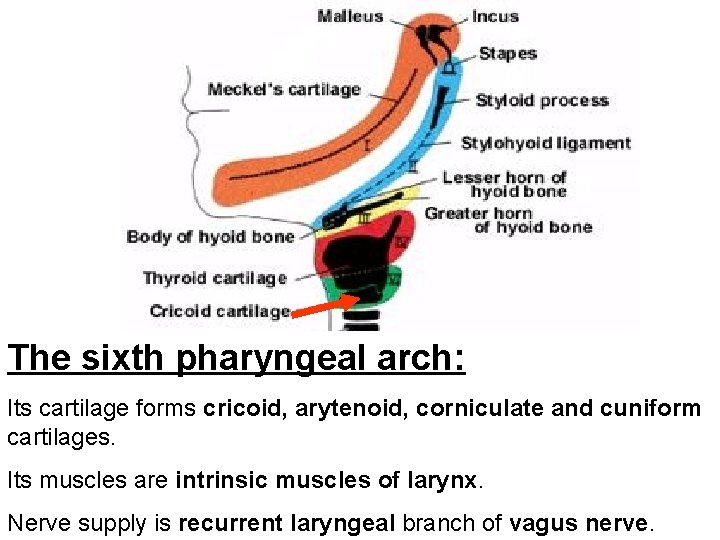
The sixth pharyngeal arch: Its cartilage forms cricoid, arytenoid, corniculate and cuniform cartilages. Its muscles are intrinsic muscles of larynx. Nerve supply is recurrent laryngeal branch of vagus nerve.
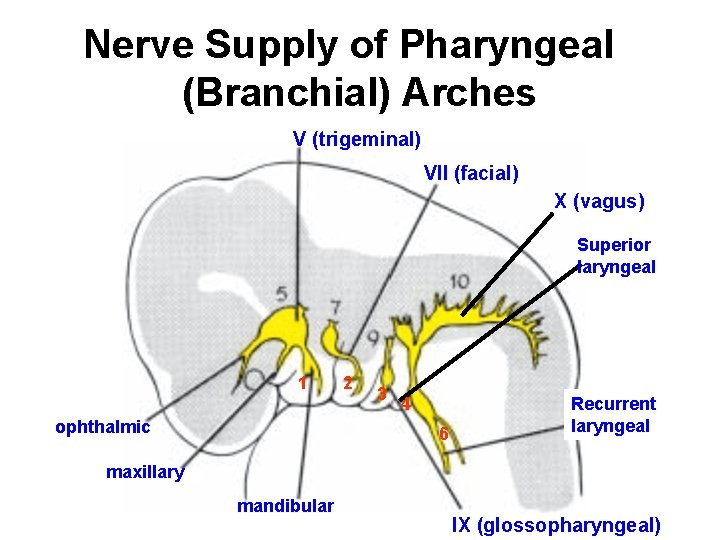
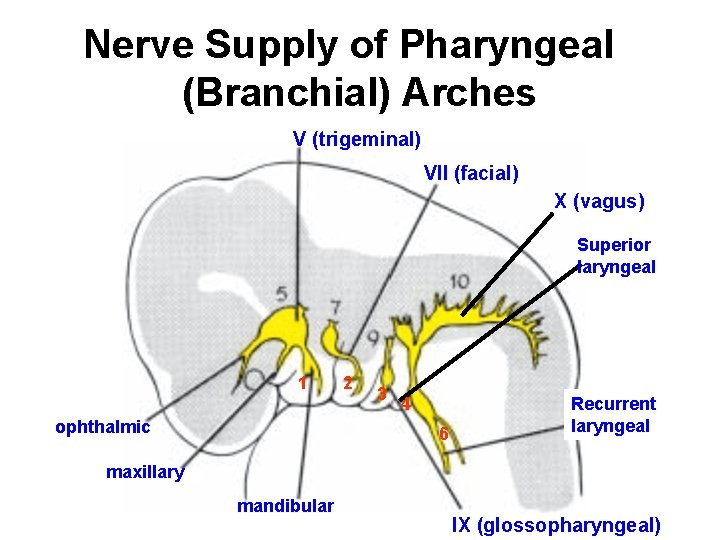
Nerve Supply of Pharyngeal (Branchial) Arches V (trigeminal) VII (facial) X (vagus) Superior laryngeal 1 ophthalmic 2 3 4 6 Recurrent laryngeal maxillary mandibular IX (glossopharyngeal)
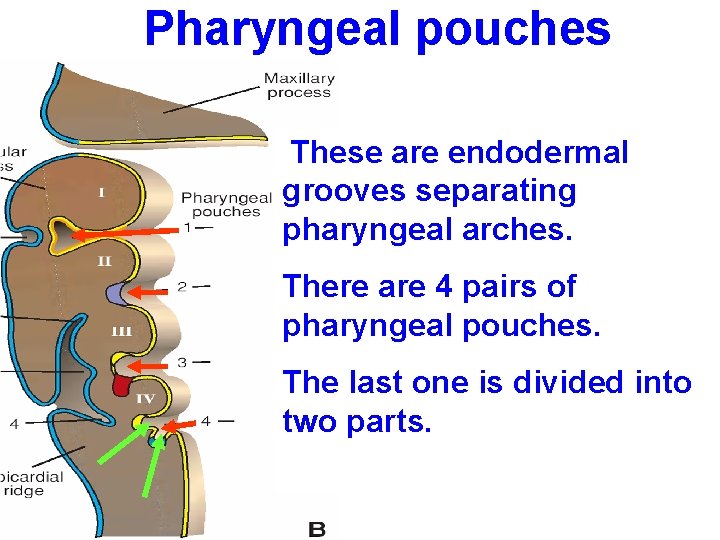
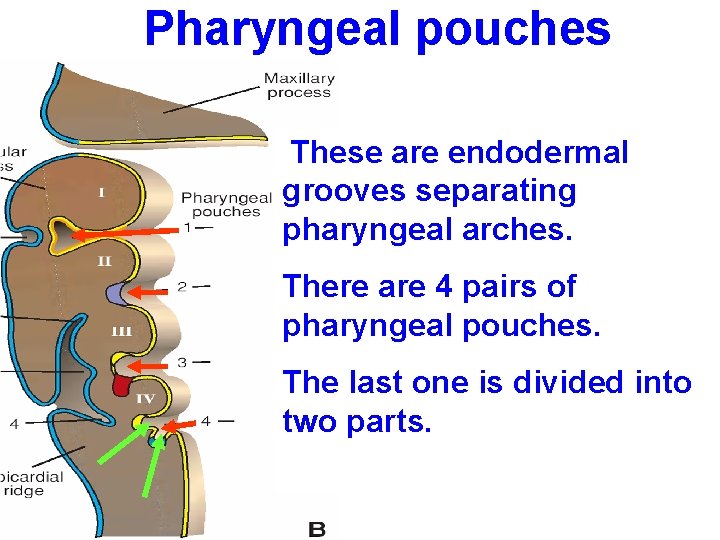
Pharyngeal pouches These are endodermal grooves separating pharyngeal arches. There are 4 pairs of pharyngeal pouches. The last one is divided into two parts.
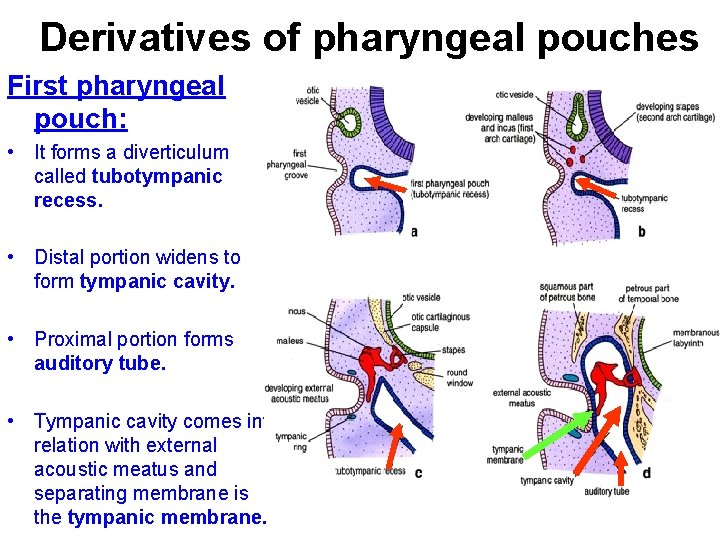
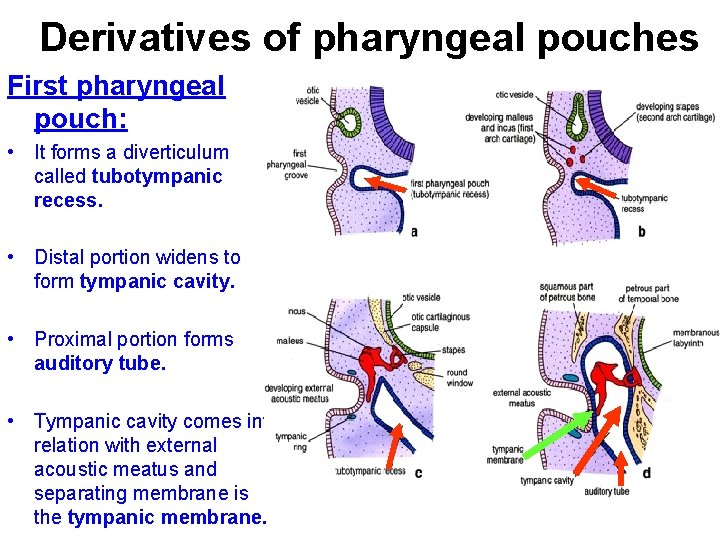
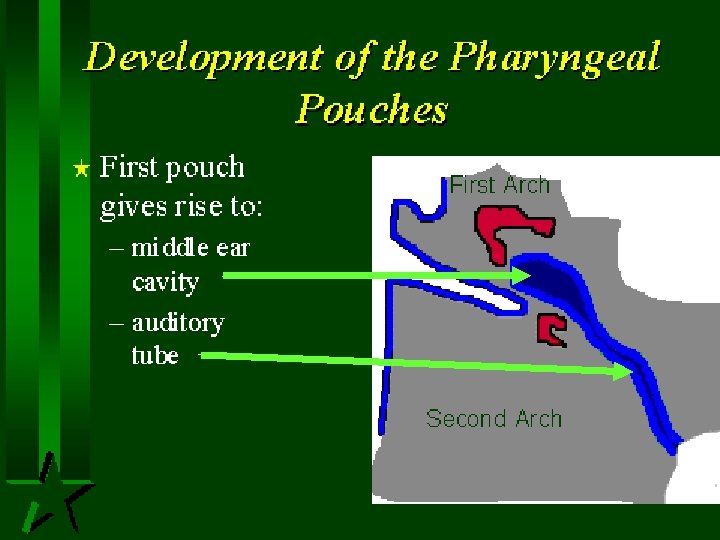
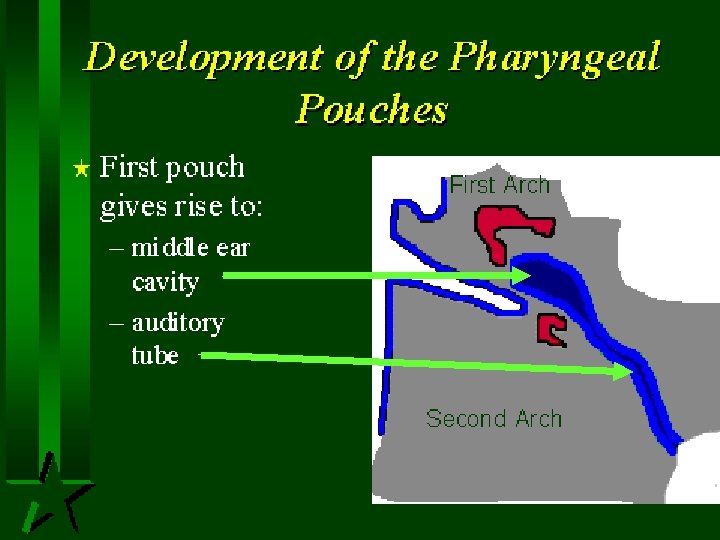
Derivatives of pharyngeal pouches First pharyngeal pouch: • It forms a diverticulum called tubotympanic recess. • Distal portion widens to form tympanic cavity. • Proximal portion forms auditory tube. • Tympanic cavity comes into relation with external acoustic meatus and separating membrane is the tympanic membrane.
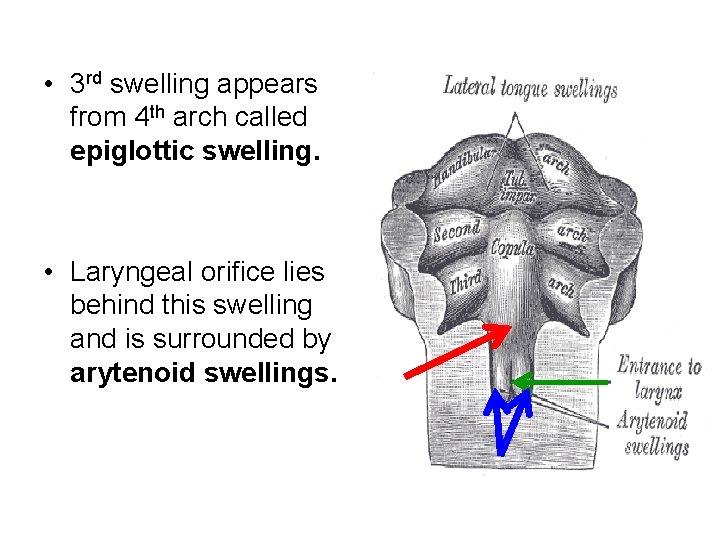
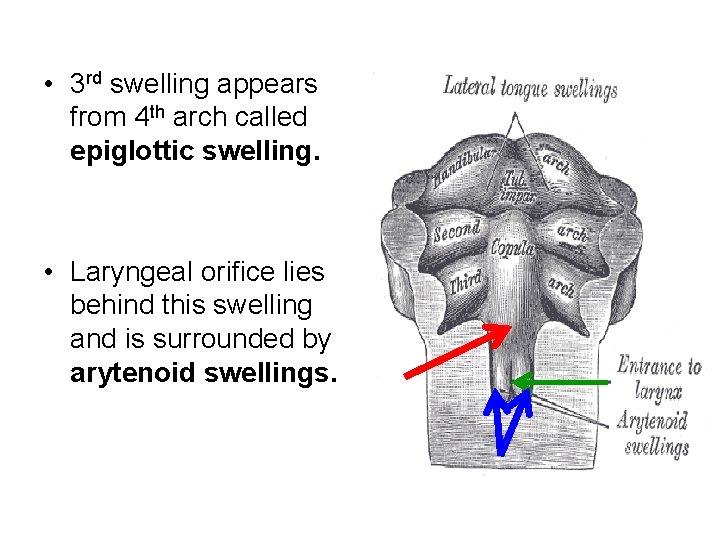
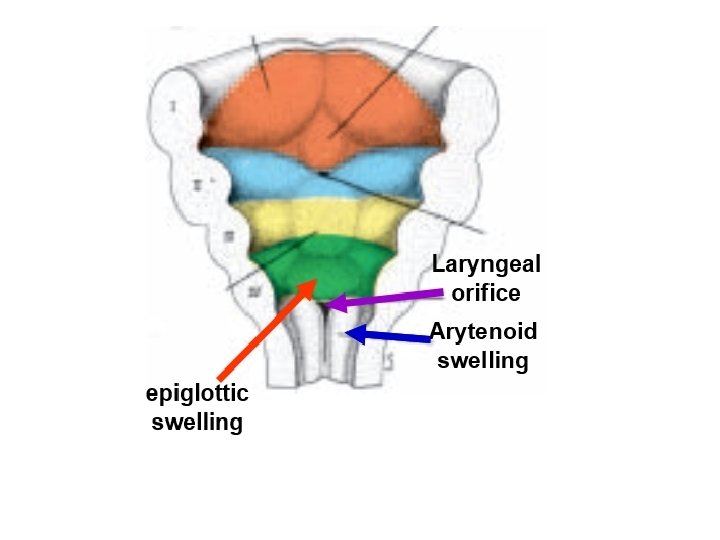
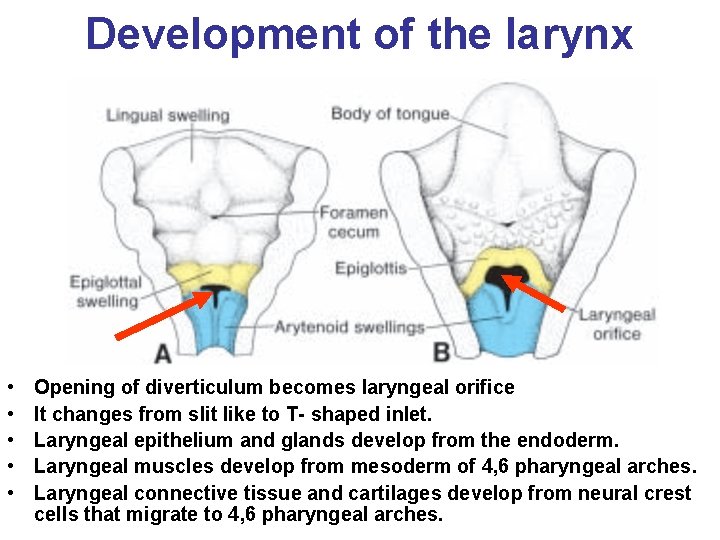
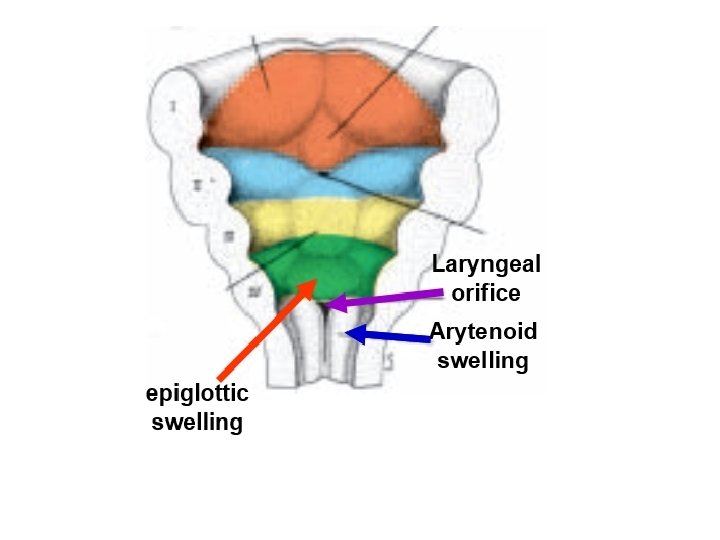
• 3 rd swelling appears from 4 th arch called epiglottic swelling. • Laryngeal orifice lies behind this swelling and is surrounded by arytenoid swellings.
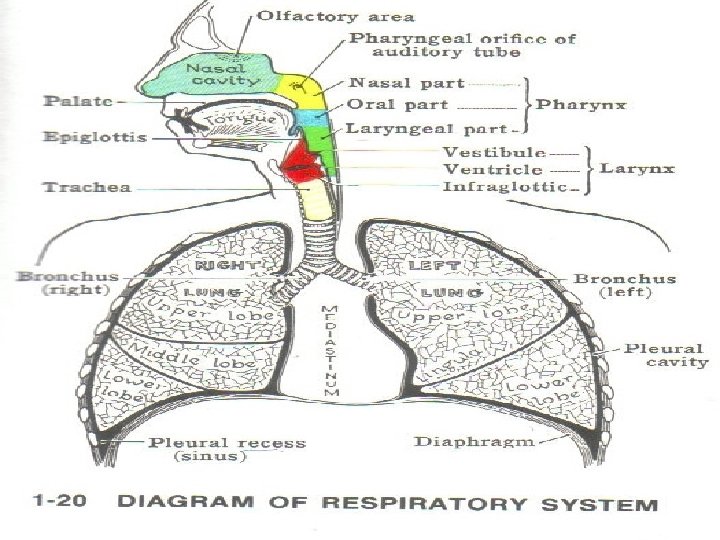
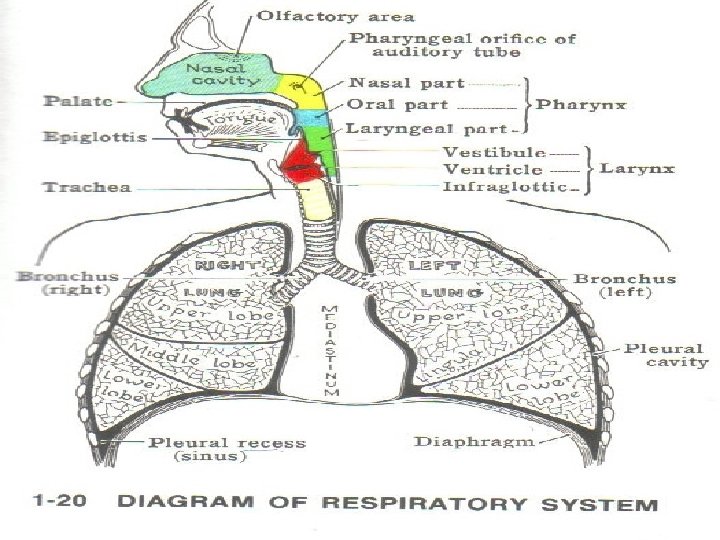
Items to be covered: • Early development • Development of the larynx • Development of trachea • Development of bronchi • Development of the lung • Congenital anomalies of respiratory system.
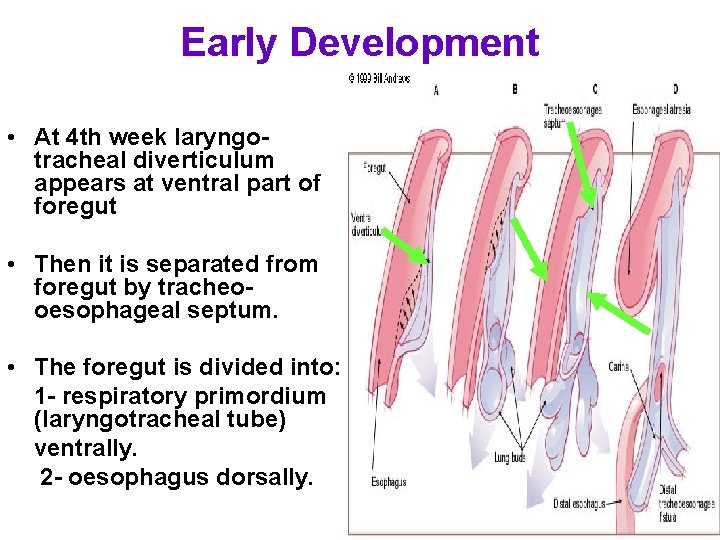
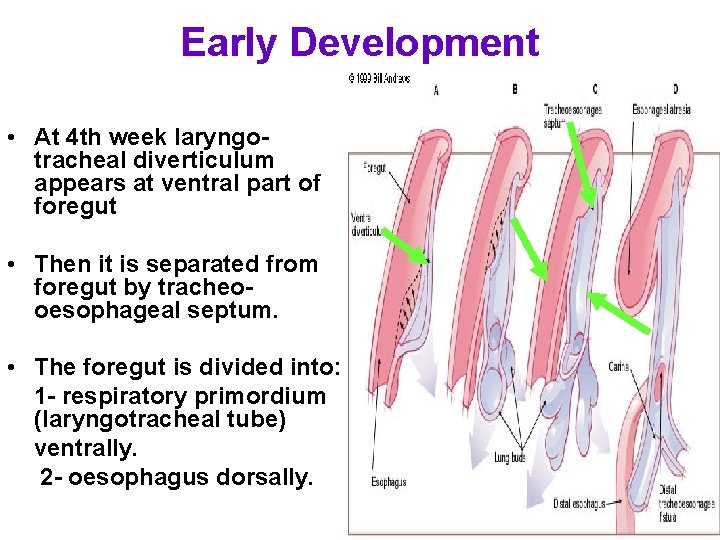
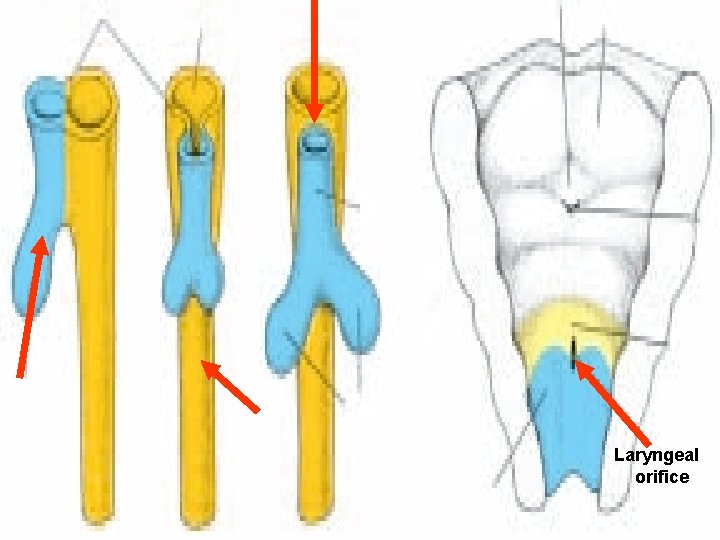
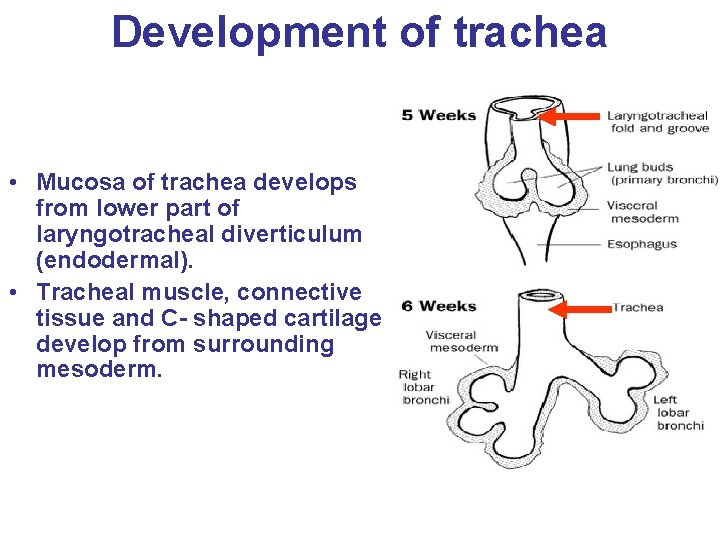
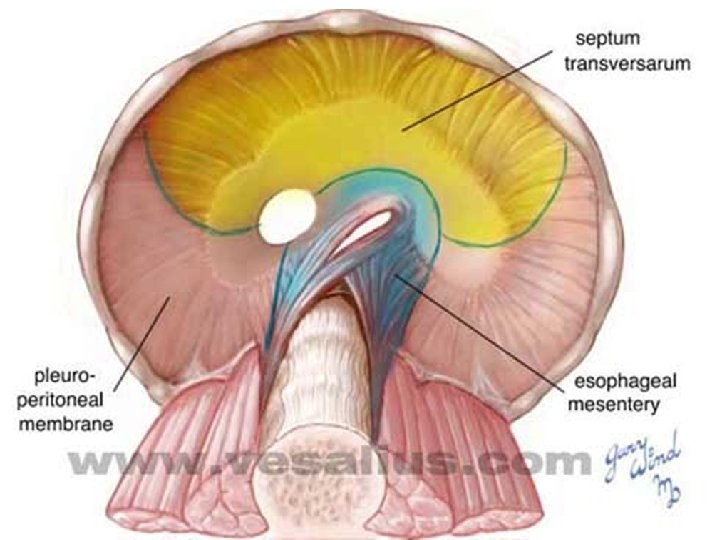
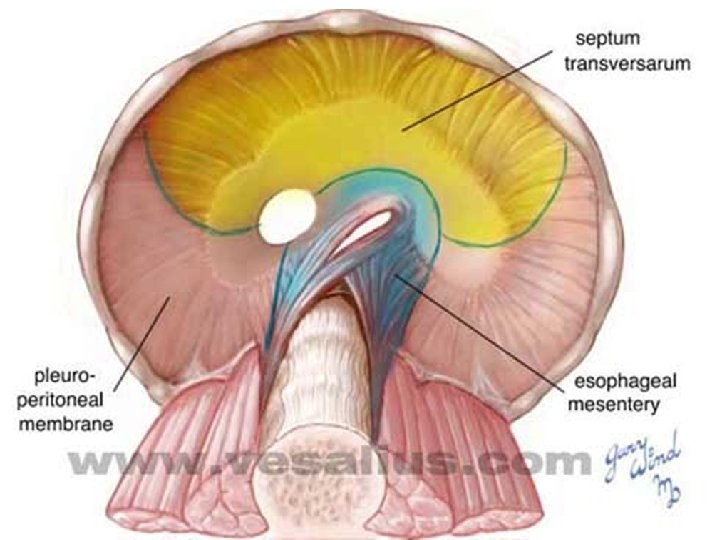
Early Development • At 4 th week laryngotracheal diverticulum appears at ventral part of foregut • Then it is separated from foregut by tracheooesophageal septum. • The foregut is divided into: 1 - respiratory primordium (laryngotracheal tube) ventrally. 2 - oesophagus dorsally.
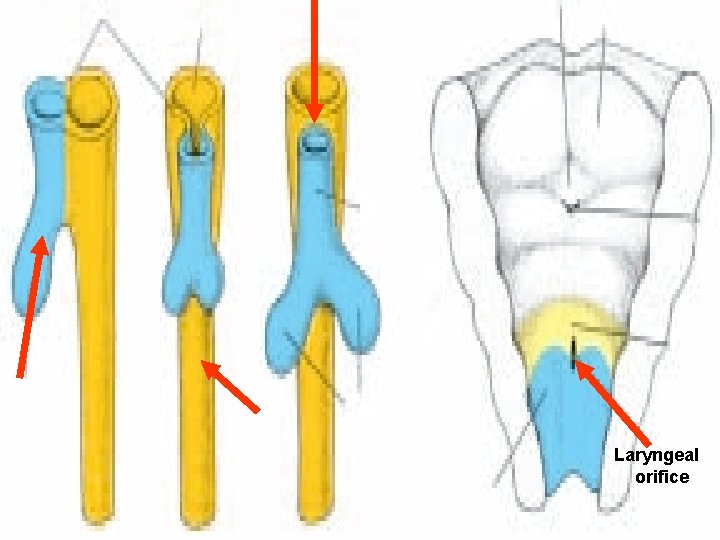
Laryngeal orifice
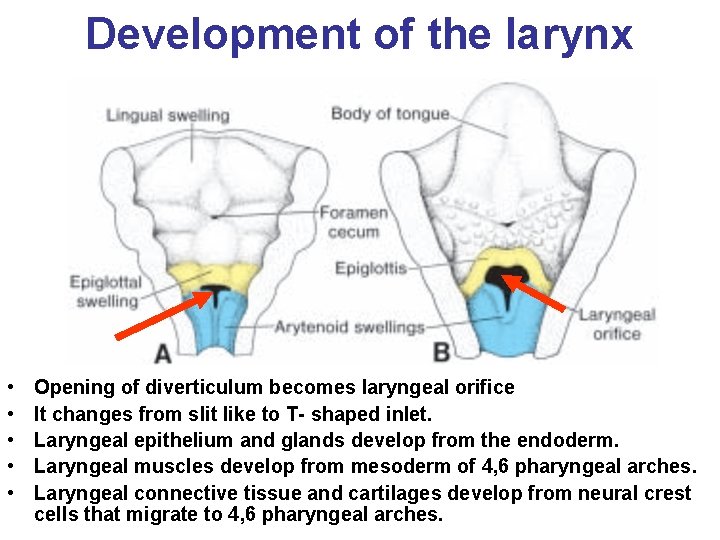
Development of the larynx • • • Opening of diverticulum becomes laryngeal orifice It changes from slit like to T- shaped inlet. Laryngeal epithelium and glands develop from the endoderm. Laryngeal muscles develop from mesoderm of 4, 6 pharyngeal arches. Laryngeal connective tissue and cartilages develop from neural crest cells that migrate to 4, 6 pharyngeal arches.
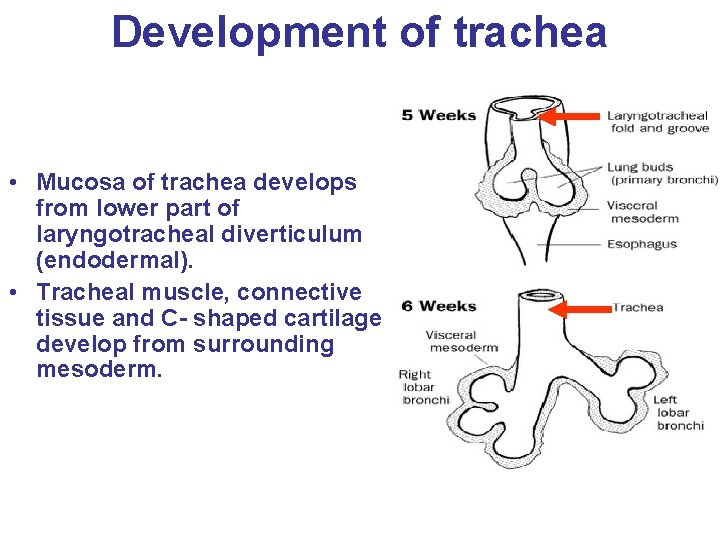
Development of trachea • Mucosa of trachea develops from lower part of laryngotracheal diverticulum (endodermal). • Tracheal muscle, connective tissue and C- shaped cartilage develop from surrounding mesoderm.
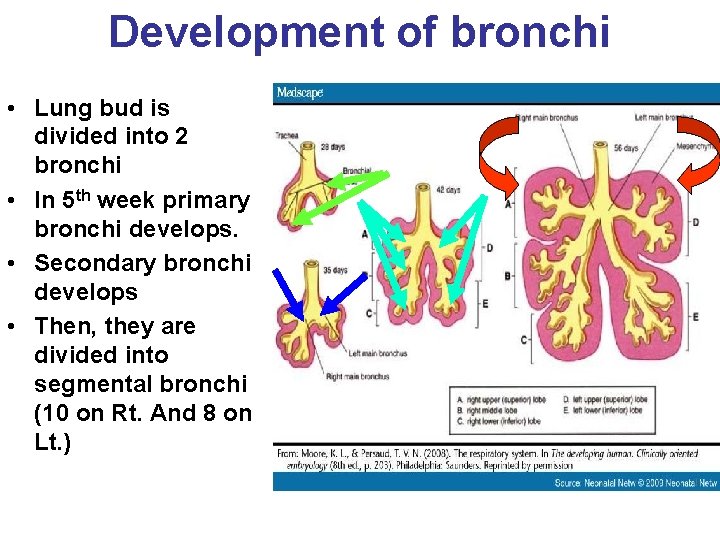
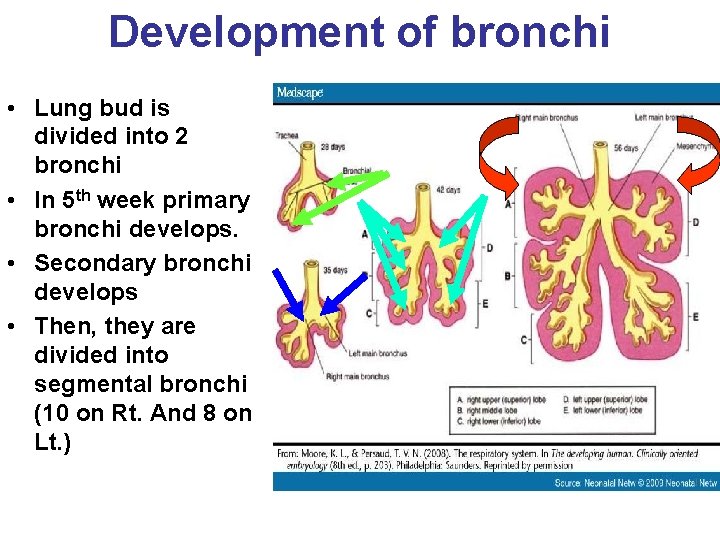
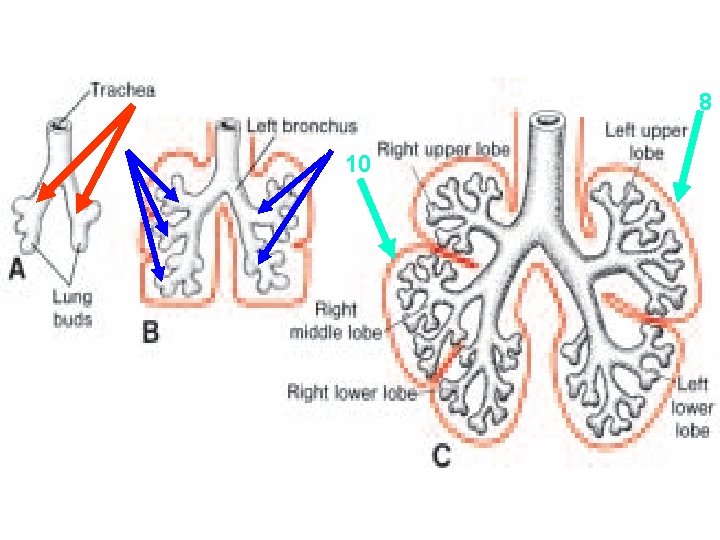
Development of bronchi • Lung bud is divided into 2 bronchi • In 5 th week primary bronchi develops. • Secondary bronchi develops • Then, they are divided into segmental bronchi (10 on Rt. And 8 on Lt. )
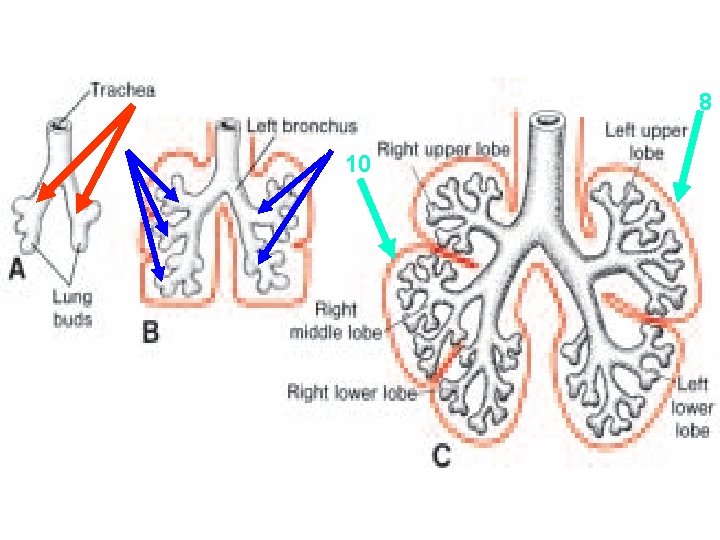
8 10
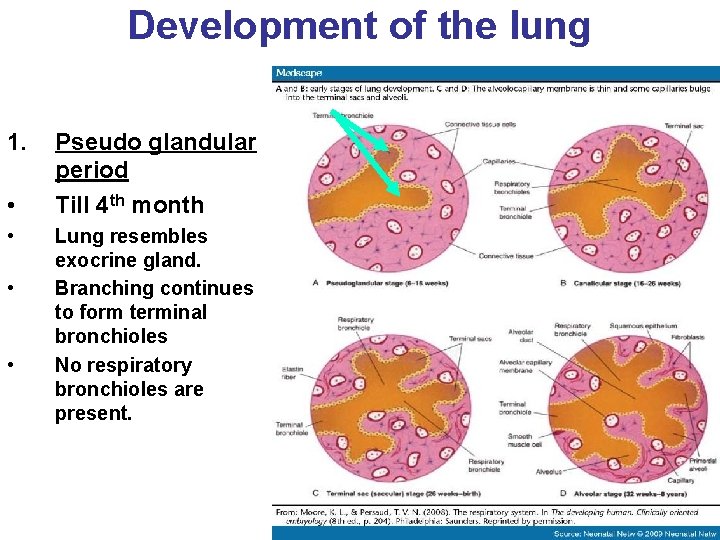
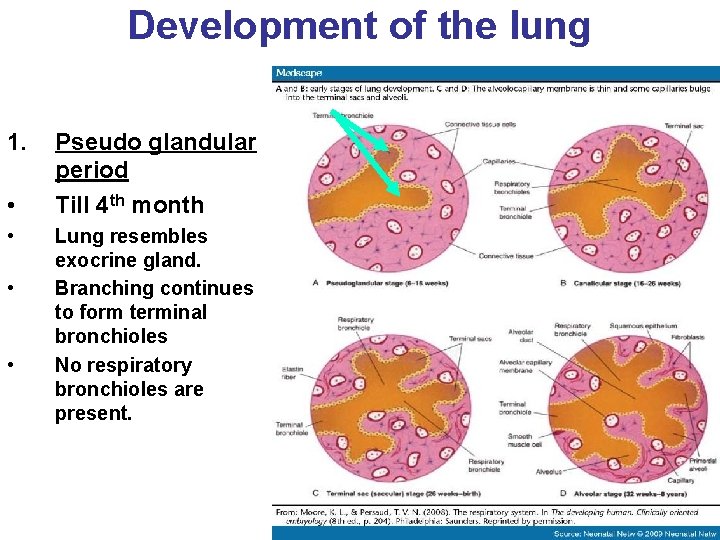
Development of the lung 1. • • Pseudo glandular period Till 4 th month Lung resembles exocrine gland. Branching continues to form terminal bronchioles No respiratory bronchioles are present.
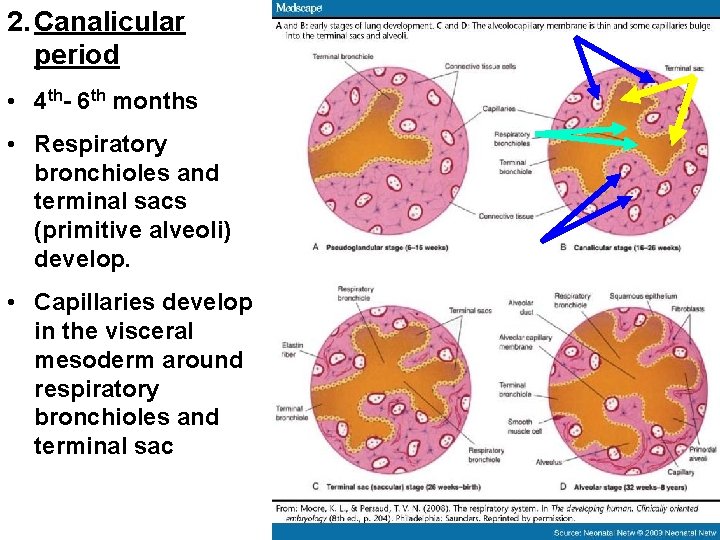
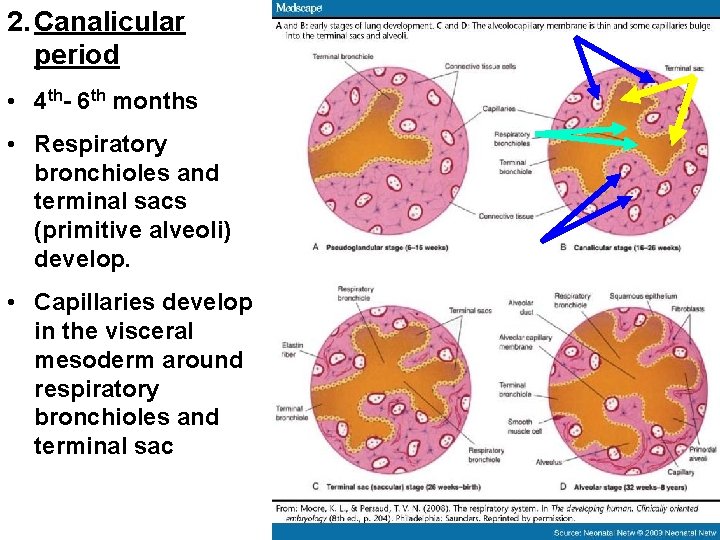
2. Canalicular period • 4 th- 6 th months • Respiratory bronchioles and terminal sacs (primitive alveoli) develop. • Capillaries develop in the visceral mesoderm around respiratory bronchioles and terminal sac
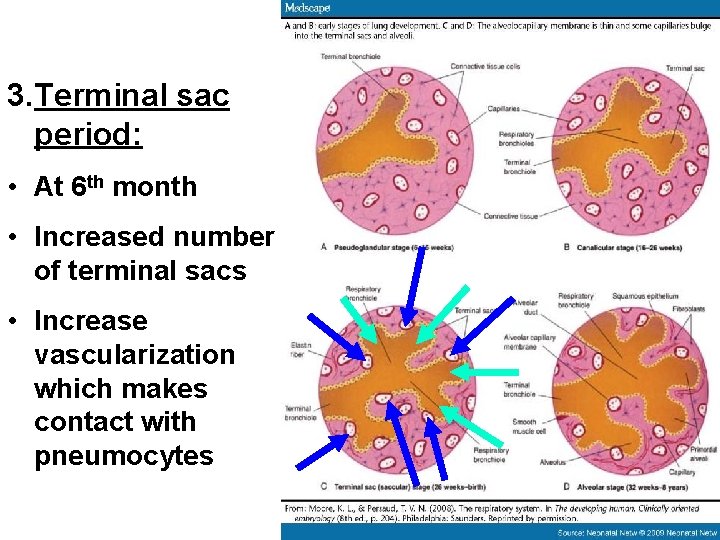
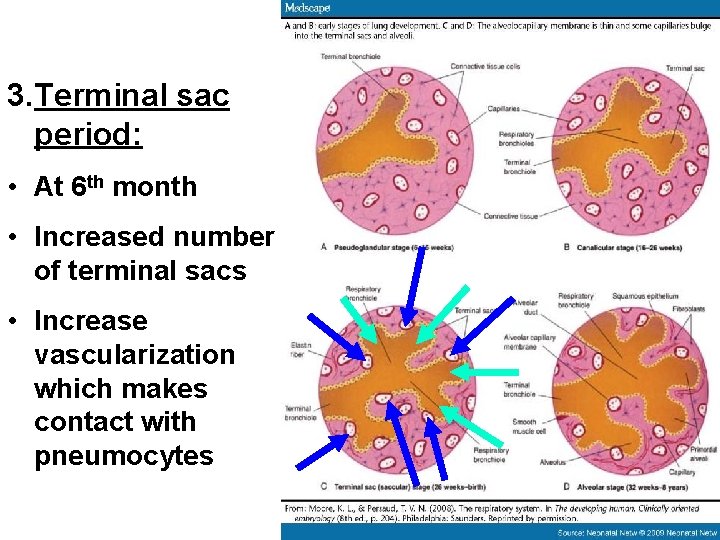
3. Terminal sac period: • At 6 th month • Increased number of terminal sacs • Increase vascularization which makes contact with pneumocytes
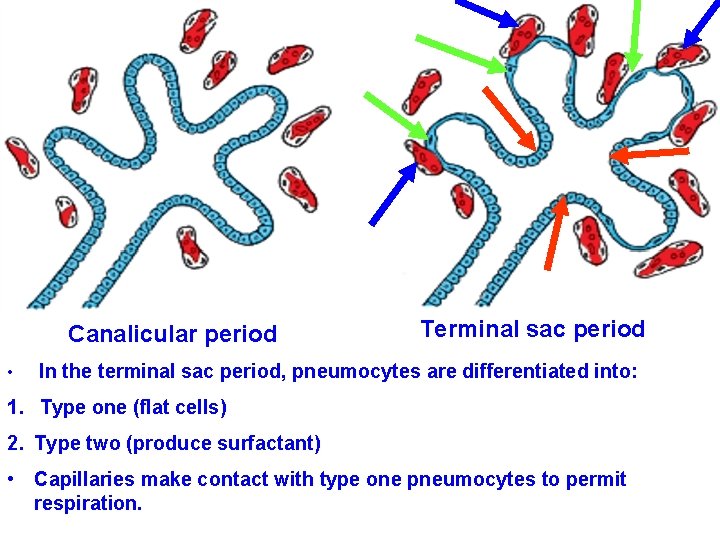
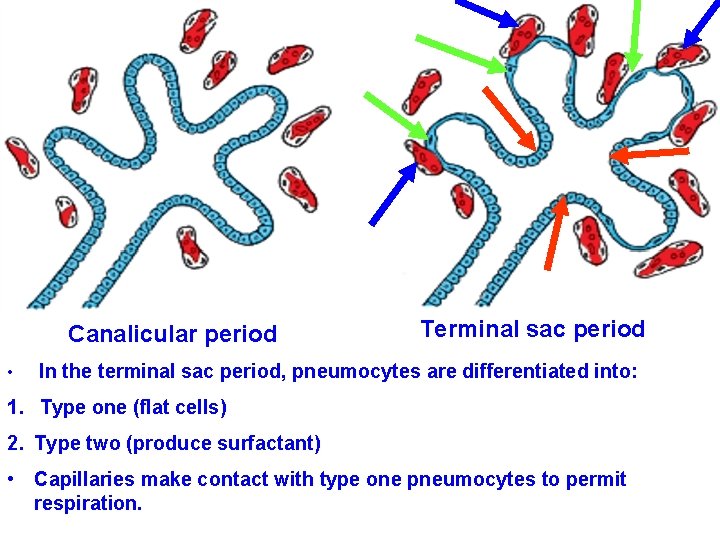
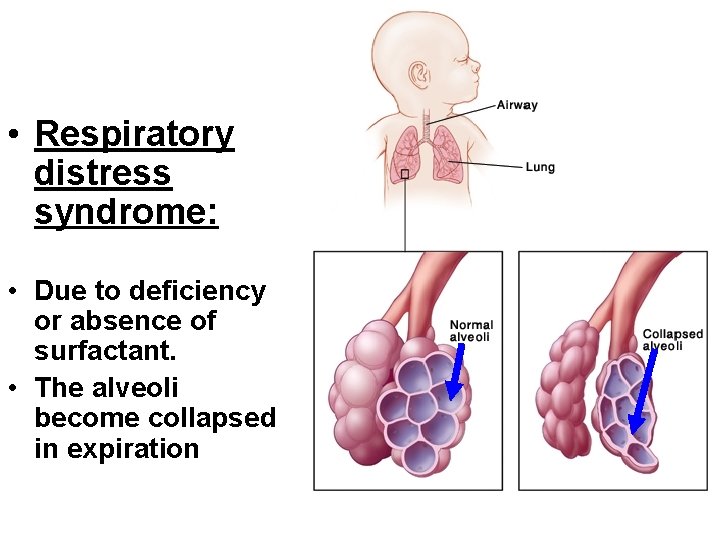
Canalicular period • Terminal sac period In the terminal sac period, pneumocytes are differentiated into: 1. Type one (flat cells) 2. Type two (produce surfactant) • Capillaries make contact with type one pneumocytes to permit respiration.
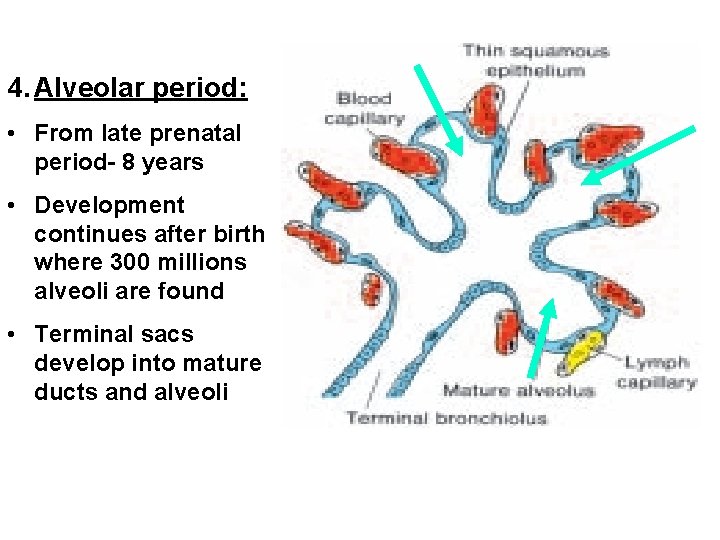
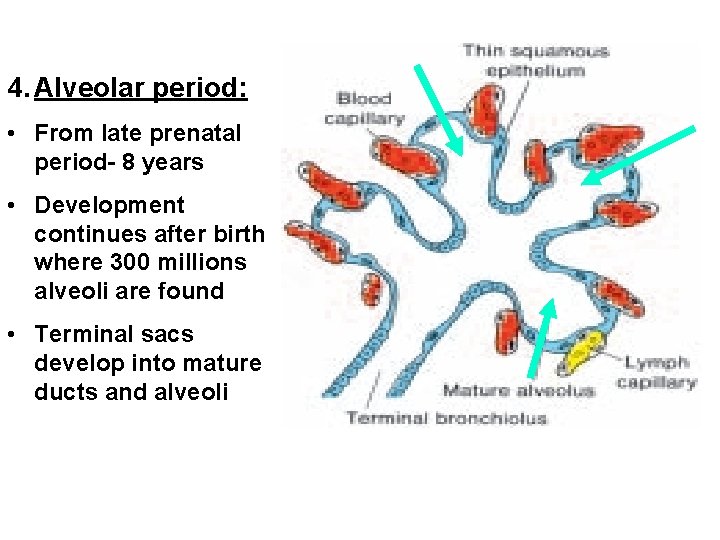
4. Alveolar period: • From late prenatal period- 8 years • Development continues after birth where 300 millions alveoli are found • Terminal sacs develop into mature ducts and alveoli
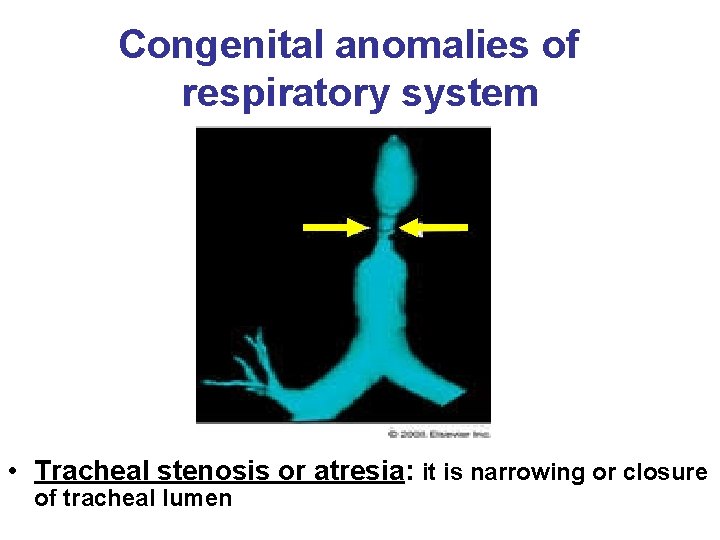
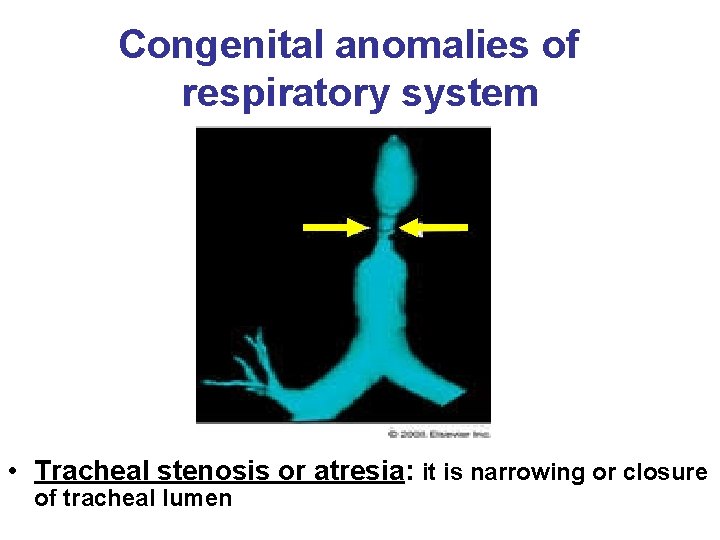
Congenital anomalies of respiratory system • Tracheal stenosis or atresia: it is narrowing or closure of tracheal lumen
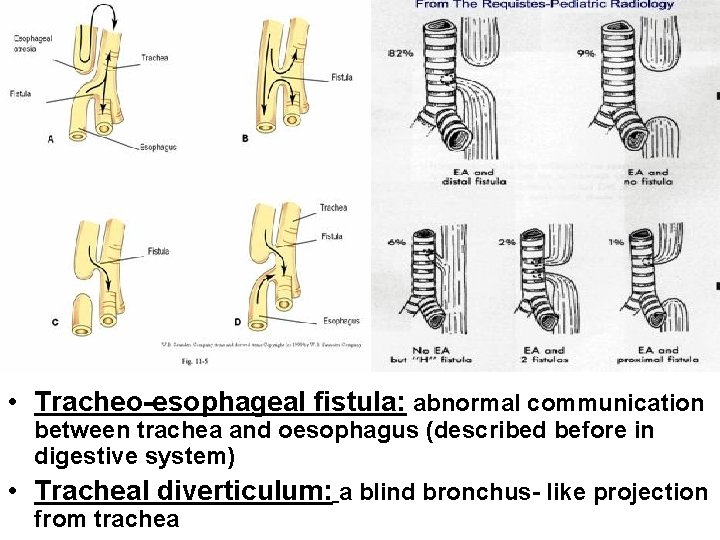
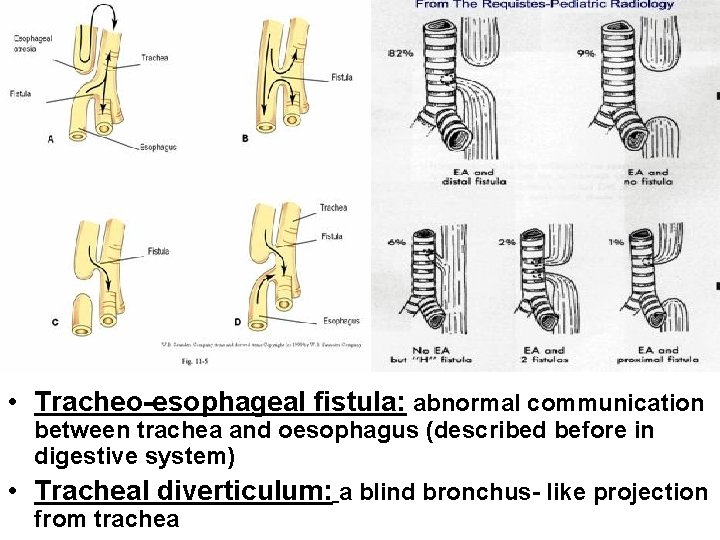
• Tracheo-esophageal fistula: abnormal communication between trachea and oesophagus (described before in digestive system) • Tracheal diverticulum: a blind bronchus- like projection from trachea
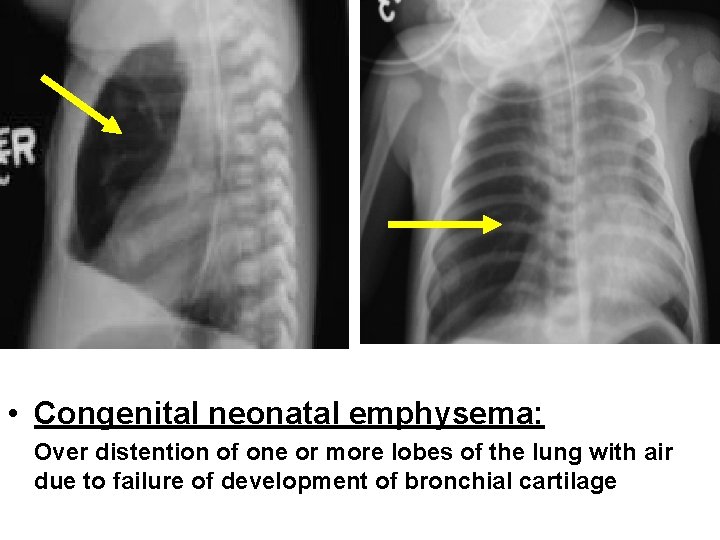
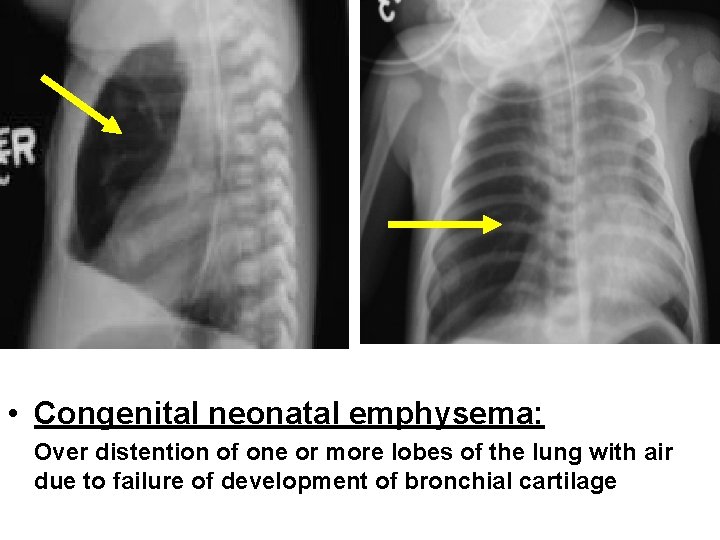
• Congenital neonatal emphysema: Over distention of one or more lobes of the lung with air due to failure of development of bronchial cartilage
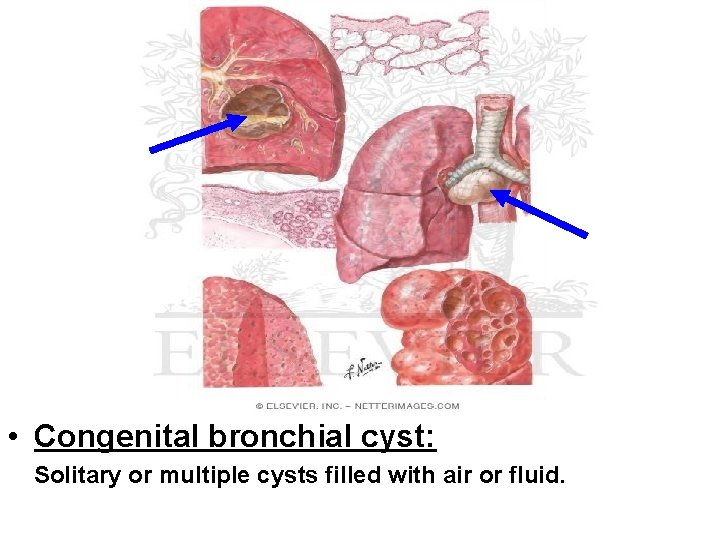
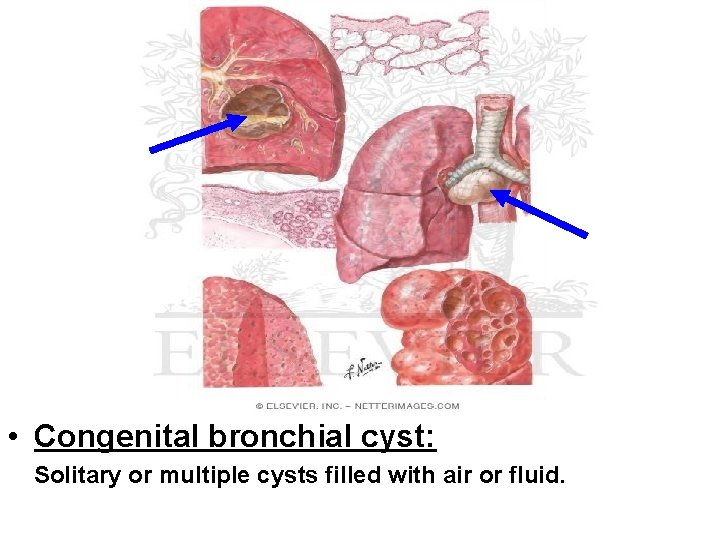
• Congenital bronchial cyst: Solitary or multiple cysts filled with air or fluid.
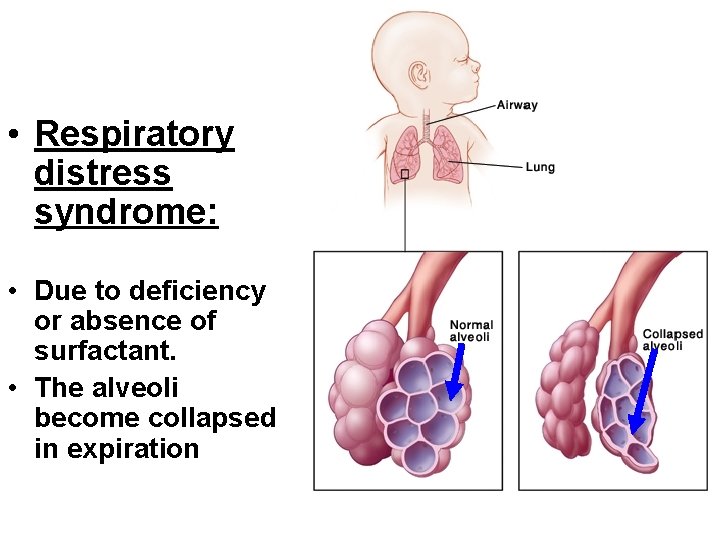
• Respiratory distress syndrome: • Due to deficiency or absence of surfactant. • The alveoli become collapsed in expiration
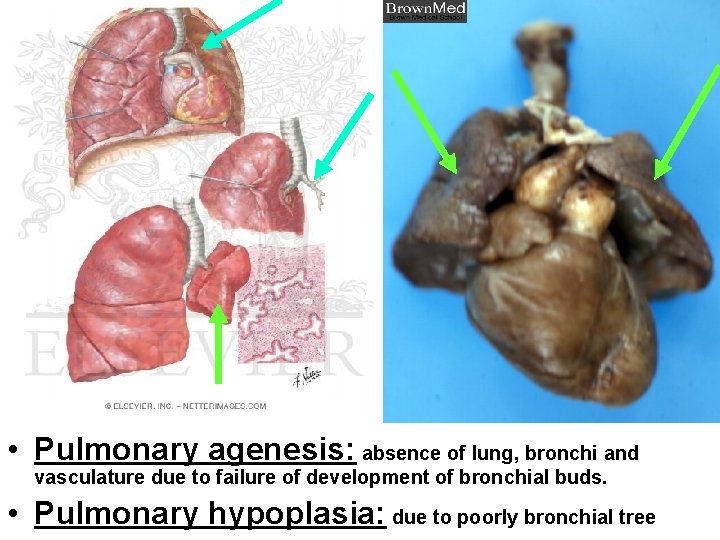
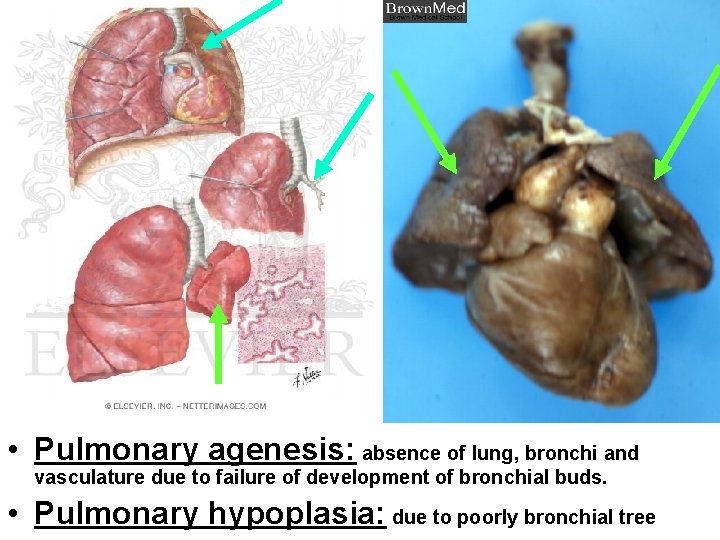
• Pulmonary agenesis: absence of lung, bronchi and vasculature due to failure of development of bronchial buds. • Pulmonary hypoplasia: due to poorly bronchial tree

Thank You