Development and Implementation of National NCD Programme Dr



- Slides: 42

Development and Implementation of National NCD Programme Dr Lal Panapitiya Director / NCD P & C Unit Ministry of Healthcare & Nutrition, Sri Lanka
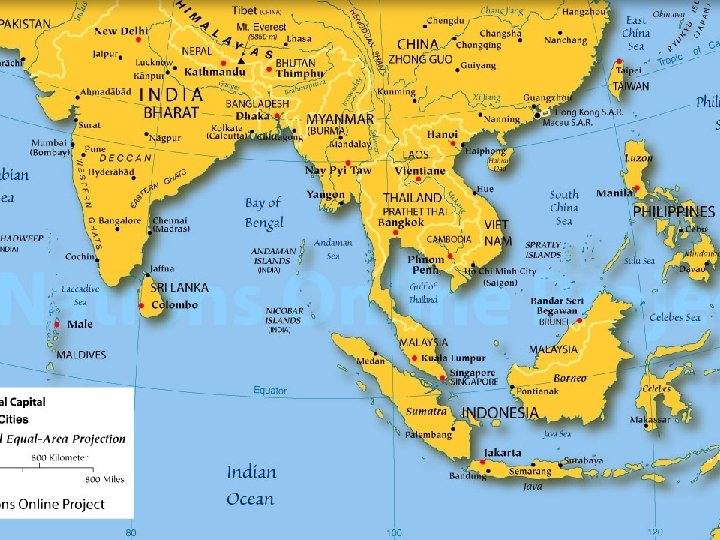
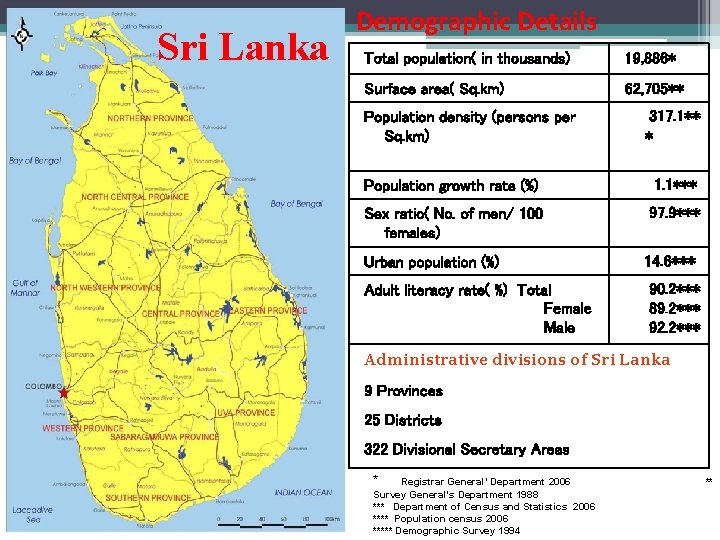
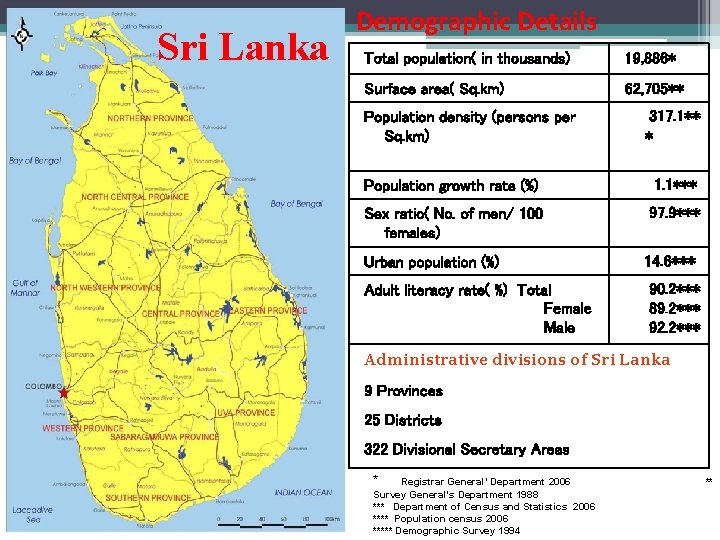
Sri Lanka Demographic Details Total population( in thousands) 19, 886* Surface area( Sq. km) 62, 705** Population density (persons per Sq. km) 317. 1** * Population growth rate (%) 1. 1*** Sex ratio( No. of men/ 100 females) 97. 9*** Urban population (%) Adult literacy rate( %) Total Female Male 14. 6*** 90. 2*** 89. 2*** 92. 2*** Administrative divisions of Sri Lanka 9 Provinces 25 Districts 322 Divisional Secretary Areas * Registrar General’ Department 2006 Survey General’s Department 1988 *** Department of Census and Statistics 2006 **** Population census 2006 ***** Demographic Survey 1994 **
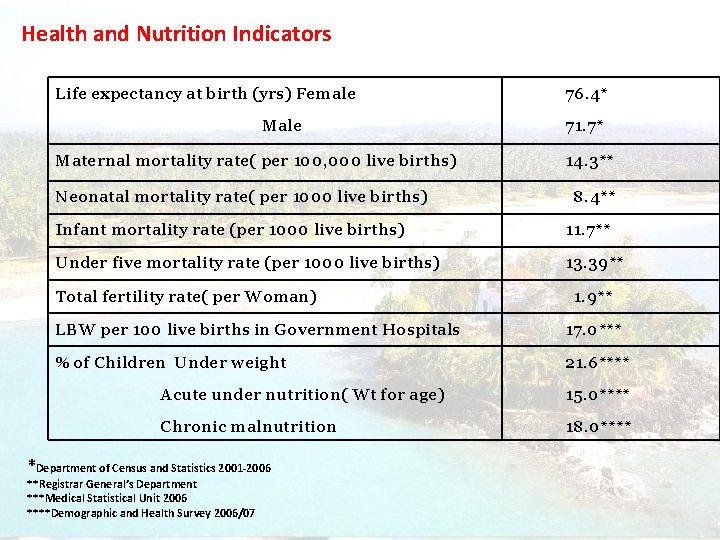
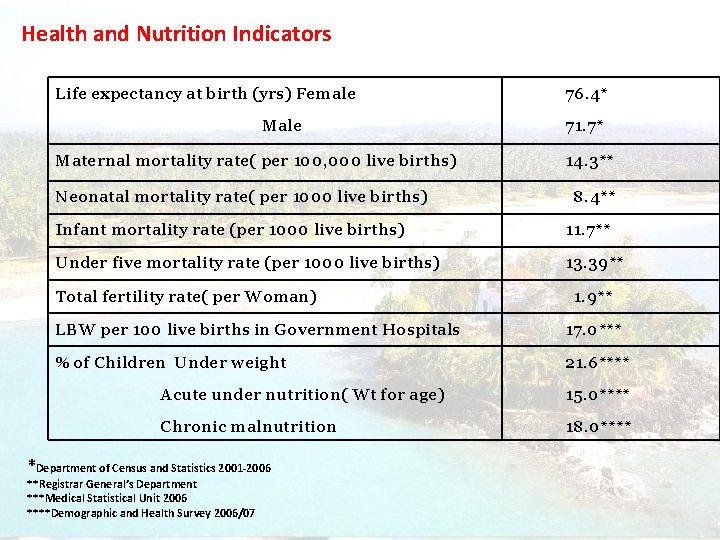
Health and Nutrition Indicators Life expectancy at birth (yrs) Female Maternal mortality rate( per 100, 000 live births) Neonatal mortality rate( per 1000 live births) 76. 4* 71. 7* 14. 3** 8. 4** Infant mortality rate (per 1000 live births) 11. 7** Under five mortality rate (per 1000 live births) 13. 39** Total fertility rate( per Woman) 1. 9** LBW per 100 live births in Government Hospitals 17. 0*** % of Children Under weight 21. 6**** Acute under nutrition( Wt for age) 15. 0**** Chronic malnutrition 18. 0**** *Department of Census and Statistics 2001 -2006 **Registrar General’s Department ***Medical Statistical Unit 2006 ****Demographic and Health Survey 2006/07
Situational Analysis Sri Lanka
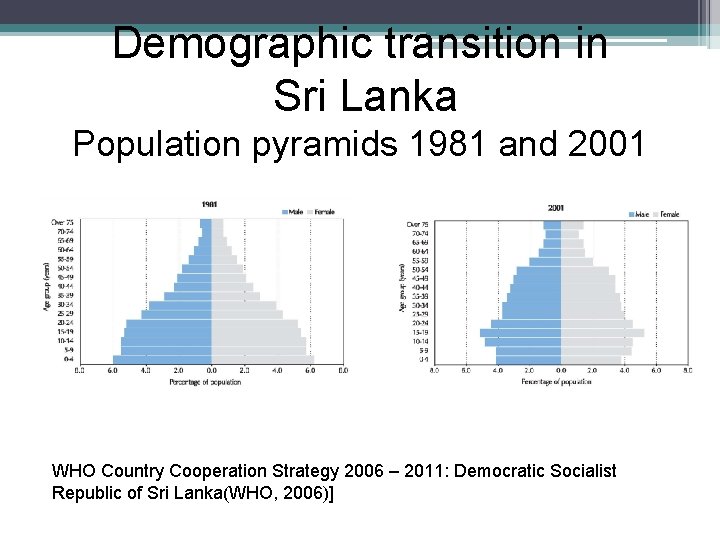
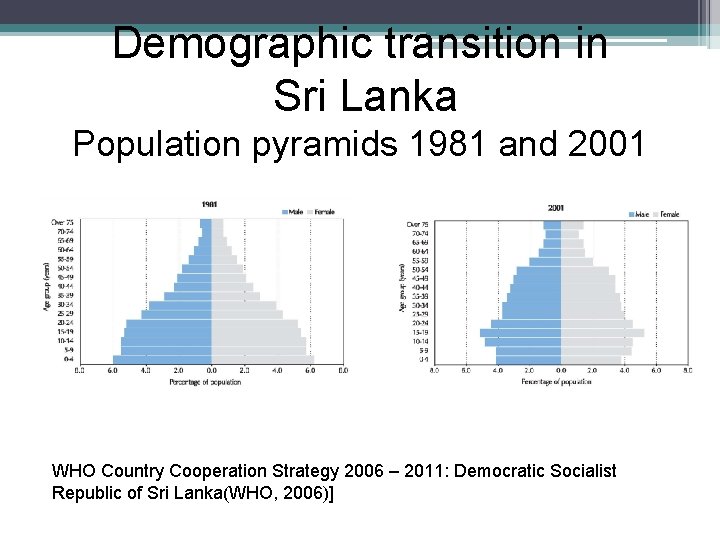
Demographic transition in Sri Lanka Population pyramids 1981 and 2001 WHO Country Cooperation Strategy 2006 – 2011: Democratic Socialist Republic of Sri Lanka(WHO, 2006)]
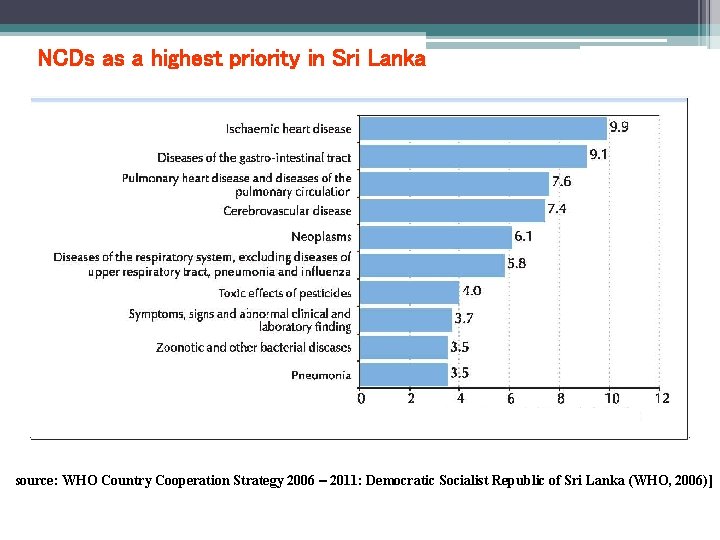
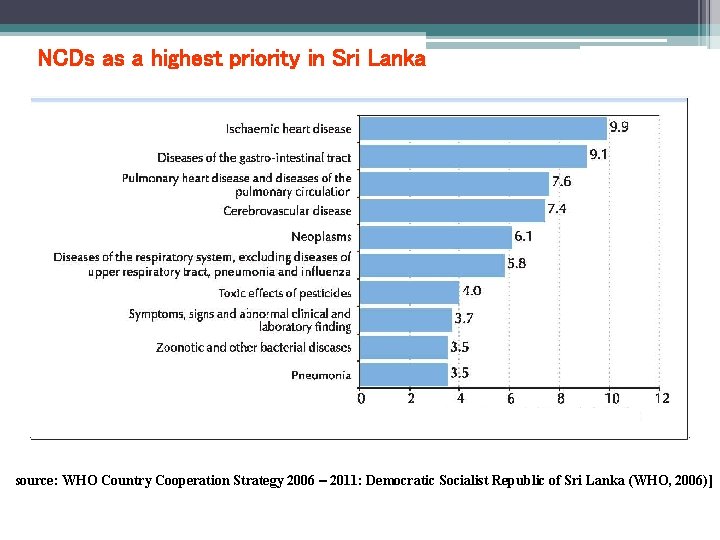
NCDs as a highest priority in Sri Lanka Source: WHO Country Cooperation Strategy 2006 – 2011: Democratic Socialist Republic of Sri Lanka (WHO, 2006)]
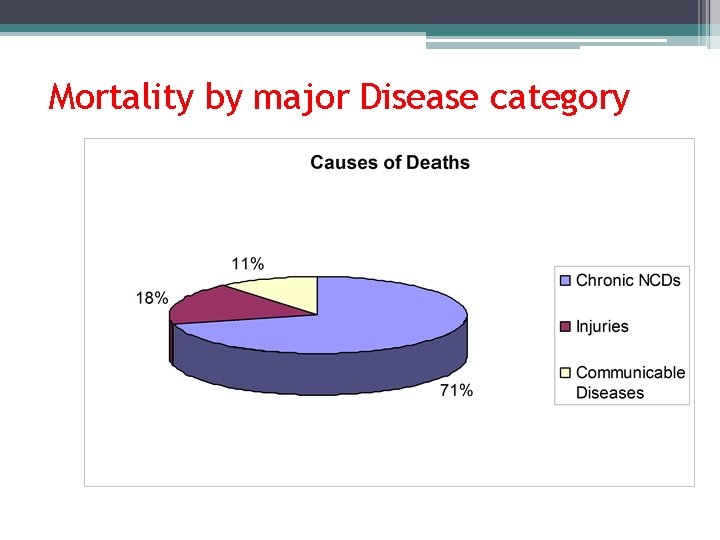
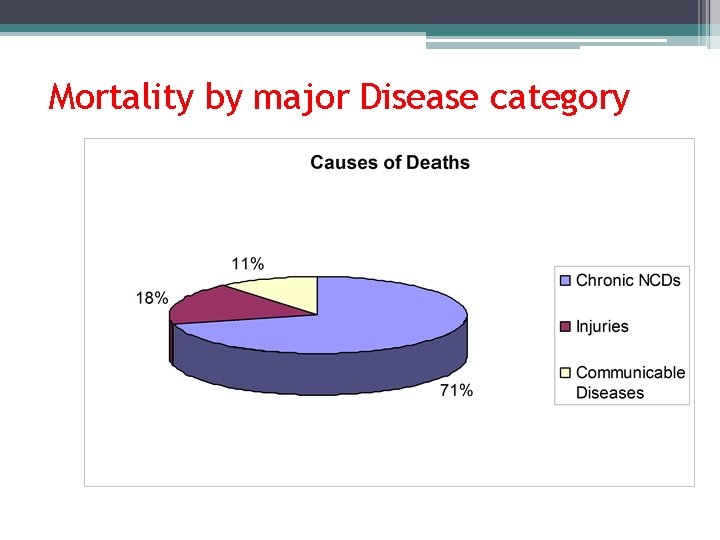
Mortality by major Disease category
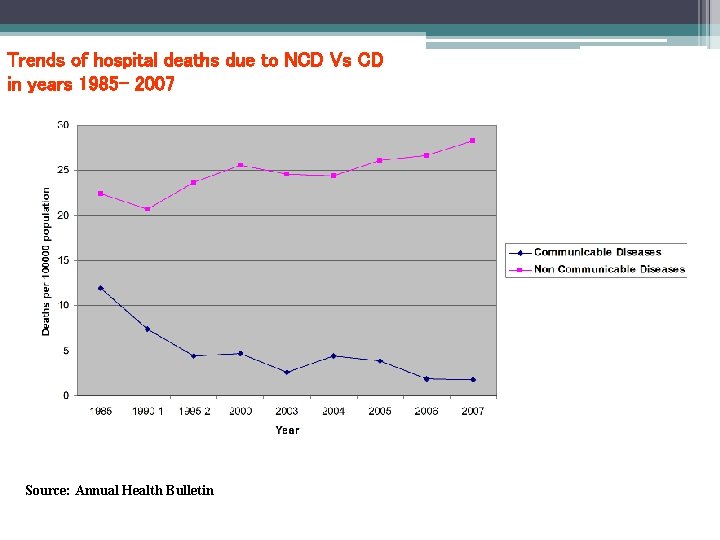
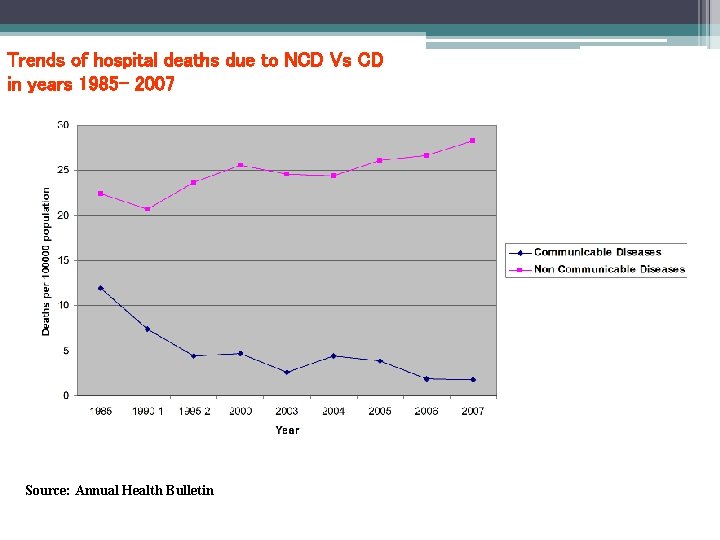
Trends of hospital deaths due to NCD Vs CD in years 1985 - 2007 Source: Annual Health Bulletin
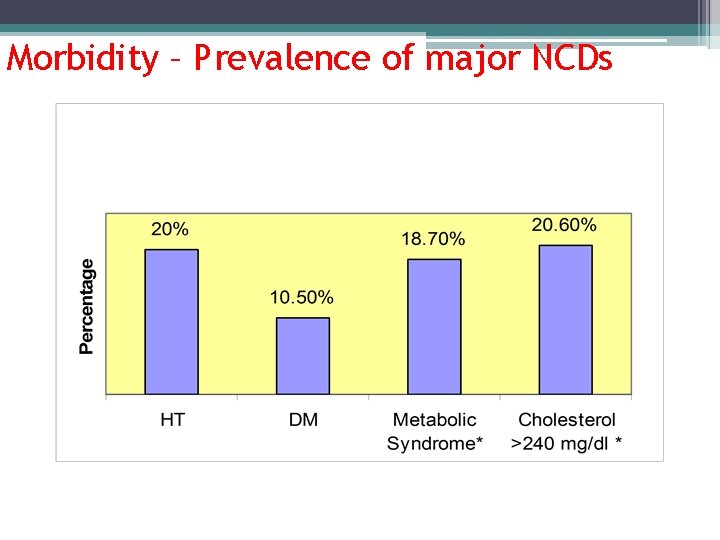
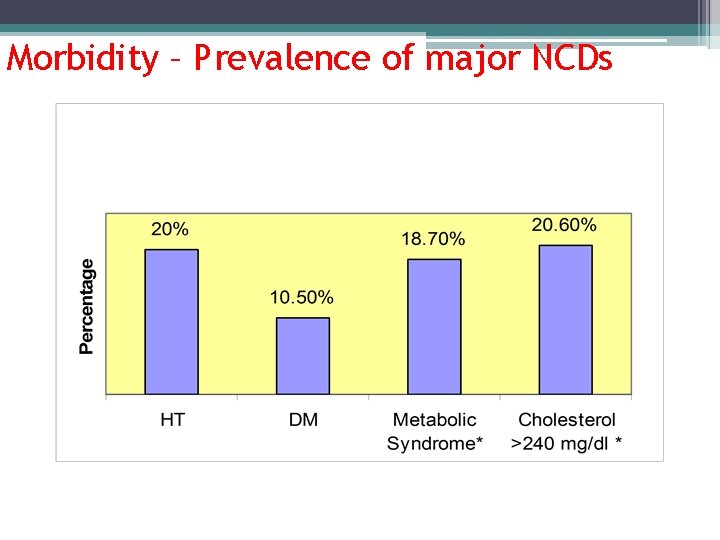
Morbidity – Prevalence of major NCDs
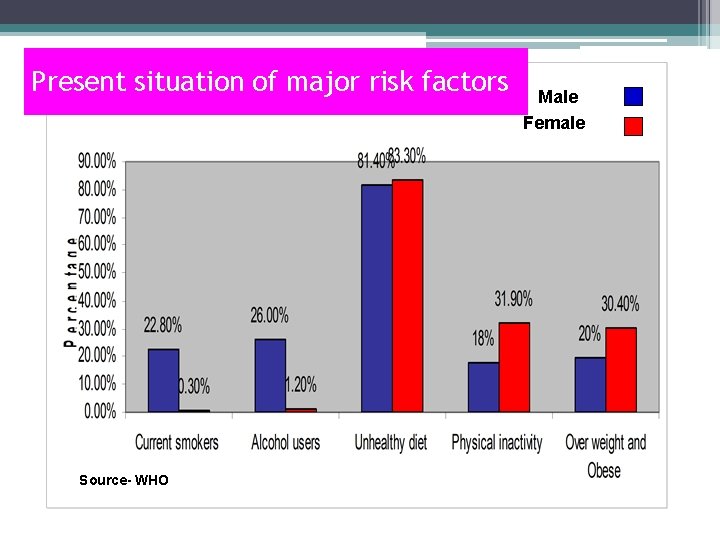
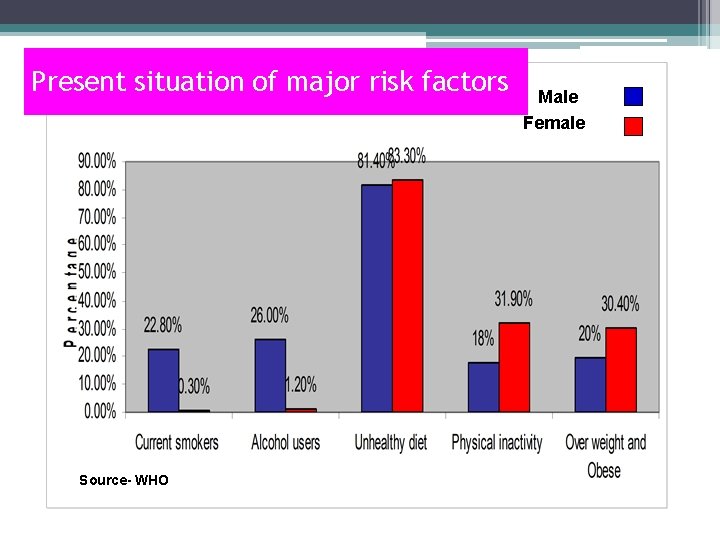
Present situation of major risk factors Source- WHO Male Female
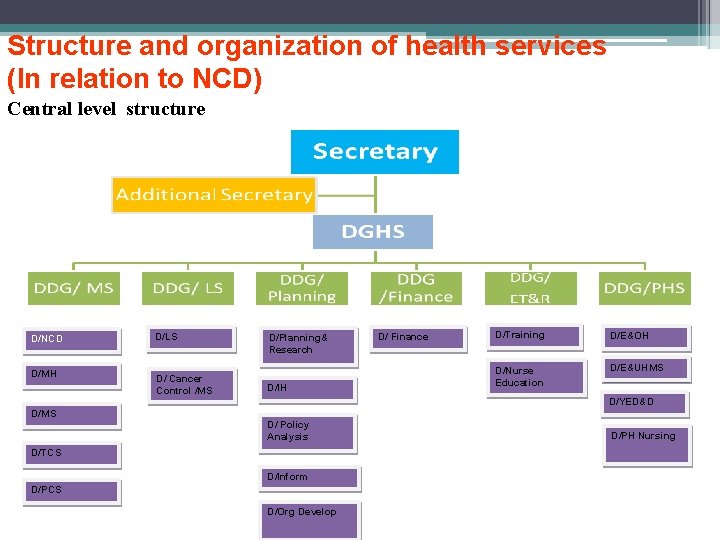
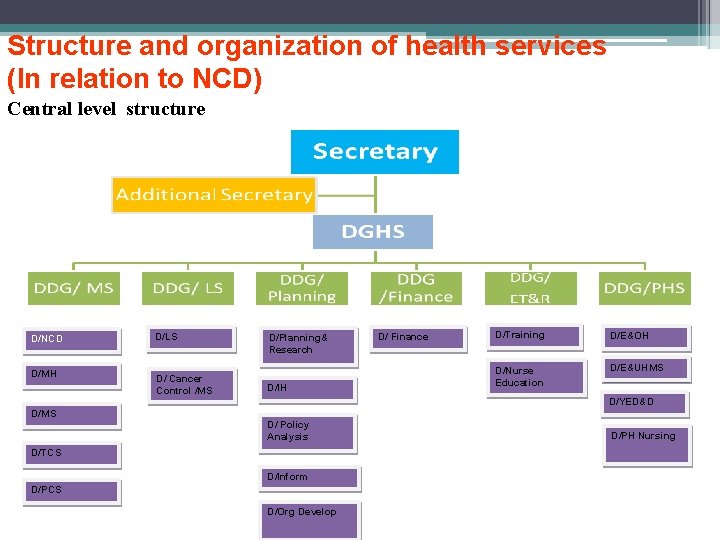
Structure and organization of health services (In relation to NCD) Central level structure D/NCD D/LS D/MH D/ Cancer Control /MS D/Planning& Research D/IH D/ Finance D/Training D/E&OH D/Nurse Education D/E&UHMS D/YED&D D/MS D/ Policy Analysis D/TCS D/Inform D/PCS D/Org Develop D/PH Nursing
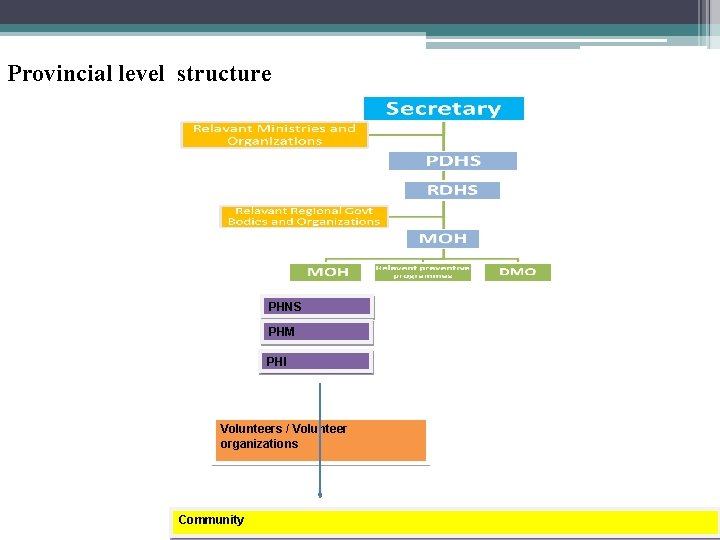
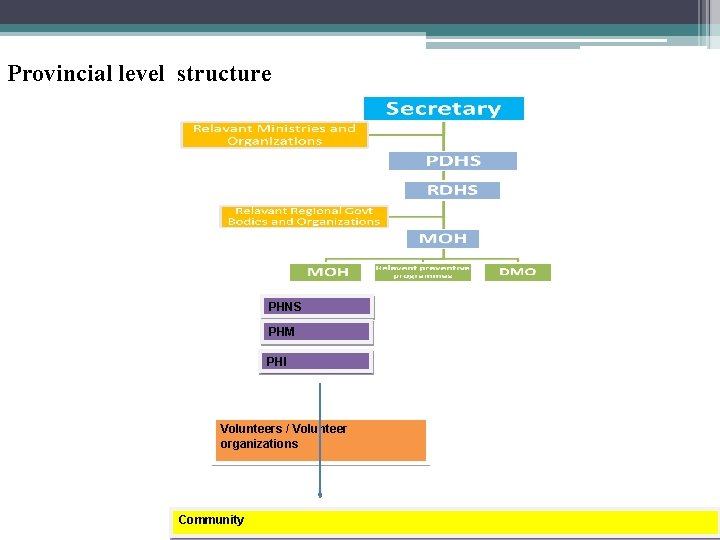
Provincial level structure PHNS PHM PHI Volunteers / Volunteer organizations Community
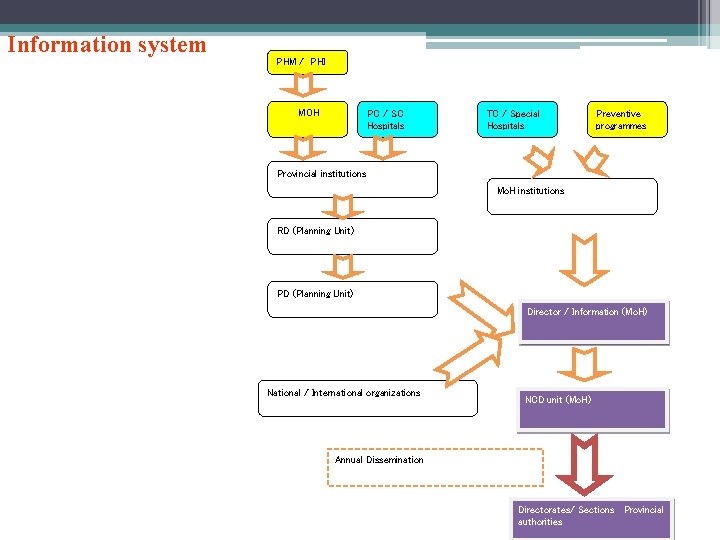
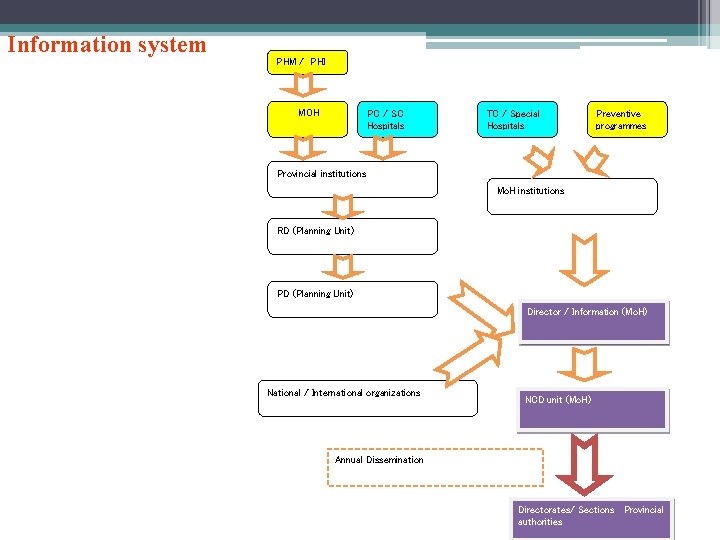
Information system PHM / PHI MOH PC / SC Hospitals TC / Special Hospitals Preventive programmes Provincial institutions Mo. H institutions RD (Planning Unit) PD (Planning Unit) Director / Information (Mo. H) National / International organizations NCD unit (Mo. H) Annual Dissemination Directorates/ Sections Provincial authorities
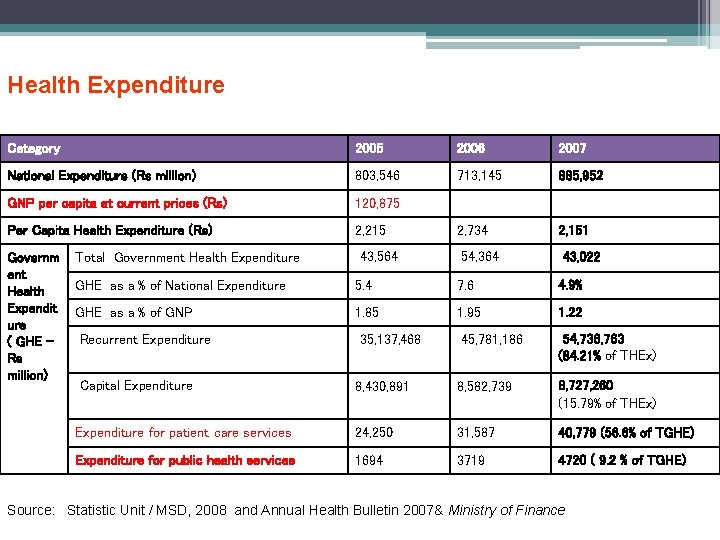
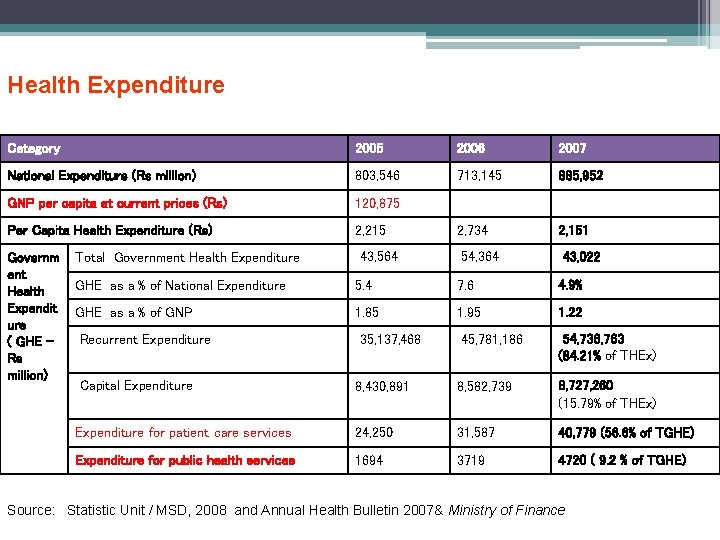
Health Expenditure Category 2005 2006 2007 National Expenditure (Rs million) 803, 546 713, 145 885, 952 GNP per capita at current prices (Rs) 120, 875 Per Capita Health Expenditure (Rs) 2, 215 2, 734 2, 151 Governm ent Health Expendit ure ( GHE Rs million) Total Government Health Expenditure 43, 564 54, 364 43, 022 GHE as a % of National Expenditure 5. 4 7. 6 4. 9% GHE as a % of GNP 1. 85 1. 95 1. 22 Recurrent Expenditure Capital Expenditure 35, 137, 468 45, 781, 186 54, 736, 763 (84. 21% of THEx) 8, 430, 891 8, 582, 739 8, 727, 260 (15. 79% of THEx) Expenditure for patient care services 24, 250 31, 587 40, 779 (56. 6% of TGHE) Expenditure for public health services 1694 3719 4720 ( 9. 2 % of TGHE) Source: Statistic Unit / MSD, 2008 and Annual Health Bulletin 2007& Ministry of Finance
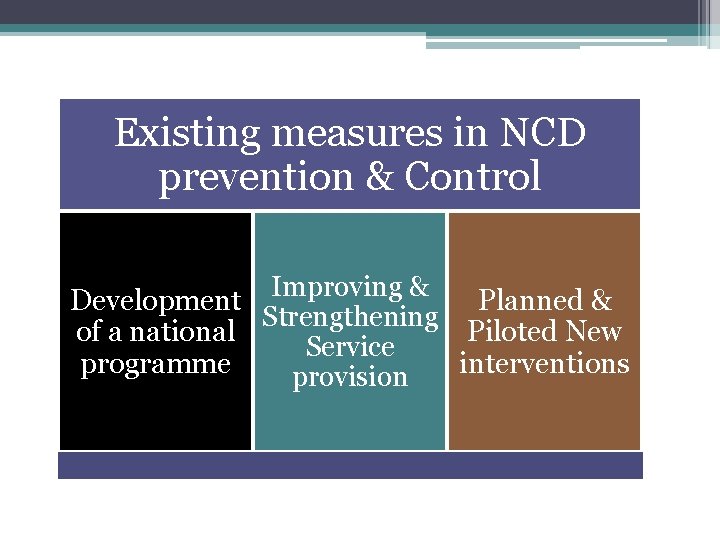
Existing Measures in NCD Prevention & Control
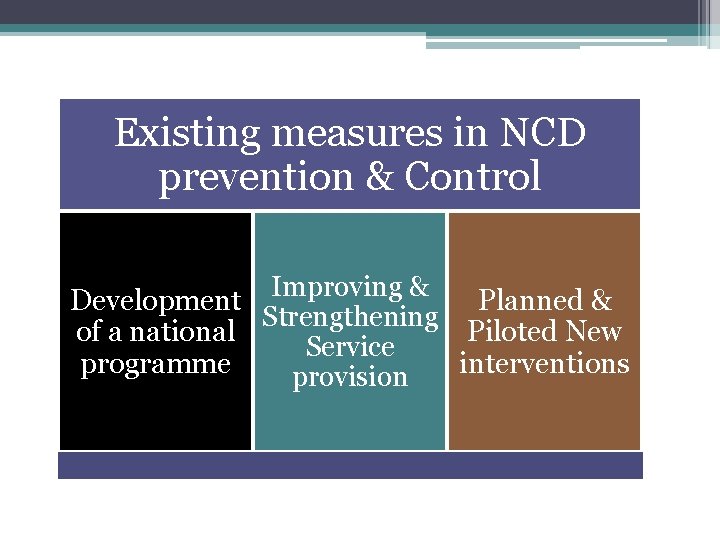
Existing measures in NCD prevention & Control Improving & Development Planned & Strengthening of a national Piloted New Service programme interventions provision
Achievements In legislation Tobacco Control Act and proper implementation In the system Identification of NCD as a priority in Health Policy and Health Master Plan Development of policy and strategic plan and district level implementation plans Pilot projects are being completed Coordination of other stakeholders – in the Mo. H as well as outside Advocacy and cooperation from other sectors to make their policy and environment healthy
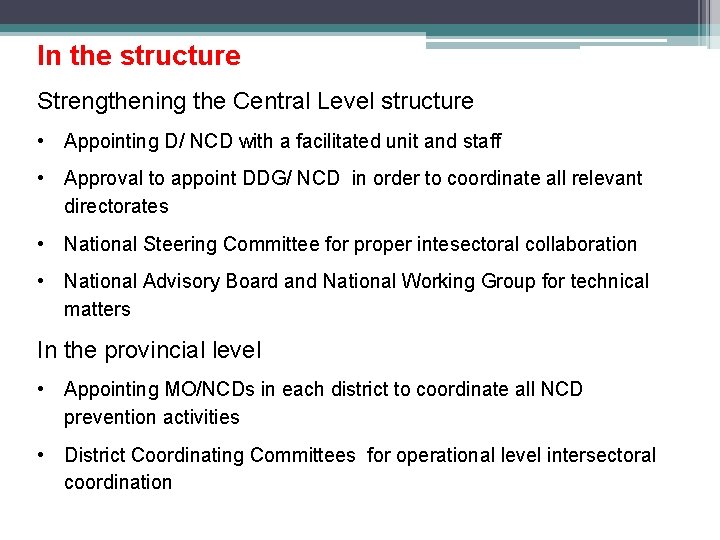
In the structure Strengthening the Central Level structure • Appointing D/ NCD with a facilitated unit and staff • Approval to appoint DDG/ NCD in order to coordinate all relevant directorates • National Steering Committee for proper intesectoral collaboration • National Advisory Board and National Working Group for technical matters In the provincial level • Appointing MO/NCDs in each district to coordinate all NCD prevention activities • District Coordinating Committees for operational level intersectoral coordination
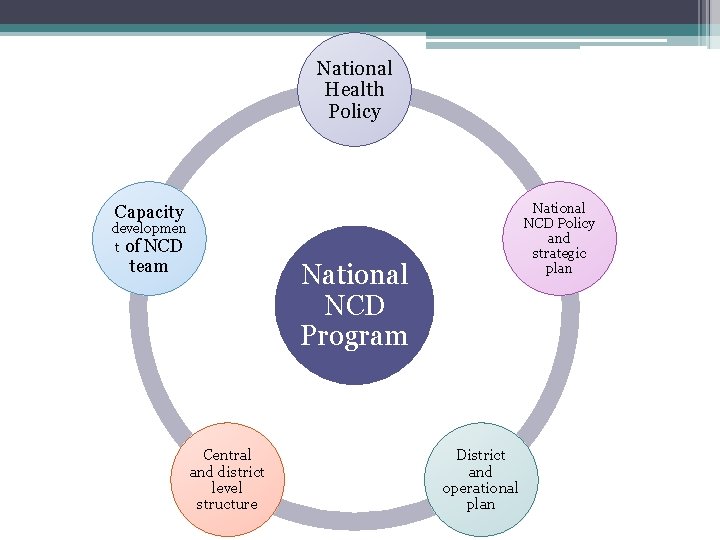
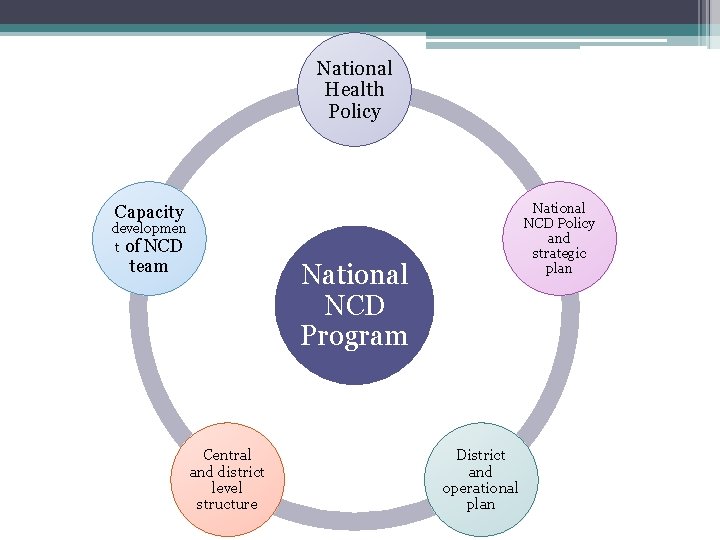
National Health Policy National NCD Policy and strategic plan Capacity developmen t of NCD team National NCD Program Central and district level structure District and operational plan
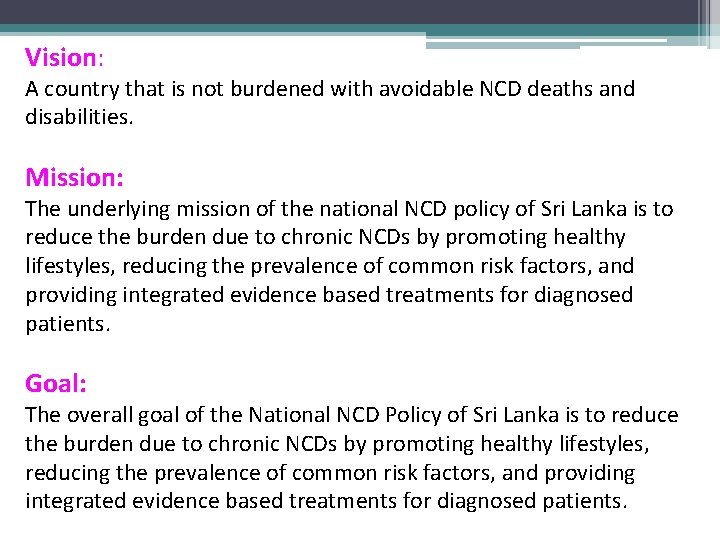
Vision: A country that is not burdened with avoidable NCD deaths and disabilities. Mission: The underlying mission of the national NCD policy of Sri Lanka is to reduce the burden due to chronic NCDs by promoting healthy lifestyles, reducing the prevalence of common risk factors, and providing integrated evidence based treatments for diagnosed patients. Goal: The overall goal of the National NCD Policy of Sri Lanka is to reduce the burden due to chronic NCDs by promoting healthy lifestyles, reducing the prevalence of common risk factors, and providing integrated evidence based treatments for diagnosed patients.
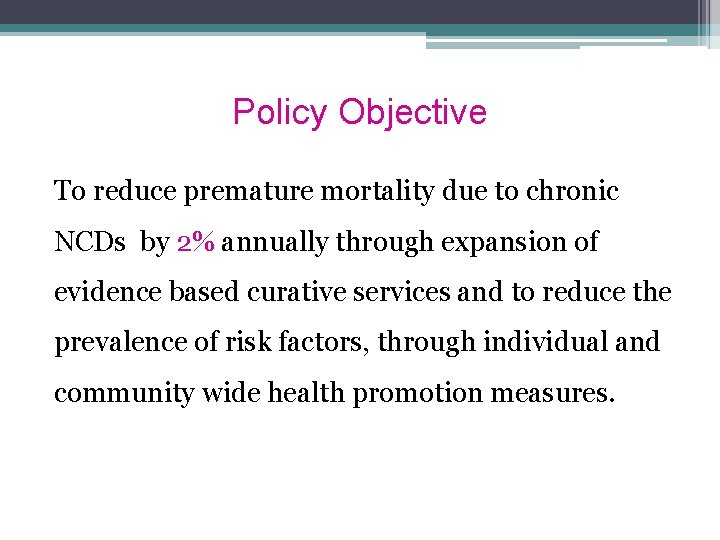
Policy Objective To reduce premature mortality due to chronic NCDs by 2% annually through expansion of evidence based curative services and to reduce the prevalence of risk factors, through individual and community wide health promotion measures.
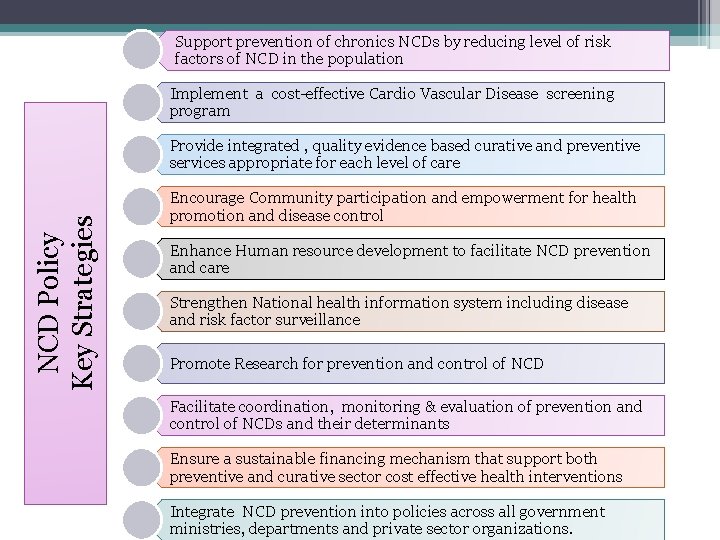
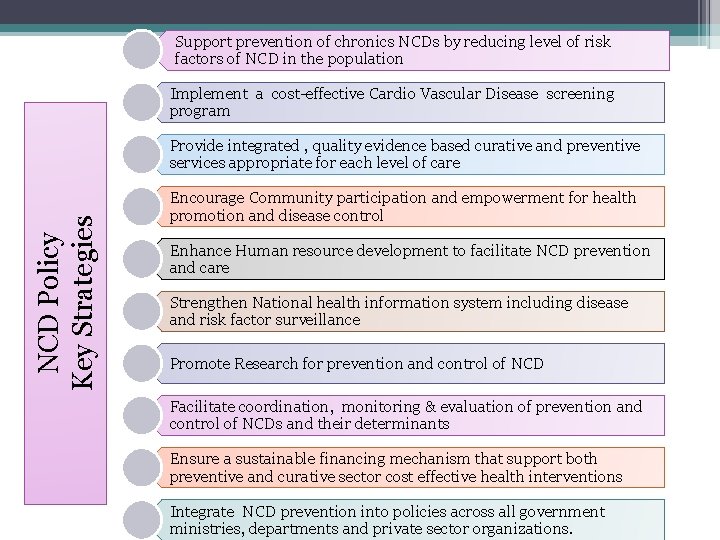
Support prevention of chronics NCDs by reducing level of risk factors of NCD in the population Implement a cost-effective Cardio Vascular Disease screening program NCD Policy Key Strategies Provide integrated , quality evidence based curative and preventive services appropriate for each level of care Encourage Community participation and empowerment for health promotion and disease control Enhance Human resource development to facilitate NCD prevention and care Strengthen National health information system including disease and risk factor surveillance Promote Research for prevention and control of NCD Facilitate coordination, monitoring & evaluation of prevention and control of NCDs and their determinants Ensure a sustainable financing mechanism that support both preventive and curative sector cost effective health interventions Integrate NCD prevention into policies across all government ministries, departments and private sector organizations.

Health Ministry Media NGO s National NCD Program Colleges (Physicians, GPs) Other Ministries Sri Lanka Medical Association (SLMA)
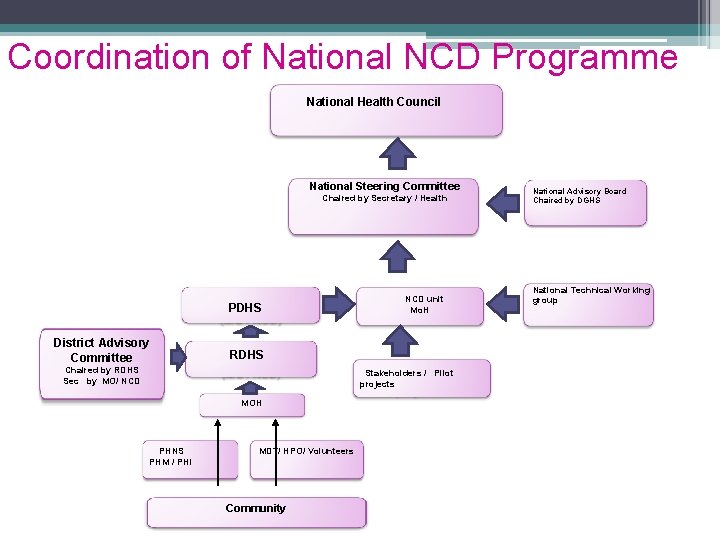
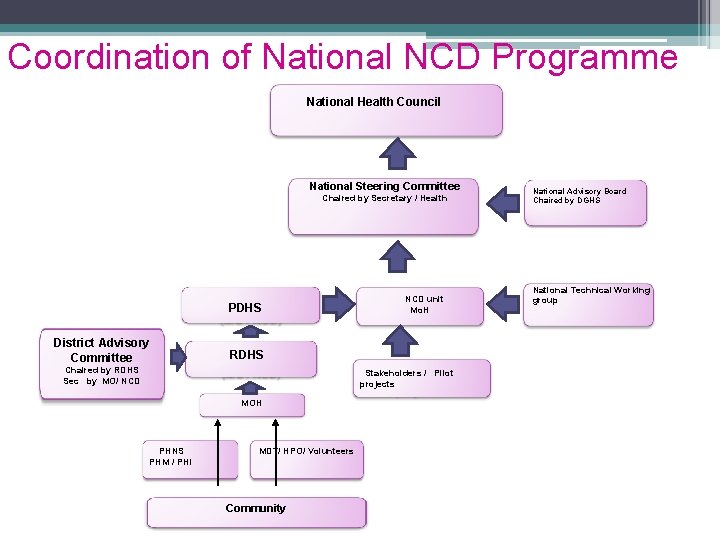
Coordination of National NCD Programme National Health Council National Steering Committee Chaired by Secretary / Health PDHS District Advisory Committee NCD unit Mo. H RDHS Chaired by RDHS Sec by MO/ NCD Stakeholders / Pilot projects MOH PHNS PHM / PHI MDT/ HPO/ Volunteers Community National Advisory Board Chaired by DGHS National Technical Working group

Inter Ministerial Collaborations Ministry of Education Ministry of Public administration & Home Affairs Health & Nutrition Ministry of Agriculture Ministry of Social Services Ministry of Media & Mass Communication
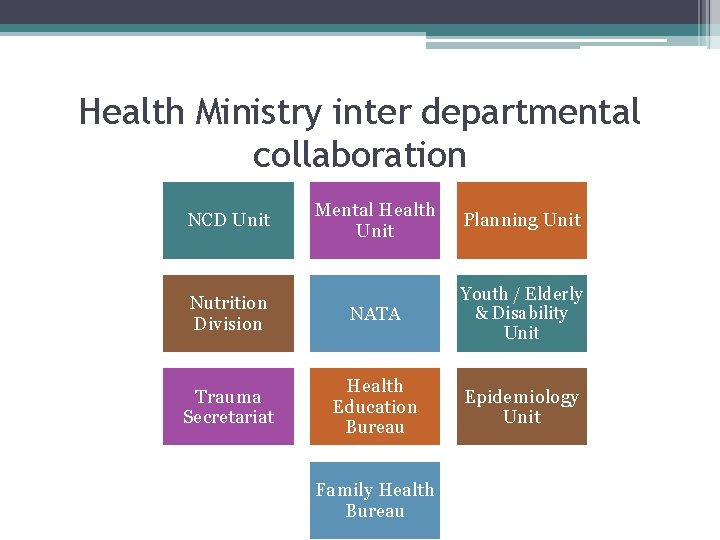
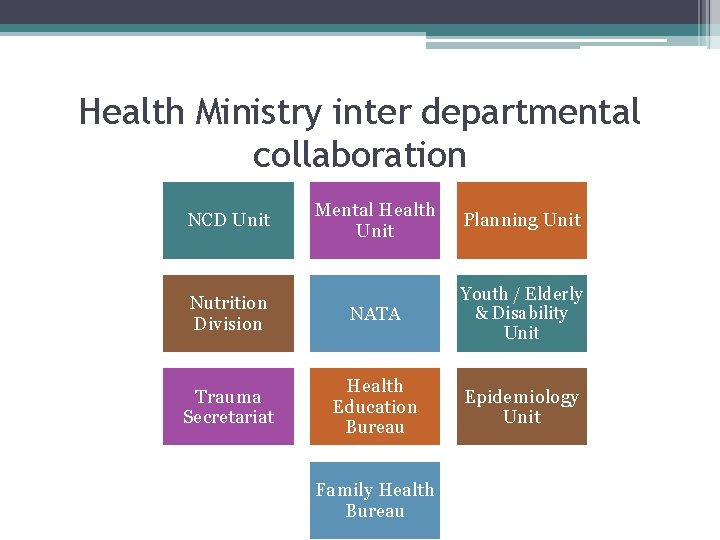
Health Ministry inter departmental collaboration Mental Health Unit Planning Unit Nutrition Division NATA Youth / Elderly & Disability Unit Trauma Secretariat Health Education Bureau Epidemiology Unit NCD Unit Family Health Bureau
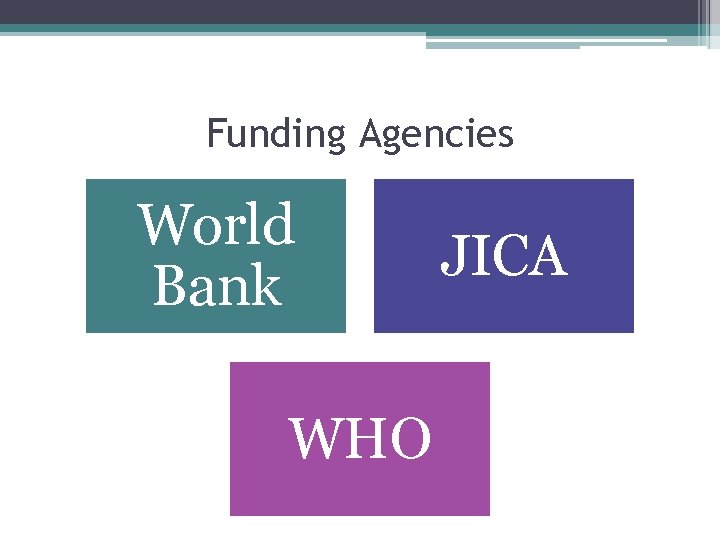
Funding Agencies World Bank WHO JICA
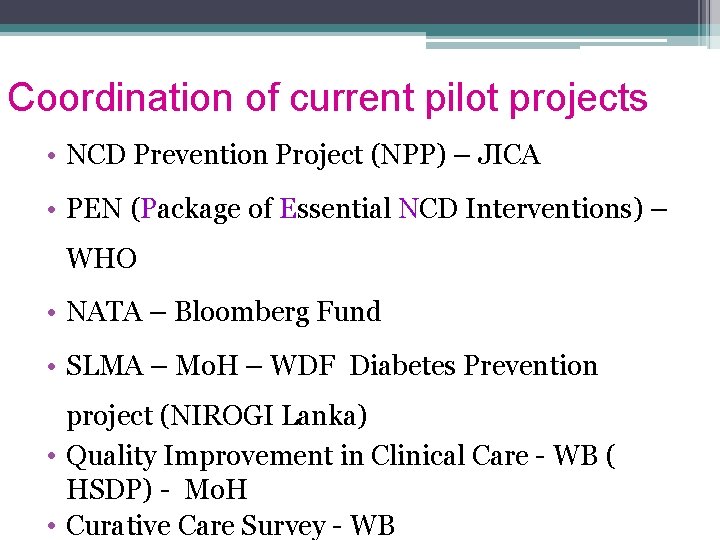
Coordination of current pilot projects • NCD Prevention Project (NPP) – JICA • PEN (Package of Essential NCD Interventions) – WHO • NATA – Bloomberg Fund • SLMA – Mo. H – WDF Diabetes Prevention project (NIROGI Lanka) • Quality Improvement in Clinical Care - WB ( HSDP) - Mo. H • Curative Care Survey - WB
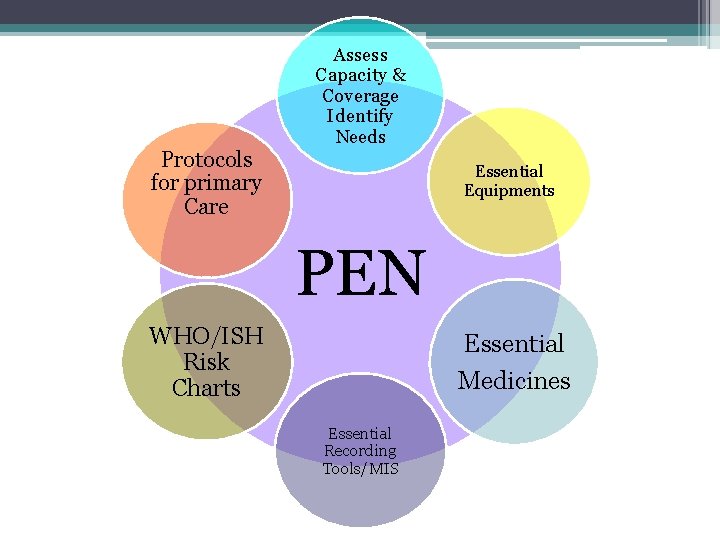
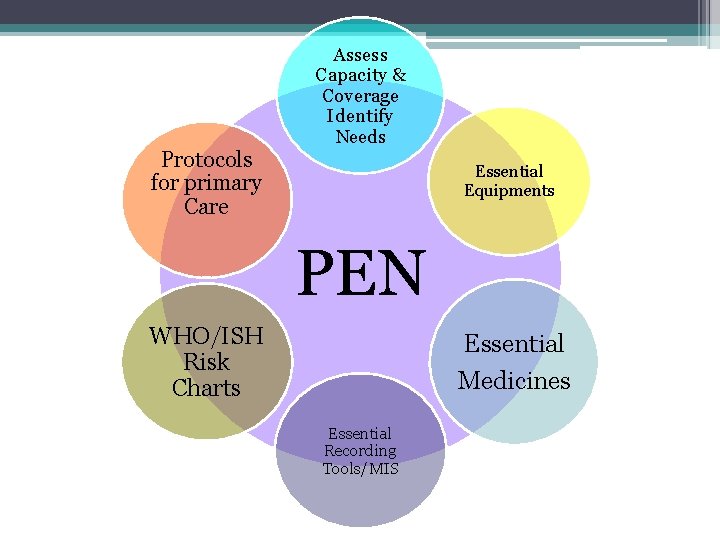
Protocols for primary Care Assess Capacity & Coverage Identify Needs Essential Equipments PEN WHO/ISH Risk Charts Essential Medicines Essential Recording Tools/MIS
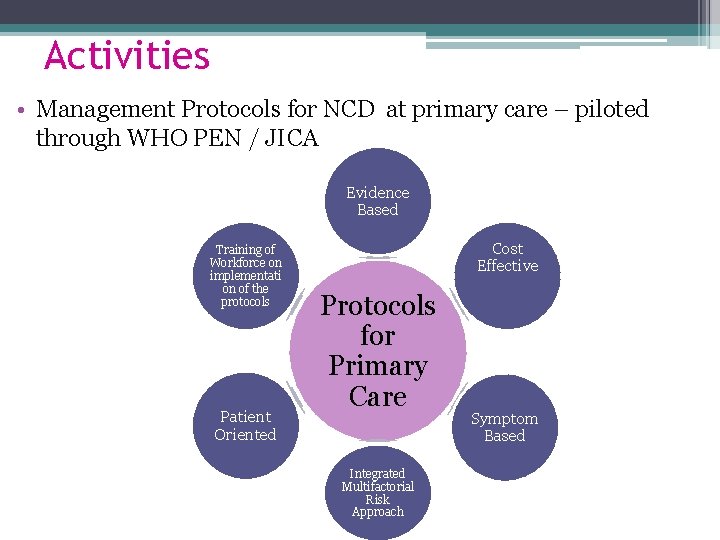
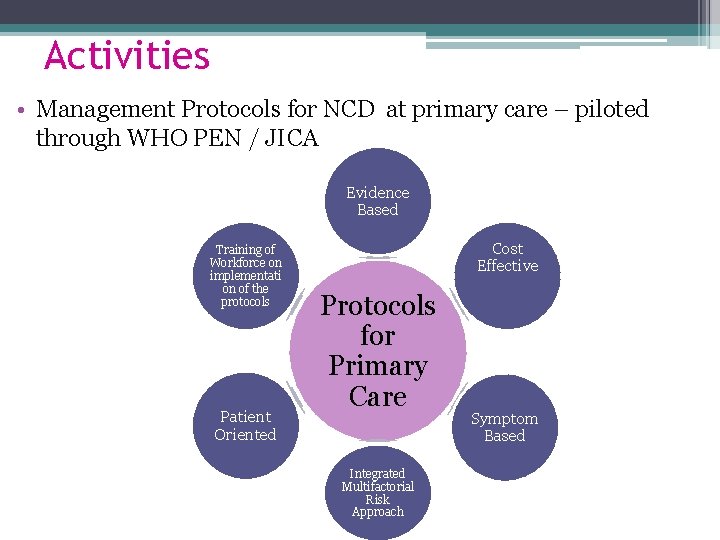
Activities • Management Protocols for NCD at primary care – piloted through WHO PEN / JICA Evidence Based Training of Workforce on implementati on of the protocols Patient Oriented Cost Effective Protocols for Primary Care Integrated Multifactorial Risk Approach Symptom Based
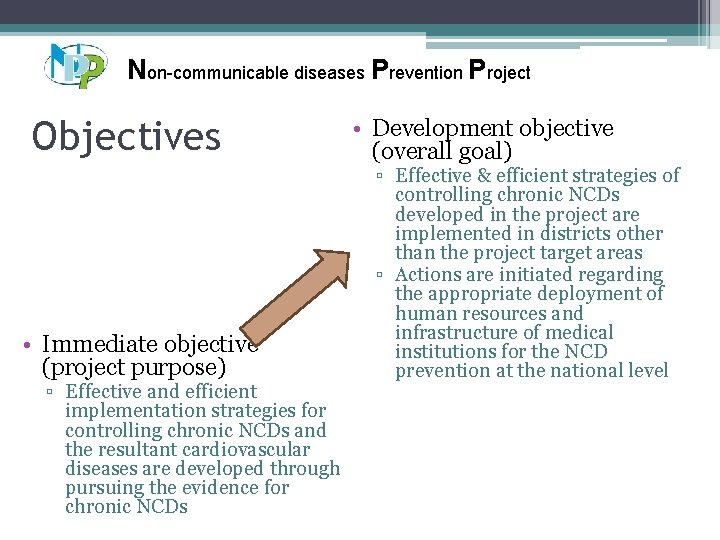
Non-communicable diseases Prevention Project Objectives • Immediate objective (project purpose) ▫ Effective and efficient implementation strategies for controlling chronic NCDs and the resultant cardiovascular diseases are developed through pursuing the evidence for chronic NCDs • Development objective (overall goal) ▫ Effective & efficient strategies of controlling chronic NCDs developed in the project are implemented in districts other than the project target areas ▫ Actions are initiated regarding the appropriate deployment of human resources and infrastructure of medical institutions for the NCD prevention at the national level 33
Future Plans
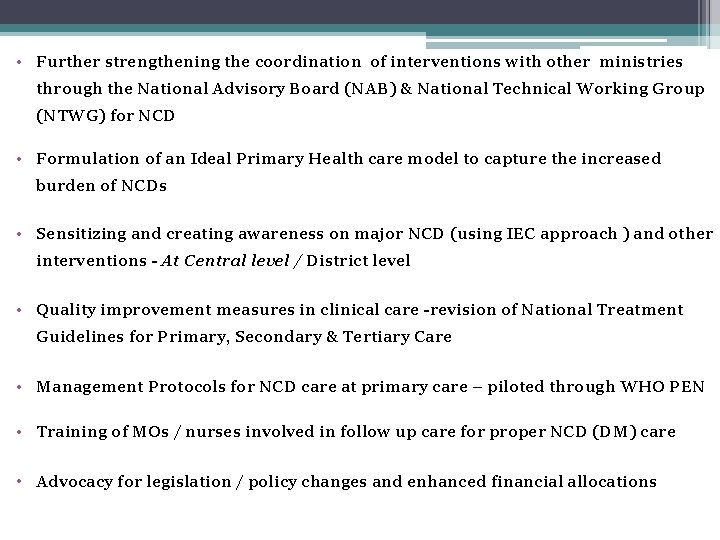
• Further strengthening the coordination of interventions with other ministries through the National Advisory Board (NAB) & National Technical Working Group (NTWG) for NCD • Formulation of an Ideal Primary Health care model to capture the increased burden of NCDs • Sensitizing and creating awareness on major NCD (using IEC approach ) and other interventions - At Central level / District level • Quality improvement measures in clinical care -revision of National Treatment Guidelines for Primary, Secondary & Tertiary Care • Management Protocols for NCD care at primary care – piloted through WHO PEN • Training of MOs / nurses involved in follow up care for proper NCD (DM) care • Advocacy for legislation / policy changes and enhanced financial allocations
Countrywide expansion of the NCD programme (with cost effective screening, health promotion, social marketing campaign) Advocacy meeting to other Ministries / provincial political authorities /Sectors / Media Advocacy for strengthening curative care in every level in relation to NCD management Review of district operational plan and district level NCD activity Development of communication strategy and surveillance system for NCD Strengthen health Promotion in all settings Initiate formulation of a National Cancer Control Strategic Plan Strengthen of the tobacco and alcohol programme Production of master trainers for NCD programme / tobacco & alcohol programme District level capacity building Training of MO/NCD, MOH, PHI, PHM & officers in other relevant sectors Mobilizing youth and community leaders towards prevention of NCD Multidisciplinary Research effort with agreed research agenda Review of pilot projects & NATA (JICA / Nirogi Lanka / PEN / Bloomberg )
Challenges in Implementing National NCD Programme
Challenges in the System : • Lack of adequate NCD /risk factor surveillance system • Quality improvement in clinical care based on standard guidelines • Maintaining coordination between all sectors & stakeholders • Behavioral change among the public • Lack of adequate Monitoring & Evaluation system • Lack of Policy decision on model of primary health care set up • Multinational company involments
Challenges in Human Resources: §HR constraints for providing optimal care for NCDs §Gaps in recruiting and training of staff for NCD care at primary and secondary care §Capacity building in central / district level §Lack of policy decision on involvement of field officers (PHI & PHM) for community level health promotion, basic screening and follow up for NCDs
Challenges in Funding: • Lack of funding for development of district level NCD implementation units • Lack of funding for district level activities • Lack of funding for social marketing campaign
lessons learnt over the last 5 yrs • Priority on Iry prevention but IIry prevention also needed • Need dedicated leadership • Intersecoral coordination and collaboration is a must
Thank You