Developing Clinic Based Case Management Care Coordination An
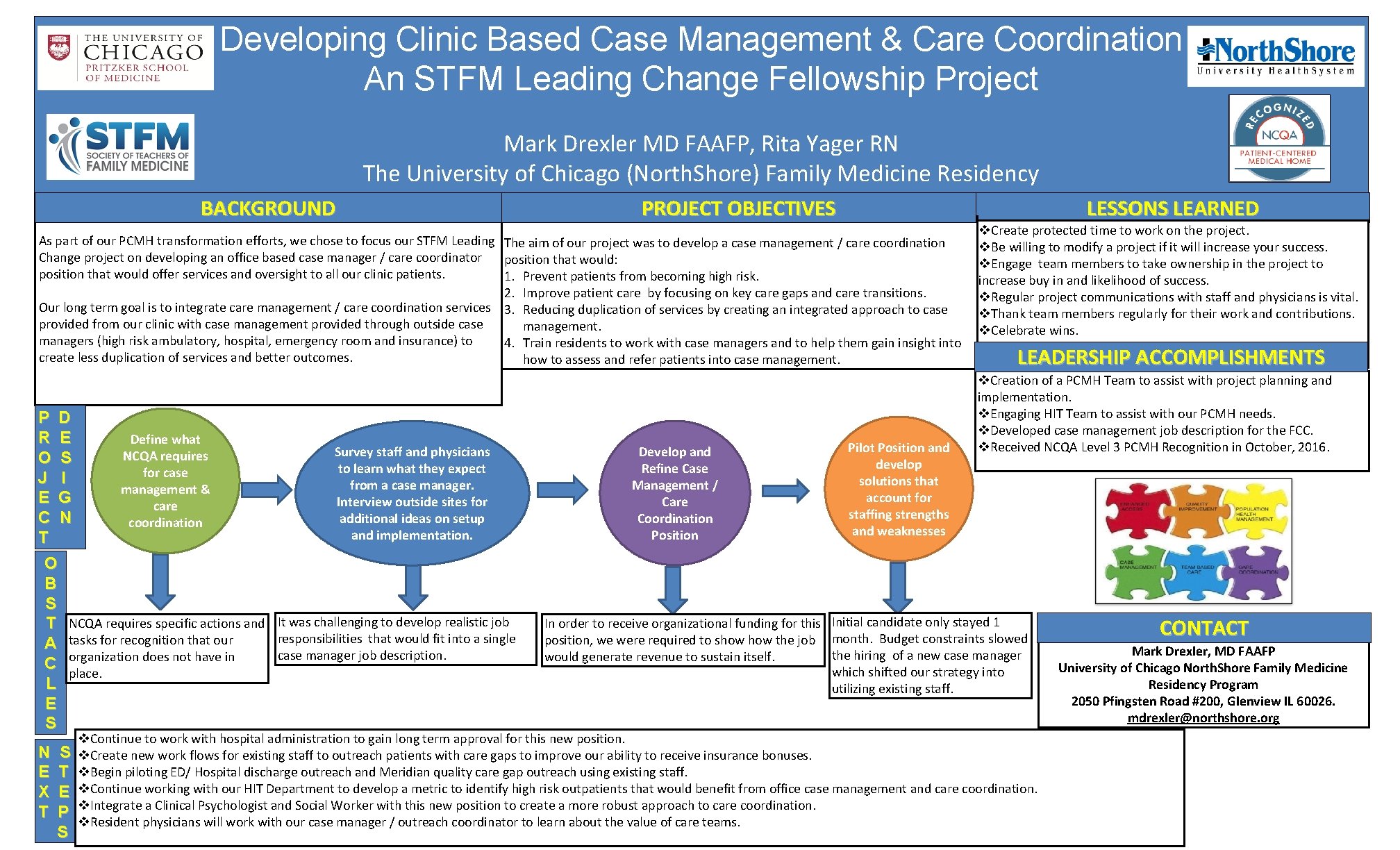
Developing Clinic Based Case Management & Care Coordination An STFM Leading Change Fellowship Project Mark Drexler MD FAAFP, Rita Yager RN The University of Chicago (North. Shore) Family Medicine Residency BACKGROUND PROJECT OBJECTIVES LESSONS LEARNED As part of our PCMH transformation efforts, we chose to focus our STFM Leading The aim of our project was to develop a case management / care coordination Change project on developing an office based case manager / care coordinator position that would: position that would offer services and oversight to all our clinic patients. 1. Prevent patients from becoming high risk. 2. Improve patient care by focusing on key care gaps and care transitions. Our long term goal is to integrate care management / care coordination services 3. Reducing duplication of services by creating an integrated approach to case provided from our clinic with case management provided through outside case management. managers (high risk ambulatory, hospital, emergency room and insurance) to 4. Train residents to work with case managers and to help them gain insight into create less duplication of services and better outcomes. how to assess and refer patients into case management. P D R E Define what Survey staff and physicians NCQA requires O S to learn what they expect for case J I from a case manager. management & E G Interview outside sites for care additional ideas on setup C N coordination and implementation. T O B S T NCQA requires specific actions and It was challenging to develop realistic job responsibilities that would fit into a single A tasks for recognition that our case manager job description. C organization does not have in place. L E S N E X T S T E P S Develop and Refine Case Management / Care Coordination Position Pilot Position and develop solutions that account for staffing strengths and weaknesses v. Create protected time to work on the project. v. Be willing to modify a project if it will increase your success. v. Engage team members to take ownership in the project to increase buy in and likelihood of success. v. Regular project communications with staff and physicians is vital. v. Thank team members regularly for their work and contributions. v. Celebrate wins. LEADERSHIP ACCOMPLISHMENTS v. Creation of a PCMH Team to assist with project planning and implementation. v. Engaging HIT Team to assist with our PCMH needs. v. Developed case management job description for the FCC. v. Received NCQA Level 3 PCMH Recognition in October, 2016. In order to receive organizational funding for this Initial candidate only stayed 1 position, we were required to show the job month. Budget constraints slowed the hiring of a new case manager would generate revenue to sustain itself. which shifted our strategy into utilizing existing staff. v. Continue to work with hospital administration to gain long term approval for this new position. v. Create new work flows for existing staff to outreach patients with care gaps to improve our ability to receive insurance bonuses. v. Begin piloting ED/ Hospital discharge outreach and Meridian quality care gap outreach using existing staff. v. Continue working with our HIT Department to develop a metric to identify high risk outpatients that would benefit from office case management and care coordination. v. Integrate a Clinical Psychologist and Social Worker with this new position to create a more robust approach to care coordination. v. Resident physicians will work with our case manager / outreach coordinator to learn about the value of care teams. CONTACT Mark Drexler, MD FAAFP University of Chicago North. Shore Family Medicine Residency Program 2050 Pfingsten Road #200, Glenview IL 60026. mdrexler@northshore. org
- Slides: 1