DEVELOPING A PROCESS MAP SAMPLE SLIDE DECK OVERVIEW
- Slides: 17
“DEVELOPING A PROCESS MAP” SAMPLE SLIDE DECK
OVERVIEW • Understand the steps to complete a process map • Create a sample process map from the hospital discharge to nursing home admission • Use principles learned to create process maps with your hospital-nursing home teams, for example: – Hospital discharge process to nursing home – Nursing home transfer process to ED – ED transfer process to inpatient hospital admission or back to the nursing home
WHY DEVELOP A PROCESS MAP? • Benefits: – To help hospitals and nursing homes better understand care transitions activities at each other’s facilities – To identify areas or tasks, that can be improved – To determine what works well and potentially apply these principles to other areas – To assist in the process of conducting case reviews
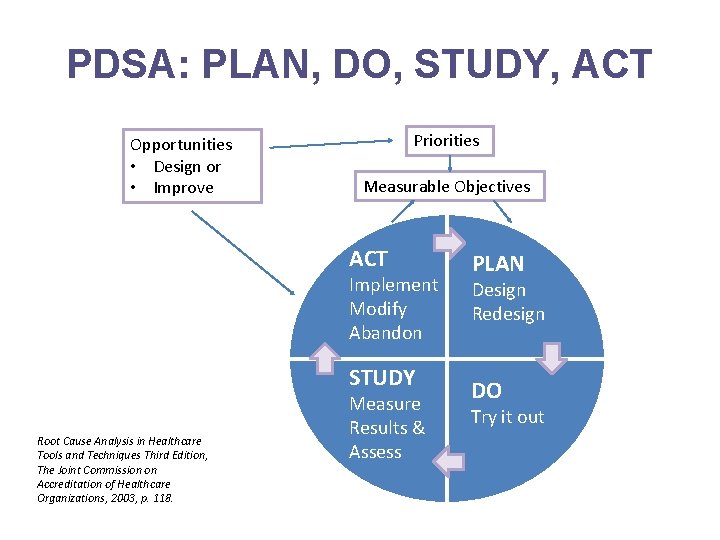
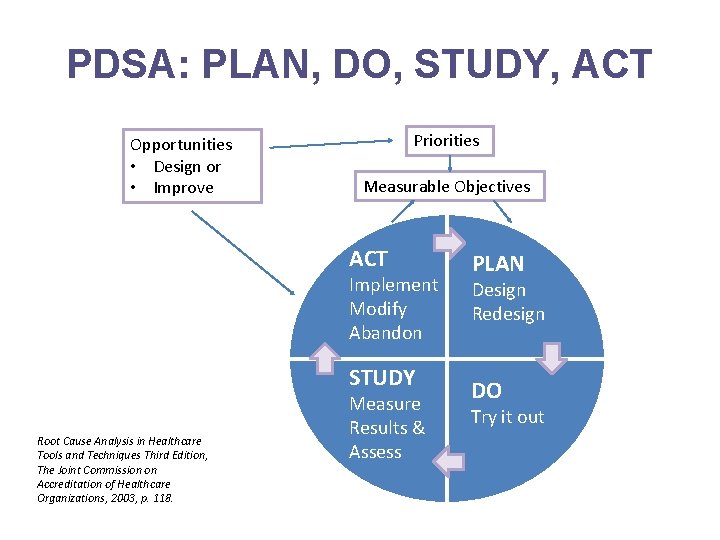
PDSA: PLAN, DO, STUDY, ACT Opportunities • Design or • Improve Priorities Measurable Objectives ACT Implement Modify Abandon STUDY Root Cause Analysis in Healthcare Tools and Techniques Third Edition, The Joint Commission on Accreditation of Healthcare Organizations, 2003, p. 118. Measure Results & Assess PLAN Design Redesign DO Try it out
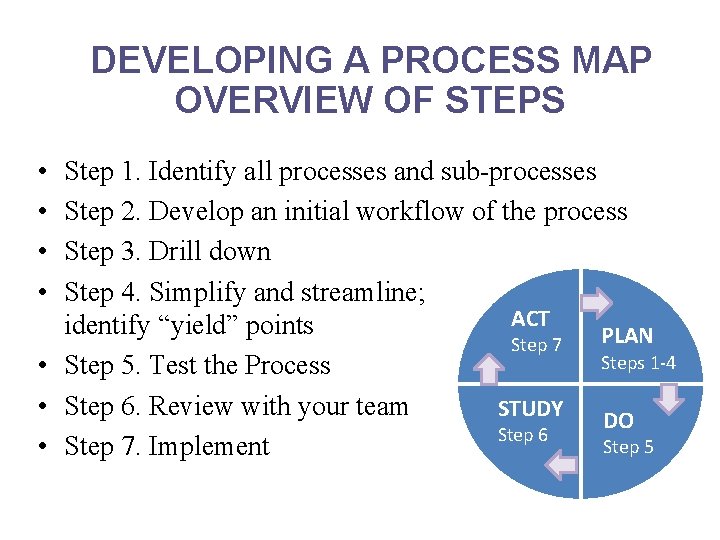
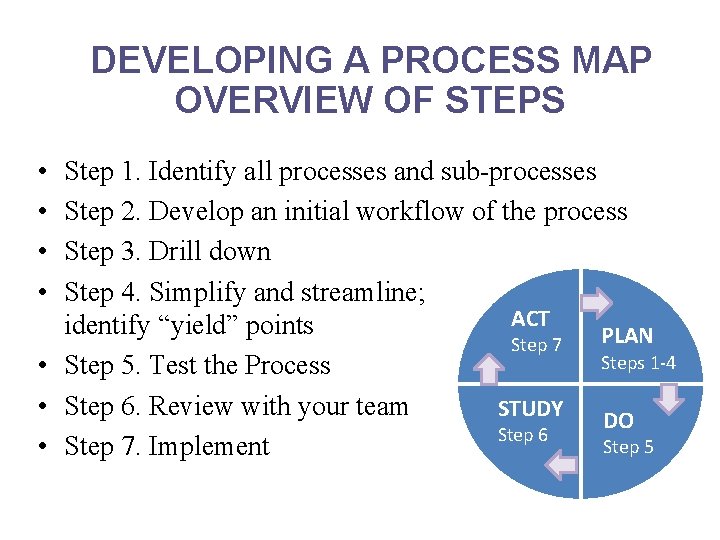
DEVELOPING A PROCESS MAP OVERVIEW OF STEPS • • Step 1. Identify all processes and sub-processes Step 2. Develop an initial workflow of the process Step 3. Drill down Step 4. Simplify and streamline; ACT identify “yield” points PLAN Step 7 Steps 1 -4 • Step 5. Test the Process • Step 6. Review with your team STUDY DO Step 6 Step 5 • Step 7. Implement
STEP 1: IDENTIFY ALL PROCESS AND SUB-PROCESSES
STEP 2: DEVELOPING AN INITIAL DRAFT • Develop an initial draft of the workflow between facilities (e. g. “warm” handoff between ED clinician and nursing home) – Can be formatted as a list or diagram • Meet as a multi-disciplinary team to discuss the processes – Ideally, ensure different disciplines are represented (clinicians, residents, nurses, social workers, case management, frontline staff etc. ) – Consider what occurs during different shifts • Clarify specific roles and contributions of the process team members
STEP 2: QUESTIONS TO CONSIDER WHEN DEVELOPING A DRAFT PROCESS MAP • What currently takes place? – Is this different from what ideally should take place? – Does this process occur 24/7? Only on weekdays? – Are certain tasks dependent on someone or something? • What processes are critical? • Where are the gaps or barriers?
STEP 3: DRILL DOWN • Consider areas that might require further drill down: – Are there points of accountability for sending and receiving information? – Improve communications during transitions between providers, patients, and caregivers • Timeliness, completeness, and accuracy of information transferred.
STEP 3: POTENTIAL AREAS THAT MAY REQUIRE FURTHER DRILL DOWN • Information Sharing Processes – – – Who is sending the information? How is the information being shared? Is the appropriate information being communicated? When is the information being shared? Is it being shared in a timely manner? • Communication Processes – For staff identified on the contact list: • What shifts do they cover? • What are the contingency plans if they are on vacation or out sick? – For phone numbers listed, is it a cell phone, landline, main hotline? – Are you aware of a hotline in the ED to call when transferring residents?
STEP 4: SIMPLIFY AND STREAMLINE; IDENTIFY “YIELD” POINTS • Identify areas where processes can be simplified, standardized and streamlined • Identify critical points in the process map – Areas that are barriers and may slow down (“yields”) processes – Areas that require proceeding with caution – Dependent tasks • Revise
STEP 4: QUESTIONS TO CONSIDER • Where are there redundancies in the process? • Where can information and communication be standardized within your organization and across care settings? • How can you streamline your readmission reduction activities?
STEP 5: TEST THE PROCESS MAP • Apply the process map to an actual case or conduct a walkthrough using the process map – Test whether the processes align; record what processes do not align – Record gaps or areas for improvement • Anticipate roadblocks • Revise as necessary
STEP 6: REVIEW THE PROCESS MAP WITH YOUR TEAM • Recap the process mapping exercise: – What did the exercise uncover? – What areas are working well? – What areas need to be improved? • Focus on the areas can easily be modified and improved – Discuss potential revisions and revise process map
STEP 7: IMPLEMENT • Develop a plan to educate frontline staff on the new process(es) • Implement and monitor progress; determine if any revisions are necessary • Consider reconvening team if significant changes are needed
HOW DO WE TRACK PROCESSES WHEN THEY SUCCEED OR FAIL?
SUSTAINING EFFORTS • Keep staff informed of progress, successes, and failures. • Share results outside of the organization. Present your process and findings with your partner organizations. • Expand the scope to include all patients transferring into, out of, or within the facility. • Regardless of starting or destination points, focus on a key area of concern, such as medication reconciliation. • Look for participation from other departments or disciplines. • Educate other disciplines on their role in improving quality and safety of health care delivery as it relates to transitions of care. • It’s an iterative process.