Detecting Psychosis in the Primary Care Setting Presented
- Slides: 23
Detecting Psychosis in the Primary Care Setting Presented by: Jonathan Betlinski, MD Date: 02/25/2016
Disclosures and Learning Objectives: • Know the prevalence of psychotic symptoms in primary care • Know the 6 common symptom clusters for schizophrenia • Be able to list at least 5 reasons why an individual might be psychotic Disclosures: Dr. Jonathan Betlinski has nothing to disclose.
Psychosis in Primary Care • • • Review the epidemiology of psychosis Review common causes of psychosis Review diagnostic criteria for psychosis Discuss screening questions for psychosis Review the basic first steps of managing psychosis • Reveal next week’s topic
Psychosis: Epidemiology • 3. 7% of primary care patients report at least one psychotic symptom • Most common symptom is believing that others are spying on or following the individual http: //www. researchgate. net/publication/14290258_Psychotic_symptoms_in_primary_care • 50 -90% of those with a serious mental illness (SMI) have at least one chronic medical illness • Individuals with SMI die 25 years earlier http: //santabarbarastreetmedicine. org/wordpress/wp-content/uploads/2011/04/Schizophrenia-for-primary-care-providers-am-jm-2012. pdf • Up to 30% of individuals with psychotic symptoms rely solely on primary care https: //books. google. com/books? id=Jxfm 86 w. OR 8 UC&pg=PA 237&lpg=PA 237&dq=psychosis+in+the+primary+care+setti
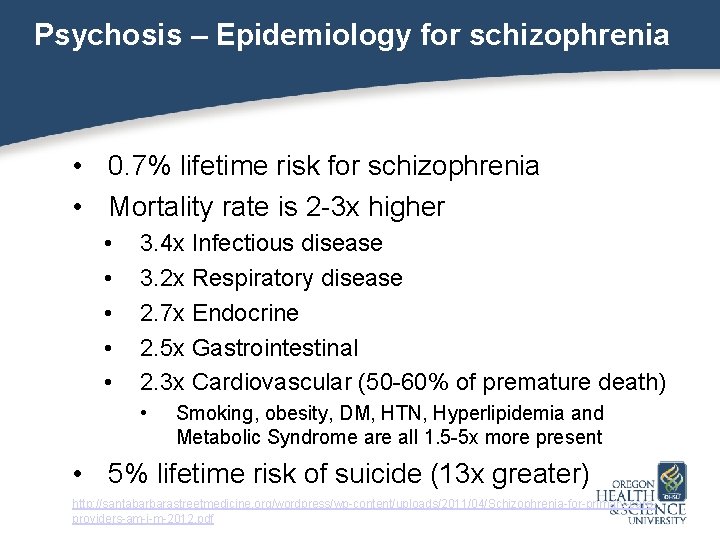
Psychosis – Epidemiology for schizophrenia • 0. 7% lifetime risk for schizophrenia • Mortality rate is 2 -3 x higher • • • 3. 4 x Infectious disease 3. 2 x Respiratory disease 2. 7 x Endocrine 2. 5 x Gastrointestinal 2. 3 x Cardiovascular (50 -60% of premature death) • Smoking, obesity, DM, HTN, Hyperlipidemia and Metabolic Syndrome are all 1. 5 -5 x more present • 5% lifetime risk of suicide (13 x greater) http: //santabarbarastreetmedicine. org/wordpress/wp-content/uploads/2011/04/Schizophrenia-for-primary-careproviders-am-j-m-2012. pdf
Psychosis is characterized by a loss of contact with reality • Delusions (fixed false beliefs) • • • Hallucinations (false sensory perceptions) Disorganized speech Disorganized behavior These problems lead to social or occupational dysfunction http: //www. nmji. in/archives/Volume_19_6_Nov_Dec_2006/Everyday_Practice_new/every_day_practice_19_6. htm
Psychosis – Psychological Causes • • • Schizophrenia Schizoaffective Disorder Brief Psychotic Disorder Major Depressive Disorder Bipolar I Disorder Psychotic Disorder, NOS Delusional Disorder Personality Disorders Narcolepsy http: //pro. psychcentral. com/dsm-5 -changes-schizophrenia-psychotic-disorders/004336. html# http: //www. nhs. uk/Conditions/Psychosis/Pages/Causes. aspx
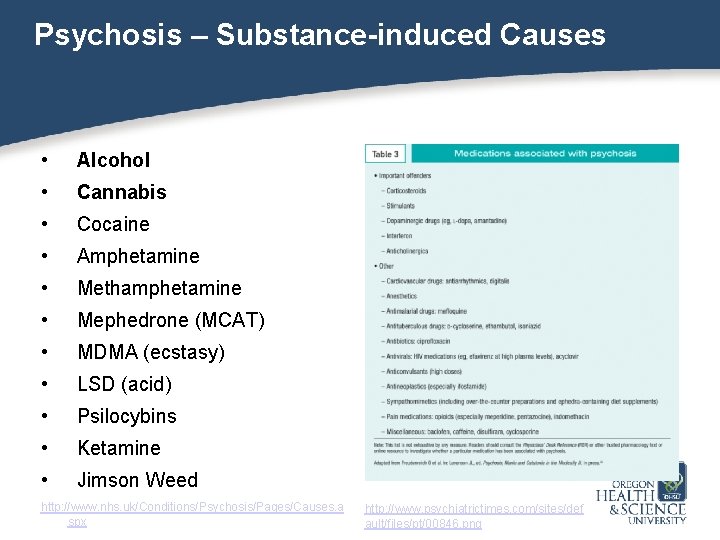
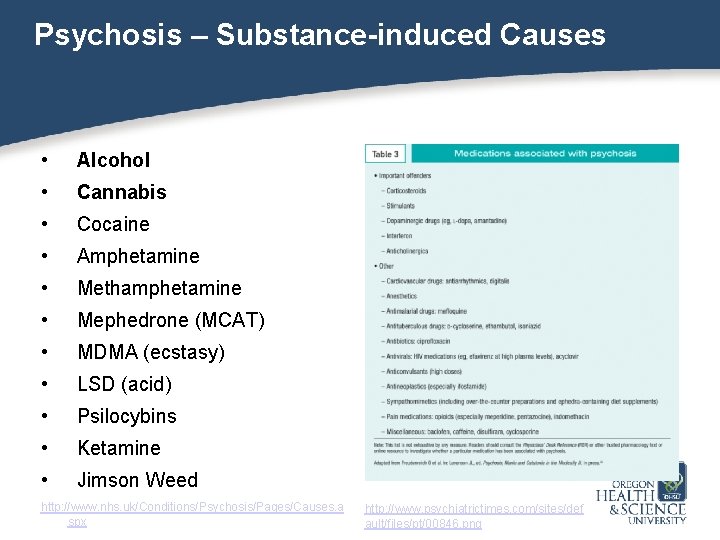
Psychosis – Substance-induced Causes • Alcohol • Cannabis • Cocaine • Amphetamine • Methamphetamine • Mephedrone (MCAT) • MDMA (ecstasy) • LSD (acid) • Psilocybins • Ketamine • Jimson Weed http: //www. nhs. uk/Conditions/Psychosis/Pages/Causes. a spx http: //www. psychiatrictimes. com/sites/def ault/files/pt/00846. png
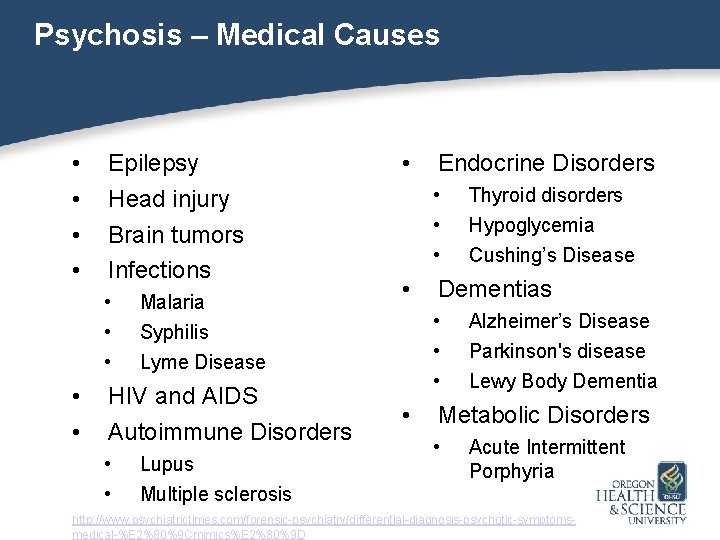
Psychosis – Medical Causes • • Epilepsy Head injury Brain tumors Infections • • • Malaria Syphilis Lyme Disease HIV and AIDS Autoimmune Disorders • • Lupus Multiple sclerosis • Endocrine Disorders • • Hypoglycemia Cushing’s Disease Dementias • • Thyroid disorders Alzheimer’s Disease Parkinson's disease Lewy Body Dementia Metabolic Disorders • Acute Intermittent Porphyria http: //www. psychiatrictimes. com/forensic-psychiatry/differential-diagnosis-psychotic-symptomsmedical-%E 2%80%9 Cmimics%E 2%80%9 D
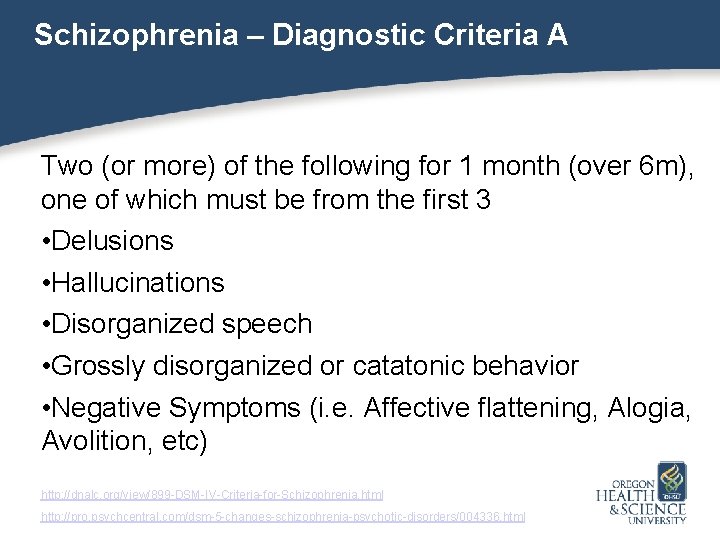
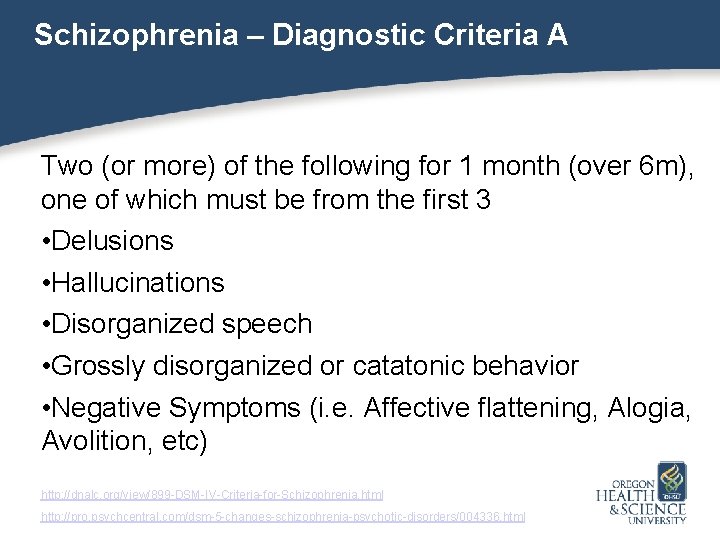
Schizophrenia – Diagnostic Criteria A Two (or more) of the following for 1 month (over 6 m), one of which must be from the first 3 • Delusions • Hallucinations • Disorganized speech • Grossly disorganized or catatonic behavior • Negative Symptoms (i. e. Affective flattening, Alogia, Avolition, etc) http: //dnalc. org/view/899 -DSM-IV-Criteria-for-Schizophrenia. html http: //pro. psychcentral. com/dsm-5 -changes-schizophrenia-psychotic-disorders/004336. html
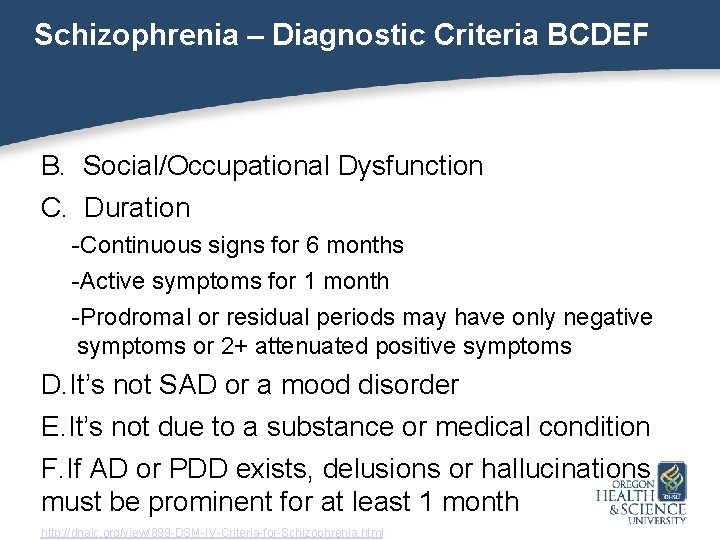
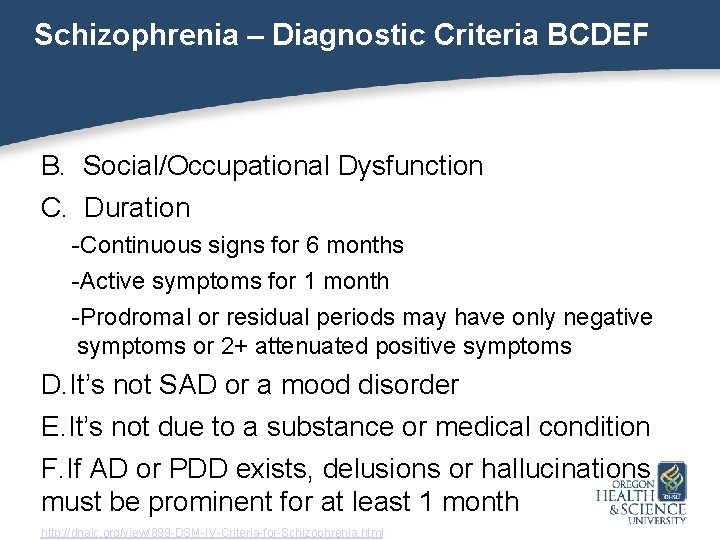
Schizophrenia – Diagnostic Criteria BCDEF B. Social/Occupational Dysfunction C. Duration -Continuous signs for 6 months -Active symptoms for 1 month -Prodromal or residual periods may have only negative symptoms or 2+ attenuated positive symptoms D. It’s not SAD or a mood disorder E. It’s not due to a substance or medical condition F. If AD or PDD exists, delusions or hallucinations must be prominent for at least 1 month http: //dnalc. org/view/899 -DSM-IV-Criteria-for-Schizophrenia. html
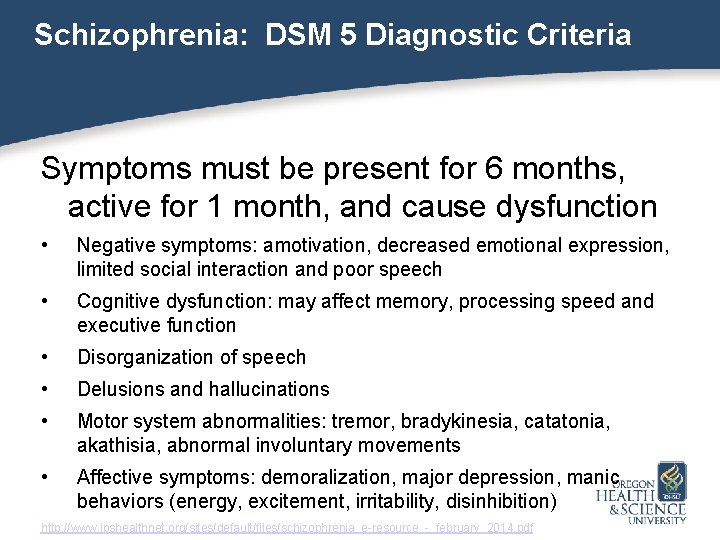
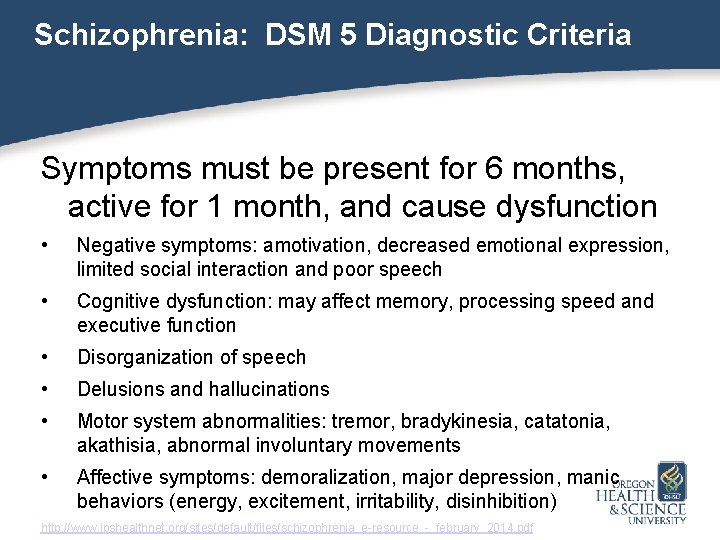
Schizophrenia: DSM 5 Diagnostic Criteria Symptoms must be present for 6 months, active for 1 month, and cause dysfunction • Negative symptoms: amotivation, decreased emotional expression, limited social interaction and poor speech • Cognitive dysfunction: may affect memory, processing speed and executive function • Disorganization of speech • Delusions and hallucinations • Motor system abnormalities: tremor, bradykinesia, catatonia, akathisia, abnormal involuntary movements • Affective symptoms: demoralization, major depression, manic behaviors (energy, excitement, irritability, disinhibition) http: //www. jpshealthnet. org/sites/default/files/schizophrenia_e-resource_-_february_2014. pdf
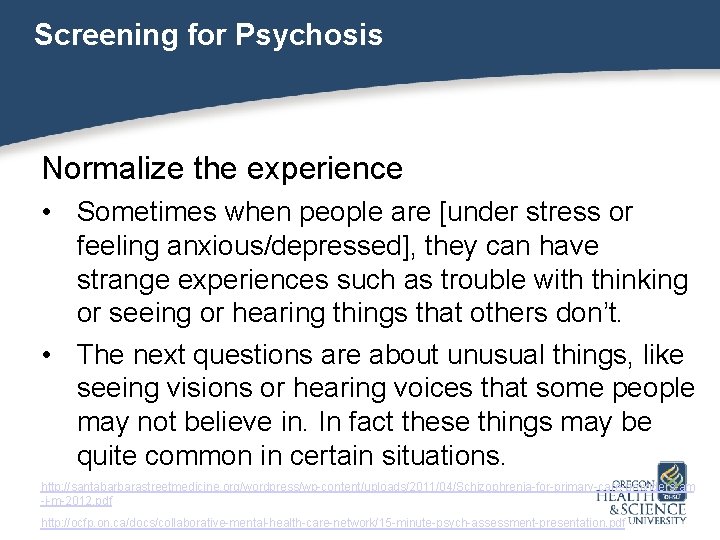
Screening for Psychosis Normalize the experience • Sometimes when people are [under stress or feeling anxious/depressed], they can have strange experiences such as trouble with thinking or seeing or hearing things that others don’t. • The next questions are about unusual things, like seeing visions or hearing voices that some people may not believe in. In fact these things may be quite common in certain situations. http: //santabarbarastreetmedicine. org/wordpress/wp-content/uploads/2011/04/Schizophrenia-for-primary-care-providers-am -j-m-2012. pdf http: //ocfp. on. ca/docs/collaborative-mental-health-care-network/15 -minute-psych-assessment-presentation. pdf
Screening for Psychosis • Have your eyes or ears (or brain) ever played tricks on you? • Have there ever been times when you heard or saw things that other people could not? • Have you ever heard voices that other people could not hear? I don't mean having good hearing, but rather…voices coming from inside your head talking to you or about you, or voices coming out of the air when there was no one around. Did you ever hear voices in this way? http: //santabarbarastreetmedicine. org/wordpress/wp-content/uploads/2011/04/Schizophrenia-for-primary-care-providers -am-j-m-2012. pdf http: //ocfp. on. ca/docs/collaborative-mental-health-care-network/15 -minute-psych-assessment-presentation. pdf
Screening for Psychosis • Have you had any strange or odd experiences lately that are difficult to explain or that others would find hard to believe? • Have you felt people are watching or following you? • Does anyone in particular seem intent on harassing or hurting you? • Have you felt like others can hear your thoughts or that you can hear another person’s thoughts? http: //santabarbarastreetmedicine. org/wordpress/wp-content/uploads/2011/04/Schizophrenia-for-primary-care-providers-am -j-m-2012. pdf http: //ocfp. on. ca/docs/collaborative-mental-health-care-network/15 -minute-psych-assessment-presentation. pdf
Screening for Psychosis • Have you ever felt that some mysterious force was inserting thoughts—that were definitely not your own thoughts—directly into your head? • Have you ever felt that your thoughts were being read by other people or were being stolen out of your mind? • Did you ever have a time when you felt that your mind was being taken over by others? • Have you ever felt that someone or something was trying to communicate directly with you by sending special signs or signals? http: //ocfp. on. ca/docs/collaborative-mental-health-care-network/15 -minute-psych-assessment-presentation. pdf
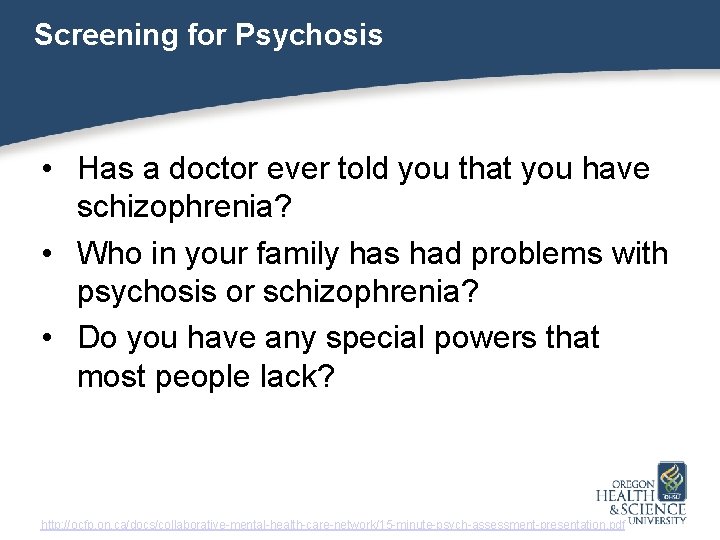
Screening for Psychosis • Has a doctor ever told you that you have schizophrenia? • Who in your family has had problems with psychosis or schizophrenia? • Do you have any special powers that most people lack? http: //ocfp. on. ca/docs/collaborative-mental-health-care-network/15 -minute-psych-assessment-presentation. pdf
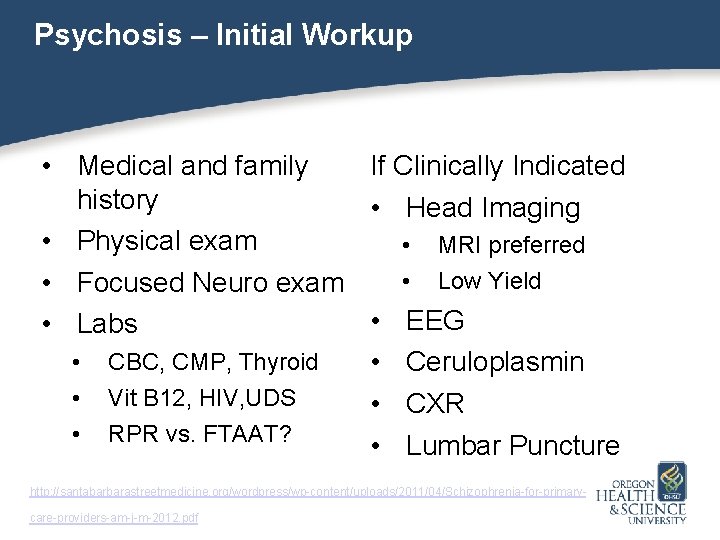
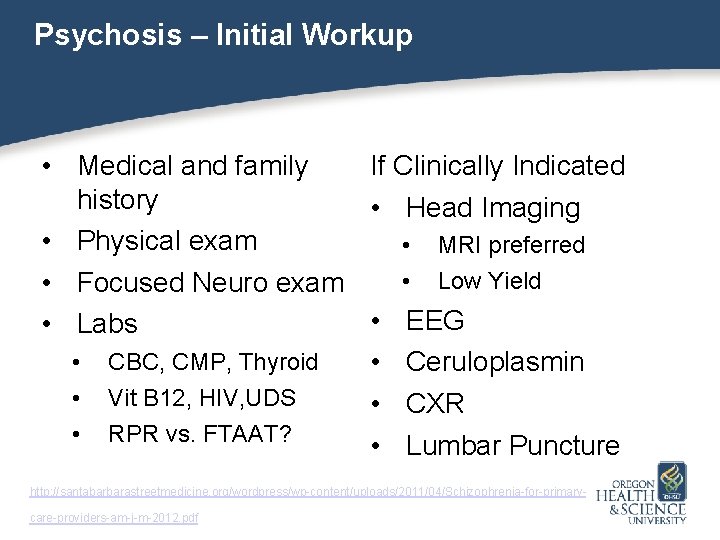
Psychosis – Initial Workup • Medical and family If Clinically Indicated history • Head Imaging • Physical exam • MRI preferred • Low Yield • Focused Neuro exam • EEG • Labs • CBC, CMP, Thyroid • Ceruloplasmin • Vit B 12, HIV, UDS • CXR • RPR vs. FTAAT? • Lumbar Puncture http: //santabarbarastreetmedicine. org/wordpress/wp-content/uploads/2011/04/Schizophrenia-for-primarycare-providers-am-j-m-2012. pdf
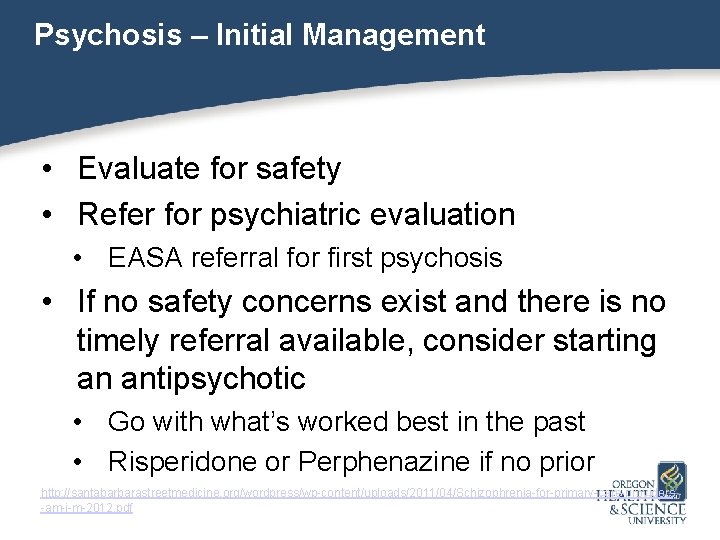
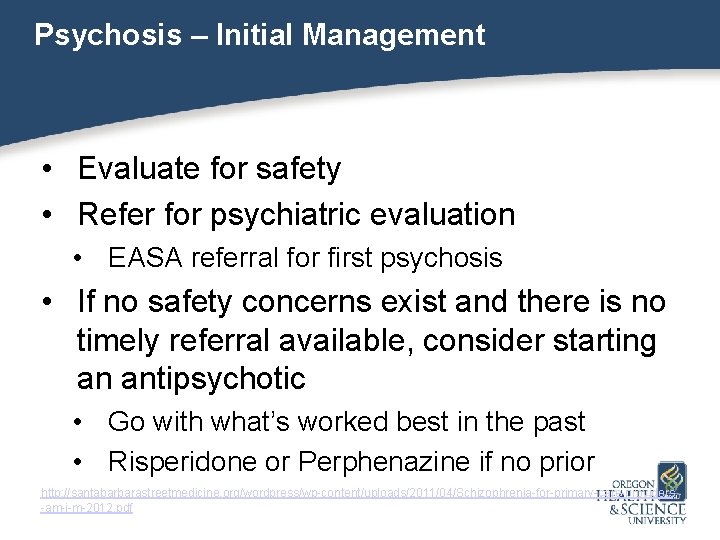
Psychosis – Initial Management • Evaluate for safety • Refer for psychiatric evaluation • EASA referral for first psychosis • If no safety concerns exist and there is no timely referral available, consider starting an antipsychotic • Go with what’s worked best in the past • Risperidone or Perphenazine if no prior http: //santabarbarastreetmedicine. org/wordpress/wp-content/uploads/2011/04/Schizophrenia-for-primary-care-providers -am-j-m-2012. pdf
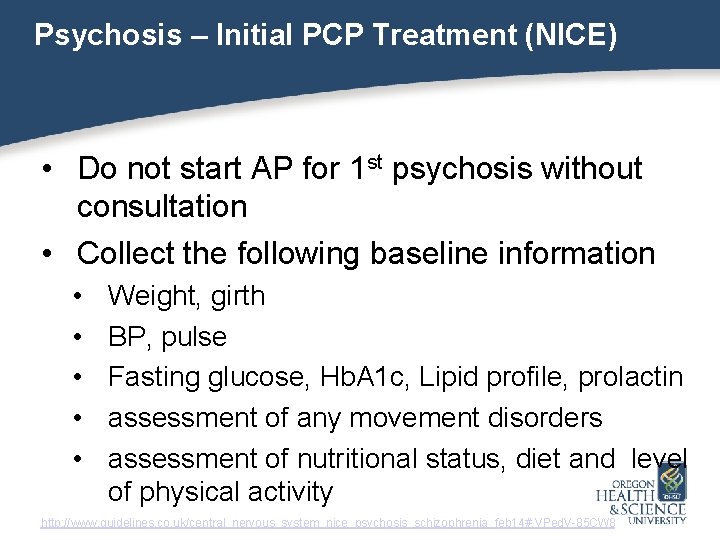
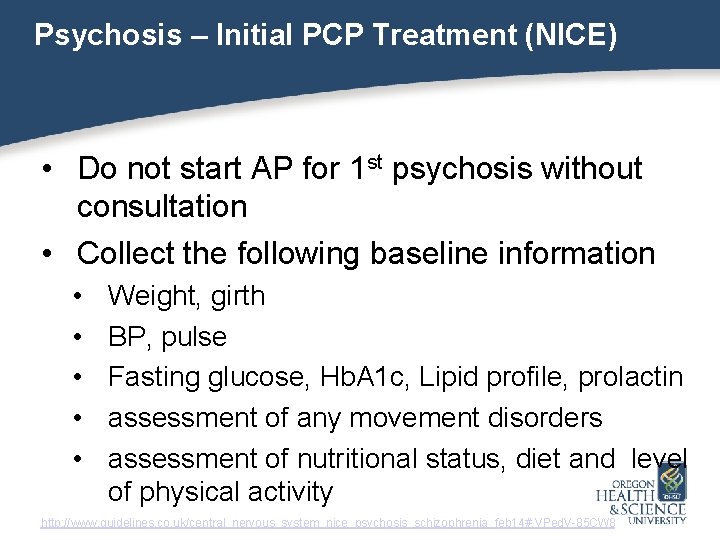
Psychosis – Initial PCP Treatment (NICE) • Do not start AP for 1 st psychosis without consultation • Collect the following baseline information • • • Weight, girth BP, pulse Fasting glucose, Hb. A 1 c, Lipid profile, prolactin assessment of any movement disorders assessment of nutritional status, diet and level of physical activity http: //www. guidelines. co. uk/central_nervous_system_nice_psychosis_schizophrenia_feb 14#. VPed. V-85 CW 8
Psychosis – Treatment Considerations APA Treatment Guidelines http: //psychiatryonline. org/pb/assets/raw/sitewide/practice_guidelines/schizophrenia. pdf http: //psychiatryonline. org/pb/assets/raw/sitewide/practice_guidelines/schizophrenia-watch. pdf http: //psychiatryonline. org/pb/assets/raw/sitewide/practice_guidelines/schizophrenia-guide. pdf NICE Treatment Guidelines http: //www. guidelines. co. uk/central_nervous_system_nice_psychosis_schizophrenia_feb 14#. VPed. V-85 CW 8 http: //www. nice. org. uk/guidance/cg 120/chapter/guidance National Medical Journal of India http: //www. nmji. in/archives/Volume_19_6_Nov_Dec_2006/Everyday_Practice_new/every_day_practice_19_6. htm Australian Guidelines http: //www. ycentral. com. au/wp-content/uploads/2014/11/Aust-Clinical-Guidelines-for-Early-Psychosis. pdf https: //www. ranzcp. org/Files/Resources/Publications/CPG/Clinician/APY 535 -pdf. aspx http: //www. guideline. gov/content. aspx? id=43862
Summary • Nearly 4% of primary care patients have psychotic symptoms • Less than 1% will have schizophrenia • Psychosis can arise for psychological, medical and substance-induced reasons • Those with psychotic symptoms tend to have worse medical outcomes • Treatment of psychosis includes medical assessment, routine monitoring and targeted interventions
The End! Pharmacologic Interventions for Psychosis Part I 03/03/16 http: //gizmodo. com/these-award-winning-underwater-photographs-are-dazzling-1760502451